Académique Documents
Professionnel Documents
Culture Documents
NCP2 - Dengue
Transféré par
Summer SuarezDescription originale:
Copyright
Formats disponibles
Partager ce document
Partager ou intégrer le document
Avez-vous trouvé ce document utile ?
Ce contenu est-il inapproprié ?
Signaler ce documentDroits d'auteur :
Formats disponibles
NCP2 - Dengue
Transféré par
Summer SuarezDroits d'auteur :
Formats disponibles
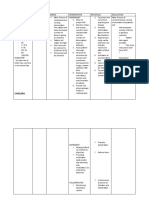
Assessment
Diagnosis
Planning
Intervention
Rationale
Evaluation
SUBJECTIVE : Nahihilo po ako, Nauuhaw at nanlalata as verbalized by the client.
Fluid Volume Deficit R/T Intravascular to Extravascular Plasma Leakage Secondary to Increase in Vascular Permeability.
OBJECTIVE : - Sunken, Dry eyes - Pale palpebral conjunctiva - Dry lips and mouth - Prolonged Capillary refill time [ 7 seconds ] - Poor skin turgor - Rapid, Thready Pulse Heart rate 110 Bpm RR 21 Bpm BP 90/60 Temp 39.2 C
After an hour of spontaneous fluid replacement, Patient will gradually abate signs and symptoms of fluid volume deficiency as evidenced by increasing blood pressure, decreasing heart rate, improving capillary refill time preferably below 5s and an improving skin turgor.
1. Anticipate fluid replacement by preparing peripheral route for IV transfusion.
* IV transfusion is a dependent nursing function. Anticipate doctors order by providing route for IV fluid replacement to save time and decrease risk for complications. * IV is considered as MEDICATION. Before initiating IV Replacement therapy, make sure that there is a current standing or verbal order from the doctor. * placing a glass of water or juice at patients bedside is the best way to encourage fluid intake. DHF patient are always thirsty prior to the defervescence stage.
2. Obtain doctors order for IV therapy As soon as possible to replace fluid volume loss IMMEDIATELY.
After an hour of intervention, Patients BP increased to 100/70, Tachycardia resolved as evidenced by a normal HR of 80bpm. CRT decreased from 7s down to 4s and there is a noticeable improvement in the clients skin turgor
3. Encourage fluid intake by placing a glass of juice or water within the patients reach.
4. Monitor total fluid intake and output every 2 hours.
*A urine output of .5 ml per kg/hr is insufficient for normal renal function and indicates onset of renal damage * Monitoring for trends for 2 to 3 days gives a more valid picture of the client's hydration status than monitoring for a shorter period. Darkcolored urine with increasing specific gravity reflects increased urine concentration. * To monitor and assess clients response and progress in the fluid replacement therapy
5. Watch trends in output for 3 days; include all routes of intake and output and note color and specific gravity of urine.
6. Monitor vital signs of clients with deficient fluid volume every hour. Observe for decreased pulse pressure first, then hypotension, tachycardia, decreased pulse volume, and increased or decreased body temperature
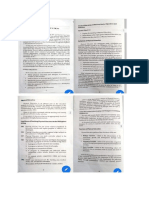
Assessment
Diagnosis
Planning
Intervention
Rationale
Evaluation
SUBJECTIVE : Ang sakit po ng tiyan ko pati mga tuhod ko at binti as verbalized by the client. OBJECTIVE : - Diaphoresis - Pupillary dilatation - Cold Clammy skin - Apparent loss of appetite A documented pain scale of 6 on Pain scale. Heart rate 125 bpm RR - 34 bpm
Acute Pain R/T Massive endothelial tissue damage Secondary to pyrogenic dissemination
After 2 hours of nursing interventions, Patient will describe the pain as tolerable with minimal and manageable side effects. Pain scale using should range from 0 to 4 and patient should show a decreased sign of pain induced parasympathetic stimulation.
1. Administer Acetaminophen at minimal dosage as ordered.
* Dengue patients experience hepatomagaly which suggests liver overcompensation that impairs drug metabolism, Acetaminophen should be given at minimal therapeutic dose. * To detect if the condition is improving or worsening, Or if there is a need to increase the dosage of the medication. * To promote adequate rest and sleep periods that will prevent fatigue and decrease severity of pain. * To decrease patients perception of pain and increase his tolerance to pain. This will also
After 2 hours of nursing interventions, The patient verbalized Hindi na po masyadong masakit ang katawan ko pati yung mata ko at tuhod Re assessing Pain scale revealed a score of 2. Diaphoresis is not anymore evident. Patient skin is now warm to touch
2. Carefully monitor patients response to the medication by assessing the client
3. Provide a quiet environment conducive to resting and sleep.
4. Provide non pharmacological comfort measures like deep breathing exercises, guided imagery, praying
and distractions like story increase the childs telling and listening to a adaptive pain soothing music behaviour.
Vous aimerez peut-être aussi
- NCP Micu Hascvd Cad - RioDocument5 pagesNCP Micu Hascvd Cad - RioRio BonifacioPas encore d'évaluation
- LRDR ProceduresDocument67 pagesLRDR ProceduresJustJ ThingsPas encore d'évaluation
- NCP - ERDocument5 pagesNCP - ERAnnelore ArcayPas encore d'évaluation
- Ineffective Tissue Perfusion - NCPDocument7 pagesIneffective Tissue Perfusion - NCPVianah Eve EscobidoPas encore d'évaluation
- NCP BronchopneumoniaDocument8 pagesNCP BronchopneumoniaCrisantaCasliPas encore d'évaluation
- Sample Letter Templates (4th Year)Document49 pagesSample Letter Templates (4th Year)Yna LafuentePas encore d'évaluation
- Health HistoryDocument2 pagesHealth HistoryFaisaliah UngkakayPas encore d'évaluation
- Assessment/ Cues Nursing Diagnosis Background Knowledge Goal and Objectives Nursing Interventions and Rationale EvaluationDocument6 pagesAssessment/ Cues Nursing Diagnosis Background Knowledge Goal and Objectives Nursing Interventions and Rationale EvaluationimnasPas encore d'évaluation
- Nursing Care Plan EportfolioDocument14 pagesNursing Care Plan Eportfolioapi-279212367Pas encore d'évaluation
- LOG101 Exercise No. 2 - Types of Definitions 20230217091032Document2 pagesLOG101 Exercise No. 2 - Types of Definitions 20230217091032Daniella TimbolPas encore d'évaluation
- ASSESSMENTDocument2 pagesASSESSMENTColeen PequitPas encore d'évaluation
- NCP DM and HCVDDocument3 pagesNCP DM and HCVDMAYBELINE OBAOB100% (1)
- Case Study RespiDocument3 pagesCase Study RespiMark Jheran AlvarezPas encore d'évaluation
- Assessment Nursing Diagnosis Planning Nsg. Intervention Rationale Evaluation SubjectiveDocument6 pagesAssessment Nursing Diagnosis Planning Nsg. Intervention Rationale Evaluation SubjectiveIngrid Eunice ConcordiaPas encore d'évaluation
- Ineffective Peripheral Tissue Perfusion Related To Vasoconstriction Secondary To High Glucose Level.Document6 pagesIneffective Peripheral Tissue Perfusion Related To Vasoconstriction Secondary To High Glucose Level.SAROL, RYAN CHRISTIAN B.Pas encore d'évaluation
- Drug StudyDocument2 pagesDrug StudyNeri ChavezPas encore d'évaluation
- Lapkas HegDocument1 pageLapkas HegkurniaPas encore d'évaluation
- Rabi PurDocument3 pagesRabi PurDiana Laura LeiPas encore d'évaluation
- MODULE-9-Biotechnology, Genetically Modified Organisms, and Gene TherapyDocument5 pagesMODULE-9-Biotechnology, Genetically Modified Organisms, and Gene TherapyKerry NuñezPas encore d'évaluation
- NCP DM Group 6Document4 pagesNCP DM Group 6Jeffrey Calicdan BucalaPas encore d'évaluation
- Ongoing AppraisalDocument2 pagesOngoing AppraisalLouisa Marie MirandaPas encore d'évaluation
- NCP Form Hyper ThermDocument1 pageNCP Form Hyper ThermomarskyPas encore d'évaluation
- HyperthermiaDocument2 pagesHyperthermiapamgee100% (11)
- NCP PainDocument2 pagesNCP PainApril_Ivy_Raga_3835Pas encore d'évaluation
- Health-Perception-Health-Management PatternDocument3 pagesHealth-Perception-Health-Management PatternBela MillenaPas encore d'évaluation
- Assignment For Oxy. Online BasedDocument5 pagesAssignment For Oxy. Online BasedNurhassem Nor AkangPas encore d'évaluation
- Nursing Care Plan On Platelet DisordersDocument8 pagesNursing Care Plan On Platelet DisordersbhavanaPas encore d'évaluation
- Actual NCPDocument2 pagesActual NCPbaki0146Pas encore d'évaluation
- Copd - NCPDocument6 pagesCopd - NCPMonique Sacherow BacherPas encore d'évaluation
- Case Study Final PortraitDocument11 pagesCase Study Final PortraitZhy CaluzaPas encore d'évaluation
- Reflective Journal 1Document4 pagesReflective Journal 1api-365605511Pas encore d'évaluation
- Physical Exam - AppendectomyDocument8 pagesPhysical Exam - Appendectomyirish felixPas encore d'évaluation
- COLCHICINE pptx1800128929Document15 pagesCOLCHICINE pptx1800128929April Mergelle LapuzPas encore d'évaluation
- Rufino, Leslie Kriztel S. BSN 3-2 Group 1Document6 pagesRufino, Leslie Kriztel S. BSN 3-2 Group 1Deinielle Magdangal RomeroPas encore d'évaluation
- Case Study 1 (Pneumonia)Document13 pagesCase Study 1 (Pneumonia)Kate EscotonPas encore d'évaluation
- Subjective: "Sumikip Ang Dibdib Ko at Hindi Ako Makahinga NG Maayos" As IndependentDocument2 pagesSubjective: "Sumikip Ang Dibdib Ko at Hindi Ako Makahinga NG Maayos" As IndependentCorinnePas encore d'évaluation
- Request Letter For CHNDocument1 pageRequest Letter For CHNdusty kawiPas encore d'évaluation
- NCP RiskDocument2 pagesNCP RiskNorries Jonell CaballarPas encore d'évaluation
- NCP MeningitisDocument2 pagesNCP MeningitisARISPas encore d'évaluation
- A Client With Cushing's Syndrome: Nursing Care PlanDocument1 pageA Client With Cushing's Syndrome: Nursing Care PlanJulius Caesar ColladoPas encore d'évaluation
- NCM 114 - NCPDocument3 pagesNCM 114 - NCPReysiela Mae ValinoPas encore d'évaluation
- Nursing Progress Notes FINALDocument2 pagesNursing Progress Notes FINALROXANNE V. LOPEZPas encore d'évaluation
- Impaired Tissue PerfusionDocument2 pagesImpaired Tissue PerfusionLyka Mae Imbat - PacnisPas encore d'évaluation
- NCP Risk InfectionDocument1 pageNCP Risk InfectionEni RahmawatiPas encore d'évaluation
- Generic Name: Classification Indication:: Hema KDocument2 pagesGeneric Name: Classification Indication:: Hema KKristine YoungPas encore d'évaluation
- III. Nursing Care Plan Nursing Priority No. 1: Ineffective Airway Clearance Related To Excessive Accumulation of Secretions Secondary To PneumoniaDocument6 pagesIII. Nursing Care Plan Nursing Priority No. 1: Ineffective Airway Clearance Related To Excessive Accumulation of Secretions Secondary To PneumoniaRae Marie Aquino100% (1)
- Case Study On MalariaDocument18 pagesCase Study On MalariaRameshKrishnanPas encore d'évaluation
- Hyperthermia and Risk For AspirationDocument3 pagesHyperthermia and Risk For AspirationAlmyr RimandoPas encore d'évaluation
- NCP Cough PneumoniaDocument2 pagesNCP Cough PneumoniaAirme Raz AlejandroPas encore d'évaluation
- Sample (Concept Map)Document1 pageSample (Concept Map)NMDNMSSDPas encore d'évaluation
- Diseases Associated in Carbohydrates 3Document2 pagesDiseases Associated in Carbohydrates 3Mary Joy FalcesoPas encore d'évaluation
- Case CHFDocument10 pagesCase CHFAgnes Erlita Distriani Patade50% (2)
- Example of Drug StudyDocument2 pagesExample of Drug Studydonna mae junioPas encore d'évaluation
- Nursing Care Plan 1: Diagnosis Goal Nursing Interventions RationaleDocument8 pagesNursing Care Plan 1: Diagnosis Goal Nursing Interventions RationaleTrysna Ayu SukardiPas encore d'évaluation
- Common ER EquipmentsDocument3 pagesCommon ER EquipmentsApple LlanesPas encore d'évaluation
- PA Tool Sample - JIJIDocument35 pagesPA Tool Sample - JIJIJirah RuedasPas encore d'évaluation
- Drug Study Domperidone CompressDocument1 pageDrug Study Domperidone CompressAngelica TolledoPas encore d'évaluation
- Learning Derived (Lysha)Document1 pageLearning Derived (Lysha)Choy DavidPas encore d'évaluation
- C C C C C C C C C C C C C C C C C C C C C C C C C C C C C C C CDocument5 pagesC C C C C C C C C C C C C C C C C C C C C C C C C C C C C C C CMichaela ArellanoPas encore d'évaluation
- Nursing Management of Patient With Community Acquired PneumoniaDocument5 pagesNursing Management of Patient With Community Acquired PneumoniaSummer SuarezPas encore d'évaluation
- Nursing Management of A Patient With An Ectopic PregnancyDocument8 pagesNursing Management of A Patient With An Ectopic PregnancySummer SuarezPas encore d'évaluation
- NCP (Afp)Document7 pagesNCP (Afp)Summer SuarezPas encore d'évaluation
- NCP2 - Acute PainDocument2 pagesNCP2 - Acute PainSummer SuarezPas encore d'évaluation
- A Diagnostic Tool That Measures and Records The Electrical Activity of The Heart. - ECG Is Recorded by Applying Electrodes and Connecting Them To A Recording ApparatusDocument12 pagesA Diagnostic Tool That Measures and Records The Electrical Activity of The Heart. - ECG Is Recorded by Applying Electrodes and Connecting Them To A Recording ApparatusSummer SuarezPas encore d'évaluation
- Drug Study (AFP)Document10 pagesDrug Study (AFP)Summer SuarezPas encore d'évaluation
- Case Study - Diabetes Mellitus (Nutrition&Dietetics)Document10 pagesCase Study - Diabetes Mellitus (Nutrition&Dietetics)Summer Suarez100% (1)
- FNCPDocument1 pageFNCPSummer SuarezPas encore d'évaluation
- Generic Name Indication Action Contraindication Adverse Reaction Nursing ConsiderationDocument8 pagesGeneric Name Indication Action Contraindication Adverse Reaction Nursing ConsiderationSummer SuarezPas encore d'évaluation
- FNCPDocument1 pageFNCPSummer SuarezPas encore d'évaluation
- Simulation Scenarios PDFDocument59 pagesSimulation Scenarios PDFryan24Pas encore d'évaluation
- QNet Products - Himalayan Crystal CollectionDocument24 pagesQNet Products - Himalayan Crystal CollectionGioan NguyenPas encore d'évaluation
- PEDocument11 pagesPEMary Joy QuilangPas encore d'évaluation
- Conduction System of HeartDocument2 pagesConduction System of HeartEINSTEIN2DPas encore d'évaluation
- Dragon Bonus WorkoutsDocument14 pagesDragon Bonus WorkoutsJeremiahgibson67% (3)
- Decreased Cardiac OutputDocument7 pagesDecreased Cardiac OutputKian Justin HidalgoPas encore d'évaluation
- PE Coursework NEA FINALDocument18 pagesPE Coursework NEA FINALkarpathos999Pas encore d'évaluation
- Marieb ch11bDocument28 pagesMarieb ch11bapi-229554503Pas encore d'évaluation
- 2000 - Mackenzie - Rockport Fitness Walking TestDocument5 pages2000 - Mackenzie - Rockport Fitness Walking TestHerdiantri SufriyanaPas encore d'évaluation
- Lab ReportDocument48 pagesLab ReportAthirah JeffryPas encore d'évaluation
- JB34 v1-0 14apr10 W502 Slides Day 2Document148 pagesJB34 v1-0 14apr10 W502 Slides Day 2Janardhan Rao MalakapalliPas encore d'évaluation
- Practica 2Document38 pagesPractica 2Sofia MoreiraPas encore d'évaluation
- Department of Education: Republic of The PhilippinesDocument21 pagesDepartment of Education: Republic of The PhilippinesJB Lopez100% (1)
- Advancement in Patient Monitoring SystemDocument23 pagesAdvancement in Patient Monitoring SystemNawaz Sherif NPas encore d'évaluation
- Detection of Cardiac Disorder Using MATLAB BasedDocument4 pagesDetection of Cardiac Disorder Using MATLAB BasedSeira LoyardPas encore d'évaluation
- Cabahug, Victoria Mae Module 1Document19 pagesCabahug, Victoria Mae Module 1bekbekk cabahugPas encore d'évaluation
- Chronic Adaptations To Training: Liveitup2Document20 pagesChronic Adaptations To Training: Liveitup2dvenumohanPas encore d'évaluation
- The Effect of Skipping Rope Exercise On Physical and Cardiovascular Fitness Among Collegiate MalesDocument6 pagesThe Effect of Skipping Rope Exercise On Physical and Cardiovascular Fitness Among Collegiate MalesK. M. Junayed AhmedPas encore d'évaluation
- Division Self Learning Modules Peh 4 Week4Document17 pagesDivision Self Learning Modules Peh 4 Week4ayra cyrenePas encore d'évaluation
- Total Hockey Training (Skahan, Sean)Document305 pagesTotal Hockey Training (Skahan, Sean)imogenis_puzzlePas encore d'évaluation
- Manua Siemes PDFDocument462 pagesManua Siemes PDFleoenpiedra100% (1)
- Newborn Resuscitation (Newborn CPR) BSN 12C: Madeline N. Gerzon, RN, MM Clinical Instructor Davao Doctors CollegeDocument59 pagesNewborn Resuscitation (Newborn CPR) BSN 12C: Madeline N. Gerzon, RN, MM Clinical Instructor Davao Doctors CollegemgerzonPas encore d'évaluation
- 5431 Titanium Console Manual TT1.0 2.0 3.0 ENGLISH PRINTDocument19 pages5431 Titanium Console Manual TT1.0 2.0 3.0 ENGLISH PRINTMilos VujasinovicPas encore d'évaluation
- Pratice Questions For NCLEX PDFDocument413 pagesPratice Questions For NCLEX PDFEmily97% (29)
- Kenneth CooperDocument9 pagesKenneth CooperAna Prancheska MatibagPas encore d'évaluation
- 2020 MS - Hurlstone Agricultural HS - Trial Paper (With Solutions)Document61 pages2020 MS - Hurlstone Agricultural HS - Trial Paper (With Solutions)Sia GuptaPas encore d'évaluation
- Problem-Based Learning For Nursing Students: Assessing Risk, Negotiating For Behavior Change, Respecting CultureDocument72 pagesProblem-Based Learning For Nursing Students: Assessing Risk, Negotiating For Behavior Change, Respecting CultureAnjelle Roselle Flores GaguiPas encore d'évaluation
- Pulsometro LabviewDocument16 pagesPulsometro Labviewm240597Pas encore d'évaluation
- Exercise Prescription For ElderlyDocument10 pagesExercise Prescription For ElderlyWasemBhatPas encore d'évaluation
- Physical Education: Grade 7Document103 pagesPhysical Education: Grade 7Anngela Arevalo BarcenasPas encore d'évaluation