Académique Documents
Professionnel Documents
Culture Documents
My Cheat Sheet
Transféré par
Tenzin KyizomCopyright
Formats disponibles
Partager ce document
Partager ou intégrer le document
Avez-vous trouvé ce document utile ?
Ce contenu est-il inapproprié ?
Signaler ce documentDroits d'auteur :
Formats disponibles
My Cheat Sheet
Transféré par
Tenzin KyizomDroits d'auteur :
Formats disponibles
Chapter 48: Somatic nervous system control skeletal muscles. Neuroglia assists cells that surround neurons.
NT cross a synapse. Saltatory conduction: process where AP only occur @ Nodes.of.Ravier. Chapter 50: Ca2+ required for tropomyosin to shift position. Cross.bridge: myosin head of the sarcomere binds actin. Sarcomere: thick filament,myosin,tropomyosin,actin. Chapter 42: time of diffusion proportional to distance2. Open circulatory system fluid: hemolymph. Atria: not a blood vessel. Pacemaker cells @ SA node. Arteries have thickest blood vessels. Capillaries: blood flow slowest. Interstitial fluid returned to blood thru lymph. Platelets: responsible for blood clot. Alveoli: site of gas exchange with blood (HUMANS). BPG, pH, CO2 conc. O2 conc. Affect affinity to Hb. Chapter 44: Nitrogenous waste of animals: Urea, Uric Acid, NH3. Glomerulus located @ Renal Cortex. Hydrostatic pressure drives filtration. ADH increases aquaporin. ANP released from heart atria. Nervous System: Na in: channel. Na out: pump, leaky channels= steady state of membrane permeability. Change in membrane permeability: needs stimulus: signaling chemic. binds, cause conformation change: open channel. Membrane potential: difference in charge or volt: Graded potential: depolar-EPSP. Hyperpol-IPSP, action potential. Potentials occur @ dendrites soma EPSP, IPSP. @ axon hillock to terminal- action potential. @axon terminal- Ca2+ flux and NT release. Membrane protein: when resting, no channels open. +NT=open channel. Vice versa. More NT = more EPSP/IPSP. Synaptic cleft: fluid space separates presynaptic & postsynaptic neurons. Prevent nerve impulse to directly pass from 1 neuron to other. Transmission across synaptic cleft: chemical event, release,diffusion& binding of NT and removal of NTs. NTs: ACh:degrade by AChase. Amines: dopamine, norepinephrine, serotonin: degrade by monoamine oxidase (MAO). Drugs; MAOInhibitor, SSRI. NTs effects: excitatory (depol) or inhibitory (hyperpol)determine by receptor type of postsynaptic neuron. Ach: excitatory @ neuromuscular junction of skeletal muscle Inhibitory @ cardiac musc. Direct action: NT bind to channel link receptor & opens ion channel, promote rapid responses. Indirect action: NT binds to G protein link receptor & acts through 2nd messenger, promotes long lasting effect. Cells communicate by chemical messenger. Local signaling: paracrine, synaptic. Long signaling: hormones> chem messenger secreted into vascular sys, transported to long distance target thru blood vessel. Cell signaling: reception, transduction & response. Reception: signal molecule (ligand) bind to receptor protein, change shape (early transduction), signal receptors are plasma membrane proteins. 3main membrane receptor: G protein-coupled receptor, receptor tyrosine kinases, ion channel receptor. Intracellular receptor: found in cytosol. Nucleus of target cell, ex: steroids chemical cross membrane & activate receptor. Transduction: cascades of molecular interactions relay signals from receptors to target molecules in cell. Signal amplification, signal cascade. 2nd messenger in pathways initiated by G-protein coupled receptors & tyrosine kinases receptor. Ex. Cyclic AMP & ca2+. Response: regulation of cellular activities, turning genes on or off, gene alteration. Termination: signal molecule leave receptor receptor inactive. Reflex: knee jerk example. Muscles: Classification of receptors: stimulus type- Mechanoreceptor: touch, atm., thermoreceptor: temp., photoreceptor: light, sight, chemoreceptor: chemical, osmoreceptor: change in osmotic pressure. Sensory neuron send info to the CNS from organs, motor neurons carry info from CNS to organs, glands & muscles. Sensory receptors: activation results in graded potentials trigger nerve impulses. characteristics of all muscles: locomotion (skeletal), blood pump (cardiac), BP maintain, squeeze substance through organs (smooth). Generate heat. Skeletal: voluntarily, overall body motility, Smooth: Special characteristics of musc. tissue, excitability: receive & respond to stimuli *Ach. Contractility: ability to shorten when stimulated, extensibility: ability to stretch, elasticity: ability to recoil to resting length. Many mitochondrias, glycosomes for glycogen storage, myoglobin for O2 storage. Sarcomere: contractile unit, region of myofibril btw 2 successive Z discs. Neuromuscular junction: midway along the length of muscle fiber, neuron releases ACh. Energy source of muscles: has ATP, with Ca2+ troponin changes shape pulls tropomyosin off of actin. More Ca2+ =more open binding sites, =more myosin pulling =more tension force effort. Contraction: crossbridge formation, powerstroke, crossbridge detachment, cocking. Muscle type-speed & energy. 1: slow oxidative, IIa: fast oxidative, IIb: fast glycolytic (strongest). Twitch: tension from 1AP, reflects Ca2+ buildup. More fiber= more strength, larger motor unit = bigger increase. Smooth: walls of hollow organs, forces food through internal channel, involuntary, contractions may be caused by stimulation from neurons in ANS. Usually 2 layers, long & circular. Persistalsis: alternating contraction & relaxations of smooth muscle layers that mix & squeeze substance through lumen of hollow organs. Long layer contract: organ dialate and shorten, circular layer contract, organ constrict and elongate.
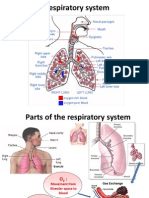
Cardiac muscle generates AP w/o neural input, not voluntary, contracts at rate set by hearts pacemaker, no twitch. Heart sound: AV valves closing: lub sound. Sound of systole. SL valves closing: dub sound: beginning of ventricular diastole. SA node: generates impulses, pacemaker begins, AP begins here. Pacemaker cells: autorythmic (steady): Due to hyperpol causing AP. EKG:P = atrial depol. P to Q is atrial systole = atrial contraction. QRS = ventricular depol = beginning of ventricular contraction results in lub sound as contraction beginsalso when atrial diastole begins QRS to the next P is atrial diastole. S to T = ventricular contraction. T = ventricular repol = end of vent. contraction or beginning of relaxation = beginning of diastole = dub sound. T to next QRS = vent. diastole. Heart: pressure gradient: driving force that keeps blood moving from high low pressure areas. High change in BP increase blood flow. High cross section area decreased flow rate. Arteries: high change in BP, low area: high vol. fast blood velocity. Capillaries: low change in BP, high area= slow blood velocity- ideal for exchange, low pressure gradient. Veins: low change in BP, high area= needs muscle milking to compensate. Lymph: fluid; what does not return to capillary indirectly returns to blood through lymphatic sys. returns fluid that leaks out in capillary beds. Vasoconstriction: contraction of smooth muscle in the walls of arterioles, increases BP. Vasodilation: relaxation of smooth muscles in the arterioles, decrease BP. Regulation of blood flow & pressure: heart: ANS neural: parasympathetic- ACh- decreases H.R, sympatheticnorepinephrine- increases H.R and strength. Hormonal: Epindephrine (adrenal medulla) increase H.R and strength. Open circulatory sys: uses hemolymph: general body fluid, bathes the organ, open ended vessels flow out among the cells. Closed circulatory sys: use blood confined to vessels, heart pumps, blood flows back to heart. Single circulation: blood enerts atrium and pumped out by ventricle. 2 chambered heart. Double circulation: oxygen poor and oxygen rich blood pumped separately from right and left side of heart. Blood vs. Hemolymph: blood is closed circ. In blood vessels. Hemolymph is in open circ. General body fluid (blood + interstitial fluid). Respiratory: large moist respiratory surface for exchange of gas btw cells and respiratory medium: air or water. In a given volume, less O2 in water than air, thats why O2 from water requires greater efficiency than air breathing. Water animals have outfoldings= greater surface for gas exchange. Gastrovascular cavity: diffusion is sufficient to reach all cells, short distance only. Ventilation moves the respiratory medium over the respiratory surface. Ventilation: controlled by pH *more pH = more ventilation. Tracheal system of insects: branching tubes that penetrate the body, supply O2 directly to body cells. Lungs are infolds. Breathing ventilates the lungs. Amphibian ventilate it lungs by (+) pressure breathing, forces air down the trachea. Birds breathe by airsacs. Alveoli in lungs, open pores, connect adjacent alveoli; allow air pressure throughout the lung to be equalized. Loading and unloading of O2 is facilitated by change in shape of Hb. If O2 binds, Hb affinity for O2 increases vice versa. Rate of laoding and unloading of O2 is regulated by Pressure O2, Temp, blood pH, PCO2, conc of BPG. Increase O2 => less CO2 = lower pH => low temperature => lower BPG (glycolysis intermediate: muscles). Very low level of O2 will increase ventilation even though CO2 levels dont change. Urinary system: osmoregulation homeostasis control of blood, salt and H2O. regulates solute concentration and balances the gain & loss of water. Controls movement of solutes between internal fluids and external environment. Excretion: getting rid of nitrogenous metabolites and other waste products. Ammonia waste: animals needs lots of water (fish), Urea waste: mammals: convert ammonia to less toxic urea, the conversion is energetically expensive. Uric acid (reptiles birds), largely insoluble in water, secreted as paste, more energetically expensive to produce than urea. Flame cells: of planaria, network of
dead end tubules conncected to external openings, smallest brances with flame bulb. The tubules excrete a dilute fluid & function in osmoregulation Metanephridia: open ended, collect coelomic luid and produce dilute urine for excretion *earthworm. Malpighian tubules: arthropods: produce dry waste matter. Excretory process Filtration: pressure filtering of body fluids, Reabsorption: reclaiming valuable solutes, Secretion: adding toxins and other solutes from the body fluids to the filtrate. Nutrients reabsorbed by cotransport with Na+. some minerals and others by passive diffusion. Loop of henle and collecting duct form a complex countercurrent system. Na/ K- pumps, establish concentration gradient of medulla.
Vous aimerez peut-être aussi
- Behavioral Neuroscience Ninth Edition BRAINDocument840 pagesBehavioral Neuroscience Ninth Edition BRAINvitor flenik89% (44)
- EKG Quick Reference ChartDocument4 pagesEKG Quick Reference ChartMildaPas encore d'évaluation
- A Simple Guide to the Heart beats, Related Diseases And Use in Disease DiagnosisD'EverandA Simple Guide to the Heart beats, Related Diseases And Use in Disease DiagnosisÉvaluation : 5 sur 5 étoiles5/5 (1)
- Basic EKG Interpretation Exam AnswersDocument3 pagesBasic EKG Interpretation Exam AnswerstwdroppointPas encore d'évaluation
- PEEP Positive End Expiratory Pressure and Its ConsequencesDocument2 pagesPEEP Positive End Expiratory Pressure and Its ConsequencesSadiq ZakariaPas encore d'évaluation
- EKG and ECG Interpretation: Learn EKG Interpretation, Rhythms, and Arrhythmia Fast!D'EverandEKG and ECG Interpretation: Learn EKG Interpretation, Rhythms, and Arrhythmia Fast!Pas encore d'évaluation
- HW InotropesDocument3 pagesHW InotropesNatalie YeohPas encore d'évaluation
- Normal Pediatric RR and HRDocument1 pageNormal Pediatric RR and HRRick FreaPas encore d'évaluation
- Ekg Panum or OsceDocument69 pagesEkg Panum or OsceGladish RindraPas encore d'évaluation
- Approach To The Patient With Respiratory DiseaseDocument6 pagesApproach To The Patient With Respiratory DiseaseRem AlfelorPas encore d'évaluation
- Heart Sounds: Mitral Regurgitation Congestive Heart FailureDocument6 pagesHeart Sounds: Mitral Regurgitation Congestive Heart FailurecindyPas encore d'évaluation
- PEEP (Positive-End Expiratory Pressure)Document5 pagesPEEP (Positive-End Expiratory Pressure)Valcrist BalderPas encore d'évaluation
- Congestive Heart FailureDocument86 pagesCongestive Heart FailureNabeel ShahzadPas encore d'évaluation
- RespiratoryDocument4 pagesRespiratoryHaliana IzatiPas encore d'évaluation
- Vanders Human Physiology The Mechanisms of Body Function 15th Edition Widmaier Test BankDocument29 pagesVanders Human Physiology The Mechanisms of Body Function 15th Edition Widmaier Test BankDavidWardrcobi100% (15)
- Chapter - 036 Arrhythmias ClassDocument129 pagesChapter - 036 Arrhythmias ClassWisdomIsMiseryPas encore d'évaluation
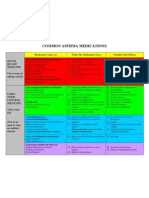
- Common Asthma MedicationsDocument1 pageCommon Asthma MedicationsHeart of the Valley, Pediatric CardiologyPas encore d'évaluation
- Laurene V. Fausett - Fundamentals of Neural Networks - Architectures, Algorithms and Applications-Pearson (1993) PDFDocument471 pagesLaurene V. Fausett - Fundamentals of Neural Networks - Architectures, Algorithms and Applications-Pearson (1993) PDFanant_nimkar9243100% (1)
- Psychology Test 1 Practice QuestionsDocument6 pagesPsychology Test 1 Practice Questionsshamim326180% (5)
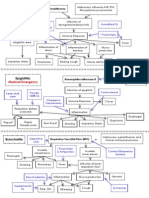
- Poster1 Arrhythmia Recognition e PDFDocument1 pagePoster1 Arrhythmia Recognition e PDFMiko RamosoPas encore d'évaluation
- Respiratory PathophysDocument1 pageRespiratory PathophysTori IkeharaPas encore d'évaluation
- Blood Flow: Right AtriumDocument2 pagesBlood Flow: Right AtriumDaffodelle AnnePas encore d'évaluation
- Davies Veterinary Specialists UnderstandingDocument3 pagesDavies Veterinary Specialists UnderstandingFelicity HumphreysPas encore d'évaluation
- Pediatric Respiratory Distress GuidelinesDocument1 pagePediatric Respiratory Distress GuidelinesRick FreaPas encore d'évaluation
- How Bloodis Propelled Throughthe Hum An Ci Rcula To Ry Sy StemDocument5 pagesHow Bloodis Propelled Throughthe Hum An Ci Rcula To Ry Sy Stemridwan100% (1)
- ABGs Respiratory/MetabolicDocument3 pagesABGs Respiratory/MetabolicJoe B100% (1)
- What Is Respiratory Alkalosis?Document3 pagesWhat Is Respiratory Alkalosis?Lorenn AdarnaPas encore d'évaluation
- IV PDFDocument63 pagesIV PDFelbagouryPas encore d'évaluation
- ReceptorsDocument9 pagesReceptorsrajenderPas encore d'évaluation
- Chapter 2.0 Cell Signalling and Endocrine RegulationDocument93 pagesChapter 2.0 Cell Signalling and Endocrine RegulationNurarief AffendyPas encore d'évaluation
- Test Bank For Psychology 12th Edition WadeDocument36 pagesTest Bank For Psychology 12th Edition Wadetrass.galenitez7jkPas encore d'évaluation
- Respiratory Physiology: Ventilation Perfusion DiffusionDocument6 pagesRespiratory Physiology: Ventilation Perfusion DiffusionShiara Ruth EdrosoloPas encore d'évaluation
- Neurotransmitters: A. Paracrine Regulators (Tissue Hormones)Document11 pagesNeurotransmitters: A. Paracrine Regulators (Tissue Hormones)Prasana100% (1)
- Cardiac Meds To MemorizeDocument4 pagesCardiac Meds To MemorizekellyaePas encore d'évaluation
- Paper 1 Ib Exam Saq NotesDocument15 pagesPaper 1 Ib Exam Saq NotesYosuke SuzukiPas encore d'évaluation
- Basics of Ventilatory SupportDocument43 pagesBasics of Ventilatory SupportAdhithya BhatPas encore d'évaluation
- Antiepileptic Drugs To Treat Psychiatric DisordersDocument435 pagesAntiepileptic Drugs To Treat Psychiatric DisordersHugo HernandezPas encore d'évaluation
- ADD Vs ADHDDocument4 pagesADD Vs ADHDatulmohan1Pas encore d'évaluation
- Lung Metabolism: Proteolysis and Antioproteolysis Biochemical Pharmacology Handling of Bioactive SubstancesD'EverandLung Metabolism: Proteolysis and Antioproteolysis Biochemical Pharmacology Handling of Bioactive SubstancesAlain JunodPas encore d'évaluation
- Heart Blood HistoDocument53 pagesHeart Blood HistoAnonymous 52lBinPas encore d'évaluation
- Breathing and Exchange of GasesDocument5 pagesBreathing and Exchange of Gaseslpc4944Pas encore d'évaluation
- Essentials of Psychiatric Mental Health Nursing 6th Edition Townsend Test BankDocument8 pagesEssentials of Psychiatric Mental Health Nursing 6th Edition Townsend Test BankTravisChristensenfteir100% (17)
- The Mentally Disabled in Philippine SettingDocument76 pagesThe Mentally Disabled in Philippine SettingAgnes Cheverloo CastilloPas encore d'évaluation
- AA GradientDocument2 pagesAA GradientzaminazzPas encore d'évaluation
- COPD Acute Management ABCDEDocument11 pagesCOPD Acute Management ABCDESSPas encore d'évaluation
- Patho Exam 3Document7 pagesPatho Exam 3menickel3Pas encore d'évaluation
- Cardiovascular Pathology 1:: Blood VesselsDocument48 pagesCardiovascular Pathology 1:: Blood VesselsRaiver CadenPas encore d'évaluation
- 3 MAJOR OPENINGS /right Atirum: Cardiovascular System Serious PericardiumDocument3 pages3 MAJOR OPENINGS /right Atirum: Cardiovascular System Serious PericardiumAebee Alcaraz100% (1)
- Sinus Rhythm DisturbancesDocument3 pagesSinus Rhythm DisturbancesMarcus Philip GonzalesPas encore d'évaluation
- Respiratory Care Standard Abbreviations and SymbolsDocument6 pagesRespiratory Care Standard Abbreviations and SymbolsHussein FatalPas encore d'évaluation
- Formula For Calculation of Hemodynamics in Cardiac Catheterization-Ver.1.1Document3 pagesFormula For Calculation of Hemodynamics in Cardiac Catheterization-Ver.1.1Sam YenPas encore d'évaluation
- Registered Respiratory TherapistDocument3 pagesRegistered Respiratory Therapistapi-76909521Pas encore d'évaluation
- Chapter (10) : Assessment of Cardiovascular SystemDocument10 pagesChapter (10) : Assessment of Cardiovascular SystemSandra GabasPas encore d'évaluation
- Symptom Flow Chart (Difficulty Breathing)Document2 pagesSymptom Flow Chart (Difficulty Breathing)Jeff ZhouPas encore d'évaluation
- JD Respiratory TherapistDocument3 pagesJD Respiratory TherapistLawrence MacaraegPas encore d'évaluation
- Physiology Lecture 10 Q-Bank (Cardiac Muscle - Action Potentials)Document15 pagesPhysiology Lecture 10 Q-Bank (Cardiac Muscle - Action Potentials)ChrisOrtPas encore d'évaluation
- Respiratory Therapy Cave - Ventilator Graphics Cheat SheetDocument2 pagesRespiratory Therapy Cave - Ventilator Graphics Cheat SheetMarwa El-DegwiPas encore d'évaluation
- Lillico NR511 SOAP Note Week 3 KatieDocument7 pagesLillico NR511 SOAP Note Week 3 Katie최인선100% (1)
- Classification of MurmursDocument2 pagesClassification of MurmursNazneen SiddiquiPas encore d'évaluation
- 406 - Respiratory Therapy Consult Service HandbookDocument28 pages406 - Respiratory Therapy Consult Service HandbookIkhsan JohnsonPas encore d'évaluation
- RsbiDocument1 pageRsbiRick FreaPas encore d'évaluation
- Registry Examination For Advanced Respiratory Therapists (RRT)Document6 pagesRegistry Examination For Advanced Respiratory Therapists (RRT)Sandy HartmanPas encore d'évaluation
- Ecg InterpretationDocument3 pagesEcg Interpretationman0billi0% (1)
- ELECTROCARDIOGRAM by Aldrin Jayson AlmadenDocument23 pagesELECTROCARDIOGRAM by Aldrin Jayson AlmadenItsMe AJPas encore d'évaluation
- Respiratory EmergenciesDocument34 pagesRespiratory EmergenciesRoshana MallawaarachchiPas encore d'évaluation
- Tara's Anatomy and Physiology - Aehlert ECGs Made EasyDocument16 pagesTara's Anatomy and Physiology - Aehlert ECGs Made EasyTara McNeillPas encore d'évaluation
- Anesthesia Cheat Sheet: Dogs CatsDocument3 pagesAnesthesia Cheat Sheet: Dogs CatsJoão Pedro Pereira100% (1)
- Mesenteric Ischemia in Dilated CardiomyopathyDocument30 pagesMesenteric Ischemia in Dilated CardiomyopathyJo AnnePas encore d'évaluation
- Physical Exam SheetDocument6 pagesPhysical Exam SheetDidi SaputraPas encore d'évaluation
- Latihan Ekg KD A III 2016Document15 pagesLatihan Ekg KD A III 2016Syamsul PutraPas encore d'évaluation
- RespiratoryDocument17 pagesRespiratorykurutalaPas encore d'évaluation
- Blog PostDocument1 pageBlog PostTenzin KyizomPas encore d'évaluation
- The Irony in Chinese Law EditorialDocument3 pagesThe Irony in Chinese Law EditorialTenzin KyizomPas encore d'évaluation
- Prose ExamDocument2 pagesProse ExamTenzin KyizomPas encore d'évaluation
- Lolita PaperDocument4 pagesLolita PaperTenzin KyizomPas encore d'évaluation
- The Great DepressionDocument29 pagesThe Great DepressionTenzin KyizomPas encore d'évaluation
- Lolita PaperDocument4 pagesLolita PaperTenzin KyizomPas encore d'évaluation
- John Lennon EssayDocument2 pagesJohn Lennon EssayTenzin KyizomPas encore d'évaluation
- PSY 200 Final Exam Study GuideDocument16 pagesPSY 200 Final Exam Study GuideJonat havensburgPas encore d'évaluation
- Physiology BCQsDocument25 pagesPhysiology BCQsReema KhanPas encore d'évaluation
- UTS - Fina1 - Learning To Be A Better Person - OriginalDocument15 pagesUTS - Fina1 - Learning To Be A Better Person - OriginalBernard PadillaPas encore d'évaluation
- Temple GrandinDocument31 pagesTemple GrandinPatricia Muñoz100% (2)
- Test Bank For Ebersole and Hess Gerontological Nursing and Healthy Aging 2nd Canadian Edition by TouhyDocument7 pagesTest Bank For Ebersole and Hess Gerontological Nursing and Healthy Aging 2nd Canadian Edition by Touhyjohnflorescdjrfwqxzs100% (28)
- Neural Control and Coordination Grade 11Document30 pagesNeural Control and Coordination Grade 11Dr. Remya RanjithPas encore d'évaluation
- 4-12th Bio Chap 17 Coordination & Control (A)Document2 pages4-12th Bio Chap 17 Coordination & Control (A)Raees Ali KhanPas encore d'évaluation
- 135 - Possible MecanismsDocument19 pages135 - Possible MecanismsEduardo BacelarPas encore d'évaluation
- Nervous System I: Basic Structure and FunctionDocument4 pagesNervous System I: Basic Structure and FunctionrohitPas encore d'évaluation
- Impact of Nutrition On Canine BehaviorDocument16 pagesImpact of Nutrition On Canine BehaviorTalita SantosPas encore d'évaluation
- Biopsycho QuestionsDocument4 pagesBiopsycho QuestionsArianne PicanaPas encore d'évaluation
- Neuropeptides in Dental Pulp - The Silent Protagonists PDFDocument16 pagesNeuropeptides in Dental Pulp - The Silent Protagonists PDFGerardo AragónPas encore d'évaluation
- Module 2.1 The Concept of The SynapseDocument4 pagesModule 2.1 The Concept of The SynapseArcanus LorreynPas encore d'évaluation
- Adenosine and Its Receptors As Therapeutic Targets An OverviewDocument9 pagesAdenosine and Its Receptors As Therapeutic Targets An OverviewLeonelLedezmaEstradaPas encore d'évaluation
- Chapter 41 - Neural Signaling (Complete)Document20 pagesChapter 41 - Neural Signaling (Complete)Liana Glorian G. NavarroPas encore d'évaluation
- Dopamine Receptors: GlossaryDocument5 pagesDopamine Receptors: Glossarytirasi1214Pas encore d'évaluation
- PIIS0896627316310078Document27 pagesPIIS0896627316310078Carolina RicárdezPas encore d'évaluation
- MPS5101 Report - 33300496Document7 pagesMPS5101 Report - 33300496Niti KakkadPas encore d'évaluation