Académique Documents
Professionnel Documents
Culture Documents
Med Castino
Transféré par
kristel_nicole18yahoCopyright
Formats disponibles
Partager ce document
Partager ou intégrer le document
Avez-vous trouvé ce document utile ?
Ce contenu est-il inapproprié ?
Signaler ce documentDroits d'auteur :
Formats disponibles
Med Castino
Transféré par
kristel_nicole18yahoDroits d'auteur :
Formats disponibles
Cecile Malasig 2014 B Date of Admission: February 9, 2013 Date of Interview: February 19, 2013
Patient Profile MC is a 35 year-old female Filipino Catholic who currently lives in Tatalon. She was born on October 3, 1975 in Bohol. Her first admission was on December 26, 2012 at UERM Hospital due to haemolytic anemia. This is her second admission. Marital Status The patient is married and she has a 6 year-old daughter. Social Hisotry The patient does not smoke and drink alcoholic beverage. She is frequently exposed to cigarette smoke. Maintenance Medicine Multivitamins, prednisone, and other unrecalled medicines for blood. Source and reliability The source of information is the patient. With fair reliability. Chief Complaint Vomiting and diarrhea of few hours duration History of Present Illness A known haemolytic anemic patient came in with a chief complaint of vomiting and diarrhea associated with epigastric pain of 2/10 pain intensity, weakness, easy fatigability, dizziness, pallor, jaundice and tea-color urine. Few hours prior to admission, the patient developed a sudden onset of vomiting, epigastric pain of 2/10 intensity and diarrhea. Her vomitous consisted of previously ingested food. She had 3-4 episodes of watery stools with no blood, no mucous, and no fishy odor. This was associated with weakness, easy fatigability, pallor, dizsziness, tea-color urine ad jaundice. She was then rushed to UERM Hospital and was subsequently admitted. The patient denies the presence of fever and chest pains. The patient has been having intermittent episodes of tea-color urine associated with jaundice, pallor and weakness since 2010 She was diagnosed with haemolytic anemia on December 26, 2012 and has been taking prednisone for 1 month. It is her first time to have vomiting and diarrhea in the course of her illness. Temporal Profile
Past Medical History The patient had intermittent bouts of tea-color urine associated with jaundice, flank pain, burning sensation upon urination, pallor and weakness since 2010. During the first episode, she was diagnosed with UTI and was prescribed with cotrimoxazole. She was also transfused with 4 bags of blood since her haemoglobin was low. This gave relief to the symptoms. Symptoms recurred 3 months later and she was again transfused with 3 bags of blood. Symptoms recurred intermittently the subsequent months but the patient never went back for check up. There were no triggering factors for the signs and symptoms noted. On 2011, she developed bipedal edema, palpitations easy faigability with shortness of breath along with the aforementioned symptoms. These also occurred intermittently but she did not seek for medical attention since these did not affect her level of activity. On December 26, 2012 she was brought to UERM ER and was admitted due to worsening of body weakness associated with jaundice, pallor and tea-color urine. She underwent urinalysis, CBC and chest x-ray. According to the patient, her chest-xray findings showed fluid in her lungs. CBC results showed a low haemoglobin. Result for urinalysis was unrecalled. The patient has no past accidents and surgeries. She denies past infections, illnesses and admissions. She has a right cataract which was diagnosed on 2012. She also has intermittent cough since 2010 and was prescribed with co-amoxiclav. Family History The patient is the sixth child among 9 children. She denies history of heart disease, cancer, blood disease, asthma, allergies, hypertension and diabetes mellitus. She has a 6-year-old daughter who has no illnesses. Review of Systems: The patient experienced fever, chills, weakness, pallor, easy fatigability, and jaundice associated with teacolor urine. She experienced shortness of breath, palpitations, and bipedal edema later on. There were no changes in her bowel habits and stool characteristics. There was no change in the amount of her urine. She did not have generalized edema and periorbital edema. She has blurring of vision due to her cataract. Physical Eaxam General: The patient is sitting on the chair, calm and cooperative with endomorph built. Her grooming is fairn. She is not in pain and not in cardiorespiratory distress. Vital Signs: RR: 21 breaths/min PR: 80breaths/min Normothermic Skin: Skin is pale and moist with good turgor. Her nailbeds are also pale. Hematomas are noted at the site of previous IV insertion at the left hand and left foot. There are normal skin appendages. No rashes seen. Head: Head is atraumatic. Her hair has normal texture and is evenly distributed. She has a moon facie. Eyes: Both eyes have ROR. Both lenses were thick and slightly opaque. There were no discharge seen. Her palpebral conjunctiva is pale. Her sclerae is white. Ears: no redness, no discharge, with cerumen, good cone of light bilaterally Neck: no lymphadenopathies, no masses palpated Throat/mouth: pink oral mucosae, with dental carries, no redness and exudates seen Chest/lung: symmetrical, no tenderness, resonant upon percussion, normal breath sounds Breast: no masses palpated CVS: regular heart rhythm. Clear s1 and s2. Systolic murmur heard at pulmonic area. PMI at 5th ICS LMCL.
Adynamic precordium Abdomen: Globular and protruding. Normal bowel sounds heard at 13/min. No tenderness. No fluid wave Peripheral Vascular: +2 pulses on all extremities, normal skin appedages, pale nailbeds, no jaundice. Left arm is swollen due to phlebitis. With bipedal pitting edema, +3. Muskuloskeletal: no deformities, no injuries, full ROM, thin extremities except for left arm and both legs (from ankle below) Endocrine: with moon facies, buffalo hump and central obesity Neurologic exam: oriented and responsive, intact motor function, no neurologic deficits seen. No neck rigidity. Intact coordination. SOAP Note Subjective: On prednisone therapy for 1 month Sudden onset of epigastric pain, vomiting, and diarrhea associated with tea-color urie, jaundice, pallor, and generalized body weakness Denies eating suspicious food Past history: o Had intermittent episodes of tea-color urine associated with jaundice, fever, flank pain, pallor, and generalized weakness o Subsequently developed intermittent easy fatigability, palpitations when lying down, and bipedal edema when the above signs and symptoms occur o Diagnosed of haemolytic anemia on December 26, 2012 o Chest x-ray showed fluid in her lungs o No chest pains o Denies intake of any medicines (pharmaceutical, herbal, vitamins) prior to onset of illness o Denies previous infections prior to onset of illness o Denies the appearance of rashes Objective: Not in cardiorespiratory distress Slightly tachypneic at 21 breaths/min Moon facies, buffalo hump, and central obesity Pale skin, nail beds, and palpebral conjunctiva Anicteric sclera, no jaundice discoloration of skin With a systolic heart murmur PMI is normal with an adynamic precordium, heart rhythm is regular Bipedal +3 pitting edema Unremarkable HEENT, chest, abdominal, and neurologic findings Assessment: The patients sudden onset of epigastric pain, vomiting, and diarrhea may be due to the prolonged use of prednisone. Prednisone is a corticosteroid which depresses the immune system. This makes the patient immunocompromized and vulnerable to any type of infection. Prednisone also inhibits the formation of mucous in the stomach which can lead to gastritis. This presents with epigastric pain and vomiting. This leads me to an impression of gastroenteritis secondary to prolonged prednisone use. Among immunocompromised patients, the
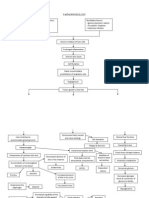
most common etiology for gastroenteritis is viral. For this patient, her diarrhea and vomiting could be due to a viral gastroenteritis. A possible gastritis can be secondary to prolonged prednisone use. Reviewing the past history of illness of the patient, we can see that the patient is suffering from anemia for almost 3 years. Her anemia is associated with intermittent jaundice, tea-color urine, flank pain, fever, and pallor which occurred spontaneously with no triggering factors appreciated. Anemia with jaundice and tea-color urine points to a haemolytic disease. There were no triggering factors appreciated in the onset of the patients hemolysis as far as the history is concerned. This leads me to an impression of a Primary or Idiopathic Autoimmune Hemolytic Anemia (AIHA). It is a rare disease which commonly affects adults of 40 years of age and above. In AIHA, there is an increased destruction of erythrocytes due to the presence of anti-erythrocyte autoantibodies (AEA). AEA are classified as cold or warm autoantibodies, as they react optimally at temperatures below 30C or at 35C to 40C respectively. The onset of AIHA is often abrupt. The haemoglobin level drops and the massive red cell destruction will produce jaundice, tea-color urine and often leads to an enlarged spleen. The diagnosis of AIHA must meet two criteria: Evidence of Hemolysis (anemia plus elevated reticulocyte count in the absence of blood loss) Evidence of RBC autoantibodies/complement, which is usually indicated by a positive Direct Coombs test Differential Diagnosis: 1. Thalassemia This also presents with hemolysis, jaundice, anemia and tea-color urine. Since this is genetic, it should have been appreciated during childhood. However, there are some forms of acquired thalassemia. But this is usually a manifestation of an underlying disease, specifically hematologic malignancy. There should be supporting symptoms pointing to malignancy prior to onset of hemolysis. Therefore this is not primarily considered. 2. Chronic Viral Hepatitis This presents with jaundice along with fever, anorexia and vomiting. Viral hepatitis can also lead to AIHA. The existence of hepatitis in the patient is still in question. Although the elicited past medical history is unremarkable for hepatitis, this disease cannot be ruled since some forms of hepatitis are subclinical and mild which can be easily neglected by the patient. Certain test must be done to confirm its existence. 3. IgA Nephropathy This presents with intermittent hematuria. However, this disease does not cause hemolysis and it is mild. Therefore it is ruled out. Plan: Diagnostic workup 1. CBC 2. Red Cell Index 3. Peripheral Smear 4. Urinalysis 5. Direct Coombs test 6. Serum bilirubin 7. LDH 8. Haptoglobulin levels 9. Hepa A IgG 10. HBsAg, anti-HBc IgG, anti-HBs 11. anti-HCV Treatment: 1. Blood transfusion for severe anemia st 2. 1 line treatment: Glucocorticoids (prednisone 1mg/kg/day) 3. For relapse: long-term immunosypresion with low dose prednisone, azathioprine or cyclosporine 4. For chronic AIHA, splenectomy may be indicated
Vous aimerez peut-être aussi
- The Yellow House: A Memoir (2019 National Book Award Winner)D'EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Évaluation : 4 sur 5 étoiles4/5 (98)
- Drug Name Mechanism of Action Indication Contraindication Side Effects/Adverse Reaction Nursing Responsibility CNS-malaiseDocument3 pagesDrug Name Mechanism of Action Indication Contraindication Side Effects/Adverse Reaction Nursing Responsibility CNS-malaisekristel_nicole18yahoPas encore d'évaluation
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeD'EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeÉvaluation : 4 sur 5 étoiles4/5 (5795)
- Diagram I Pathogenesis of Insulin Dependent DM (Type 1) : DiagramsDocument2 pagesDiagram I Pathogenesis of Insulin Dependent DM (Type 1) : Diagramskristel_nicole18yahoPas encore d'évaluation
- Shoe Dog: A Memoir by the Creator of NikeD'EverandShoe Dog: A Memoir by the Creator of NikeÉvaluation : 4.5 sur 5 étoiles4.5/5 (537)
- Middle Adulthood (40 To 65 Years)Document1 pageMiddle Adulthood (40 To 65 Years)kristel_nicole18yahoPas encore d'évaluation
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureD'EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureÉvaluation : 4.5 sur 5 étoiles4.5/5 (474)
- Monday, Tuesday, Thursday & Friday: St. Pio of Pietrelcina ChapelDocument2 pagesMonday, Tuesday, Thursday & Friday: St. Pio of Pietrelcina Chapelkristel_nicole18yahoPas encore d'évaluation
- Grit: The Power of Passion and PerseveranceD'EverandGrit: The Power of Passion and PerseveranceÉvaluation : 4 sur 5 étoiles4/5 (588)
- Chemistry Date: 04/29/14: Developed or Changed The Ranges From Her Chemistry LabDocument1 pageChemistry Date: 04/29/14: Developed or Changed The Ranges From Her Chemistry Labkristel_nicole18yahoPas encore d'évaluation
- On Fire: The (Burning) Case for a Green New DealD'EverandOn Fire: The (Burning) Case for a Green New DealÉvaluation : 4 sur 5 étoiles4/5 (74)
- Nursing Care Process: University of The East Ramon MagsaysayDocument5 pagesNursing Care Process: University of The East Ramon Magsaysaykristel_nicole18yahoPas encore d'évaluation
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryD'EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryÉvaluation : 3.5 sur 5 étoiles3.5/5 (231)
- Assessment Diagnosis Rationale Planning Implementation Rationale EvaluationDocument2 pagesAssessment Diagnosis Rationale Planning Implementation Rationale Evaluationkristel_nicole18yahoPas encore d'évaluation
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceD'EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceÉvaluation : 4 sur 5 étoiles4/5 (895)
- 3rd NCP Risk For ConstipationDocument2 pages3rd NCP Risk For Constipationkristel_nicole18yaho100% (3)
- Never Split the Difference: Negotiating As If Your Life Depended On ItD'EverandNever Split the Difference: Negotiating As If Your Life Depended On ItÉvaluation : 4.5 sur 5 étoiles4.5/5 (838)
- Hinds & Gattuso, 1999Document1 pageHinds & Gattuso, 1999kristel_nicole18yahoPas encore d'évaluation
- The Little Book of Hygge: Danish Secrets to Happy LivingD'EverandThe Little Book of Hygge: Danish Secrets to Happy LivingÉvaluation : 3.5 sur 5 étoiles3.5/5 (400)
- Clinical Teaching Behavior Student'S Learning Response: Conceptual FrameworkDocument5 pagesClinical Teaching Behavior Student'S Learning Response: Conceptual Frameworkkristel_nicole18yahoPas encore d'évaluation
- Pathophysiology of Spinal Cord Injury 1Document1 pagePathophysiology of Spinal Cord Injury 1kristel_nicole18yaho60% (5)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersD'EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersÉvaluation : 4.5 sur 5 étoiles4.5/5 (345)
- Assessment Diagnosis Rationale Planning Implementation Rationale EvaluationDocument2 pagesAssessment Diagnosis Rationale Planning Implementation Rationale Evaluationkristel_nicole18yahoPas encore d'évaluation
- Predisposing Factors Precipitating FactorsDocument1 pagePredisposing Factors Precipitating Factorskristel_nicole18yahoPas encore d'évaluation
- The Unwinding: An Inner History of the New AmericaD'EverandThe Unwinding: An Inner History of the New AmericaÉvaluation : 4 sur 5 étoiles4/5 (45)
- Past Health History Medward3Document1 pagePast Health History Medward3kristel_nicole18yahoPas encore d'évaluation
- Team of Rivals: The Political Genius of Abraham LincolnD'EverandTeam of Rivals: The Political Genius of Abraham LincolnÉvaluation : 4.5 sur 5 étoiles4.5/5 (234)
- Evidence-Based Practice: Acute Upper Gastrointestinal Bleeding: ManagementDocument3 pagesEvidence-Based Practice: Acute Upper Gastrointestinal Bleeding: Managementkristel_nicole18yahoPas encore d'évaluation
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyD'EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyÉvaluation : 3.5 sur 5 étoiles3.5/5 (2259)
- Family Nursing Care Plan. 1st and 2nd Level AssessmentDocument7 pagesFamily Nursing Care Plan. 1st and 2nd Level Assessmentkristel_nicole18yaho100% (1)
- Childlessness Is Defined As The Condition of Being Without ChildrenDocument2 pagesChildlessness Is Defined As The Condition of Being Without Childrenkristel_nicole18yahoPas encore d'évaluation
- Case Study: Post-Cesarian Section: University of The EastDocument3 pagesCase Study: Post-Cesarian Section: University of The Eastkristel_nicole18yahoPas encore d'évaluation
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaD'EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaÉvaluation : 4.5 sur 5 étoiles4.5/5 (266)
- PathophysiologyDocument2 pagesPathophysiologykristel_nicole18yahoPas encore d'évaluation
- The Emperor of All Maladies: A Biography of CancerD'EverandThe Emperor of All Maladies: A Biography of CancerÉvaluation : 4.5 sur 5 étoiles4.5/5 (271)
- Mobile Health Clinic InitiativeDocument47 pagesMobile Health Clinic InitiativededdyPas encore d'évaluation
- h2s Hand BookDocument34 pagesh2s Hand BookJorge Eliecer Ferro Cotes100% (4)
- Material Safety Data Sheet: Liquefied Petroleum GasDocument1 pageMaterial Safety Data Sheet: Liquefied Petroleum GasardhanhendroPas encore d'évaluation
- Activity 1: Write Your Answer On The Space ProvidedDocument4 pagesActivity 1: Write Your Answer On The Space ProvidedEki OmallaoPas encore d'évaluation
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreD'EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreÉvaluation : 4 sur 5 étoiles4/5 (1090)
- Nov 19 INTEGUMENTARY-INFLAMMATORY-DISORDERS-for-presentation-2022Document79 pagesNov 19 INTEGUMENTARY-INFLAMMATORY-DISORDERS-for-presentation-2022Jean Gwyneth GatchalianPas encore d'évaluation
- Jurnal ParuDocument31 pagesJurnal Parudr. syah sembung wasisoPas encore d'évaluation
- Qand ADocument5 pagesQand AJoshua PascasioPas encore d'évaluation
- Araldite - GT7074Document2 pagesAraldite - GT7074maz234Pas encore d'évaluation
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)D'EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Évaluation : 4.5 sur 5 étoiles4.5/5 (121)
- 7 Contoh Analytical Exposition Pendek Bahasa InggrisDocument6 pages7 Contoh Analytical Exposition Pendek Bahasa InggrisDarsi YujiwatiPas encore d'évaluation
- Medicine Supplies & First Aid Treatment LogsheetDocument4 pagesMedicine Supplies & First Aid Treatment LogsheetMark BuendiaPas encore d'évaluation
- Final Stock ReportDocument63 pagesFinal Stock ReportKarthik SunnyPas encore d'évaluation
- Adoption LawsDocument10 pagesAdoption LawsAneesh PandeyPas encore d'évaluation
- Definition of Physical EducationDocument7 pagesDefinition of Physical EducationRose Jane BangisPas encore d'évaluation
- Synopsis - Anu Varghese and Dr. M H Salim, 2015 - Handloom Industry in Kerala A Study of The Problems and ChallengesDocument8 pagesSynopsis - Anu Varghese and Dr. M H Salim, 2015 - Handloom Industry in Kerala A Study of The Problems and ChallengesNandhini IshvariyaPas encore d'évaluation
- PNF 8th EditionDocument7 pagesPNF 8th EditionDanisaWajePas encore d'évaluation
- MSDS Phthalic AnhydrideDocument6 pagesMSDS Phthalic AnhydrideBansi TumbadiaPas encore d'évaluation
- SAFed Tests PDFDocument88 pagesSAFed Tests PDFDanPas encore d'évaluation
- Rules Related Statutes All CodesDocument150 pagesRules Related Statutes All CodesRod SatrePas encore d'évaluation
- Her Body and Other Parties: StoriesD'EverandHer Body and Other Parties: StoriesÉvaluation : 4 sur 5 étoiles4/5 (821)
- Sex Should Be Taught in Schools: Shafira Anindya Maharani X IPS 1 /29Document11 pagesSex Should Be Taught in Schools: Shafira Anindya Maharani X IPS 1 /29Shafira Anindya MaharaniPas encore d'évaluation
- MSDS Baybl T65 901510Document8 pagesMSDS Baybl T65 901510gnavarroPas encore d'évaluation
- A Study On Pandemic Related Challenges Faced in Rural Areas: Patel Preja ID No: 20BBA125Document9 pagesA Study On Pandemic Related Challenges Faced in Rural Areas: Patel Preja ID No: 20BBA125PREJA PATELPas encore d'évaluation
- HEALTH-TEACHING-PLAN sUGATON EVALDocument9 pagesHEALTH-TEACHING-PLAN sUGATON EVALPrincess Faniega SugatonPas encore d'évaluation
- 04fc75de986c12 Pharmaceutics-I AROMATIC WATERSDocument14 pages04fc75de986c12 Pharmaceutics-I AROMATIC WATERSsultanPas encore d'évaluation
- Vieillard-Baron2018 Article DiagnosticWorkupEtiologiesAndMDocument17 pagesVieillard-Baron2018 Article DiagnosticWorkupEtiologiesAndMFranciscoPas encore d'évaluation
- Activity 2: General Biology 2 (Quarter IV-Week 3)Document4 pagesActivity 2: General Biology 2 (Quarter IV-Week 3)KatsumiJ AkiPas encore d'évaluation
- EdCaN Specialty Module 4Document23 pagesEdCaN Specialty Module 4cindy8127Pas encore d'évaluation
- Body GuideDocument46 pagesBody GuideBárbara Leite95% (22)
- Corpus Alienum PneumothoraxDocument3 pagesCorpus Alienum PneumothoraxPratita Jati PermatasariPas encore d'évaluation
- Pelvic Fracture Case StudyDocument48 pagesPelvic Fracture Case StudyYves BasanPas encore d'évaluation
- Tsoukaki 2012Document8 pagesTsoukaki 2012Marina JoelPas encore d'évaluation
- Love Life: How to Raise Your Standards, Find Your Person, and Live Happily (No Matter What)D'EverandLove Life: How to Raise Your Standards, Find Your Person, and Live Happily (No Matter What)Évaluation : 3 sur 5 étoiles3/5 (1)
- Summary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedD'EverandSummary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedÉvaluation : 4.5 sur 5 étoiles4.5/5 (82)
- The Age of Magical Overthinking: Notes on Modern IrrationalityD'EverandThe Age of Magical Overthinking: Notes on Modern IrrationalityÉvaluation : 4 sur 5 étoiles4/5 (32)