Académique Documents
Professionnel Documents
Culture Documents
Recommendations and Regimens For Pediatric Sepsis and Septic Shock
Transféré par
Robertus MaharyadyTitre original
Copyright
Formats disponibles
Partager ce document
Partager ou intégrer le document
Avez-vous trouvé ce document utile ?
Ce contenu est-il inapproprié ?
Signaler ce documentDroits d'auteur :
Formats disponibles
Recommendations and Regimens For Pediatric Sepsis and Septic Shock
Transféré par
Robertus MaharyadyDroits d'auteur :
Formats disponibles
Recommendations and Regimens for Pediatric Sepsis and Septic Shock
The definition of severe sepsis and septic shock in children is similar to that in adults. However, in pediatric patients, a systemic inflammatory response includes an abnormal temperature or abnormal leukocyte count as part of the clinical presentation. In addition, there are age-specific normative values for vital signs.[1] Time-sensitive, goal-directed therapy is the rule. Consensus guidelines and reviews are available.[2, 3] Most guidelines are available online through the Pediatric Sepsis Initiative.[4] The Pediatric Advanced Life Support (PALS) Pocket Reference Card provides a summary algorithm. [5] Details of early recognition and treatment of sepsis and septic shock are provided below. 1. Recognize signs of poor perfusion (0-5min) Decreased mental status Cold extremities Delayed capillary refill Weak pulses, differential central and peripheral pulses Low urine output Hypotension or low BP: Minimum systolic BP by age: < 1mo: 60 mmHg; 1mo to 10y: 70 + (2 age in years); 10y: 90 mmHg 2. Assess ABCs (0-5 min) Provide 100% oxygen at high flow rate (15L) Early intubation may be necessary in neonates and infants Breathing assistance as necessary, including mechanical ventilation 3. Establish IV access and place on monitor (0-5min)
2 large-bore peripheral IVs (PIVs) preferred: if difficult IV, place IO access per PALS guidelines; 1 PIV may be sufficient unless vasoactive drugs needed (see Step No. 6, below) Consider labs on IV placement: blood gas, lactate, glucose, ionized calcium, CBC, cultures (glucose check through finger stick preferred for rapid result) 4. Fluid and electrolyte resuscitation (5-15min) Fluids: Push 20 mL/kg fluid (isotonic crystalloid) IV/IO over 5-20min or faster if needed (reassess for signs of shock; see Step No. 11, below) Repeat 20 mL/kg bolus push of fluid (up to 60 mL/kg) until clinical symptoms improve or patient develops respiratory distress/rales/ hepatomegaly May continue to require additional fluid above 60 mL/kg (fluid refractory) (see Step No. 6, below) Fluid needs may approach 200 mL/kg in warm septic shock (warm extremities, flash capillary refill) Correct hypoglycemia: Glucose levels in hypoglycemia: Neonates < 45 mg/dL; infants/children < 60 mg/dL Glucose dosage: 0.5-1 g/kg IV/IO (max that can be administered through a peripheral vein is 25% dextrose in water) (see alternative treatments immediately below) Treatment options to provide 0.5-1 g/kg glucose: For infant/child: dextrose 25% in water: 2-4 mL/kg IV/IO; dextrose 10% in water: 5-10 mL/kg IV/IO; for neonate: dextrose 10% in water: 2-4 mL IV/IO; consider maintenance fluid containing dextrose Correct hypocalcemia for low ionized calcium: Calcium gluconate 100 mg/kg IV/IO (max 2g) PRN
Calcium chloride 20 mg/kg IV/IO PRN (Note: central line administration preferred over 60min in nonarrest situation) 5. Infection control (5-60min) Immediate considerations:
Administer antibiotics immediately after cultures obtained (blood, urine, +/- CSF/ sputum) Do not delay antibiotics because of delay in obtaining cultures; initial antibiotics should be given within 1h General treatment recommendations:
Empiric therapy should be used for unknown etiology of sepsis; Tailoring of therapy to address suspected pathogens or to achieve adequate drug penetration may be necessary; Broader initial coverage may be needed for initial stabilization Dosing varies by age and weight (see specific recommendations and dosages immediately below) Neonates < 2kg: Consult institution pharmacist and primary medication references for your institution practice and for preterm infants and neonates < 2kg Neonates >2kg:
Ampicillin plus gentamicin: Ampicillin for 0-7d: 50 mg/kg IV/IM/IO q8h; ampicillin >7d: 50 mg/kg IV/IM/IO q6h plus gentamicin (dosing institution dependent): 4mg/kg IV/IO/IM q24h (alternative for 07d: 2.5 mg/kg IV/IO/IM q12h; alternative for >7d: 2.5 mg/kg IV/IO/IM q8h) or Ampicillin plus cefotaxime: Ampicillin for 0-7d: 50 mg/kg IV/IM/IO q8h; ampicillin >7d: 50 mg/kg IV/IM/IO q6h plus cefotaxime 50 mg/kg IV/IO q8h Infants (>1mo) and children: Ceftriaxone 75 mg/kg (max 2g) IV/IO/IM q24h plus vancomycin 15mg/kg (max 1g) IV/IO q8h Immunosuppressed patients: Vancomycin 15 mg/kg IV/IO (max 1 g/dose) q8h plus cefepime 50 mg/kg IV/IO (max 2g/dose) q8h; consider antifungal therapy Duration of therapy:
Determined by ultimate source of infection; 7-10d is typically sufficient Above regimens may be empiric therapy for 48-72h, until cultures and sensitivities are known, so as to accurately tailor treatment If culture-negative sepsis, antibiotic choice and duration determined by severity of presentation and most likely pathogen Infectious disease consultation may be necessary 6. Fluid-refractory shock (persisting after 60 mL/kg fluid) (15-60 min) Continue fluid resuscitation and initiate vasopressor therapy titrated to correct hypotension/poor perfusion Central line placement and arterial monitoring if not already established; vasopressors should not be delayed for line placements Normotensive shock (impaired perfusion but normal blood pressure): Dopamine 2-20 mcg/kg/min IV/IO, titrate to desired effect; if continued poor perfusion, consider dobutamine infusion 2-20 mcg/kg/min IV/IO, titrate to desired effect (may cause hypotension, tachycardia) Warm shock (warm extremities, flash capillary refill): Norepinephrine 0.1-2 mcg/kg/min IV/IO infusion, titrate to desired effect Cold shock (cool extremities, delayed capillary refill): Epinephrine 0.1-1 mcg/kg/min IV/IO infusion, titrate to desired effect 7. Shock persists following vasopressor initiation (60 min)
Continued fluid replacement; obtain CVP measurement to guide SvO2 < 70% (cold shock): Transfuse Hgb >10 g/dL; optimize arterial saturation through oxygen therapy, ventilation; epinephrine 0.1-1 mcg/kg/min IV/IO infusion, titrate to desired effect SvO2 < 70% (normal BP but impaired perfusion): Transfuse Hgb >10 g/dL; optimize arterial saturation through oxygen therapy, ventilation; consider addition of milrinone 0.25-0.75 mcg/kg/min IV/IO (titrate to desired effect) ornitroprusside 0.3-5 mcg/kg/min IV/IO (titrate to desired effect) SvO2 >70% (warm shock): Norepinephrine 0.1-2 mcg/kg/min IV/IO infusion, titrate to desired effect; consider vasopressin 0.2-2 mU/kg/min infusion, titrate to desired effect 8. Fluid refractory and vasopressor-dependent shock) (60 min) Consider adrenal insufficiency Hydrocortisone 2 mg/kg (max 100mg) IV/IO bolus; obtain baseline cortisol level; if unsure, consider ACTH stimulation test; duration depends on response, laboratory evaluation 9. Continued shock Consider cardiac output measurement to direct further therapy Consider extracorporeal membrane oxygenation (ECMO) 10. Supplemental therapies Blood transfusion considered for Hgb < 10 g/dL (ideal threshold for transfusion unknown) Sedation/analgesia while ventilated Optimize oxygenation through ventilation IV immunoglobulin can be considered (unknown benefit; see Step No. 6 Infection Control for dosing information) 11. Therapeutic endpoints Clinical Heart Rate normalized for age Capillary refill < 2sec Normal pulse quality No difference in central and peripheral pulses Warm extremities Blood pressure normal for age Urine output >1 mL/kg/h Normal mental status CVP >8 mmHg Laboratory Decreasing lactate SvO2 >70%
Vous aimerez peut-être aussi
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryD'EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryÉvaluation : 3.5 sur 5 étoiles3.5/5 (231)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)D'EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Évaluation : 4.5 sur 5 étoiles4.5/5 (120)
- Grit: The Power of Passion and PerseveranceD'EverandGrit: The Power of Passion and PerseveranceÉvaluation : 4 sur 5 étoiles4/5 (588)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaD'EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaÉvaluation : 4.5 sur 5 étoiles4.5/5 (266)
- The Little Book of Hygge: Danish Secrets to Happy LivingD'EverandThe Little Book of Hygge: Danish Secrets to Happy LivingÉvaluation : 3.5 sur 5 étoiles3.5/5 (399)
- Never Split the Difference: Negotiating As If Your Life Depended On ItD'EverandNever Split the Difference: Negotiating As If Your Life Depended On ItÉvaluation : 4.5 sur 5 étoiles4.5/5 (838)
- Shoe Dog: A Memoir by the Creator of NikeD'EverandShoe Dog: A Memoir by the Creator of NikeÉvaluation : 4.5 sur 5 étoiles4.5/5 (537)
- The Emperor of All Maladies: A Biography of CancerD'EverandThe Emperor of All Maladies: A Biography of CancerÉvaluation : 4.5 sur 5 étoiles4.5/5 (271)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeD'EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeÉvaluation : 4 sur 5 étoiles4/5 (5794)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyD'EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyÉvaluation : 3.5 sur 5 étoiles3.5/5 (2259)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersD'EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersÉvaluation : 4.5 sur 5 étoiles4.5/5 (344)
- Team of Rivals: The Political Genius of Abraham LincolnD'EverandTeam of Rivals: The Political Genius of Abraham LincolnÉvaluation : 4.5 sur 5 étoiles4.5/5 (234)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreD'EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreÉvaluation : 4 sur 5 étoiles4/5 (1090)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceD'EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceÉvaluation : 4 sur 5 étoiles4/5 (895)
- Her Body and Other Parties: StoriesD'EverandHer Body and Other Parties: StoriesÉvaluation : 4 sur 5 étoiles4/5 (821)
- Pharmacology and The Nursing Process - Linda Lane Lilley PDFDocument2 073 pagesPharmacology and The Nursing Process - Linda Lane Lilley PDFChristopher Patch95% (20)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureD'EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureÉvaluation : 4.5 sur 5 étoiles4.5/5 (474)
- Catapres (Clonidine)Document2 pagesCatapres (Clonidine)Adrianne BazoPas encore d'évaluation
- The Unwinding: An Inner History of the New AmericaD'EverandThe Unwinding: An Inner History of the New AmericaÉvaluation : 4 sur 5 étoiles4/5 (45)
- The Yellow House: A Memoir (2019 National Book Award Winner)D'EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Évaluation : 4 sur 5 étoiles4/5 (98)
- s37 Cello Syl RCM 2013 Online SecuredDocument102 pagess37 Cello Syl RCM 2013 Online SecuredRobertus Maharyady100% (4)
- On Fire: The (Burning) Case for a Green New DealD'EverandOn Fire: The (Burning) Case for a Green New DealÉvaluation : 4 sur 5 étoiles4/5 (73)
- Test Bank For Basic Pharmacology For Nursing 17th EditionDocument10 pagesTest Bank For Basic Pharmacology For Nursing 17th EditionUsman HaiderPas encore d'évaluation
- Standard Operating Procedure Cold Chain ManagementDocument3 pagesStandard Operating Procedure Cold Chain ManagementDaniel Yves IV Paez100% (1)
- Objection Handling With ConfidenceDocument3 pagesObjection Handling With ConfidenceAnup Soans100% (2)
- Microencapsulation SummaryDocument48 pagesMicroencapsulation SummaryDullah Zungu100% (2)
- Philippines Pharmaceutical Country ProfileDocument347 pagesPhilippines Pharmaceutical Country Profilemrk_rlndPas encore d'évaluation
- Textbook of Forensic PharmacyDocument201 pagesTextbook of Forensic PharmacyAmbika DurgPas encore d'évaluation
- Detailed Drug StudyDocument5 pagesDetailed Drug StudyKarl Vincent SosoPas encore d'évaluation
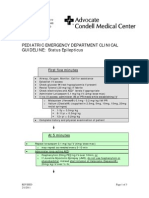
- Condell PedStatusEpilepticusGuildlines 2011Document3 pagesCondell PedStatusEpilepticusGuildlines 2011Robertus MaharyadyPas encore d'évaluation
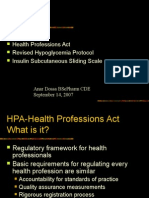
- Health Professions Act Revised Hypoglycemia Protocol Insulin Subcutaneous Sliding ScaleDocument55 pagesHealth Professions Act Revised Hypoglycemia Protocol Insulin Subcutaneous Sliding ScaleRobertus MaharyadyPas encore d'évaluation
- Morpot TN Jhony TampubolonDocument1 pageMorpot TN Jhony TampubolonRobertus MaharyadyPas encore d'évaluation
- JNC 7 (Klasifikasi Hipertensi) PDFDocument2 pagesJNC 7 (Klasifikasi Hipertensi) PDFAbdur RahmanPas encore d'évaluation
- Cerebral Palsy PDFDocument6 pagesCerebral Palsy PDFRobertus MaharyadyPas encore d'évaluation
- Masalah: Aktif: Pasif:: PH: PP: DPJPDocument2 pagesMasalah: Aktif: Pasif:: PH: PP: DPJPRobertus MaharyadyPas encore d'évaluation
- PropanolDocument8 pagesPropanolStacey CamillePas encore d'évaluation
- Applying For Eligibility To Complete An Overseas Pharmacists Assessment Programme March 2021 3Document28 pagesApplying For Eligibility To Complete An Overseas Pharmacists Assessment Programme March 2021 3DuaaPas encore d'évaluation
- Introduction To Pharmacology by ZebDocument31 pagesIntroduction To Pharmacology by ZebSanam MalikPas encore d'évaluation
- Critical Thinking Essay-Animal Testing: Rough DraftDocument10 pagesCritical Thinking Essay-Animal Testing: Rough Draftjeremygcap2017Pas encore d'évaluation
- Introduction To Microbiology: by T. Topodzi Bpharm (Hons) University of ZimbabweDocument13 pagesIntroduction To Microbiology: by T. Topodzi Bpharm (Hons) University of ZimbabweVon Valentine MhutePas encore d'évaluation
- Dyspepsia in PregnancyDocument1 pageDyspepsia in Pregnancydownload spssPas encore d'évaluation
- Strategy of Pharmacitical IndustryDocument3 pagesStrategy of Pharmacitical IndustrysukeshPas encore d'évaluation
- Ascendant PQP1Document19 pagesAscendant PQP1Raaja VishwaPas encore d'évaluation
- HMR TemplateDocument2 pagesHMR TemplatepharmacisticusPas encore d'évaluation
- Pharma Parenteral Dosage CalculationDocument3 pagesPharma Parenteral Dosage CalculationMaxinne RoseñoPas encore d'évaluation
- CRESTOR Citizen's PetitionDocument14 pagesCRESTOR Citizen's Petitiontuckerd99Pas encore d'évaluation
- JurnalDocument7 pagesJurnalAdy Adha NorsaniePas encore d'évaluation
- Biocon Business EthicsDocument21 pagesBiocon Business EthicsNirjon Dip100% (1)
- Breast Cancer FinaleDocument30 pagesBreast Cancer Finaleخايزورا راهيمPas encore d'évaluation
- Keuntungan Dan Kerugian PastaDocument2 pagesKeuntungan Dan Kerugian PastaMiranda MilePas encore d'évaluation
- Clinical Pharmacist Health Consultant in Pittsburgh PA Resume Michele MosierDocument2 pagesClinical Pharmacist Health Consultant in Pittsburgh PA Resume Michele MosierMicheleMosierPas encore d'évaluation
- Trudell Resume 2Document2 pagesTrudell Resume 2api-323367567Pas encore d'évaluation
- Transition of CareDocument52 pagesTransition of CareAffan PresentationsPas encore d'évaluation
- Intravenous Bolus Administration Part II PDFDocument44 pagesIntravenous Bolus Administration Part II PDFAlaa MansourPas encore d'évaluation
- DR - Saleh SFDA Bioeq IntroductionDocument8 pagesDR - Saleh SFDA Bioeq IntroductionkathreentracyPas encore d'évaluation
- JPM Healthcare Conf HandoutDocument25 pagesJPM Healthcare Conf HandoutkriznanPas encore d'évaluation