Académique Documents
Professionnel Documents
Culture Documents
Gerontology Project: Name: Onipha Tappin Date: 1 Teacher: Sis Smith Class: Group 16
Transféré par
Blake KamminTitre original
Copyright
Formats disponibles
Partager ce document
Partager ou intégrer le document
Avez-vous trouvé ce document utile ?
Ce contenu est-il inapproprié ?
Signaler ce documentDroits d'auteur :
Formats disponibles
Gerontology Project: Name: Onipha Tappin Date: 1 Teacher: Sis Smith Class: Group 16
Transféré par
Blake KamminDroits d'auteur :
Formats disponibles
Gerontology Project
Name: Onipha Tappin Date: 1st Aug, 2013 Teacher: Sis Smith Class: Group 16
Table of contents
Introduction.. Biographical Data.... Subjective Data. Review of Systems. Head to Toe Assessment Social Support System... Care Plan...
Introduction
In this project you will find the assessment done on my choice of gerontology client. The home chosen for the setting of this project was the Bishop John E. Knight home for the elderly.
Assessment
Biographical Data
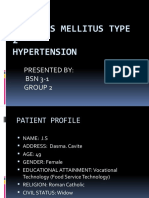
Name: Clara J King Sex: Female D.O.B: 12/09/31 Age: 81 years Address: Clare Hall Village Contact #: Tel: 560-3695
Country of Birth: Antigua Nationality: Antiguan Religion: Methodist Race: Black Place of Employment: None Marital Status: Married (spouse deceased) Next of Kin: Velvet Charles Address: Glanville Village Medical Insurance: No Family physician: Dr Stevens The source of information is reliable Informant: Clara King Relationship: Friend Tel: 720-1003
Chief Complaint No complaints
History of Present Illness
Hypertension
Past Medical History
Childhood Illness: History of Measles. No history of mumps, mumps, chickenpox, rubella, frequent ear infections, frequent streptococcal infections or sore throats, rheumatic fever, scarlet fever, pertussis, or asthma.
Accidents/Injuries: No accidents or injuries
Chronic Illnesses: Hypertension
Obstetric History: Gravida 2 para 2
Immunization:
All childhood vaccinations received measles, mumps, rubella, chickenpox, hepatitis B, diphtheria, polio, Tetanus 2nd booster.
Hospitalizations: Surgical removal of Fibroids in the 1970s at age 43, hospitalized for two weeks at the Holberton hospital.
Last Examinations: Every Sunday.
Allergies: No known allergies
Current medications: Zesteretic 20mg daily, ASA 81mg daily.
Current health status
General health is OK. No changes in appetite or weight. Able to perform ADLs without difficulty. No history of weakness, unexplained fevers, or unusual symptoms.
Family History
Eugenia is the 2nd child out of 3, parents were married, mother had hypertension and sister also. Her husband died from complications of hypertension
Psychosocial History
Self-concept- Completed education to the 7th grade of secondary school then stayed to help care for the family. Believes in god and is very religious. Believes self to be loving, kind, Lifestyle- No smoking. Drinks wine on special occasions.
Diet-Eats breakfast but sometimes skip lunch due to lack of appetite but eats dinner, believes nutritional status is adequate. Gets approximately 12 hours of sleep. Spends most of the day sleeping and watching television. Exercise- She exercises every morning. Social- Describes life as happy and contented. Has a good relationship with family and other residents.
Review of Systems
Neurological: No history of fainting, seizures, loss of consciousness, head injuries, changes in cognition or memory, hallucinations, disorientation, speech problems, sensory disorientation such as numbness, tingling or loss of sensations, motor problems, problems with gait, balance or coordination. No impact on ADLs.
Respiratory: No history of breathing problems, cough, bloody sputum, SOB with activity, wheezing, pneumonia, bronchitis or tuberculosis. Cardiovascular: History of hypertension. No history of chest pain, palpitations, murmurs, skipped beats, awakening at night with SOB, dizzy spells, cold hand or feet, colour changes in hands and feet, pain in the legs while walking, swelling of the extremities, hair loss on legs, poor wound healing. Has never done an EKG.
Gastrointestinal: No history, indigestion, change in appetite, heartburn, nausea, vomiting, liver or gallbladder disease, jaundices, changes in bowel patterns; colour of stool, constipation or diarrhoea, hemorroids, weight changes (loss or gain), use of laxatives and acids.
Genitourinary: No history of pain on urination, burning, urgency, dribbling, incontinence, hesitancy, changes in urine stream or colour, no history of urinary tract infections, kidney infections, kidney disease, kidney stones, or frequent urination at night.
Musculoskeletal: No history of fractures, history of sprains, muscle cramps, pain, weakness, noise with movement, spinal deformities, low back pain, loss of height, osteoporosis, degenerative joint disease, or rheumatoid arthritis.
Skin: No history of rashes, lumps, sores, mild dryness, no colour changes. No history of changes in hair or nail.
Head/Neck: No history of unusual headaches, head injury or surgery, dizziness, loss of consciousness or fainting. No history of stiff neck, injury or surgery, pain with movement of head and neck, swollen glands, nodes or masses.
Eye: No history of blurred vision, vision loss, colour or depth perception.
Ears: No history of difficulty hearing, sensitivity to sounds, ear pain, drainage, vertigo, ear infections, ringing, fullness in the ears.
Nose: No history of nosebleeds, use of recreational drugs, allergies, broken nose, difficulty breathing through the nose, sneezing.
Mouth/Throat: No history of sore throats, streptococcal infections, mouth sores, oral herpes, difficulty chewing or swallowing, changes in sense of taste.
Breast: No history of masses, lumps, discharge, pain, swelling, changes in breast or nipple, breast cancer, breast surgery.
Head-to-Toe Assessment
Height: 55 B/P: 110/70mmHg Pulse: 76 bpm
Weight: 170lbs Temp: 97F Resp: 20 bpm
General health survey: Eugenia Jones is a 81 year old black female, she articulates clearly, ambulates without difficulty.
Skin, Hair, Nails: skin, uniform in colour, warm, dry, intact, turgor good. Hair, normal distribution and texture, no lice or other inhabitants, mostly white and sheared. Nails, no clubbing, biting present, no discolorations. Nail beds pink and firm with prompt capillary refill. Wrinkles on face.
Head: Normocephalic, no lesions, lumps, scaling, parasites, or tenderness. Face, symmetric, no weakness, no involuntary movements.
Eyes: Glasses worn when reading. Visual fields adequate. Eye movement adequate. Sclera clear. Eye lashes and eye browns are white. Ears: Symmetrical with no deformities. Canals clear. Pinna, no mass, lesions, scaling, discharge, or tenderness on palpation. Whispered words equally heard.
Nose: Symmetrical. No deformities or tenderness on palpation. Nares patent. Mucosa pink, no lesions. Septum midline, no perforation. No sinus tenderness.
Mouth: Mucosa and gums pink, no lesions or bleeding. Slight yellowing to teeth noted, no cavities present, four incisors missing. Tongue symmetric, protrudes midline. Uvula rises midline. Gag reflex present. Dentures worn.
Neck: Symmetric, no masses, tenderness. Trachea midline. Thyroid nonpalpable, not tender. Neck supple with full ROM.
Spine and Back: Normal alignment of spine, no deformities noted. No tenderness on palpation.
Thorax and Lungs: Equal bilateral chest expansion. Breath sounds audible. Diaphragmatic excursion equal bilaterally. Lungs field clear with no adventitious sounds.
Breasts: Symmetric, no discharge or lesions. No masses or tenderness on palpation.
Heart: No pulsations, lifts or heaves. Heart sounds normal, no murmurs or thrills present.
Abdomen: Round, symmetric. Skin smooth with no lesions, scars or striae. Bowel sounds present, no bruits. Abdomen soft, no organomegaly.
Musculoskeletal: Colour distribution on extremities equal, no deformities or lesions. No tenderness. All peripheral pulses present and equal bilaterally. Full ROM present. No tenderness or weakness in joints. Muscle strength able to maintain flexion against resistance and without tenderness.
Neurologic: Alert and oriented to person place and time. Thought coherent. Remote and recent memories intact. Cranial nerves ii through xii intact. Sensory, pin prick, light touch intact. Able to identify objects. No atrophy, weakness or tremors. No gait abnormalities. Cerebellar, finger to nose smoothly intact.
Social support system
The client has a very good social system her friends visit regularly and her family visits during holidays. They aid in meeting all her economic and other needs.
Physical and psychological environment The physical and psychological environment is very structured and comforting. Everything is free from clutter so there is a reduced risk for injury. It is also filled with personal items that offer comfort. There is also a lot of stimuli available without it overloading the client.
Area of need for education
The area identified for need for education is the need for proper hypertension management. If this is not done properly it may lead to other health problems example stroke, heart attack and heart failure, vision problems and poor blood supplies to lower extremities. The reason this area was identified is because the client has fluctuating blood pressures. She also needs education on proper stress management as this causes her fluctuating blood pressures.
Assessment Elderly female client with difficulty managing hypertension
Nursing Diagnosis Knowledge deficit related to managing blood pressure evidence by clientsfluctuating blood pressures
Goal Client will be to adequately manage blood pressure
Interventions - Monitor blood pressure readings daily. This aids in noting elevation or depression of Bp.
Outcome Criteria - client able to adequately manage blood pressure
- Advise client to take prescribed medication ad directed at all times unless asked to stop by doctor. This aids In maintaining an adequate blood pressure level. - Keep a dated record of Blood pressure readings. This keeps a set record of blood pressure changes. - Assist client in finding ways to
manage stress. As stress causes an increase in blood pressure. - Encourage regular exercise approximately 30-40 minutes daily 3-4 times per week. This aids in both managing blood pressure and relieves stress. - encourage client to maintain a healthy weight. Excess weight increases risk for high blood pressure and cholesterol problems. -Advise client to decrease salt intake and foods high in fat and cholesterol. These cause a rise in blood pressure.
Assessment Elderly client with difficulty managing stress
Nursing Diagnosis Impaired coping mechanism related to stress evidenced by clients fluctuating blood pressures.
Goal Client will have an adequate coping mechanism to manage stress with health teaching
Interventions Encourage the client to think positively when under stressful situations as this help to calm her thus relieving stress.
Outcome Criteria Client is adequately able to manage stress
Encourage the client to try relaxing exercises such as meditating reading etc. as this aids to relieve stress.
Encourage the client to seek spiritual guidance(i f she is spiritual) a this offers guidance and relieves stress
Managing Hypertension Monitor blood pressure regularly. This notes elevation or depression in blood pressure. Keep a dated record of blood pressure readings. This aids in better managing blood pressure and also aids clinician in noting changes in your blood pressure. Managing stress aids in managing your blood pressure. Stress increases you blood pressure. So practice activities that you find restful to aid in lowering your stress level thereby lowering your blood pressure. Limit alcohol or cease alcohol consumption. Get regular exercise approximately 30-40 minutes daily 3-4 times a week. This manages stress and maintains a healthy lifestyle. Decrease salt intake, read packages of food products. Take prescribe medication as ordered unless contraindicated by your doctor. Reduce intake of foods high in fat and cholesterol. Maintain a healthy weight. Excess weight increases for high blood pressure and cholesterol problems. Stop smoking. It damages blood vessels which is dangerous in person with high blood pressure.
Vous aimerez peut-être aussi
- Chronic Diseases - Lymes, Hpv, Hsv Mis-Diagnosis and Mistreatment: A New Approach to the EpidemicD'EverandChronic Diseases - Lymes, Hpv, Hsv Mis-Diagnosis and Mistreatment: A New Approach to the EpidemicÉvaluation : 5 sur 5 étoiles5/5 (1)
- Oniphas Homewoek 2Document14 pagesOniphas Homewoek 2Blake KamminPas encore d'évaluation
- SOAP Note 1 - Breast CADocument4 pagesSOAP Note 1 - Breast CAacvalvarioPas encore d'évaluation
- Low Back PainDocument9 pagesLow Back PainDoc AchondoPas encore d'évaluation
- Acute PancreatitisDocument7 pagesAcute PancreatitisPatrick DycocoPas encore d'évaluation
- Health Assessment Project: Name: Ena Lewis Tutor: Sis Francis Group: 15Document27 pagesHealth Assessment Project: Name: Ena Lewis Tutor: Sis Francis Group: 15Blake KamminPas encore d'évaluation
- 6904 Module 1 HistoryDocument3 pages6904 Module 1 Historyapi-618492022Pas encore d'évaluation
- 312 ENT Patient InterviewDocument5 pages312 ENT Patient InterviewDorish Faith CarilloPas encore d'évaluation
- HSP Case Presentation PDFDocument71 pagesHSP Case Presentation PDFJoan Luis100% (1)
- Constitutional: General Appearance: Healthy-Appearing, Well-Nourished, and Well-Developed. Level ofDocument10 pagesConstitutional: General Appearance: Healthy-Appearing, Well-Nourished, and Well-Developed. Level ofRichard ObinwankwoPas encore d'évaluation
- CASE 3 MEDICINE JULY 10 2019 AcutePyeloDocument15 pagesCASE 3 MEDICINE JULY 10 2019 AcutePyeloTrisPas encore d'évaluation
- Clinical Case: Section A - Group 8Document68 pagesClinical Case: Section A - Group 8madison Deli100% (1)
- Chief ComplaintDocument7 pagesChief ComplaintyohannesPas encore d'évaluation
- Final Assessment Soap NoteDocument13 pagesFinal Assessment Soap Noteapi-494643478100% (3)
- Genome PaperDocument7 pagesGenome Paperapi-444163791100% (1)
- Bedside Rounds ZCMC Ward 8: History Taking and Physical ExaminationDocument28 pagesBedside Rounds ZCMC Ward 8: History Taking and Physical ExaminationneilaldentanPas encore d'évaluation
- Final HX and Physical Dec 2022Document5 pagesFinal HX and Physical Dec 2022Mallory ZaborPas encore d'évaluation
- History 1Document11 pagesHistory 1KaleabPas encore d'évaluation
- Case Study - NSVD ScribdDocument20 pagesCase Study - NSVD ScribdShar EnriquezPas encore d'évaluation
- Health AssessmentDocument26 pagesHealth AssessmentBlake Kammin100% (1)
- Soap 2Document5 pagesSoap 2api-456313554Pas encore d'évaluation
- Jocelyn PrietoDocument11 pagesJocelyn PrietoAndrew Joever PrietoPas encore d'évaluation
- Carbuncle, Incision, Drainage, DebridementDocument11 pagesCarbuncle, Incision, Drainage, DebridementAlvin Germo PasuquinPas encore d'évaluation
- Sample SoapDocument9 pagesSample SoapDouglas Greg Cook90% (20)
- Name: Onipha Tappin DATE: 31 OCTOBER, 2012 Teacher: Is Francis Subject: Health AssessmentDocument26 pagesName: Onipha Tappin DATE: 31 OCTOBER, 2012 Teacher: Is Francis Subject: Health AssessmentNichola TappinPas encore d'évaluation
- Grand Case PresentationDocument50 pagesGrand Case PresentationJean Michelle100% (1)
- A Narrative Report On: Physical AssesmentDocument11 pagesA Narrative Report On: Physical AssesmentchelseyPas encore d'évaluation
- Final Practicum - Soap Note 1Document16 pagesFinal Practicum - Soap Note 1api-49464347867% (3)
- Form Health History Documentation: Biographical DataDocument7 pagesForm Health History Documentation: Biographical DataSandra SanonPas encore d'évaluation
- Junsay, Twinkle Mae D. Section A - Group 10 History #1Document15 pagesJunsay, Twinkle Mae D. Section A - Group 10 History #1Twinkle Mae JunsayPas encore d'évaluation
- Nurs 5018 - Soap Note Well-Woman ExamDocument7 pagesNurs 5018 - Soap Note Well-Woman Examapi-308904543Pas encore d'évaluation
- Scrib AssignmentDocument9 pagesScrib AssignmentShayne Jessemae AlmarioPas encore d'évaluation
- Template Gyn Lo Abd PainDocument18 pagesTemplate Gyn Lo Abd PainHassan HarirPas encore d'évaluation
- Comprehensive H and P ExampleDocument5 pagesComprehensive H and P ExampleMallory ZaborPas encore d'évaluation
- Highest Blood Pressure Was 140/90 MMHGDocument5 pagesHighest Blood Pressure Was 140/90 MMHGFG ArciagaPas encore d'évaluation
- FNP 2 ObesityDocument24 pagesFNP 2 Obesityapi-554096544Pas encore d'évaluation
- Pedia - History Taking and Physical Exam - PGI Leira BarbosaDocument6 pagesPedia - History Taking and Physical Exam - PGI Leira BarbosaLeira BarbosaPas encore d'évaluation
- NU 665 Pediatric Gastrointestinal Case Study - Michelle - StewardDocument10 pagesNU 665 Pediatric Gastrointestinal Case Study - Michelle - StewardMichelle StewardPas encore d'évaluation
- IM Gastro FinalDocument10 pagesIM Gastro FinalIzzyMaxinoPas encore d'évaluation
- Geri SOAPsampleDocument8 pagesGeri SOAPsampleJacquelinePas encore d'évaluation
- Date and Time: June 23, 2018, 3PM Chief Complaint: Difficulty of Breathing History of Present IllnessDocument3 pagesDate and Time: June 23, 2018, 3PM Chief Complaint: Difficulty of Breathing History of Present IllnessConcepcion R. AquinoPas encore d'évaluation
- Sample Write UpDocument2 pagesSample Write UpNar Patrick Padilla100% (1)
- Grand Case PresentationDocument44 pagesGrand Case PresentationAilyn LoroPas encore d'évaluation
- AbortionDocument16 pagesAbortionKim Lompot100% (1)
- CRVHD Percipitated by IEDocument14 pagesCRVHD Percipitated by IEKemotherapy LifesucksPas encore d'évaluation
- Pediatric No 1 Soap Notes 1Document5 pagesPediatric No 1 Soap Notes 1darrolddeleon1992Pas encore d'évaluation
- Pediatric SOAP Note 1Document7 pagesPediatric SOAP Note 1darrolddeleon1992Pas encore d'évaluation
- Case PresentationDocument15 pagesCase PresentationHarriette Quimby TibucPas encore d'évaluation
- CASE STUDY Lung Ca With Pleural EffDocument8 pagesCASE STUDY Lung Ca With Pleural EffL4 CLERK - UY, Rhea Andrea F.Pas encore d'évaluation
- SOAP NoteDocument8 pagesSOAP NoteAnonymous p0y5mmLQPas encore d'évaluation
- I. Vital InformationDocument9 pagesI. Vital InformationAlecPas encore d'évaluation
- 2 - 23 - 23 AM WardDocument10 pages2 - 23 - 23 AM WardkellogskrispiesPas encore d'évaluation
- Tehnik Penyusunan StatusDocument7 pagesTehnik Penyusunan StatusShelly Stephanie BintoroPas encore d'évaluation
- BPH Sample To Case ReportDocument12 pagesBPH Sample To Case ReportBirhanu ShiferawPas encore d'évaluation
- Case ReportDocument17 pagesCase ReportdenekePas encore d'évaluation
- Week 3 Case - DOBDocument3 pagesWeek 3 Case - DOBKirk Matthew ZhuPas encore d'évaluation
- Focused Thyroid ExamDocument6 pagesFocused Thyroid ExamyellowishmustardPas encore d'évaluation
- Exam 5Document1 pageExam 5BrianJakeDelRosarioPas encore d'évaluation
- Care Plan 5Document13 pagesCare Plan 5مالك مناصرةPas encore d'évaluation
- Antigua National SymbolsDocument4 pagesAntigua National SymbolsBlake Kammin100% (1)
- Tour Guide ApplicationDocument1 pageTour Guide ApplicationBlake KamminPas encore d'évaluation
- Christmas ListDocument5 pagesChristmas ListBlake KamminPas encore d'évaluation
- Rosie Carbon Lower Ottos ST Johns AntiguaDocument1 pageRosie Carbon Lower Ottos ST Johns AntiguaBlake KamminPas encore d'évaluation
- Charts October 2013Document2 pagesCharts October 2013Blake KamminPas encore d'évaluation
- E.D.P.M Homework Sylvani CharlesDocument2 pagesE.D.P.M Homework Sylvani CharlesBlake KamminPas encore d'évaluation
- Fluid & Electrolytes-Range ReferenceDocument4 pagesFluid & Electrolytes-Range ReferenceBlake KamminPas encore d'évaluation
- Pscyhology Handout - Social Learning TheoryDocument2 pagesPscyhology Handout - Social Learning TheoryBlake KamminPas encore d'évaluation
- Antigua National SymbolsDocument4 pagesAntigua National SymbolsBlake Kammin100% (1)
- Pscyhology Handout - Social Learning Theory Pg2Document2 pagesPscyhology Handout - Social Learning Theory Pg2Blake KamminPas encore d'évaluation
- Pscyhology Handout - Social Learning Theory Pg2Document2 pagesPscyhology Handout - Social Learning Theory Pg2Blake KamminPas encore d'évaluation
- The Bacteria: Dr. Linroy ChristianDocument16 pagesThe Bacteria: Dr. Linroy ChristianBlake KamminPas encore d'évaluation
- Antigua and BarbudaDocument2 pagesAntigua and BarbudaBlake KamminPas encore d'évaluation
- Fluid and ElectrolytesDocument8 pagesFluid and ElectrolytesWithlove AnjiPas encore d'évaluation
- Lecture 5 - Fungi and AlgaeDocument15 pagesLecture 5 - Fungi and AlgaeBlake KamminPas encore d'évaluation
- Introduction To Immunology: Dr. Linroy ChristianDocument24 pagesIntroduction To Immunology: Dr. Linroy ChristianBlake KamminPas encore d'évaluation
- Internal Host Defence: Dr. Linroy ChristianDocument17 pagesInternal Host Defence: Dr. Linroy ChristianBlake KamminPas encore d'évaluation
- Pathogenic Microorganisms: Dr. Linroy ChristianDocument19 pagesPathogenic Microorganisms: Dr. Linroy ChristianBlake KamminPas encore d'évaluation
- Lecture 9 - Spread of InfectionDocument22 pagesLecture 9 - Spread of InfectionBlake KamminPas encore d'évaluation
- Lecture 9 - Spread of InfectionDocument22 pagesLecture 9 - Spread of InfectionBlake KamminPas encore d'évaluation
- An Introduction To Viruses: Dr. Linroy ChristianDocument15 pagesAn Introduction To Viruses: Dr. Linroy ChristianBlake KamminPas encore d'évaluation
- Lecture 2 - Introduction To Microbiology PT 2Document18 pagesLecture 2 - Introduction To Microbiology PT 2Blake KamminPas encore d'évaluation
- Introduction To Microbiology: Dr. Linroy ChristianDocument21 pagesIntroduction To Microbiology: Dr. Linroy ChristianBlake KamminPas encore d'évaluation
- Important Nosocomial Infections: Dr. Linroy D. ChristianDocument17 pagesImportant Nosocomial Infections: Dr. Linroy D. ChristianBlake KamminPas encore d'évaluation
- Protozoa: Dr. Linroy ChristianDocument20 pagesProtozoa: Dr. Linroy ChristianBlake KamminPas encore d'évaluation
- PotterDocument2 pagesPotterBlake KamminPas encore d'évaluation
- Lease LetterDocument1 pageLease LetterBlake KamminPas encore d'évaluation
- Where Breathing BeginsDocument1 pageWhere Breathing BeginsBlake KamminPas encore d'évaluation
- I. Motor ResponseDocument2 pagesI. Motor ResponseBlake KamminPas encore d'évaluation
- PharmacologyDocument15 pagesPharmacologyBlake KamminPas encore d'évaluation