Académique Documents
Professionnel Documents
Culture Documents
Sterilization
Transféré par
Nicole SooCopyright
Formats disponibles
Partager ce document
Partager ou intégrer le document
Avez-vous trouvé ce document utile ?
Ce contenu est-il inapproprié ?
Signaler ce documentDroits d'auteur :
Formats disponibles
Sterilization
Transféré par
Nicole SooDroits d'auteur :
Formats disponibles
Sterilization Sterilization -processes by which all pathogenic and nonpathogenic microorganisms, including spores, are killed.
This term refers only to a process capable of destroying all forms of microbial life, including spores. Bacterial spores are the most resistant of all living organisms because of their capacity to withstand external destructive agents. The sterilizer* is a piece of equipment used to attain either physical or chemical sterilization. The agent used must be capable of killing all forms of microorganisms. Sterilization vs Disinfection The sterilization process should provide the highest level of assurance that an item can be expected to be free of known viable pathogenic and nonpathogenic microorganisms, including spores. For items and materials that cannot be sterilized, disinfectants are used to kill as many microorganisms in the environment as possible. Terms associated with sterilization Sterile- microorganisms are at an irreducible minimum. Terminal cleaning- thorough cleaning and disinfection of the perioperative environment at the end of use. Terminal sterilization and disinfection- procedures carried out for the destruction of pathogens at the end of the surgical procedure in the OR or in other areas of patient contact. (e.g., PACU, ICU, patient care unit) Case cart- system of preselecting and delivering instruments and supplies to the perioperative environment. Some models include provision for the return of instruments and contaminated items to the appropriate decontamination area. Custom packs- prepackaged disposable supplies prepared by the manufacturer or the distributor according to specific instructions and requests by a particular service at a facility. Turnover- activity geared toward cleaning and preparation of the operating room between cases for the next patients arrival. Wet pack- internal aspect of sterile package is moist or damp. Indicates a nonsterile item. Wicking- passage of fluids through a material by passive action. Also referred to as capillary action or strike-through.
Reliability parameters for sterilization Product-associated parameters Bioburden- the degree of contamination with microorganisms and organic debris. Bioresistance- factors such as heat and/or moisture sensitivities and product stability. Biostate- nutritional, physical, and/or reproductive phase of microorganisms. Bioshielding- characteristics of the packaging materials. Density- factors affecting penetration and evacuation of the agent. Process-associated parameters Temperature
Humidity/moisture/hydration Time Purity of the agent and air and the residual effects or residues Saturation/penetration Capacity of the sterilizer and the position of items within the chamber.
Sterilization cycle/process cycle- time required to achieve sterilization. Heat up and/or penetration of the agent Kill time (i.e., exposure to the agent) Safety factor for bioburden Evacuation or dissipation of the agent
Monitoring the sterilization cycle Administrative monitoring Decontaminating, terminally sterilizing, and cleaning all reusable items; disposing of disposable items in the appropriate manner Packaging and labeling items Loading and unloading the sterilizer Operating the sterilizer Monitoring and maintaining the records of each cycle Adhering to safety precautions and preventive maintenance protocol Storing sterile items Handling sterile items ready for use Making a sterile transfer to the sterile field at the point of use Tracking and recalling items if an item in a particular load is not safe for use Mechanical indicators Routine maintenance that consists of daily inspections and scheduled cleanings per the manufacturers recommendation Preventive maintenance: periodic calibration, lubrication, and function checks by qualified personnel on a scheduled basis. Each PM should be documented. Chemical indicators- help monitor the physical conditions within the sterilizer to alert personnel to malfunctions, human errors in packaging, or improper loading of sterilizer. (external indicator tape, labels, or paper strips and internal indicator/integrator) Biologic indicators- a preparation of living spores that are resistant to the sterilizing agent. Bacterial spores used in biologic control tests: Bacillus stearothermophilus at 131 to 140 (55 to 60 ) tests steam under pressure daily and with each load of implantables. Bacillus subtilis at 95 to 98.6 (35-37 ) tests dry heat and ethylene oxide with every load. B. subtilis testing is performed daily for lower temperature hydrogen peroxide plasma Peracetic acid sterilizers are tested according to the manufacturers recommendations. B. stearothermophilus-bound enzyme- a rapid read-out biologic indicator specifically for monitoring a high-speed pressure steam sterilizer with a gravity displacement cycle based on fluorometric detection.
Steps for assembling instrument sets 1. Make sure the instruments are thoroughly dry. 2. Unless contraindicated, place an absorbent towel or foam in the bottom of the tray to absorb condensate. 3. Count instruments as they are placed in the tray, and record the number of each type. 4. Arrange the instruments in a definite pattern to protect them from damage and to facilitate their removal for counting and use. 5. Place heavy instruments in the bottom of the tray. 6. Open the hinges and box locks on all hinged instruments. 7. Place ring-handled instruments on stringers or holders designed for this purpose. 8. Place sharp and delicate instruments on top of other instruments. 9. Place concave or cup instruments with the cupped surfaces down so that water condensate does not collect in them during sterilization and drying. 10. Disassemble all detachable parts. 11. Separate dissimilar metals. 12. Place instruments with a lumen in as near horizontal position as possible. 13. Distribute weight as evenly as possible in the tray. 14. Wrap the tray, or place it in a rigid container. 15. Place a chemical sterilization indicator on the outside wrapper or container. 16. Label sets appropriately with their intended use, the date sterilized and the control number. Packaging Instruments and Other Items for Sterilization
Packaging considerations: Permit penetration of the sterilizing agent to achieve sterilization of all items in the package. Allow the release of sterilizing agent at the end of the exposure period and allow adequate drying or aerating. Withstand the physical conditions of sterilizing process. Maintain integrity of the package at varying atmospheric and humidity levels. Provide an impermeable barrier to microorganisms, dust particles, and moisture after sterilization. Cover items completely and easily and fasten securely with tape or a heat seal that cannot be resealed after opening. Resist tears and punctures in handling Permit identification of the contents and evidence of exposure to a sterilizing agent. Be free of toxic ingredients and nonfast dyes. Be lint-free or low-linting Protect the contents from physical damage Permit easy removal of the contents with transfer to the sterile field without contamination or delamination Be economical
Types of wrapping
Sequential wrapping with two wrappers Single wrap
Methods of wrapping Square fold Envelope fold
Packaging materials and methods Woven fabrics (muslin or linens) -this type of fabric is not moisture-resistant and is used in a double thickness. -this wrapper should withstand between 50-75 launderings before becoming too worn to be a microbial barrier -Should be stored at a room temperature of 18-22 and in a relative humidity of 3570%. Nonwoven fabrics -combination of cellulose and rayon with strands of nylon randomly oriented through it, or other natural and synthetic fibers bonded by a method other than weaving. -these fabrics have the flexibility and handling qualities of woven materials and are available in several weights. -provide excellent barrier against microorganisms and moisture during storage after sterilization. They are disposable and virtually lint-free. Peel packs or pouches -made of a combination of paper on one side and clear plastic film on the other. -are satisfactory for wrapping single instruments, odd-shaped items, and small items. Sealants and labeling -chemical indicator tape, steam-sensitive tape, gas-sensitive tape Wrapped trays Rigid closed containers Specialized tray sets -a fitted case or rack for a set of instruments or implants to help protect the instruments and keep them separated for sterilization and use.
METHODS OF STERILIZATION 1. Thermal sterilization Steam under pressure (moist heat sterilization) -moist heat in the form of steam under pressure causes the denaturation and coagulation of protein or the enzyme-protein system within cells. -most microorganisms at their vegetative forms are killed in a few minutes at temp 54-65 ; however certain bacterial spores will withstand at a temp of 115 for more than 3 hrs. No living thing can survive direct exposure to saturated steam at 121 for longer than 15 minutes. -prions such as Creutzfeldt-Jacob disease are infectious protein material and must be steam-sterilized for a minimum of 1 hr at 132 after soaking in sodium hydroxide at room temp for 1 hr. Advantages: a. Easiest, safest, and surest method of on-site sterilization b. Fastest method c. Least expensive and most easily supplied agent d. Most sterilizers have automatic controls and recording devices e. Steam leaves no harmful residue Disadvantages: a. Precautions must be used in preparing and packaging items, loading and operating the sterilizer, and drying the load. b. Items need to be clean, free of grease and oil, and not sensitive to heat. c. Steam must have direct contact with all areas of an item. d. Timing adjustments are variables of human error. e. Steam may not be pure. Types of steam sterilizers a. Gravity displacement sterilizer b. Prevacuum sterilizer c. Flash/high-speed pressure sterilizer Dry heat sterilization -used primarily to sterilize anhydrous oils, petroleum products and talc, which steam and ethylene oxide gas cannot penetrate. Advantages: a. Hot air penetrates substances that cannot be sterilized by steam or another method b. Dry heat is a protective method of sterilizing some delicate, sharp, or cuttingedge instruments Disadvantages: a. A long exposure period is required b. Time and temperature required will vary for different substances
c. Overexposure may ruin some substances Types of dry heat sterilizers a. Mechanical convection oven b. Gravity convection oven Packaging materials: a. Glass b. Stainless steel boats or trays c. Aluminum foil d. Woven fabric or peel pouches 2. Chemical sterilization Ethylene oxide gas sterilization -used to sterilize items that are sensitive to heat or moisture. -EO is a chemical alkylating agent that kills microorganisms by interfering with the normal metabolism of protein and reproductive processes, resulting in cell death. -highly flammable and explosive in air -Toxic emissions and residue present health hazards -Parameters: concentration, temperature, humidity, time. Advantages: a. Effective substitute agent to use with most items that cannot be sterilized by heat. b. Noncorrosive and does not damage items c. Completely permeates all porous materials; does not penetrate metal, glass, petroleum-based lubricants d. Automatic controls preclude human error e. Leaves no film on items Disadvantages: a. b. c. d. Complicated process that is carefully monitored A long, slow process Requires special, expensive equipment Toxic by-products can be formed in the presence of moisture droplets during exposure of some plastics e. A vesicant when in contact with skin and mucous membranes f. Overexposure causes nasal and throat irritation g. Carcinogenic in long-term exposure Hydrogen peroxide plasma sterilization -hydrogen peroxide can be activated to create reactive plasma. -free radicals of the hydrogen peroxide in the cloud interact with cell membranes, enzymes, and nucleic acids to disrupt the life functions of microorganisms. Advantages: a. Dry and nontoxic
b. By-products of O2 and water vapor are safely evacuated into the room atmosphere c. Aeration is not necessary d. Low-temperature allows safe sterilization of heat-sensitive items e. Plasma has significantly less effect on metal than does steam sterilization f. Sterilizer is simple in design and connects to standard electrical outlets Disadvantages: a. Metal trays block radiofrequency waves b. Not compatible with cellulose c. Nylon becomes brittle after repeated exposure d. Not approved in US for use with endoscopic lumens Ozone gas sterilization -ozone sterilizes by oxidation, a process that destroys organic and inorganic matter. It penetrates the membrane of cells, causing them to explode. -a low temp method of sterilization Advantages: a. Sterilizer generates its own agent. It is simple and inexpensive to operate. b. Provides alternative to EO gas sterilization c. Does not affect titanium, chromium, silicone, neophene, and Teflon. d. Aeration is not necessary e. Low temp Disadvantages: a. Can be corrosive; oxidizes steel, aluminum, copper, iron, brass. b. Destroys natural rubber Chemical sterilants in solution Advantages: a. Solution has a low surface tension; penetrates into crevices and is readily rinsed from items. b. Noncorrosive, nonstaining, and safe for instruments that can be immersed in a chemical solution c. Does not damage lenses, or cement on lensed endoscopes d. Not absorbed by rubber or plastics e. Has low volatility and stable Disadvantages: a. b. c. d. Prolonged exposure may be necessary Some have hazardous effects associated with exposure Items must be thoroughly rinsed in sterile distilled water before use Failure to adequately rinse an endoscope may cause chemically induced colitis e. Sterile transfer is difficult f. Items cant be held in long term storage g. Solution can become diluted during use
Types of chemical sterilant: a. Acetic acid- kills microorganisms by a process of oxidation to denature proteins. Process takes 20 minutes at room temperature of 25 . b. Formaldehyde- 37% aqueous solution (formalin) or 8% formaldehyde in 70% isopropyl alcohol kills m.o. by coagulating protein in the cells. At room temp. Has pungent odor and irritating to the eyes and nasal passages. Its vapors can be toxic. c. Glutaraldehyde- kills mo.o by denaturation of protein in cells. d. Peracetic acid- inactivates critical microbial systems e. Hypochlorus acid- derived from electrochemical activation of brine solution 3. Radiation sterilization Microwave sterilization - The nonionizing radiation of microwaves produces hyperthermic conditions that disrupt life processes. - Uses low-pressure steam with the nonionizing radiation to produce the localized heat that kills microorganisms. Gamma ray and beta particle sterilization -Cobalt-60 is a radioactive isotope capable of disintegrating to produce gamma rays and is the most commonly used source for irradiation sterilization -is commonly used for commercially prepared single-use disposable items such as catheters, syringes, IV sets, and gloves.
Vous aimerez peut-être aussi
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeD'EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeÉvaluation : 4 sur 5 étoiles4/5 (5794)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreD'EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreÉvaluation : 4 sur 5 étoiles4/5 (1090)
- Never Split the Difference: Negotiating As If Your Life Depended On ItD'EverandNever Split the Difference: Negotiating As If Your Life Depended On ItÉvaluation : 4.5 sur 5 étoiles4.5/5 (838)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceD'EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceÉvaluation : 4 sur 5 étoiles4/5 (894)
- Grit: The Power of Passion and PerseveranceD'EverandGrit: The Power of Passion and PerseveranceÉvaluation : 4 sur 5 étoiles4/5 (587)
- Shoe Dog: A Memoir by the Creator of NikeD'EverandShoe Dog: A Memoir by the Creator of NikeÉvaluation : 4.5 sur 5 étoiles4.5/5 (537)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureD'EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureÉvaluation : 4.5 sur 5 étoiles4.5/5 (474)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersD'EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersÉvaluation : 4.5 sur 5 étoiles4.5/5 (344)
- Her Body and Other Parties: StoriesD'EverandHer Body and Other Parties: StoriesÉvaluation : 4 sur 5 étoiles4/5 (821)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)D'EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Évaluation : 4.5 sur 5 étoiles4.5/5 (119)
- The Emperor of All Maladies: A Biography of CancerD'EverandThe Emperor of All Maladies: A Biography of CancerÉvaluation : 4.5 sur 5 étoiles4.5/5 (271)
- The Little Book of Hygge: Danish Secrets to Happy LivingD'EverandThe Little Book of Hygge: Danish Secrets to Happy LivingÉvaluation : 3.5 sur 5 étoiles3.5/5 (399)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyD'EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyÉvaluation : 3.5 sur 5 étoiles3.5/5 (2219)
- The Yellow House: A Memoir (2019 National Book Award Winner)D'EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Évaluation : 4 sur 5 étoiles4/5 (98)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaD'EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaÉvaluation : 4.5 sur 5 étoiles4.5/5 (265)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryD'EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryÉvaluation : 3.5 sur 5 étoiles3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnD'EverandTeam of Rivals: The Political Genius of Abraham LincolnÉvaluation : 4.5 sur 5 étoiles4.5/5 (234)
- On Fire: The (Burning) Case for a Green New DealD'EverandOn Fire: The (Burning) Case for a Green New DealÉvaluation : 4 sur 5 étoiles4/5 (73)
- The Unwinding: An Inner History of the New AmericaD'EverandThe Unwinding: An Inner History of the New AmericaÉvaluation : 4 sur 5 étoiles4/5 (45)
- ChemDocument2 pagesChemBaliuag Guia100% (4)
- Tigers Binocular Vision Enables Depth PerceptionDocument5 pagesTigers Binocular Vision Enables Depth PerceptionpaidalaPas encore d'évaluation
- CBR Lab Report: Soil Subgrade TestingDocument4 pagesCBR Lab Report: Soil Subgrade Testingsdcsdcdcw33% (3)
- Anatomy and Physiology of The BreastDocument42 pagesAnatomy and Physiology of The BreastNicole SooPas encore d'évaluation
- Kidney CancerDocument5 pagesKidney CancerNicole SooPas encore d'évaluation
- Clopidogrel Drug StudyDocument1 pageClopidogrel Drug StudyNicole Soo89% (9)
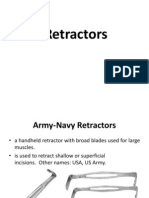
- RetractorsDocument18 pagesRetractorsNicole SooPas encore d'évaluation
- Name of Drug General Action Specific Action Indications Contraindications Adverse Reaction Nursing ResponsibilitiesDocument1 pageName of Drug General Action Specific Action Indications Contraindications Adverse Reaction Nursing ResponsibilitiesNicole SooPas encore d'évaluation
- Modified surgical positions and skin preparationDocument7 pagesModified surgical positions and skin preparationNicole Soo100% (1)
- Name of Drug General Action Specific Action Indications Contraindications Adverse Reaction Nursing ResponsibilitiesDocument1 pageName of Drug General Action Specific Action Indications Contraindications Adverse Reaction Nursing ResponsibilitiesNicole SooPas encore d'évaluation
- Specialized Surgical EquipmentDocument73 pagesSpecialized Surgical EquipmentNicole Soo50% (2)
- Surgical InstrumentationDocument93 pagesSurgical InstrumentationNicole SooPas encore d'évaluation
- Dopamine Drug StudyDocument3 pagesDopamine Drug StudyNicole Soo78% (9)
- Surgical InstrumentationDocument93 pagesSurgical InstrumentationNicole SooPas encore d'évaluation
- Pharma PORCILDocument4 pagesPharma PORCILNicole SooPas encore d'évaluation
- XI Maths - I Terminal ExamDocument2 pagesXI Maths - I Terminal ExamPurisai Rajamani KumarPas encore d'évaluation
- HW2 Solutions FinalDocument5 pagesHW2 Solutions Finalpande_100Pas encore d'évaluation
- Metrology AssignmentDocument31 pagesMetrology AssignmentKailas Sree Chandran100% (1)
- WISDM-dataset-description 2Document5 pagesWISDM-dataset-description 2yuliasihkripsianditaPas encore d'évaluation
- DMCR Detection Measurement Control RelayDocument5 pagesDMCR Detection Measurement Control RelayMuhammad AbuzarPas encore d'évaluation
- Conversion RPM G CentrifugaDocument1 pageConversion RPM G CentrifugaEsaú E RodriguezPas encore d'évaluation
- Fluid MechanicsDocument29 pagesFluid Mechanicsaminur3rahman-1Pas encore d'évaluation
- Electrical and Optical Properties of Indium-Tin Oxide (ITO) Films by Ion-Assisted Deposition (IAD) at Room TemperatureDocument6 pagesElectrical and Optical Properties of Indium-Tin Oxide (ITO) Films by Ion-Assisted Deposition (IAD) at Room Temperaturereza mirzakhaniPas encore d'évaluation
- Measuring Elastic Modulus of Beams Using Deflection MethodDocument14 pagesMeasuring Elastic Modulus of Beams Using Deflection MethodHaziq PazliPas encore d'évaluation
- ME 555 Stress Analysis Unit 4Document57 pagesME 555 Stress Analysis Unit 4TheoPas encore d'évaluation
- Ferroresonance During Single-Phase Switching of Distribution TransformersDocument6 pagesFerroresonance During Single-Phase Switching of Distribution TransformersDiego Betancourt MejiaPas encore d'évaluation
- 4-1 r14Document12 pages4-1 r14hafizgPas encore d'évaluation
- CHY382-01 Ester Hydrolysis Lab ReportDocument5 pagesCHY382-01 Ester Hydrolysis Lab ReportJoshua AunPas encore d'évaluation
- The Statistical Imagination: Chapter 7. Using Probability Theory To Produce Sampling DistributionsDocument18 pagesThe Statistical Imagination: Chapter 7. Using Probability Theory To Produce Sampling DistributionsVictoria LiendoPas encore d'évaluation
- Design Considerations of High Voltage AnDocument114 pagesDesign Considerations of High Voltage AnEL BRIGHLIPas encore d'évaluation
- Glazed Aluminum Curtain Walls (Thermawall SM 2600)Document12 pagesGlazed Aluminum Curtain Walls (Thermawall SM 2600)RsjBugtongPas encore d'évaluation
- Acceleration (Inclined Plane)Document5 pagesAcceleration (Inclined Plane)jambunaPas encore d'évaluation
- LM 08Document38 pagesLM 08Tôi Là Đăng TèoPas encore d'évaluation
- Calculating Energy: Complete These Questions in Your Exercise Books, With Full ESTAU Working OutDocument2 pagesCalculating Energy: Complete These Questions in Your Exercise Books, With Full ESTAU Working Outruby lillyPas encore d'évaluation
- Hooke's Law and Property of MaterialsnotesDocument5 pagesHooke's Law and Property of MaterialsnotesPrithu PareekPas encore d'évaluation
- FDG Production-Theory Operations-FDG Synthesis Chemistr1Document25 pagesFDG Production-Theory Operations-FDG Synthesis Chemistr1Cesar Adolfo SanchezPas encore d'évaluation
- Irjet V5i5256 PDFDocument5 pagesIrjet V5i5256 PDFMuhsinaPas encore d'évaluation
- Alpha 900 and HD LineDocument32 pagesAlpha 900 and HD Linebertan dağıstanlıPas encore d'évaluation
- 11 TransportationDocument61 pages11 TransportationWindi Astuti0% (1)
- Overview Aerodynamics 2017Document10 pagesOverview Aerodynamics 2017marcoPas encore d'évaluation
- Trư NG Thcs : Question IV. Find and Correct The Mistake in Each Sentence. (1p)Document2 pagesTrư NG Thcs : Question IV. Find and Correct The Mistake in Each Sentence. (1p)Anh ThưPas encore d'évaluation