Académique Documents
Professionnel Documents
Culture Documents
Pathophysiology Acute Bacterial Meningitis
Transféré par
Nadira Farah PrayogoCopyright
Formats disponibles
Partager ce document
Partager ou intégrer le document
Avez-vous trouvé ce document utile ?
Ce contenu est-il inapproprié ?
Signaler ce documentDroits d'auteur :
Formats disponibles
Pathophysiology Acute Bacterial Meningitis
Transféré par
Nadira Farah PrayogoDroits d'auteur :
Formats disponibles
Nenny
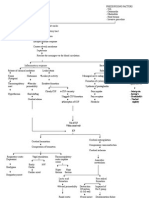
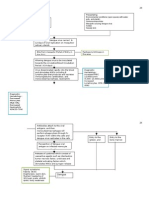
PATHOPHYSIOLOGY Acute Bacterial Meningitis
The most common bacteria that cause meningitis, S. pneumoniae and N. meningitidis, initially colonize the nasopharynx by attaching to nasopharyngeal epithelial cells. Bacteria are transported across epithelial cells in membrane-bound vacuoles to the intravascular space or invade the intravascular space by creating separations in the apical tight junctions of columnar epithelial cells. Once in the bloodstream, bacteria are able to avoid phagocytosis by neutrophils and classic complementmediated bactericidal activity because of the presence of a polysaccharide capsule. Bloodborne bacteria can reach the intraventricular choroid plexus, directly infect choroid plexus epithelial cells, and gain access to the CSF. Some bacteria, such as S. pneumoniae, can adhere to cerebral capillary endothelial cells and subsequently migrate through or between these cells to reach the CSF. Bacteria are able to multiply rapidly within CSF because of the absence of effective host immune defenses. Normal CSF contains few white blood cells (WBCs) and relatively small amounts of complement proteins and immunoglobulins. The paucity of the latter two prevents effective opsonization of bacteria, an essential prerequisite for bacterial phagocytosis by neutrophils. Phagocytosis of bacteria is further impaired by the fluid nature of CSF, which is less conducive to phagocytosis than a solid tissue substrate. A critical event in the pathogenesis of bacterial meningitis is the inflammatory reaction induced by the invading bacteria. Many of the neurologic manifestations and complications of bacterial meningitis result from the immune response to the invading pathogen rather than from direct bacteria-induced tissue injury. As a result, neurologic injury can progress even after the CSF has been sterilized by antibiotic therapy. The lysis of bacteria with the subsequent release of cellwall components into the subarachnoid space is the initial step in the induction of the inflammatory response and the formation of a purulent exudate in the subarachnoid space (Fig. 376-2). Bacterial cell-wall components, such as the lipopolysaccharide (LPS) molecules of gram-negative bacteria and teichoic acid and peptidoglycans of S. pneumoniae, induce meningeal inflammation by stimulating the production of inflammatory cytokines and chemokines by microglia, astrocytes, monocytes, microvascular endothelial cells, and CSF leukocytes. In experimental models of meningitis, cytokinesTNF and IL-1 are present in CSF within 12 h of intracisternal inoculation of LPS. This cytokine response is quickly followed by an increase in CSF protein concentration and leukocytosis. Chemokines (cytokines that induce chemotactic migration in leukocytes) and a variety of other proinflammatory cytokines are also produced and secreted by leukocytes and tissue cells that are stimulated by IL-1 and TNF. In addition, bacteremia and the inflammatory cytokines induce the production of excitatory amino acids, reactive oxygen and nitrogen species (free oxygen radicals, nitric oxide, and peroxynitrite), and other mediators that can induce death of brain cells.
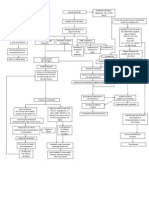
Nenny
Much of the pathophysiology of bacterial meningitis is a direct consequence of elevated levels of CSF cytokines and chemokines. TNF and IL-1 act synergistically to increase the permeability of the blood-brain barrier, resulting in induction of vasogenic edema and the leakage of serum proteins into the subarachnoid space (Fig. 376-2). The subarachnoid exudate of proteinaceous material and leukocytes obstructs the flow of CSF through the ventricular system and diminishes the resorptive capacity of the arachnoid granulations in the dural sinuses, leading to obstructive and communicating hydrocephalus and concomitant interstitial edema. Inflammatory cytokines upregulate the expression of selectins on cerebral capillary endothelial cells and leukocytes, promoting leukocyte adherence to vascular endothelial cells and subsequent migration into the CSF. The adherence of leukocytes to capillary endothelial cells increases the permeability of blood vessels, allowing for the leakage of plasma proteins into the CSF, which adds to the inflammatory exudate. Neutrophil degranulation results in the release of toxic metabolites that contribute to cytotoxic edema, cell injury, and death. During the very early stages of meningitis, there is an increase in cerebral blood flow, soon followed by a decrease in cerebral blood flow and a loss of cerebrovascular autoregulation. Narrowing of the large arteries at the base of the brain due to encroachment by the purulent exudate in the subarachnoid space and infiltration of the arterial wall by inflammatory cells with intimal thickening (vasculitis) also occur and may result in ischemia and infarction, obstruction of branches of the middle cerebral artery by thrombosis, thrombosis of the major cerebral venous sinuses, and thrombophlebitis of the cerebral cortical veins. The combination of interstitial, vasogenic, and cytotoxic edema leads to raised ICP and coma. Cerebral herniation usually results from the effects of cerebral edema, either focal or generalized; hydrocephalus and dural sinus or cortical vein thrombosis may also play a role.
Vous aimerez peut-être aussi
- Entity Level ControlsDocument45 pagesEntity Level ControlsNiraj AlltimePas encore d'évaluation
- TOGAF 9 Foundation Part 1 Exam Preparation GuideDocument114 pagesTOGAF 9 Foundation Part 1 Exam Preparation GuideRodrigo Maia100% (3)
- Etiology and Pathophysiology of MeningitisDocument2 pagesEtiology and Pathophysiology of MeningitisGlenn Asuncion Pagaduan50% (2)
- 1.pathophysiology of MeningitisDocument1 page1.pathophysiology of Meningitisshielamaygo05100% (1)
- Pathophysiology of DMDocument4 pagesPathophysiology of DMNicole Louise N. VillanuevaPas encore d'évaluation
- Qtsoi Concept MapDocument5 pagesQtsoi Concept MapGenella BabantoPas encore d'évaluation
- POTTs Disease PathoDocument3 pagesPOTTs Disease PathoEdgel QuidolesPas encore d'évaluation
- Pathophysiology of TuberculosisDocument2 pagesPathophysiology of TuberculosisLeikkaPas encore d'évaluation
- ASMOPS 2016 - International Invitation PHILIPPINEDocument4 pagesASMOPS 2016 - International Invitation PHILIPPINEMl Phil0% (3)
- Casting Procedures and Defects GuideDocument91 pagesCasting Procedures and Defects GuideJitender Reddy0% (1)
- Bacterial and Viral MeningitisDocument12 pagesBacterial and Viral Meningitisapi-3704562Pas encore d'évaluation
- Pathophysiology of MeningitisDocument4 pagesPathophysiology of MeningitisDaryl BalanguePas encore d'évaluation
- Pathophy - Nephrotic SyndromeedDocument1 pagePathophy - Nephrotic Syndromeedianecunar100% (1)
- Acute Lymphocytic LeukemiaDocument12 pagesAcute Lymphocytic Leukemiajustin_sanePas encore d'évaluation
- Pathology Polycystic Kidney DiseaseDocument4 pagesPathology Polycystic Kidney DiseaseOnyedika EgbujoPas encore d'évaluation
- Case Study PneumoniaDocument14 pagesCase Study PneumoniaJester GalayPas encore d'évaluation
- Rabies: A Deadly Viral Disease Spread by Animal BitesDocument3 pagesRabies: A Deadly Viral Disease Spread by Animal BitesDavid CalaloPas encore d'évaluation
- History: Symptoms Associated With Specific Viral InfectionsDocument12 pagesHistory: Symptoms Associated With Specific Viral InfectionsFatima Love Ariate-ArcasetasPas encore d'évaluation
- Typhoid FeverDocument1 pageTyphoid FeverMarkChesterSaguidNagen100% (1)
- Acute Glomerulonephritis: What is it and What Causes itDocument12 pagesAcute Glomerulonephritis: What is it and What Causes itSara Sonnya Ayutthaya NapitupuluPas encore d'évaluation
- PathophysiologyDocument5 pagesPathophysiologyJessyl GirayPas encore d'évaluation
- Cancer PathophysiologyDocument10 pagesCancer PathophysiologyGia Bautista-AmbasingPas encore d'évaluation
- Anatomy and Phsyiology of MeningococcemiaDocument2 pagesAnatomy and Phsyiology of MeningococcemiaKevin Comahig100% (1)
- Hiv AidsDocument14 pagesHiv Aidsapi-221532663Pas encore d'évaluation
- Pathophysiology of Bacterial MeningitisDocument2 pagesPathophysiology of Bacterial MeningitisEvangel PaduaPas encore d'évaluation
- The Pathophysiology of Peptic UlcerDocument15 pagesThe Pathophysiology of Peptic UlcerKike Meneses100% (1)
- Discharge PlanDocument1 pageDischarge PlanKamille Bianca Macapagal ÜPas encore d'évaluation
- Patho Congenital HypothyroidismDocument1 pagePatho Congenital HypothyroidismCzarm FarillasPas encore d'évaluation
- Bladder Cancer Types, Symptoms, Tests & TreatmentDocument1 pageBladder Cancer Types, Symptoms, Tests & TreatmentCarmina AguilarPas encore d'évaluation
- Personal Medical Records Document SummaryDocument16 pagesPersonal Medical Records Document SummaryJayselle FelipePas encore d'évaluation
- Pathophysiology of Meningococcal Meningitis and SepticaemiaDocument8 pagesPathophysiology of Meningococcal Meningitis and SepticaemiaEugen TarnovschiPas encore d'évaluation
- Pathophy of Appendicitis (Or) by Mizzy BaylonDocument2 pagesPathophy of Appendicitis (Or) by Mizzy BaylonmizzybaylonPas encore d'évaluation
- Case Study 102Document6 pagesCase Study 102Cheska Lopez100% (1)
- Pathophysiology of Nephrotic SyndromeDocument1 pagePathophysiology of Nephrotic SyndromeRan MaPas encore d'évaluation
- H MoleDocument2 pagesH MoleJoanna Marie Datahan EstomoPas encore d'évaluation
- PKD Pathophysiology: How Polycystic Kidney Disease Causes Renal and Extrarenal ComplicationsDocument2 pagesPKD Pathophysiology: How Polycystic Kidney Disease Causes Renal and Extrarenal Complicationsacey torrePas encore d'évaluation
- Pa Tho Physiology Part 1Document1 pagePa Tho Physiology Part 1anonymous89ify100% (2)
- Pathophysiology and Schematic Diagram of Typhoid FeverDocument3 pagesPathophysiology and Schematic Diagram of Typhoid FeverCyrus De AsisPas encore d'évaluation
- ChlamydiaDocument37 pagesChlamydiaElizabeth QuiñonesPas encore d'évaluation
- Leptospirosis FinalDocument5 pagesLeptospirosis FinalufriePas encore d'évaluation
- Brain AbscessDocument5 pagesBrain AbscessEugene Briagas Roque100% (1)
- Rabies: Ragina AguilaDocument55 pagesRabies: Ragina AguilaCharles Lester AdalimPas encore d'évaluation
- Case AnalysisDocument12 pagesCase AnalysisFroilan TaracatacPas encore d'évaluation
- Hyperglycemic Hyperosmolar State - A Diabetic EmergencyDocument2 pagesHyperglycemic Hyperosmolar State - A Diabetic EmergencyNiken AninditaPas encore d'évaluation
- Central Nervous System Infections: Gonzalo B. Roman JR.,MD.,FPSPDocument72 pagesCentral Nervous System Infections: Gonzalo B. Roman JR.,MD.,FPSPBenjamin PrabhuPas encore d'évaluation
- EncephalitisDocument20 pagesEncephalitisBenita Putri MDPas encore d'évaluation
- Management MastitisDocument6 pagesManagement MastitisReza Hardian NatsirPas encore d'évaluation
- Dengue PathophysioDocument4 pagesDengue PathophysioHonhon MacasaquitPas encore d'évaluation
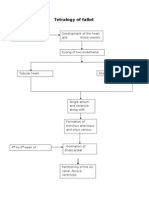
- Tetralogy of FallotDocument3 pagesTetralogy of FallotJohn Mark PocsidioPas encore d'évaluation
- Pathophysiology of DiarrheaDocument3 pagesPathophysiology of DiarrheaFathur RahmatPas encore d'évaluation
- PATHOPHYSIOLOGY Bacterial Meningitis 2Document2 pagesPATHOPHYSIOLOGY Bacterial Meningitis 2Luis Leh100% (2)
- HemorrhoidsDocument15 pagesHemorrhoidspologroPas encore d'évaluation
- Lupus Case ReportDocument1 pageLupus Case ReportMendy HararyPas encore d'évaluation
- Case Scenario Dengue FeverDocument2 pagesCase Scenario Dengue FeverJaslir MendozaPas encore d'évaluation
- Path o Physiology of SyphilisDocument1 pagePath o Physiology of Syphilis3S - JOCSON, DENESE NICOLE LEE M.Pas encore d'évaluation
- ChickenpoxDocument16 pagesChickenpoxJeet ThuraiPas encore d'évaluation
- Dengue FeverDocument8 pagesDengue Feverramoli1988Pas encore d'évaluation
- Hepatitis ADocument21 pagesHepatitis Avanessa100% (6)
- Pathophysiology of Amoebiasis: Ingestion to ExcretionDocument1 pagePathophysiology of Amoebiasis: Ingestion to ExcretionCathy AcquiatanPas encore d'évaluation
- Community Acquired Pneumonia, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsD'EverandCommunity Acquired Pneumonia, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsPas encore d'évaluation
- PATHOGENESIS MeningitisDocument3 pagesPATHOGENESIS MeningitisfebrichandraPas encore d'évaluation
- Patogenesis Infeksi Bakteri, Infeksi Lokal, Dan SepsisDocument52 pagesPatogenesis Infeksi Bakteri, Infeksi Lokal, Dan SepsisNia AnestyaPas encore d'évaluation
- Inflammation Seminar OverviewDocument19 pagesInflammation Seminar OverviewDrGurinder Kanwar100% (1)
- Oninla 2014Document7 pagesOninla 2014Nadira Farah PrayogoPas encore d'évaluation
- Polip NasalDocument5 pagesPolip NasalNadira Farah PrayogoPas encore d'évaluation
- Nasal Polyps: Causes, Symptoms, and TreatmentDocument19 pagesNasal Polyps: Causes, Symptoms, and TreatmentAnnisaa FitrianiPas encore d'évaluation
- Bahan PresKasDocument13 pagesBahan PresKasNadira Farah PrayogoPas encore d'évaluation
- Daftar PertanyaanDocument1 pageDaftar PertanyaanNadira Farah PrayogoPas encore d'évaluation
- Bahan PresKasDocument13 pagesBahan PresKasNadira Farah PrayogoPas encore d'évaluation
- Gene Expression in Breast Carcinomas: Pathogenesis (Hormone Sensitive)Document3 pagesGene Expression in Breast Carcinomas: Pathogenesis (Hormone Sensitive)Nadira Farah PrayogoPas encore d'évaluation
- Daftar PertanyaanDocument1 pageDaftar PertanyaanNadira Farah PrayogoPas encore d'évaluation
- CAD AjasjhfiueghrfDocument3 pagesCAD AjasjhfiueghrfNadira Farah PrayogoPas encore d'évaluation
- EsheiuhDocument23 pagesEsheiuhNadira Farah PrayogoPas encore d'évaluation
- Definition, Epidemiology, & Etiology-RenataDocument2 pagesDefinition, Epidemiology, & Etiology-RenataNadira Farah PrayogoPas encore d'évaluation
- Treatment & Prognosis of MeningitisDocument1 pageTreatment & Prognosis of MeningitisNadira Farah PrayogoPas encore d'évaluation
- Data AlumniDocument2 pagesData AlumniNadira Farah PrayogoPas encore d'évaluation
- Treatment & Prognosis of MeningitisDocument1 pageTreatment & Prognosis of MeningitisNadira Farah PrayogoPas encore d'évaluation
- Guardian March2013Document26 pagesGuardian March2013Nadira Farah PrayogoPas encore d'évaluation
- Guardian WS 18 24mar2013Document2 pagesGuardian WS 18 24mar2013Nadira Farah PrayogoPas encore d'évaluation
- Explaining GenogramsDocument4 pagesExplaining GenogramsNadira Farah Prayogo100% (5)
- Guias JNC 8Document15 pagesGuias JNC 8María Jennifer Serrano BPas encore d'évaluation
- Explaining GenogramsDocument4 pagesExplaining GenogramsNadira Farah Prayogo100% (5)
- Diabetes Knowledge TestDocument1 pageDiabetes Knowledge TestNadira Farah PrayogoPas encore d'évaluation
- Reversal of Type 2 Diabetes Normalisation of Beta Cell Function in Association With Decreased Pancreas and Liver TriacylglycerolDocument9 pagesReversal of Type 2 Diabetes Normalisation of Beta Cell Function in Association With Decreased Pancreas and Liver Triacylglycerolsitnuciana_123Pas encore d'évaluation
- Adherence CompilationDocument2 pagesAdherence CompilationNadira Farah PrayogoPas encore d'évaluation
- Morisky ScaleDocument1 pageMorisky ScaleAnisaVitrianaPas encore d'évaluation
- Morisky Scale (Not Modified/ The New One)Document1 pageMorisky Scale (Not Modified/ The New One)Nadira Farah PrayogoPas encore d'évaluation
- Who DMG PDFDocument65 pagesWho DMG PDFShelly Silvia BintangPas encore d'évaluation
- Iso 9001 CRMDocument6 pagesIso 9001 CRMleovencePas encore d'évaluation
- Final Thesis Report YacobDocument114 pagesFinal Thesis Report YacobAddis GetahunPas encore d'évaluation
- Merchandising Calender: By: Harsha Siddham Sanghamitra Kalita Sayantani SahaDocument29 pagesMerchandising Calender: By: Harsha Siddham Sanghamitra Kalita Sayantani SahaSanghamitra KalitaPas encore d'évaluation
- Unit 1 - Gear Manufacturing ProcessDocument54 pagesUnit 1 - Gear Manufacturing ProcessAkash DivatePas encore d'évaluation
- Rohit Patil Black BookDocument19 pagesRohit Patil Black BookNaresh KhutikarPas encore d'évaluation
- IoT BASED HEALTH MONITORING SYSTEMDocument18 pagesIoT BASED HEALTH MONITORING SYSTEMArunkumar Kuti100% (2)
- SEG Newsletter 65 2006 AprilDocument48 pagesSEG Newsletter 65 2006 AprilMilton Agustin GonzagaPas encore d'évaluation
- Ir35 For Freelancers by YunojunoDocument17 pagesIr35 For Freelancers by YunojunoOlaf RazzoliPas encore d'évaluation
- Fernandez ArmestoDocument10 pagesFernandez Armestosrodriguezlorenzo3288Pas encore d'évaluation
- SD8B 3 Part3Document159 pagesSD8B 3 Part3dan1_sbPas encore d'évaluation
- Chem 102 Week 5Document65 pagesChem 102 Week 5CAILA CACHEROPas encore d'évaluation
- FSRH Ukmec Summary September 2019Document11 pagesFSRH Ukmec Summary September 2019Kiran JayaprakashPas encore d'évaluation
- BPL Millipacs 2mm Hardmetrics RarDocument3 pagesBPL Millipacs 2mm Hardmetrics RarGunter BragaPas encore d'évaluation
- Three-D Failure Criteria Based on Hoek-BrownDocument5 pagesThree-D Failure Criteria Based on Hoek-BrownLuis Alonso SAPas encore d'évaluation
- 2010 - Impact of Open Spaces On Health & WellbeingDocument24 pages2010 - Impact of Open Spaces On Health & WellbeingmonsPas encore d'évaluation
- ServiceDocument47 pagesServiceMarko KoširPas encore d'évaluation
- Service and Maintenance Manual: Models 600A 600AJDocument342 pagesService and Maintenance Manual: Models 600A 600AJHari Hara SuthanPas encore d'évaluation
- NewspaperDocument11 pagesNewspaperКристина ОрёлPas encore d'évaluation
- To Introduce BgjgjgmyselfDocument2 pagesTo Introduce Bgjgjgmyselflikith333Pas encore d'évaluation
- 3ccc PDFDocument20 pages3ccc PDFKaka KunPas encore d'évaluation
- 50 Years of Teaching PianoDocument122 pages50 Years of Teaching PianoMyklan100% (35)
- Mercedes BenzDocument56 pagesMercedes BenzRoland Joldis100% (1)
- PRODUCTDocument82 pagesPRODUCTSrishti AggarwalPas encore d'évaluation
- Cold Rolled Steel Sections - Specification: Kenya StandardDocument21 pagesCold Rolled Steel Sections - Specification: Kenya StandardPEng. Tech. Alvince KoreroPas encore d'évaluation
- Accomplishment Report 2021-2022Document45 pagesAccomplishment Report 2021-2022Emmanuel Ivan GarganeraPas encore d'évaluation
- Oracle Learning ManagementDocument168 pagesOracle Learning ManagementAbhishek Singh TomarPas encore d'évaluation