Académique Documents
Professionnel Documents
Culture Documents
Immune Mediated Autonomic Neuropathies
Transféré par
iri_balDescription originale:
Copyright
Formats disponibles
Partager ce document
Partager ou intégrer le document
Avez-vous trouvé ce document utile ?
Ce contenu est-il inapproprié ?
Signaler ce documentDroits d'auteur :
Formats disponibles
Immune Mediated Autonomic Neuropathies
Transféré par
iri_balDroits d'auteur :
Formats disponibles
Immune Mediated Autonomic Neuropathies
Roy Freeman, MD
Department of Neurology, Beth Israel Deaconess Medical Center Harvard Medical School, Boston, Massachusetts, U.S.A.
Address correspondence to: Roy Freeman M.D. Autonomic and Peripheral Nerve Laboratory Department of Neurology, Beth Israel Deaconess Medical Center 1 Deaconess Road, Boston, MA 02215, U.S.A. Phone: (617) 632-8454 FAX: (617) 632-8454 Email: rfreeman@bidmc.harvard.edu
Page 2
Freeman
Introduction Autonomic nerve fibers are affected in most generalized peripheral neuropathies. While this involvement is often mild or subclinical, there are a group of peripheral neuropathies in which the small or unmyelinated fibers are selectively or prominently targeted. While most generalized peripheral polyneuropathies are accompanied by clinical or subclinical autonomic dysfunction, there are a group of peripheral neuropathies in which the small or unmyelinated fibers are selectively targeted. In these neuropathies, autonomic dysfunction is the primary manifestation. A constellation of signs and symptoms occur from impairment of cardiovascular, gastrointestinal, urogenital, thermoregulatory, sudomotor and pupillomotor autonomic function.
Autonomic peripheral neuropathies have been associated with the presence of specific autoantibodies and also may present as feature of a presumed immune mediated peripheral neuropathy. This review will cover those neuropathies in which autonomic dysfunction is a prominent and clinically significant manifestation associated with a specific antibody or where an immune mediated etiology is presumed.
Acute and subacute autonomic neuropathies The Guillain-Barr syndrome (acute inflammatory demyelinating polyradiculoneuropathy) is a monophasic illness of immune etiology that presents as an acutely evolving sensorimotor polyneuropathy of varying severity. Autonomic manifestations such as sinus tachycardia, sinus pauses and other tachy- and bradyarrhythmias, blood pressure lability, bowel and bladder dysfunction, pupillomotor disturbances, sudomotor dysfunction, and vasomotor abnormalities frequently accompany the Guillain-Barr syndrome.[Tuck and McLeod 1981;Zochodne 1994] Autonomic manifestations, which occasionally may be the presenting feature of the Guillain-Barr syndrome,[Cortelli et al. 1990] may be more prominent in patients with respiratory failure, severe motor deficits, and the axonal variant of the Guillain-Barr syndrome.[Feasby et al. 1986;Winer and Hughes 1988;Ropper et al. 1991] The autonomic features can result in significant mortality and morbidity in some patients, although they are usually overshadowed by the motor features of the disorder.
Page 3
Freeman
Autonomic manifestations may be the sole or predominant feature of an acute or subacute peripheral neuropathy.[Suarez et al. 1994] The hallmark of these autonomic neuropathies is the acute or subacute presentation, in varying combinations, of orthostatic hypotension, anhidrosis, constipation, bladder atony, impotence, secretomotor paralysis, and blurring of vision associated with tonic pupils. Mild sensorimotor features may accompany the autonomic manifestations but these are not the predominant aspect of the presentation. The autonomic features of this disorder may involve both the sympathetic and parasympathetic divisions of the autonomic nervous system (pandysautonomia)[Young et al. 1975] or the sympathetic or parasympathetic nervous system alone (also called cholinergic dysautonomia).[Hart and Kanter 1990] Only 40% of cases recover fully to premorbid status. For an estimated 12%, symptoms persist to a significant degree. Full or partial recovery, when reported, occurred over the course of months to years. Autonomic testing in the recovery phase of illness in these patients, often shows evidence of persisting subclinical autonomic dysfunction. [Suarez, Fealey, Camilleri, and Low1994]
Sural nerve biopsy specimens have shown loss of small myelinated and unmyelinated fibers in some [Low et al. 1983;Feldman et al. 1991;Kanda et al. 1990] but not all studies.[Taubner and Salanova 1984;Low, Dyck, Lambert, Brimijoin, Trautmann, Malagelada, Fealey, and Barrett1983;Young, Asbury, Corbett, and Adams1975] A perivascular mononuclear infiltrate may be present in some cases.[Suarez, Fealey, Camilleri, and Low1994] Other investigators have observed pathological changes in the sympathetic ganglia[Tohgi et al. 1989;Satake et al. 1998] and their pre- and postganglionic neurons.[Stoll et al. 1991]
The presence of subtle sensory and motor signs and the albuminocytologic dissociation in cerebrospinal fluid has prompted speculation that acute and subacute dysautonomias may represent variants of Guillain-Barr syndrome.[Low, Dyck, Lambert, Brimijoin, Trautmann, Malagelada, Fealey, and Barrett1983] In analogous fashion to Guillain-Barr syndrome, infectious and parainfectious immune-mediated mechanisms may be operative
Page 4
Freeman
in the pathogenesis of these autonomic neuropathies. Acute dysautonomia has been described in association with infectious mononucleosis or Epstein Barr virus,[Yahr and Frontera 1975;Fujii et al. 1982] streptococcus,[Thomashefsky et al. 1972], Coxsackie B virus,[Pavesi et al. 1992] rubella[Summers and Harris 1987] and herpes simplex virus[Neville and Sladen 1984] infections in addition to other non-diagnosed viral syndromes. Associations with malignancies[Fagius et al. 1983;van Lieshout et al. 1986] (see below), and connective tissue diseases have been described in other cases.[Hoyle et al. 1985;Arruda et al. 1989;Wright et al. 1999] Lending further support to the likelihood that some of these cases are immune-mediated, a positive therapeutic response to intravenous immunoglobulin has been reported in uncontrolled case studies.[Heafield et al. 1996;Smit et al. 1997]
Paraneoplastic Autonomic Neuropathy Paraneoplastic autonomic neuropathies have been associated with the presence of specific autoantibodies. These neuropathies usually present subacutely although acute and chronic presentations are reported. Paraneoplastic autonomic neuropathy occurs commonly in association with anti-Hu antibodies (also known as Type 1 anti-neuronal nuclear antibody, ANNA-1). Anti-Hu antibodies are present most often in patients with small cell lung cancer, but can be seen in non-small cell lung cancer or other malignancies of the gastrointestinal tract, prostate, breast, bladder, kidney, pancreas, testicle and ovary.[Lucchinetti et al. 1998;Lennon et al. 1991;Dalmau et al. 1992;Camdessanche et al. 2002] Peripheral neuropathy develops in 60-95% of patients with a malignancy and antiHu antibodies.[Dalmau, Graus, Rosenblum, and Posner1992] Subacute sensory neuronopathy, due to injury to the sensory nerve cell bodies in the dorsal nerve root ganglia, is the most common neuropathy associated with anti-Hu antibodies.
Paraneoplastic autonomic neuropathy is characterized by the subacute onset of symptoms including bowel hypomotility, intestinal obstruction, bladder dysfunction, orthostatic hypotension, blood pressure instability, pupillomotor and sudomotor dysfunction, impotence, and xerophthalmia. Autonomic neuropathy may be the sole manifestation of an anti-Hu related paraneoplastic disorder or may be part of a generalized paraneoplastic
Page 5
Freeman
syndrome that variably includes sensory neuronopathy, limbic and brainstem encephalitis, encephalomyelitis, cerebellar degeneration and a sensorimotor peripheral neuropathy. In recent series of patients with anti-Hu antibodies, dysautonomia was present in 10[Graus et al. 2001]-30[Dalmau, Graus, Rosenblum, and Posner1992;Camdessanche, Antoine, Honnorat, Vial, Petiot, Convers, and Michel2002] of patients, and was the predominant symptom at presentation in 4[Graus, Keime-Guibert, Rene, Benyahia, Ribalta, Ascaso, Escaramis, and Delattre2001]-9%.[Dalmau, Graus, Rosenblum, and Posner1992]
Paraneoplastic autonomic neuropathy has been associated with other antibodies in addition to anti-Hu antibodies, including Purkinje cell cytoplasmic antibodies Type 2 (PCA-2)[Vernino and Lennon 2000] and antibodies to the neuron cytoplasmic protein, collapsin response-mediator protein-5 (CRMP-5).[Yu et al. 2001]
Ganglionic Acetylcholine Receptor Antibody Autonomic Neuropathy High levels of blocking and binding autoantibodies specific for neuronal nicotinic acetylcholine receptors in the autonomic ganglia also have been found in patients with idiopathic and paraneoplastic autonomic neuropathy. Malignancies associated with these antibodies include small-cell lung carcinoma, thymoma, bladder carcinoma, and rectal carcinoma. Characteristic features of this disorder are a subacute onset of symptoms that include gastrointestinal dysmotility, dry eyes and mouth, and abnormal pupillary responses to light and accommodation. There is a positive correlation between high levels of ganglionic-receptor antibodies and the severity of autonomic dysfunction, suggesting that the antibodies may have a pathogenic role in these autonomic neuropathies.[Vernino et al. 2000] These antibodies may be present in patients with the clinical phenotype of pure autonomic failure.[Goldstein et al. 2002] When cholinergic features are prominent, the diagnosis of an immune mediated autonomic neuropathy should be entertained.[Klein et al. 2003]
Lambert-Eaton Myasthenic Syndrome Lambert-Eaton myasthenic syndrome is a subacute, autoimmune disorder of neuromuscular transmission. This disorder is characterized by the production of antibodies directed against presynaptic, voltage-gated calcium channels that impair
Page 6 acetylcholine release and lead to weakness, hyporeflexia, and autonomic
Freeman
dysfunction.[Waterman 2001;Mamdani et al. 1985;O'Suilleabhain et al. 1998] Many cases are paraneoplastic. Dysautonomia is a common manifestation of the LambertEaton syndrome in patients with and without malignancies.[Waterman2001] Symptoms suggesting cholinergic dysfunction such as dry mouth, erectile failure, constipation, blurred vision, and impaired sweating occur most frequently. Autonomic tests, demonstrating unresponsive pupils that constrict to dilute pilocarpine, reduced sweating, salivary and lacrimal secretomotor failure suggest the abnormality is predominantly restricted to the parasympathetic nervous system although adrenergic abnormalities are seen as well.[Mamdani, Walsh, Rubino, Brannegan, and Hwang1985;O'Suilleabhain, Low, and Lennon1998] Treatment is directed at any underlying tumor with immunosuppression used for idiopathic and refractory cases. Motor and autonomic symptoms may improve with the use of 3,4-diaminopyridine, which enhances acetylcholine release.[McEvoy et al. 1989]
Myasthenia Gravis Myasthenia gravis is an autoimmune disorder characterized by antibodies directed at the postsynaptic acetylcholine receptor. These antibodies disrupt neuromuscular transmission leading to fluctuating weakness, with a predilection for ocular and bulbar muscles. An autonomic neuropathy may rarely accompany myasthenia gravis. Investigators have documented autonomic dysfunction with sympathetic and parasympathetic nervous system features.[Vernino et al. 2001] Antibodies directed against muscle acetylcholine receptor (AChR) were present in all patients. Antibodies against neuronal ganglionic AChRs were present in 42% of patients. Gastrointestinal dysmotility, which is a prominent manifestation, may improve following the administration of an acetylcholinesterase inhibitor.[Vernino, Cheshire, and Lennon2001]
Page 7
Freeman
TABLE Specific Antibodies Associated with Autonomic Neuropathies Antinuclear antibody Rheumatoid factor anti-Ro/SSA anti-La/SSB Neuronal nicotinic acetylcholine receptor antibodies P/Q-type Ca2+ channel antibodies Acetylcholine receptor antibodies Paraneoplastic antibodies Anti-Hu antibodies (Type 1 anti-neuronal nuclear antibody, ANNA-1) Purkinje cell antibodies Type 2 (PCA-2) Collapsing response mediator protein-5 (CRMP-5)
Page 8 Reference List
Freeman
Arruda WO, Teive HA, Ramina R, Wunder PR, Rocha LC. Autonomic neuropathy in systemic lupus erythematosus. J.Neurol.Neurosurg.Psychiatry 1989; 52: 539-540. Camdessanche JP, Antoine JC, Honnorat J et al. Paraneoplastic peripheral neuropathy associated with anti-Hu antibodies. A clinical and electrophysiological study of 20 patients. Brain 2002; 125: 166-175. Cortelli P, Contin M, Lugaresi A, Baruzzi A, Montagna P. Severe dysautonomic onset of Guillain-Barr:e syndrome with good recovery. A clinical and autonomic follow-up study. Ital.J.Neurol.Sci. 1990; 11: 159-162. Dalmau J, Graus F, Rosenblum MK, Posner JB. Anti-Hu--associated paraneoplastic encephalomyelitis/sensory neuronopathy. A clinical study of 71 patients. Medicine 1992; 71: 59-72. Fagius J, Westerberg CE, Olsson Y. Acute pandysautonomia and severe sensory deficit with poor recovery. A clinical, neurophysiological and pathological case study. J.Neurol.Neurosurg.Psychiatry 1983; 46: 725-733. Feasby TE, Gilbert JJ, Brown WF et al. An acute axonal form of Guillain-Barre polyneuropathy. Brain 1986; 109: 1115-1126. Feldman EL, Bromberg MB, Blaivas M, Junck L. Acute pandysautonomic neuropathy. Neurology 1991; 41: 746-748. Fujii N, Tabira T, Shibasaki H, Kuroiwa Y, Ohnishi A, Nagaki J. Acute autonomic and sensory neuropathy associated with elevated Epstein-Barr virus antibody titre [letter]. J.Neurol.Neurosurg.Psychiatry. 1982; 45: 656-657. Goldstein DS, Holmes C, Dendi R, Li ST, Brentzel S, Vernino S. Pandysautonomia associated with impaired ganglionic neurotransmission and circulating antibody to the neuronal nicotinic receptor. Clin.Auton.Res. 2002; 12: 281-285. Graus F, Keime-Guibert F, Rene R et al. Anti-Hu-associated paraneoplastic encephalomyelitis: analysis of 200 patients. Brain 2001; 124: 1138-1148. Hart RG, Kanter MC. Acute autonomic neuropathy. Two cases and a clinical review. Arch.Intern.Med. 1990; 150: 2373-2376. Heafield MT, Gammage MD, Nightingale S, Williams AC. Idiopathic dysautonomia treated with intravenous gammaglobulin. Lancet 1996; 347: 28-29. Hoyle C, Ewing DJ, Parker AC. Acute autonomic neuropathy in association with systemic lupus erythematosus. Ann.Rheum.Dis. 1985; 44: 420-424.
Page 9
Freeman
Kanda F, Uchida T, Jinnai K et al. Acute autonomic and sensory neuropathy: a case report. J.Neurol. 1990; 237: 42-44. Klein CM, Vernino S, Lennon VA et al. The spectrum of autoimmune autonomic neuropathies. Ann.Neurol. 2003; 53: 752-758. Lennon VA, Sas DF, Busk MF et al. Enteric neuronal autoantibodies in psuedoobstruction with small cell lung carcinoma. Gastroenterology 1991; 100: 137-142. Low PA, Dyck PJ, Lambert EH et al. Acute panautonomic neuropathy. Ann.Neurol. 1983; 13: 412-417. Lucchinetti CF, Kimmel DW, Lennon VA. Paraneoplastic and oncologic profiles of patients seropositive for type 1 antineuronal nuclear autoantibodies. Neurology 1998; 50: 652-657. Mamdani MB, Walsh RL, Rubino FA, Brannegan RT, Hwang MH. Autonomic dysfunction and Eaton Lambert syndrome. J.Auton.Nerv.Syst. 1985; 12: 315-320. McEvoy KM, Windebank AJ, Daube JR, Low PA. 3,4-Diaminopyridine in the treatment of Lambert-Eaton myasthenic syndrome. N.Engl.J.Med. 1989; 321: 1567-1571. Neville BG, Sladen GE. Acute autonomic neuropathy following primary herpes simplex infection. J.Neurol.Neurosurg.Psychiatry. 1984; 47: 648-650. O'Suilleabhain P, Low PA, Lennon VA. Autonomic dysfunction in the Lambert-Eaton myasthenic syndrome: serologic and clinical correlates. Neurology 1998; 50: 88-93. Pavesi G, Gemignani F, Macaluso GM et al. Acute sensory and autonomic neuropathy: possible association with coxsackie B virus infection. J.Neurol.Neurosurg.Psychiatry. 1992; 55: 613-615. Ropper AH, Wijdicks EFM, Truax BT. Guillain Barre Syndrome. Philadelphia: F.A. Davis, 1991. Satake M, Nakagawa Y, Yamashita S et al. Subacute autonomic and sensory ganglionopathy: a postmortem case. J.Neurol.Neurosurg.Psychiatry 1998; 64: 561. Smit AA, Vermeulen M, Koelman JH, Wieling W. Unusual recovery from acute panautonomic neuropathy after immunoglobulin therapy. Mayo Clin.Proc. 1997; 72: 333335. Stoll G, Thomas C, Reiners K, Schober R, Hartung HP. Encephalo-myelo-radiculoganglionitis presenting as pandysautonomia. Neurology 1991; 41: 723-726. Suarez GA, Fealey RD, Camilleri M, Low PA. Idiopathic autonomic neuropathy: clinical, neurophysiologic, and follow-up studies on 27 patients. Neurology 1994; 44: 1675-1682.
Page 10
Freeman
Summers Q, Harris A. Autonomic neuropathy after rubella infection. Med.J.Aust. 1987; 147: 353-355. Taubner RW, Salanova V. Acute dysautonomia and polyneuropathy. Arch.Neurol. 1984; 41: 1100-1101. Thomashefsky AJ, Horwitz SJ, Feingold MH. Acute autonomic neuropathy. Neurology 1972; 22: 251-255. Tohgi H, Sano M, Sasaki K et al. Acute autonomic and sensory neuropathy: report of an autopsy case. Acta Neuropathol.(Berl) 1989; 77: 659-663. Tuck RR, McLeod JG. Autonomic dysfunction in Guillain-Barre syndrome. J.Neurol.Neurosurg.Psychiatry. 1981; 44: 983-990. van Lieshout JJ, Wieling W, van Montfrans GA et al. Acute dysautonomia associated with Hodgkin's disease [published erratum appears in J Neurol Neurosurg Psychiatry 1986 Dec;49(12): 1461]. J.Neurol.Neurosurg.Psychiatry. 1986; 49: 830-832. Vernino S, Cheshire WP, Lennon VA. Myasthenia gravis with autoimmune autonomic neuropathy. Auton.Neurosci. 2001; 88: 187-192. Vernino S, Lennon VA. New Purkinje cell antibody (PCA-2): marker of lung cancerrelated neurological autoimmunity. Ann.Neurol. 2000; 47: 297-305. Vernino S, Low PA, Fealey RD, Stewart JD, Farrugia G, Lennon VA. Autoantibodies to ganglionic acetylcholine receptors in autoimmune autonomic neuropathies. N.Engl.J.Med. 2000; 343: 847-855. Waterman SA. Autonomic dysfunction in Lambert-Eaton myasthenic syndrome. Clin.Auton.Res. 2001; 11: 145-154. Winer JB, Hughes RAC. Identification of patients at risk of arrhythmia in the GuillainBarre syndrome. Q.J.Med. 1988; 257: 735-739. Wright RA, Grant IA, Low PA. Autonomic neuropathy associated with sicca complex. J.Auton.Nerv.Syst. 1999; 75: 70-76. Yahr MD, Frontera AT. Acute autonomic neuropathy. Its occurrence in infectious mononucleosis. Arch.Neurol. 1975; 32: 132-133. Young RR, Asbury AK, Corbett JL, Adams RD. Pure pan-dysautonomia with recovery. Brain 1975; 98: 613-636. Yu Z, Kryzer TJ, Griesmann GE, Kim K, Benarroch EE, Lennon VA. CRMP-5 neuronal autoantibody: marker of lung cancer and thymoma-related autoimmunity. Ann.Neurol. 2001; 49: 146-154.
Page 11
Freeman
Zochodne DW. Autonomic involvement in Guillain-Barre syndrome: a review. Muscle Nerve 1994; 17: 1145-1155.
Vous aimerez peut-être aussi
- Liver Function in Early Lyme PDFDocument6 pagesLiver Function in Early Lyme PDFiri_balPas encore d'évaluation
- Lyme Combat IVDocument51 pagesLyme Combat IViri_balPas encore d'évaluation
- ULDN Inverse Titration Protocol FINALDocument50 pagesULDN Inverse Titration Protocol FINALiri_bal100% (2)
- Naltrexone and Autoimmune Disease - Grandpa's Cmpding RXDocument6 pagesNaltrexone and Autoimmune Disease - Grandpa's Cmpding RXiri_balPas encore d'évaluation
- Brain Wave VibrationDocument6 pagesBrain Wave Vibrationiri_bal100% (2)
- Alternative DietDocument31 pagesAlternative Dietiri_balPas encore d'évaluation
- The Yellow House: A Memoir (2019 National Book Award Winner)D'EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Évaluation : 4 sur 5 étoiles4/5 (98)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeD'EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeÉvaluation : 4 sur 5 étoiles4/5 (5795)
- Shoe Dog: A Memoir by the Creator of NikeD'EverandShoe Dog: A Memoir by the Creator of NikeÉvaluation : 4.5 sur 5 étoiles4.5/5 (537)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureD'EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureÉvaluation : 4.5 sur 5 étoiles4.5/5 (474)
- Grit: The Power of Passion and PerseveranceD'EverandGrit: The Power of Passion and PerseveranceÉvaluation : 4 sur 5 étoiles4/5 (588)
- On Fire: The (Burning) Case for a Green New DealD'EverandOn Fire: The (Burning) Case for a Green New DealÉvaluation : 4 sur 5 étoiles4/5 (74)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryD'EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryÉvaluation : 3.5 sur 5 étoiles3.5/5 (231)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceD'EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceÉvaluation : 4 sur 5 étoiles4/5 (895)
- Never Split the Difference: Negotiating As If Your Life Depended On ItD'EverandNever Split the Difference: Negotiating As If Your Life Depended On ItÉvaluation : 4.5 sur 5 étoiles4.5/5 (838)
- The Little Book of Hygge: Danish Secrets to Happy LivingD'EverandThe Little Book of Hygge: Danish Secrets to Happy LivingÉvaluation : 3.5 sur 5 étoiles3.5/5 (400)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersD'EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersÉvaluation : 4.5 sur 5 étoiles4.5/5 (345)
- The Unwinding: An Inner History of the New AmericaD'EverandThe Unwinding: An Inner History of the New AmericaÉvaluation : 4 sur 5 étoiles4/5 (45)
- Team of Rivals: The Political Genius of Abraham LincolnD'EverandTeam of Rivals: The Political Genius of Abraham LincolnÉvaluation : 4.5 sur 5 étoiles4.5/5 (234)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyD'EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyÉvaluation : 3.5 sur 5 étoiles3.5/5 (2259)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaD'EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaÉvaluation : 4.5 sur 5 étoiles4.5/5 (266)
- The Emperor of All Maladies: A Biography of CancerD'EverandThe Emperor of All Maladies: A Biography of CancerÉvaluation : 4.5 sur 5 étoiles4.5/5 (271)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreD'EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreÉvaluation : 4 sur 5 étoiles4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)D'EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Évaluation : 4.5 sur 5 étoiles4.5/5 (121)
- Her Body and Other Parties: StoriesD'EverandHer Body and Other Parties: StoriesÉvaluation : 4 sur 5 étoiles4/5 (821)
- Impaired Urinary EliminationDocument5 pagesImpaired Urinary Eliminationapi-279878989Pas encore d'évaluation
- UNIT 16 Spa Treatments Syllabus V2Document7 pagesUNIT 16 Spa Treatments Syllabus V2Jowie SooPas encore d'évaluation
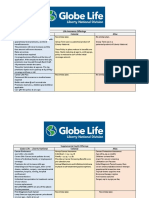
- Life Insurance Offerings Globe Life - Liberty National Colonial AflacDocument3 pagesLife Insurance Offerings Globe Life - Liberty National Colonial AflacTina Hughes0% (1)
- Lec - 4 - Risk AnalysisDocument22 pagesLec - 4 - Risk Analysisحسن خالد وسوPas encore d'évaluation
- Sarcoma Surveillance A Review of Current Evidence.2Document12 pagesSarcoma Surveillance A Review of Current Evidence.2Fernanda Lorena AcevesPas encore d'évaluation
- Miracle MineralsDocument32 pagesMiracle MineralsTURGIS100% (13)
- Immunotherapy For Lung CancerDocument3 pagesImmunotherapy For Lung CancerPongwirat ChantasoontornPas encore d'évaluation
- Grabovoi NumbersDocument17 pagesGrabovoi Numbershealthy57Pas encore d'évaluation
- It's Official! Vegetarian Centenarians Are Happier Healthier Than Aging Meat-eaters - Mrs. Nasib Kaur Surpasses 100 Years Old Eating Plant-based Diet and Loving It - Majid Ali, Nir Barzilai - Non-LowCarb Non-Paleo Longevity DietDocument3 pagesIt's Official! Vegetarian Centenarians Are Happier Healthier Than Aging Meat-eaters - Mrs. Nasib Kaur Surpasses 100 Years Old Eating Plant-based Diet and Loving It - Majid Ali, Nir Barzilai - Non-LowCarb Non-Paleo Longevity DietPaleoCentenarianDietPas encore d'évaluation
- Journal ReadingDocument29 pagesJournal ReadingAchmad YasinPas encore d'évaluation
- New GOLD Guideline 2011Document25 pagesNew GOLD Guideline 2011ebramnainggolanPas encore d'évaluation
- The Timber News! - November 2010Document20 pagesThe Timber News! - November 2010TheTimberNewsPas encore d'évaluation
- BBBBBXXDocument5 pagesBBBBBXXodi jayaPas encore d'évaluation
- Nuclear Medicine - Radioactivity For Diagnosis and TherapyDocument217 pagesNuclear Medicine - Radioactivity For Diagnosis and TherapyPriscila FloresPas encore d'évaluation
- Exam 1 PracticumDocument9 pagesExam 1 Practicumapi-310181843Pas encore d'évaluation
- Congress Program September 2022 Anglisht 1 1Document17 pagesCongress Program September 2022 Anglisht 1 1ediPas encore d'évaluation
- Leeward Microbiology 130 DR - Kae Final ExamDocument164 pagesLeeward Microbiology 130 DR - Kae Final Examraymond theardPas encore d'évaluation
- Buccal Mucosa CancerDocument9 pagesBuccal Mucosa Cancermuhammad_ariefPas encore d'évaluation
- MRCPCH - Important Skin DiseasesDocument42 pagesMRCPCH - Important Skin DiseasesarjumandPas encore d'évaluation
- Xiaoming Zhu China's Technology Innovators Selected Cases On Creating and Staying Ahead of Business TrendsDocument193 pagesXiaoming Zhu China's Technology Innovators Selected Cases On Creating and Staying Ahead of Business TrendsrezasattariPas encore d'évaluation
- Kontrasepsi: Brahmantyo Danang GuntoroDocument22 pagesKontrasepsi: Brahmantyo Danang GuntoroAzuma Asma Azizah100% (1)
- Saudi Counsel Exams For LabDocument30 pagesSaudi Counsel Exams For Labasif86% (14)
- Bio Energetic TherapyDocument19 pagesBio Energetic TherapyVishnu Moorthy Raja Singam100% (2)
- Head and Neck Laryngeal Tumors An OverviewDocument7 pagesHead and Neck Laryngeal Tumors An OverviewpupuayuwandiraPas encore d'évaluation
- Chapter 22 - The Respiratory SystemDocument15 pagesChapter 22 - The Respiratory SystemTony Snearly100% (1)
- Psa Testing A Critical Look at Current RecommendationsDocument4 pagesPsa Testing A Critical Look at Current Recommendationsapi-306915317Pas encore d'évaluation
- The Cellular Basis of Disease: Cell Injury 3 Apoptosis and Necrosis Cellular AgingDocument49 pagesThe Cellular Basis of Disease: Cell Injury 3 Apoptosis and Necrosis Cellular AgingZabella SilvianaPas encore d'évaluation
- 2 - Cell Culture LectureDocument45 pages2 - Cell Culture LectureSathvik PalakurtyPas encore d'évaluation
- Skippers United Pacific, Inc. vs. Lagne DigestDocument4 pagesSkippers United Pacific, Inc. vs. Lagne DigestEmir MendozaPas encore d'évaluation
- BRVO PPT by Dr. Chinmay KharadeDocument31 pagesBRVO PPT by Dr. Chinmay KharadeChinmay KharadePas encore d'évaluation