Académique Documents
Professionnel Documents
Culture Documents
Respiratory System
Transféré par
Enggrajati Moses SilitongaCopyright
Formats disponibles
Partager ce document
Partager ou intégrer le document
Avez-vous trouvé ce document utile ?
Ce contenu est-il inapproprié ?
Signaler ce documentDroits d'auteur :
Formats disponibles
Respiratory System
Transféré par
Enggrajati Moses SilitongaDroits d'auteur :
Formats disponibles
Shier, Butler, and Lewis: Holes Human Anatomy and Physiology, 10th ed.
Chapter 19: Respiratory System
Chapter 19: Respiratory System I. Introduction A. The respiratory system consists of passages that filter incoming air and transport it to the body, into the lungs, and to the many microscopic air sacs where gases are exchanged. B. Respiration is the entire process o exchanging gases between the atmosphere and body cells. C. Respiration consists of ventilation, external respiration, transport of gases be the blood between lungs and body cells, internal respiration, and cellular respiration. D. Ventilation is the movement of air in and out of the lungs. E. External respiration is the exchange of gases between the air in the lungs and the blood F. Internal respiration is the exchange of gases between the blood and the body cells. G. Cellular respiration is oxygen utilization and production of carbon dioxide in body cells. II. Why We Breathe A. Respiration enables cells to harness the energy held in chemical bonds of nutrient molecules. B. Without oxygen as a final electron acceptor, much energy remains locked in nutrients. C. A metabolic waste of respiration is carbon dioxide. D. Carbon dioxide, when it reacts with water, forms carbonic acid which contributes to the pH of blood. E. Too much carbon dioxide will lower blood pH. F. Cellular respiration and control of blood pH explain why we must obtain oxygen and get rid of carbon dioxide.
III. Organs of the Respiratory System A. Introduction 1. The upper respiratory tract includes nose, nasal cavity, sinuses, and pharynx. 2. The lower respiratory tract includes larynx, trachea, bronchial tree, and lungs. B. Nose 1. The nose is supported internally by muscle, bone, and cartilage. 2. Nostrils are openings through which air can enter and leave the nasal cavity. 3. Internal hairs of nostrils prevent entry of large particles carried in air. C. Nasal Cavity 1. The nasal cavity is a hollow space behind the nose. 2. The nasal septum is a structure that divides the nasal cavity into left and right halves. 3. The nasal cavity is separated from the cranial cavity by the cribiform plate of the ethmoid bone and from the oral cavity by by the hard palate. 4. Nasal conchae are located on the lateral walls of the nasal cavity and divide the nasal cavity into superior, inferior, and middle meatuses. 5. Nasal conchae function to support the mucous membranes that line the nasal cavity and to increase the surface area of the nasal cavity. 6. The lining of the upper portion of the nasal cavity contains olfactory receptors. 7. Most of the nasal cavity conducts air to and from the nasopharynx. 8. The mucous membrane lining the nasal cavity contains pseudostratified ciliated epithelium that is rich in mucous-secreting goblet cells. 9. The functions of the mucous membrane of the nasal cavity are to warm the air, to moisten the air, and to trap small particles entering the nasal cavity. 10. Cilia of the nasal cavity function to move mucous and any entrapped particles toward the pharynx.
D. Sinuses 1. Sinuses are air-filled spaces located within skull bones. 2. Bones that contain sinuses are maxillae, frontal, ethmoid, and sphenoid. 3. The functions of sinuses are to reduce the weight of the skull and to serve as resonant chambers that affect the quality of the voice. E. Pharynx 1. The pharynx is located posterior to the oral cavity and between the nasal cavity and the larynx. 2. Functions of the pharynx are to move food into the esophagus, to move air into the larynx, and to aid in the production of sound. F. Larynx 1. The larynx is an enlargement in the airway superior to the trachea and inferior to the pharynx. 2. The functions of the larynx are to move air into the trachea, prevent foreign objects from entering the trachea, and to house vocal cords. 3. The larynx is composed of a framework of muscles and cartilages bound by elastic tissue. 4. The cartilages of the larynx are thyroid, cricoid, and epiglottic. 5. The thyroid cartilage is located just superior to the thyroid gland. 6. The cricoid cartilage is located inferior to the thyroid cartilage. 7. The epiglottic cartilage is located attached to the upper border of the thyroid cartilage. 8. The epiglottis is flaplike structure supported by the epiglottic cartilage. 9. The functions of the epiglottis are to prevent foods and liquids from entering the air passages and to allow air to pass into the trachea. 10. The arytenoid cartilages are located superior to and on either side of the cricoid cartilage. 11. The corniculate cartilages are located attached to the tips of the arytenoid cartilages.
12. The arytenoids and corniculate cartilages are attachments sites for muscles that help regulate tension on the vocal cords during speech and aid in closing the larynx during swallowing. 13. The cuneiform cartilages are located between the epiglottic and arytenoid cartilages and function to stiffen soft tissue in this region. 14. False vocal cords are located inside the larynx and are composed of muscle tissue and connective tissue with a covering of mucous membrane. 15. The function of the false vocal cords is to help close the larynx during swallowing. 16. The true vocal cords are located inferior to the false vocal cords and are composed of elastic fibers. 17. The functions of the true vocal cords are to produce sounds of speech. 18. A higher pitch of the voice is produced by increasing tension on true vocal cords and a lower pitch is produced by decreasing the tension on the cords. 19. The loudness of a vocal sound depends on upon the force of air passing over the vocal cords. 20. The glottis is the opening between vocal cords. 21. The mucous membrane that lines the larynx continues to filter incoming air by entrapping particles and moving them toward the pharynx by ciliary action. G. Trachea 1. The trachea is a flexible cylindrical tube and is located anterior to the esophagus in the thoracic cavity. 2. The trachea splits into right and left bronchi. 3. The inner wall of the trachea is lined with a ciliated mucous membrane that contains many goblet cells. 4. The mucous membrane of the trachea functions to filter incoming air and to move entrapped particles upward into the pharynx where the mucous can be swallowed.
5. The wall of the trachea is composed of C shaped pieces of hyaline cartilage, smooth muscle, and connective tissues. 6. The cartilaginous rings of the trachea prevent the trachea from collapsing and blocking the airway. 7. The soft tissues that complete the rings in the back of the trachea allow the esophagus to expand as food moves through it on the way to the stomach. 8. A blocked trachea causes asphyxiation. 9. A tracheostomy is the production of a temporary hole in the trachea. H. Bronchial Tree 1. Introduction a. The bronchial tree consists of branched airways leading from the trachea to the microscopic air sacs in the lungs. b. Primary bronchi are the first branches of the trachea. c. The carina is ridge of cartilage that separates the primary bronchi. d. Each bronchus, accompanied by blood vessels and nerves, enters its respective lung. 2. Branches of the Bronchial Tree a. Primary bronchi branch into secondary bronchi. b. Secondary bronchi branch into tertiary bronchi. c. Tertiary bronchi branch into intralobular bronchioles. d. A bronchopulmonary segment is a portion of a lung supported by a tertiary segment. e. Intralobular bronchioles branch into terminal bronchioles. f. Terminal bronchioles branch into respiratory bronchioles. g. Respiratory bronchioles branch into alveolar ducts. h. Alveolar ducts give rise to alveolar sacs. i. Alveolar sacs are thin-walled, closely packed outpouchings of the alveolar ducts.
j. Alveoli are thin-walled, microscopic air sacs that open to an alveolar sac. 3. Structure of the Respiratory Tubes a. The structure of a bronchus is similar to that of the trachea except the C shaped cartilaginous rings are replaced with cartilaginous plates where the bronchus enters the lung. b. Finer branches of the respiratory tree have decreased amounts of cartilage and increased amounts of smooth muscle. c. Elastic fibers are scattered throughout the lungs. d. Other changes in the tubes of the respiratory tree as they get smaller are the changes in cells types that line the airways. 4. Functions of the Respiratory Tubes and Alveoli a. The branches of the bronchial tree function to filter incoming air and distribute it to the alveoli in all parts of the lungs. b. The alveoli function to provide a large surface area of thin epithelial cells through which gas exchanges can occur. I. Lungs 1. The lungs are cone shaped and located the thoracic cavity. 2. The right and left lungs are separated by the heart and the mediastinum and enclosed by the diaphragm and thoracic cage. 3. The hilus of the lung is an indention on the medial surface of a lung. 4. Visceral pleura are serous membranes attached to the surfaces of the lungs. 5. Parietal pleura is a serous membrane that lines the thoracic cavity. 6. The pleural cavity is the potential space between the visceral pleura and parietal pleura. 7. The functions of serous fluid in the pleural cavity are to lubricate serous membranes and reduce friction during lung movements. 8. The lobes of the right lung are superior, middle, and inferior. 9. The lobes of the left lung are superior and inferior. 10. Lobules of the lungs are divisions of lung lobes.
IV. Breathing Mechanism A. Introduction 1. Breathing or ventilation is the movement of air from outside the body into the bronchial tree and alveoli, followed by a reversal of this air movement. 2. Inspiration is inhalation. 3. Expiration is exhalation. B. Inspiration 1. The force that moves air into the lungs is atmospheric pressure. 2. If the pressure inside the lungs and alveoli decreases, outside air will flow into the airways. 3. The diaphragm is located just inferior to the lungs and is composed of skeletal muscle. 4. The nerves that stimulate the diaphragm are the phrenic nerves. 5. When the diaphragm contracts it moves inferiorly and the thoracic cavity enlarges. 6. When the thoracic cavity enlarges, the intra-alveolar pressure decreases. 7. When intra-alveolar pressure falls, air is moved into the airways. 8. The action of external intercostals muscles is to raise the ribs and elevates the sternum, which increases the size of the thoracic cavity. 9. When intercostals muscles move the thoracic wall upward and outward, the parietal pleura and visceral pleura move. 10. Movement of the parietal and visceral pleura upward and outward expands the lungs in all directions. 11. Surface tension is the attraction certain molecule to each other. 12. Surfactant is located in alveolar spaces and functions to reduce the alveolis tendency to collapse. 13. If a person needs to take a deeper than normal breath, the diaphragm and external intercostals muscles may contract to a greater extent.
14. Other muscles that can be used to enlarge the thoracic cavity are the pectoralis minors and sternocleidomastoids. 15. Compliance is the ease at which the lungs can expand as a result of pressure changes occurring during breathing. 16. In a normal lung, compliance decreases as lung volume increases because an inflated lung is more difficult to expand that a lung at rest. 17. Factors that lead to a decrease in lung compliance are conditions that obstruct air passages, destroy lunlung tissue, or impede lung expansion in other ways. C. Expiration 1. The forces responsible for normal expiration come from elactic recoil of lung tissues and from surface tension. 2. As the diaphragm and external intercostals muscles relax, the elastic tissues cause the lungs to recoil. 3. Air is forced out of respiratory passageways because intra-alveolar pressure rises above atmospheric pressure. 4. Muscles that aid in a more forceful exhalation than normal are internal intercostal muscles and abdominal wall muscles. D. Respiratory Volumes and Capacities 1. Spirometry is the measure of air volumes. 2. A respiratory cycle is one inspiration plus the following expiration. 3. Tidal volume is the amount of air that enters of leaves during a respiratory cycle. 4. Inspiratory reserve volume is the additional quantity of air after the resting tidal volume that can enter the lungs. 5. Expiratory reserve volume is the additional quantity of air that can exit the lungs after a resting tidal volume. 6. Residual volume is the amount of air that remains in the lungs after a forceful expiration. 7. Vital capacity is maximum amount of air that can be exhaled after taking the deepest breath possible.
8. Inspiratory capacity is maximum volume of air that can be inhaled following exhalation of tidal volume. 9. Functional residual capacity is volume of air that remains in the lungs following exhalation of tidal volume. 10. Total lung capacity is total volume of air that the lungs can hold. 11. Anatomic dead space is the space in airways. 12. Alveolar dead space is space in alveoli that do not carry out gas exchange due to poor blood flow. 13. Physiologic dead space is anatomical dead space plus alveolar dead space. 14. A spirometer measures respiratory air volumes. 15. Respiratory volumes and capacities are used to evaluate the course of respiratory illnesses. E. Alveolar Ventilation 1. Minute ventilation is the amount of new atmospheric air that is moved into the respiratory passages each minute and equals the tidal volume multiplied by the breathing rate. 2. The volume of air that reaches alveoli is calculated by subtracting the physiologic dead space from the tidal volume. 3. Alveolar ventilation rate is the volume of air that reaches alveoli multiplied by breathing rate and is a major factor affecting the concentrations of oxygen and carbon dioxide in alveoli. F. Nonrespiratory Air Movements 1. Nonrespiratory air movements are air movements that occur in addition to breathing. 2. Examples of nonrespiratory air movements are coughing, sneezing, crying and laughing. 3. Nonrespiratory air movements usually result from reflexes. 4. Coughing involves take a deep breath, closing the glottis, and forcing air upward from the lungs against the closure. Then the glottis is suddenly
opened, and a blast of air is forced upward from the lower respiratory tract. 5. The function of a sneeze is to clear the upper respiratory passages. 6. Laughing involves taking a deep breath and releasing it in a series of short expirations. 7. A hiccup is caused by sudden inspiration due to a spasmodic contraction of the diaphragm while the glottis is closed. 8. The function of a yawn is to aid respiration by providing an occasional deep breath. V. Control of Breathing A. Respiratory Center 1. The respiratory center is composed of groups of neurons in the brainstem which controls breathing. 2. The functions of the respiratory center are to cause inhalation and exhalation, and to adjust the rate and depth of breathing. 3. The components for the respiratory center are located widely scattered throughout the pons and medulla oblongata. 4. The medullary rhythmicity area includes two groups of neurons that extend throughout the length of the medulla oblongata. 5. The dorsal respiratory group is responsible for the basic rhythm of breathing. 6. The functions of the ventral respiratory center are to generate impulses for more forceful breathing movements. 7. The functions of the pneumotaxic area are to regulate the duration of inspiratory bursts originating from the dorsal group. This area basically controls the rate of breathing. B. Factors Affecting Breathing 1. Partial pressure of a gas is amount of pressure each gas contributes. 2. High concentrations of carbon dioxide in blood are detected by central chemoreceptors.
3. In response to high carbon dioxide levels, the respiratory center triggers an increase in alveolar ventilation, which decreases carbon dioxide levels and hydrogen ions levels in blood. 4. High concentrations of hydrogen ions in blood or cerebrospinal fluid are detected by central chemoreceptors. 5. In response to high hydrogen ion levels, the respiratory center triggers an increase in alveolar ventilation, which decreases hydrogen ions in blood. 6. Low concentrations of oxygen in blood are detected by peripheral chemoreceptors. 7. When blood levels of oxygen are low, ventilation increases and the concentration of oxygen in blood increases. 8. The inflation reflex helps regulate the depth of breathing. 9. The inflation reflex occurs when stretch receptors in the visceral pleura, bronchioles, and alveoli are stimulated as lung tissues are stretched. 10. The inflation reflex prevents overinflation of the lungs. 11. Hyperventilation is rapid and deep breathing and it lowers the blood concentration of carbon dioxide. VII. Alveolar Gas Exchanges A. Alveoli 1. Alveoli are microscopic air sacs clustered at the distal ends of the finest respiratory tubes. 2. An alveolus consists of a tiny space surrounded by a thin wall that separates it from adjacent alveoli. 3. Alveolar pores are tiny openings in the walls of some alveoli. 4. Alveolar macrophages are phagocytic cells and function to destroy airborne agents that reach alveoli. B. Respiratory Membrane 1. The respiratory membrane is composed of two layers of epithelial cells and two basement membranes.
2. The respiratory membrane is the site of gas exchange between alveolar air and the blood. C. Diffusion Through the Respiratory Membrane 1. Molecules diffuse from regions where they are in higher concentration toward regions where they are in lower concentration. 2. Carbon dioxide diffuses from blood in pulmonary capillaries to alveolar air because the partial pressure of carbon dioxide is higher in the blood of pulmonary capillaries than in alveolar air. 3. Oxygen diffuses from alveolar air to blood in pulmonary capillaries because the partial pressure of oxygen is higher in alveolar air than in the blood of pulmonary capillaries. 4. Factors that affect diffusion across the respiratory membrane are surface area, distance, solubility of gases, partial pressure gradients, and diseases. 5. Diseases that harm respiratory membranes are pneumonia and emphysema. 6. Breath analysis can detect alcohol in the blood because the respiratory membrane is so thin that alcohol can diffuse into alveolar air and be exhaled. VIII. Gas Transport A. Introduction 1. The blood transports oxygen and carbon dioxide between the lungs and the body cells. 2. As oxygen and carbon dioxide enter blood, they dissolve in plasma or combine chemically with other atoms or molecules. B. Oxygen Transport 1. Almost all the oxygen carried in blood is bound to hemoglobin. 2. A small amount of oxygen is carried in blood dissolved in plasma. 3. Hemoglobin consists of two types of components called heme and globin. 4. Each heme group contains an atom of iron.
5. Oxyhemoglobin is the combination of oxygen and hemoglobin. 6. Deoxyhemoglobin is hemoglobin that is not carrying oxygen. 7. Factors that promote the release of oxygen from hemoglobin are a decrease in the partial pressure of oxygen, increasing blood concentrations of carbon dioxide, acidity, and increased temperatures. C. Carbon Dioxide Transport 1. Blood flowing through capillaries gain carbon dioxide because the tissues have a high partial pressure of carbon dioxide. 2. Carbon dioxide is transported to lungs in one of the following three forms: bound to hemoglobin, dissolved in plasma, or as bicarbonate ions. 3. Carbaminohemoglobin is the combination of carbon dioxide and hemoglobin. 4. Hemoglobin can carry oxygen and carbon dioxide at the same time because they bind at different sites on hemoglobin. 5. The most important carbon dioxide transport mechanism involves the formation of bicarbonate ions. 6. Carbon dioxide forms carbonic acid when it reacts with water. 7. Carbonic anhydrase is an enzyme that speeds up the reaction between carbon dioxide and water and is located inside red blood cells. 8. Carbonic acid dissociates into hydrogen ions and bicarbonate ions. 9. The chloride shift is the exchange of chloride ions and bicarbonate ions across the red blood cell membrane and functions to maintain the ionic balance between the red blood cells and the plasma. 10. When blood reaches the pulmonary capillaries, hydrogen ions and bicarbonate ions recombine to form carbonic acid. 11. In the pulmonary capillaries, carbonic acid becomes carbon dioxide and water. 12. In the lungs, carbon dioxide diffuses out of the blood until equilibrium is established between the partial pressure of carbon dioxide of the blood and that of the alveolar air. IX. Life-Span Changes
A. Changes in the respiratory system over a lifetime reflect both the accumulation of environmental influences and the effects of aging in other organ systems. B. People who have been exposed to foul air are more likely to develop chronic bronchitis, emphysema, or lung cancer. C. The factors the change the ability of the respiratory system to clear pathogens from the lungs are a decreases in activity of cilia, thickening of mucus, and the slowing of swallowing, gagging and coughing reflexes. D. Factors that contribute to an overall increase in effort required to breathe are calcification of cartilage between the sternum and ribs and changes in skeletal structure of the thoracic cavity. E. The microscopic changes that occur in the lungs are expansion of alveolar walls, an increase in the amount of collagen, and a decreased amount of elastin.
Vous aimerez peut-être aussi
- Repiratory System Hand OutDocument3 pagesRepiratory System Hand OutAlyana AbrantesPas encore d'évaluation
- Respiratory SystemDocument19 pagesRespiratory SystemSri Ganesh ComputersPas encore d'évaluation
- Respiratory System A. BDocument5 pagesRespiratory System A. BPhoebe Kates Dela CruzPas encore d'évaluation
- Respiratory System: Ventilation Cellular RespirationDocument4 pagesRespiratory System: Ventilation Cellular RespirationSoleil MaxwellPas encore d'évaluation
- Dulutalias - Chapter23-THE RESPIRATORY SYSTEMDocument15 pagesDulutalias - Chapter23-THE RESPIRATORY SYSTEMKie MusstisquePas encore d'évaluation
- Unit 7: Respiratory System (2 Hours Lecture/3 Hours Lab) : at The End of This Unit, Students Will Be Able ToDocument4 pagesUnit 7: Respiratory System (2 Hours Lecture/3 Hours Lab) : at The End of This Unit, Students Will Be Able ToRUSSEL AQUINOPas encore d'évaluation
- Respiratory SystemDocument87 pagesRespiratory Systemd...Pas encore d'évaluation
- Respiratory ReviewerDocument8 pagesRespiratory ReviewerBLAIRY ZYPas encore d'évaluation
- D77be476 C1ec 4034 A6e7 305113d3044dphysiology of RespirationDocument9 pagesD77be476 C1ec 4034 A6e7 305113d3044dphysiology of RespirationMalti SharmaPas encore d'évaluation
- Respiratory System NotesDocument5 pagesRespiratory System NotesBrandice BradleyPas encore d'évaluation
- CHAPTER 22 The Respiratory SystemDocument11 pagesCHAPTER 22 The Respiratory System楊畯凱Pas encore d'évaluation
- Respiratory SystemDocument12 pagesRespiratory SystemshreyacrkPas encore d'évaluation
- Human Respiratory SystemDocument16 pagesHuman Respiratory SystemJohn marcus ViadoPas encore d'évaluation
- Human Anatomy Reading ComprehensionDocument16 pagesHuman Anatomy Reading ComprehensionRhams BairullaPas encore d'évaluation
- Our Lungs Are The Organs That Bring in Oxygen Into Our BodyDocument17 pagesOur Lungs Are The Organs That Bring in Oxygen Into Our BodySaidatul Atyah Mohd ApendaiPas encore d'évaluation
- Anatomy of The Respiratory System 1Document8 pagesAnatomy of The Respiratory System 1Grace Noviyanthi SinambelaPas encore d'évaluation
- Anatomy of The Respiratory SystemDocument37 pagesAnatomy of The Respiratory SystemPal SedPas encore d'évaluation
- Lab Module Activity Respiratory SystemDocument8 pagesLab Module Activity Respiratory SystemJecel LazarraPas encore d'évaluation
- Respiratory System: Student Learning OutcomesDocument9 pagesRespiratory System: Student Learning Outcomeslily1liang-1Pas encore d'évaluation
- Respiratory System Anatomy and PhysiologyDocument19 pagesRespiratory System Anatomy and PhysiologyKBDPas encore d'évaluation
- Airway Mngt. Module 1.Document11 pagesAirway Mngt. Module 1.marc gorospePas encore d'évaluation
- The Respiratory SystemDocument8 pagesThe Respiratory SystemDavid DanielPas encore d'évaluation
- Group2 (Respiration)Document12 pagesGroup2 (Respiration)dinaPas encore d'évaluation
- Chapter 22 Notes Respiratory SystemDocument36 pagesChapter 22 Notes Respiratory SystemMarilia BonorinoPas encore d'évaluation
- The Respiratory SystemDocument16 pagesThe Respiratory SystemAirene Mae Lamputi SupilarPas encore d'évaluation
- Supplementary Material 3.1 Basic Concepts and Assessment (N) - 2Document13 pagesSupplementary Material 3.1 Basic Concepts and Assessment (N) - 2Kent Borro CantomayorPas encore d'évaluation
- LP 1 - OksigenasiDocument22 pagesLP 1 - OksigenasiWini SarahPas encore d'évaluation
- Chapter 8-1Document12 pagesChapter 8-1Syafrianda PanggabeanPas encore d'évaluation
- Respiratory SystemDocument3 pagesRespiratory Systemๆรำำทแร หบหฝำมฟPas encore d'évaluation
- Experiment No. Aim: To Study The Human Respiratory System. RequirementsDocument6 pagesExperiment No. Aim: To Study The Human Respiratory System. RequirementsRohan Saste100% (1)
- Module 4 Respiratory SystemDocument8 pagesModule 4 Respiratory SystemJake Donely C. PaduaPas encore d'évaluation
- Bilology XII 2014 CH - 14 RespirationDocument16 pagesBilology XII 2014 CH - 14 RespirationMuhammad UsmanPas encore d'évaluation
- The Human Respiratory SystemDocument15 pagesThe Human Respiratory SystemNandita Halder100% (1)
- Notes 1Document12 pagesNotes 1Muhammad TaimoorPas encore d'évaluation
- Respiratory System-Chapter 17Document7 pagesRespiratory System-Chapter 17Yza S.Pas encore d'évaluation
- ANAPHYDocument10 pagesANAPHYcharles babasaPas encore d'évaluation
- What Are The Parts of Respiratory System With FunctionsDocument3 pagesWhat Are The Parts of Respiratory System With FunctionsMelx UbaldePas encore d'évaluation
- The Cells of The Human Body Require A Constant Stream of Oxygen To Stay AliveDocument14 pagesThe Cells of The Human Body Require A Constant Stream of Oxygen To Stay AlivePeperoniiPas encore d'évaluation
- Respiratory System PreDocument11 pagesRespiratory System PrecontehamosaPas encore d'évaluation
- Lab 6Document9 pagesLab 6InactiveAccountPas encore d'évaluation
- NAMA: Intan Fajria NIM: 1707201077 Semester: Vi/C Task One To Explore Initial Knowledge About The Material To Be Discussed, First ExamineDocument3 pagesNAMA: Intan Fajria NIM: 1707201077 Semester: Vi/C Task One To Explore Initial Knowledge About The Material To Be Discussed, First ExamineintanPas encore d'évaluation
- Anatony Lung PartsDocument23 pagesAnatony Lung PartsNejib ReshadPas encore d'évaluation
- Respiratory System - Anatomy and PhysiologyDocument6 pagesRespiratory System - Anatomy and PhysiologyJay Crishnan Morales CajandingPas encore d'évaluation
- Materi BingDocument17 pagesMateri BingCindy Ari SantiPas encore d'évaluation
- RespiratoryDocument20 pagesRespiratoryBon BonselPas encore d'évaluation
- Anatomy and Physiology of The Respiratory SystemDocument3 pagesAnatomy and Physiology of The Respiratory SystemLyka100% (1)
- Mark Dave Villasencio & Hope DuranoDocument11 pagesMark Dave Villasencio & Hope DuranoMark Dave VillasencioPas encore d'évaluation
- Respiratory System s2 2019Document56 pagesRespiratory System s2 2019noviantyramadhani12Pas encore d'évaluation
- Respiratory System: Reported By: C.M. HerreraDocument19 pagesRespiratory System: Reported By: C.M. HerreraTsume ShoutaroPas encore d'évaluation
- Core Concepts in Anatomy and PhysiologyDocument50 pagesCore Concepts in Anatomy and PhysiologyMohamed Abdullah KhojaliPas encore d'évaluation
- 05 Respiratory SystemDocument117 pages05 Respiratory SystemcelynjasminegPas encore d'évaluation
- Body SystemDocument15 pagesBody SystemChris Timothy TurdanesPas encore d'évaluation
- Anatomi Saluran PernapasanDocument6 pagesAnatomi Saluran PernapasanfidyaPas encore d'évaluation
- Parts and Functions of Respiratory SystemDocument18 pagesParts and Functions of Respiratory Systemjosephabram051590Pas encore d'évaluation
- Functions of The Respiratory System: BloodDocument12 pagesFunctions of The Respiratory System: BloodSesrine BuendiaPas encore d'évaluation
- Ma Nurfaizah Ma04200026 Respiratory System April 2020Document3 pagesMa Nurfaizah Ma04200026 Respiratory System April 2020Nur Faizah Binti Jamail MAPas encore d'évaluation
- Respiratory Sistem Kel 2..Document16 pagesRespiratory Sistem Kel 2..Arif WahyuPas encore d'évaluation
- A Simple Guide to the Nose and Its Disorders, Diagnosis, Treatment and Related ConditionsD'EverandA Simple Guide to the Nose and Its Disorders, Diagnosis, Treatment and Related ConditionsPas encore d'évaluation
- Lung Diseases, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsD'EverandLung Diseases, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsPas encore d'évaluation
- Cholinergic Urticaria Associated With Acquired Hypohidrosis: An Ultrastructural StudyDocument2 pagesCholinergic Urticaria Associated With Acquired Hypohidrosis: An Ultrastructural StudyEnggrajati Moses SilitongaPas encore d'évaluation
- Do You Think It Is A Good Idea For Teachers To Give Homework To The Students?Document1 pageDo You Think It Is A Good Idea For Teachers To Give Homework To The Students?Enggrajati Moses SilitongaPas encore d'évaluation
- Dynamics of Body Fluids MovementDocument39 pagesDynamics of Body Fluids MovementEnggrajati Moses SilitongaPas encore d'évaluation
- Behavioural DisordersDocument26 pagesBehavioural DisordersEnggrajati Moses SilitongaPas encore d'évaluation
- Feb 1 - ScottDocument17 pagesFeb 1 - ScottNyannnPas encore d'évaluation
- LITERATURE MATRIX PLAN LastimosaDocument2 pagesLITERATURE MATRIX PLAN LastimosaJoebelle LastimosaPas encore d'évaluation
- Di Franco Amended Factum 2021-05-03Document30 pagesDi Franco Amended Factum 2021-05-03Michael BueckertPas encore d'évaluation
- CM PhysicalDocument14 pagesCM PhysicalLulu Nur HidayahPas encore d'évaluation
- Endogenic Processes (Erosion and Deposition) : Group 3Document12 pagesEndogenic Processes (Erosion and Deposition) : Group 3Ralph Lawrence C. PagaranPas encore d'évaluation
- Dwnload Full Conceptual Physics 12th Edition Hewitt Test Bank PDFDocument36 pagesDwnload Full Conceptual Physics 12th Edition Hewitt Test Bank PDFscreamsoaring.pm7hcv100% (13)
- TreeAgePro 2013 ManualDocument588 pagesTreeAgePro 2013 ManualChristian CifuentesPas encore d'évaluation
- HSE Matrix PlanDocument5 pagesHSE Matrix Planवात्सल्य कृतार्थ100% (1)
- SKI Report2008 - 50 2Document46 pagesSKI Report2008 - 50 2nada safitriPas encore d'évaluation
- The Magical Number SevenDocument3 pagesThe Magical Number SevenfazlayPas encore d'évaluation
- BurnsDocument80 pagesBurnsAlina IlovanPas encore d'évaluation
- Map Index: RD - To CE MP AR KDocument1 pageMap Index: RD - To CE MP AR KswaggerboxPas encore d'évaluation
- Project Dayan PrathaDocument29 pagesProject Dayan PrathaSHREYA KUMARIPas encore d'évaluation
- Thailand Day 2Document51 pagesThailand Day 2Edsel BuletinPas encore d'évaluation
- Geographical Milieu of Ancient KashiDocument14 pagesGeographical Milieu of Ancient Kashismk11Pas encore d'évaluation
- The Acceptability of Indian Mango Leaves Powdered As A Tea: (Mangifera Indica Linn.)Document22 pagesThe Acceptability of Indian Mango Leaves Powdered As A Tea: (Mangifera Indica Linn.)Marissa M. DoriaPas encore d'évaluation
- AC2104 - Seminar 5Document3 pagesAC2104 - Seminar 5Rachel LiuPas encore d'évaluation
- Basic Catholic Prayer 1Document88 pagesBasic Catholic Prayer 1Josephine PerezPas encore d'évaluation
- Norman 2017Document7 pagesNorman 2017Lee HaeunPas encore d'évaluation
- Modbus Manual TD80 PDFDocument34 pagesModbus Manual TD80 PDFAmar ChavanPas encore d'évaluation
- CNS Drugs Pharmaceutical Form Therapeutic Group: 6mg, 8mgDocument7 pagesCNS Drugs Pharmaceutical Form Therapeutic Group: 6mg, 8mgCha GabrielPas encore d'évaluation
- The Old Man and The SeaDocument6 pagesThe Old Man and The Seahomeless_heartPas encore d'évaluation
- Gallery IsKCON Desire Tree PDF MudrasDocument2 pagesGallery IsKCON Desire Tree PDF MudrassanatanPas encore d'évaluation
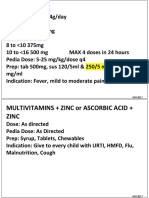
- Common RHU DrugsDocument56 pagesCommon RHU DrugsAlna Shelah IbañezPas encore d'évaluation
- Theology and Pipe Smoking - 7pDocument7 pagesTheology and Pipe Smoking - 7pNeimar HahmeierPas encore d'évaluation
- Đại Từ Quan Hệ Trong Tiếng AnhDocument5 pagesĐại Từ Quan Hệ Trong Tiếng AnhNcTungPas encore d'évaluation
- Hanssen, Eirik.Document17 pagesHanssen, Eirik.crazijoePas encore d'évaluation
- The Distracted Mind - ExcerptDocument15 pagesThe Distracted Mind - Excerptwamu885Pas encore d'évaluation
- Role LibrariesDocument57 pagesRole LibrariesGiovanni AnggastaPas encore d'évaluation
- Complexity. Written Language Is Relatively More Complex Than Spoken Language. ..Document3 pagesComplexity. Written Language Is Relatively More Complex Than Spoken Language. ..Toddler Channel TVPas encore d'évaluation