Académique Documents
Professionnel Documents
Culture Documents
Flutrimazole Shampoo 1% Versus Ketoconazole Shampoo 2% in The Treatment of Pityriasis Versicolor. A Randomised Double-Blind Comparative Trial
Transféré par
Tommy HardiantoDescription originale:
Titre original
Copyright
Formats disponibles
Partager ce document
Partager ou intégrer le document
Avez-vous trouvé ce document utile ?
Ce contenu est-il inapproprié ?
Signaler ce documentDroits d'auteur :
Formats disponibles
Flutrimazole Shampoo 1% Versus Ketoconazole Shampoo 2% in The Treatment of Pityriasis Versicolor. A Randomised Double-Blind Comparative Trial
Transféré par
Tommy HardiantoDroits d'auteur :
Formats disponibles
Original article
Flutrimazole shampoo 1% versus ketoconazole shampoo 2% in the treatment of pityriasis versicolor. A randomised double-blind comparative trial
D. Rigopoulos,1 S. Gregoriou,1 G. Kontochristopoulos,2 A. Ifantides3 and A. Katsambas1
1 3
Department of Dermatology, University of Athens, A Sygros Hospital, Athens, 22nd Department of Dermatology, A Sygros Hospital, Athens and Biopathologist, Private Practice, Athens, Greece
Summary
Flutrimazole is an imidazole derivative that has been proven to be efcient in supercial skin fungal infections. The aim of this randomised double-blind study was to compare for the rst time, the efciency and safety of utrimazole 1% shampoo versus ketoconazole 2% shampoo in the treatment of tinea versicolor. Study population consisted of 60 patients with pityriasis versicolor diagnosed clinically and through direct microscopy and culture. Patients were randomly assigned to two groups: one instructed to apply utrimazole shampoo 1% and one instructed to apply ketoconazole shampoo 2% both on head and body for 14 days. Patients were re-evaluated 14 days after the end of treatment clinically and through direct microscopy and culture. Twenty-one of 26 patients (80.8%) in the ketoconazole and 22 of 29 patients (75.9%) in the utrimazole group had both visual healing and negative mycological evaluation. Comparison of the response between the two groups with the Yates corrected chisquare was found statistically not signicant (v2 0.19, d.f. 1, P 0.91). None of the patients in the two groups reported any adverse effects. Fourteen (53%) patients in the ketoconazole group and 23 (79%) in the utrimazole group assessed the shampoos as cosmetically acceptable regarding texture, smell and foam properties. Flutrimazole shampoo 1% appears to present efcacy comparable with ketoconazole 2% in the treatment of tinea versicolor.
Key words: utrimazole, ketoconazole, pityriasis versicolor, therapy.
Introduction
Pityriasis versicolor is a supercial fungal infection caused by lipophilic yeast of Malassezia species. The disease is very common throughout the world affecting mainly young adults of both sexes. Classical treatment includes agents such as propylene glycol, zinc pyrithione, selenium sulde, ciclopiroxolamine and imidazole derivatives.1
Correspondence: Dimitris Rigopoulos MD, PhD, Asst Professor of Dematology, Andreas Syngros Hospital, 5 Ionos Dragoumi str, 16121 Athens, Greece. Tel.: +2107265194. Fax: +2107211122. E-mail: drigop@hol.gr Accepted for publication 8 November 2006
Flutrimazole is an azole derivative that has been proven to be efcient when applied in cream formulation in supercial skin fungal infections.2 The aim of this randomised double-blind study was to compare for the rst time, the efciency and safety of utrimazole 1% shampoo versus ketoconazole 2% shampoo in the treatment of tinea versicolor.
Subjects and methods
Study population consisted of 60 patients with pityriasis versicolor diagnosed clinically, after uorescence examination of involved areas under Woods light, and through direct microscopy and culture. Skin scrapings from lesional and perilesional skin were examined with KOH 10% and strippings taken by Scotch tape were
2007 The Authors Journal Compilation 2007 Blackwell Publishing Ltd Mycoses (2007), 50, 193195
doi:10.1111/j.0933-7407.2006.01352.x
D. Rigopoulos et al.
cultured in Petri dishes with Dixon medium.3 Patients were excluded from the study, if they had serious concurrent diseases, other fungal infections or eye problems that could be irritated by the shampoo. The patients included in the study had not used any topical or systemic antifungal agent for the past month and gave informed written consent. Patients were randomly assigned by a computer to one of two groups. Patients in Group A were instructed to apply utrimazole shampoo 1% and patients in Group B ketoconazole shampoo 2%, on both head and body and leave it for 5 min (conrmed by timers) before rinsing. The formula of the utrimazole shampoo was: utrimazole gel 1% mgw/v, polysorbate 20, capryly/ capryl glucoside 60%, cocamidopropyl betaine 30%, acrylate/steareth-20methacrylate copolymer, 30% diazolinidyl urea, dimethicone propyl pg-betaine 30%, sodium hydroxide, essence puried water (manufactured by Olvos Science, Athens, Greece). The formula of the ketoconazole shampoo was: ketoconazole 2%, sodium lauryl sulphate, disodium monolauryl ether sulphosuccinate, coconut fatty acid diethanolamide, laurdimonium hydrolised animal collagen, macrogol 120 methyl glucose dioleate, concentrated hydrochloric acid, imidurea, perfume bouquet, erythrosine, sodium hydroxide, sodium chloride, water puried (Fungoral 2% Janssen-Cilag, Athens, Greece). Both products came in identical containers. Patients repeated the procedure every day for 14 days. The classical treatment duration of 14 days was preferred against the ultra short treatment of 3 days because of the better established response rates. Clinical and laboratorial re-evaluation through culture and direct microscopy took place 14 days after the end of treatment. Investigators assessing the clinical outcome were blinded concerning the therapeutical agent used. A patient was considered to show positive response if all visual evidence/symptoms
of fungal disease had disappeared (scaling and itching) with the exception of hypopigmentation and direct microscopy and culture were negative on day 28. Patients were also asked to report any adverse events and cosmetically evaluate the shampoo. A statistical analysis between the two groups was performed by using t-test for age, sex and duration of the disease and Yates corrected chi-square for the efcacy of the two shampoos.
Results
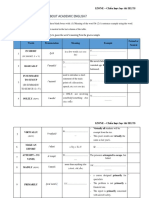
Fifty-ve patients (26 for the ketoconazole and 29 for the utrimazole group) returned for the follow-up visit. Demographics of all patients and duration of the disease in the two groups are presented in Table 1. There were no statistically signicant differences regarding age, sex and duration of the disease for the patients in the two groups. Twenty-one patients (80.8%) in the ketoconazole and 22 (75.9%) in the utrimazole group had both clinical response and negative mycological evaluation. When considering only clinical response, cure rates on day 28 were 88% (23 of 26) and 86% (25 of 29), respectively (Table 2). Comparison of response between the two groups with the Yates corrected chi-square was found statistically not signicant (v2 0.19, d.f. 1, P 0.91). None of the patients reported any adverse effect. Fourteen (53%) patients in the ketoconazole group and 23 (79%) in the utrimazole group assessed the shampoos as cosmetically acceptable regarding texture, smell and foam properties.
Discussion
Flutrimazole shares the mode of action of other imidazole- or triazole-containing antifungals, i.e. inhibition of fungal lanosterol 14 a-demethylase, as it strongly
Table 1 Demographic data and duration of disease for the patients in both groups at baseline Sex (male/female) Flutrimazole Ketoconazole P-value 14/15 14/12 >0.05 Age (years; mean SD) 32.8 7.4 30.5 9.2 >0.05 Duration (months; mean SD) 5.2 4.7 5.9 5.1 >0.05
Table 2 Clinical cure of scaling and itching but excluding hypopigmentation, negative direct microscopy examination and negative culture results in the two groups on day 28 Clinical response Flutrimazole Ketoconazole 25/29, 86.2% 23/26, 88.5% Negative KOH examination 22/29, 75.9% 22/26, 84.6% Negative culture 22/29, 75.9% 21/26, 80.8% Clinical and mycological cure 22/29, 75.9% 21/26, 80.8%
Comparison of response between the two groups with the Yates corrected chi-square was found statistically not signicant (v2 0.19, d.f. 1, P 0.91).
194
2007 The Authors Journal Compilation 2007 Blackwell Publishing Ltd Mycoses (2007), 50, 193195
Flutrimazole 1% shampoo in pityriasis versicolor
inhibits ergosterol biosynthesis in a cell-free homogenate of Candida albicans, with an IC50 value of 0.071 lmol l)1. It displays potent broad-spectrum in vitro activity against dermatophytes, lamentous fungi and yeast, saprophytic and pathogenic to animals and humans (minimum inhibitory concentration, MIC: 0.0255.0 lg ml)1).2 Studies have shown that the activity of utrimazole is comparable with that of clotrimazole and ketoconazole and markedly higher than that of bifonazole.46 Although utrimazoles antifungal properties have been well established, no formal study exists on the agents efcacy regarding the treatment of pityriasis versicolor in human patients. In vitro testing against 23 isolates of Malassezia furfur from guinea-pigs has shown that ketoconazole presents stronger inhibitory activity than utrimazole (geometric mean MIC: 0.51 lg ml)1 vs. 16 lg ml)1).7 In animal experiments involving three consecutive days of topical treatments, bifonazole 1% cream, clotrimazole 1% cream, utrimazole 1% and 2% creams, ketoconazole 2% cream and shampoo and miconazole 2% cream all reduced M. furfur dermatitis lesion severity below that of untreated control animals.8 In the patient population under study, there was no signicant difference in the cure rates between the ketoconazole and utrimazole groups suggesting that excellent outcome can be achieved with either agent. Moreover, the utrimazole shampoo formulation seems to exhibit antifungal activity comparable with the ketoconazole shampoo formulation available for decades. None of the patients in the two groups reported any adverse effects, conrming the reported low incidence of allergic contact reactions after imidazole topical application, despite their widespread use.8 In addition to the utrimazole shampoo formulation sharing the well established safety prole of the utrimazole cream formulation,9 more users attributed to the product an acceptable cosmetic prole than its ketoconazole counterpart. In conclusion, utrimazole 1% appears to present efcacy comparable with ketoconazole 2% in the treatment of pityriasis versicolor. Taking into account the better tolerability of the shampoo formulation, a
factor important for patients compliance, we believe that utrimazole shampoo 1% should be considered as an excellent alternative therapy for the management of tinea versicolor.
References
1 2 Gupta AK, Batra R, Bluhm R, Faergemann J. Pityriasis versicolor. Dermatol Clin 2003; 21: 41329. Garcia Rafanell J, Dronda MA, Merlos M et al. In vitro and in vivo studies with flutrimazole, a new imidazole derivative with antifungal activity. Arzneimittelforschung 1992; 42: 83640. Curvale-Fauchet N, Botterel F, Legrand P et al. Frequency of intravascular catheter colonization by Malassezia spp. in adult patients. Mycoses 2004; 47: 4914. Binet O, Soto-Melo J, Delgadillo J, Videla S, Izquierdo I, Forn J. Flutrimazole 1% dermal cream in the treatment of dermatomycoses: a randomized, multicentre, double-blind, comparative clinical trial with 1% clotrimazole cream. Flutrimazole Study Group. Mycoses 1994; 37: 4559. Alomar A, Videla S, Delgadillo J, Gich I, Izquierdo I, Forn J. Flutrimazole 1% dermal cream in the treatment of dermatomycoses: a multicentre, double-blind, randomized, comparative clinical trial with bifonazole 1% cream. Efficacy of flutrimazole 1% dermal cream in dermatomycoses. Catalan Flutrimazole Study Group. Dermatology 1995; 190: 295300. del Palacio A, Cuetara S, Perez A, Garau M, Calvo T, Sanchez-Alor G. Topical treatment of dermatophytosis and cutaneous candidosis with flutrimazole 1% cream: doubleblind, randomized comparative trial with ketoconazole 2% cream. Mycoses 1999; 42: 64955. Van Gerven F, Odds FC. The anti-Malassezia furfur activity in vitro and in experimental dermatitis of six imidazole antifungal agents: bifonazole, clotrimazole, flutrimazole, ketoconazole, miconazole and sertaconazole. Mycoses 1995; 38: 38993. Dooms-Goossens A, Matura M, Drieghe J, Degreef H. Contact allergy to imidazoles used as antimycotic agents. Contact Dermatitis 1995; 33: 737. Izquierdo I, Bayes M, Jane J, Alomar A, Forn J. Local and systemic tolerance of flutrimazole skin creams following single and repeated topical application in healthy volunteers. Arzneimittelforschung 1992; 42: 85960.
2007 The Authors Journal Compilation 2007 Blackwell Publishing Ltd Mycoses (2007), 50, 193195
195
Vous aimerez peut-être aussi
- Practical Patch Testing and Chemical Allergens in Contact DermatitisD'EverandPractical Patch Testing and Chemical Allergens in Contact DermatitisPas encore d'évaluation
- Pharmaceutics 12 00446Document24 pagesPharmaceutics 12 00446Nikita jainPas encore d'évaluation
- Anti-Aging Therapeutics Volume XIVD'EverandAnti-Aging Therapeutics Volume XIVÉvaluation : 3 sur 5 étoiles3/5 (1)
- RCT Keto Foam 1% Vs Keto Cream 2% in PVDocument4 pagesRCT Keto Foam 1% Vs Keto Cream 2% in PVnurjiPas encore d'évaluation
- Biologic and Systemic Agents in DermatologyD'EverandBiologic and Systemic Agents in DermatologyPaul S. YamauchiPas encore d'évaluation
- Efficacy of 2% Metronidazole Gel in Moderate Acne Vulgaris: Therapeutic RoundDocument5 pagesEfficacy of 2% Metronidazole Gel in Moderate Acne Vulgaris: Therapeutic RoundFebniPas encore d'évaluation
- Jurnal Kulit 1 (Aloe-Vera)Document7 pagesJurnal Kulit 1 (Aloe-Vera)Alifan HaqiPas encore d'évaluation
- ClindamycinDocument5 pagesClindamycinRatna HusnanisaPas encore d'évaluation
- Us Bactroban OintmentDocument4 pagesUs Bactroban OintmentJayCee AriasPas encore d'évaluation
- 106 New CharmDocument5 pages106 New CharmAmit Kumar PandeyPas encore d'évaluation
- Jcdsa20120300010 79060760Document5 pagesJcdsa20120300010 79060760iqbalPas encore d'évaluation
- Chottawornsak2019 PDFDocument6 pagesChottawornsak2019 PDFnadifaPas encore d'évaluation
- Effectiveness of Glutathione (GSH) 2%, Tocopheryl Acetate 1%, and Magnesium Ascorbyl Phosphate 3% Combination Cream Compared With Hydroquinone 4% Cream As A Skin Lightening Agent: A Randomised StudyDocument7 pagesEffectiveness of Glutathione (GSH) 2%, Tocopheryl Acetate 1%, and Magnesium Ascorbyl Phosphate 3% Combination Cream Compared With Hydroquinone 4% Cream As A Skin Lightening Agent: A Randomised StudyKorry Meliana PangaribuanPas encore d'évaluation
- Eberconazole Vs TerbinafineDocument4 pagesEberconazole Vs TerbinafineBayu Zeva WirasaktiPas encore d'évaluation
- Gupta2014Document7 pagesGupta2014Lodewyk Kefas JoshoaPas encore d'évaluation
- Oral Itraconazole For The Treatment of Severe Seborrhoeic DermatitisDocument4 pagesOral Itraconazole For The Treatment of Severe Seborrhoeic DermatitisSilvia SafitriPas encore d'évaluation
- Assessment of The Efficacy and Tolerance of A New Combination of Retinoids and Depigmenting Agents in The Treatment of MelasmaDocument8 pagesAssessment of The Efficacy and Tolerance of A New Combination of Retinoids and Depigmenting Agents in The Treatment of MelasmaAna Karina Alvarado OsorioPas encore d'évaluation
- Topical Histamine Stimulates Repigmentation of Nonsegmental Vitiligo by A Receptor-Dependent MechanismDocument7 pagesTopical Histamine Stimulates Repigmentation of Nonsegmental Vitiligo by A Receptor-Dependent MechanismManu PalaoPas encore d'évaluation
- The Use of Pycnogenol in The Treatment of Melasma: Original ArticlesDocument5 pagesThe Use of Pycnogenol in The Treatment of Melasma: Original ArticlesfreitasjonashenriquePas encore d'évaluation
- Ebruary M CAD ErmatolDocument1 pageEbruary M CAD ErmatolDrAmit VermaPas encore d'évaluation
- Treatment of MelasmaDocument10 pagesTreatment of MelasmaPriska Paramita PringgoredjoPas encore d'évaluation
- Roles of Adapalene in The Treatment of Pityriasis VersicolorDocument5 pagesRoles of Adapalene in The Treatment of Pityriasis VersicolorexaPas encore d'évaluation
- Comparison of Efficacy of Adapalene (0.1% Gel) Monotherapy Ve Adapalene (0.1%) Plus Benzyl Peroxide (2.5%) Combination Therapy For Treatment of Mild To Moderate Acne VulgarisDocument3 pagesComparison of Efficacy of Adapalene (0.1% Gel) Monotherapy Ve Adapalene (0.1%) Plus Benzyl Peroxide (2.5%) Combination Therapy For Treatment of Mild To Moderate Acne VulgarisMushthafa HabiburrahmanPas encore d'évaluation
- GJHS 5 150Document5 pagesGJHS 5 150Wisnu Aditya WardanaPas encore d'évaluation
- Open Comparative Study of Efficacy and Safety of Ketoconazole Soap and Oral Ketoconazole in Tinea VersicolorDocument5 pagesOpen Comparative Study of Efficacy and Safety of Ketoconazole Soap and Oral Ketoconazole in Tinea VersicolorYohanes WidjajaPas encore d'évaluation
- Dermatologica Sinica: Brief ReportDocument3 pagesDermatologica Sinica: Brief ReportTelavani umriPas encore d'évaluation
- Antimicrob. Agents Chemother.-2011-Carrillo-Muсoz-AAC.00219-11Document13 pagesAntimicrob. Agents Chemother.-2011-Carrillo-Muсoz-AAC.00219-11neleatucicovshiiPas encore d'évaluation
- MJCU - Volume 86 - Issue September - Pages 3083-3092Document10 pagesMJCU - Volume 86 - Issue September - Pages 3083-3092gàbbý pédràszàPas encore d'évaluation
- The Scientific World Journal, 2020 - ER - CompressedDocument14 pagesThe Scientific World Journal, 2020 - ER - CompressederlidawatiPas encore d'évaluation
- 1096 2687 1 PBDocument6 pages1096 2687 1 PBRabia OmarPas encore d'évaluation
- ART20202715Document3 pagesART20202715jamila ilPas encore d'évaluation
- Averrhoa Carambola: Original ArticleDocument8 pagesAverrhoa Carambola: Original ArticleelvinaPas encore d'évaluation
- TransleteDocument8 pagesTransleteNisapratiwi96Pas encore d'évaluation
- BJD 13441Document53 pagesBJD 13441Remaja IslamPas encore d'évaluation
- HTTPDocument6 pagesHTTPFebniPas encore d'évaluation
- Adapalene 0.1% Gel Is Better Tolerated Than Tretinoin 0.025% Gel in Acne PatientsDocument3 pagesAdapalene 0.1% Gel Is Better Tolerated Than Tretinoin 0.025% Gel in Acne PatientsFenni OktoberryPas encore d'évaluation
- Dermatologica Sinica: Jung Won Shin, Kyoung Chan ParkDocument6 pagesDermatologica Sinica: Jung Won Shin, Kyoung Chan ParkGiovan GaulPas encore d'évaluation
- Itraconazole Therapy in Pityriasis VersicolorDocument10 pagesItraconazole Therapy in Pityriasis VersicolorKopitesPas encore d'évaluation
- 1 s2.0 S0190962214000462 MainDocument1 page1 s2.0 S0190962214000462 MainMuhamad Fikri IhsanPas encore d'évaluation
- Therapeutic RoundDocument6 pagesTherapeutic RoundFebniPas encore d'évaluation
- Comparative Study of The Efficacy and Safety of Topical Antifungal Agents Clotrimazole Versus Sertaconazole in The Treatment of Tinea Corporis/crurisDocument5 pagesComparative Study of The Efficacy and Safety of Topical Antifungal Agents Clotrimazole Versus Sertaconazole in The Treatment of Tinea Corporis/crurisRasyid Ali NatioPas encore d'évaluation
- Staphylococcus Epidermidis and S. Aureus. Especially, It Exerted Strong Anti-P. Acnes Ability. TheDocument18 pagesStaphylococcus Epidermidis and S. Aureus. Especially, It Exerted Strong Anti-P. Acnes Ability. TheEntang The'FirsterPas encore d'évaluation
- PDF MMJ 658Document4 pagesPDF MMJ 658ezradamanikPas encore d'évaluation
- Antimicrob. Agents Chemother. 1994 Pershing 90 5Document6 pagesAntimicrob. Agents Chemother. 1994 Pershing 90 5vickyPas encore d'évaluation
- Hormonas and AcneDocument3 pagesHormonas and AcneRistiana Suci d'KemponPas encore d'évaluation
- Cannabis y Atopia en PerrosDocument6 pagesCannabis y Atopia en PerrosAndres RodriguezPas encore d'évaluation
- Odumosu and EkweDocument4 pagesOdumosu and EkwePutri Nur HandayaniPas encore d'évaluation
- Evaluation of The Efficacy and Safety of Topical and Oral Glutathione in Treatment of MelasmaDocument10 pagesEvaluation of The Efficacy and Safety of Topical and Oral Glutathione in Treatment of Melasmagàbbý pédràszàPas encore d'évaluation
- TopicalDocument5 pagesTopicalazizasyifaPas encore d'évaluation
- Jurding VitiligoDocument9 pagesJurding VitiligoDini MariniPas encore d'évaluation
- Antimicrobial Efficacy of Granulysin-Derived Synthetic Peptides in Acne VulgarisDocument11 pagesAntimicrobial Efficacy of Granulysin-Derived Synthetic Peptides in Acne VulgarisOvienanda KristiPas encore d'évaluation
- Therapeutic Roun2Document5 pagesTherapeutic Roun2FebniPas encore d'évaluation
- Potential Phytotherapy of Atopic Dermatitis, Acne, Psoriasis, VitiligoDocument7 pagesPotential Phytotherapy of Atopic Dermatitis, Acne, Psoriasis, VitiligoMUHAMMAD BUKHARIPas encore d'évaluation
- High ThroutDocument7 pagesHigh ThroutashrafbookPas encore d'évaluation
- Cosmetic Contact Sensitivity in PatientsDocument11 pagesCosmetic Contact Sensitivity in PatientsLeonardo de SouzaPas encore d'évaluation
- A Cream of Herbal Mixture To Improve MelasmaDocument8 pagesA Cream of Herbal Mixture To Improve MelasmaRatih Anindita Rahajeng RipyonoPas encore d'évaluation
- IndianDermatolOnlineJ52128-3296446 090924Document4 pagesIndianDermatolOnlineJ52128-3296446 090924Arifudin Cipto HusodoPas encore d'évaluation
- Efficacy and Safety of Cream Containing Climbazole/Piroctone Olamine For Facial Seborrheic Dermatitis: A Single-Center, Open-Label Split-Face Clinical StudyDocument7 pagesEfficacy and Safety of Cream Containing Climbazole/Piroctone Olamine For Facial Seborrheic Dermatitis: A Single-Center, Open-Label Split-Face Clinical StudynurulPas encore d'évaluation
- Arasa Et Al-2014-Experimental DermatologyDocument6 pagesArasa Et Al-2014-Experimental DermatologyIndah PratiwiPas encore d'évaluation
- Prof. Barmawi KULIAH 5 AMOEBIASISDocument43 pagesProf. Barmawi KULIAH 5 AMOEBIASISTommy HardiantoPas encore d'évaluation
- Mammals and Birds Secrete A Hypertonic UrineDocument2 pagesMammals and Birds Secrete A Hypertonic UrineTommy HardiantoPas encore d'évaluation
- Mammals and Birds Secrete A Hypertonic UrineDocument2 pagesMammals and Birds Secrete A Hypertonic UrineTommy HardiantoPas encore d'évaluation
- Presentasi JurnalDocument23 pagesPresentasi JurnalTommy HardiantoPas encore d'évaluation
- Journal ReadingDocument7 pagesJournal ReadingTommy HardiantoPas encore d'évaluation
- Compartement Syndrom (21 Juni 2012)Document12 pagesCompartement Syndrom (21 Juni 2012)Tommy HardiantoPas encore d'évaluation
- Ujian Essay OrthopaedicDocument2 pagesUjian Essay OrthopaedicTommy HardiantoPas encore d'évaluation
- CFSS Monitoring Tool 2019Document7 pagesCFSS Monitoring Tool 2019JULIE100% (10)
- BB - Self AuditDocument18 pagesBB - Self AuditFe Rackle Pisco JamerPas encore d'évaluation
- SBMWSM2016Document491 pagesSBMWSM2016maimaiyeuem123100% (1)
- 2-Acute Abdominal PainDocument24 pages2-Acute Abdominal Painabdalmajeed alshammaryPas encore d'évaluation
- A Report - Noise Pollution in Urban AreasDocument14 pagesA Report - Noise Pollution in Urban AreasArjita SinghPas encore d'évaluation
- IZONE Academic WordlistDocument59 pagesIZONE Academic WordlistTrung KiênPas encore d'évaluation
- Effect of A Physiotherapy Program in Women With Primary DysmenorrheaDocument6 pagesEffect of A Physiotherapy Program in Women With Primary DysmenorrheaPaula RangelPas encore d'évaluation
- Urinary Tract InfectionDocument10 pagesUrinary Tract Infectionjaah diazPas encore d'évaluation
- The CSI Effect - Google FormsDocument12 pagesThe CSI Effect - Google FormsZivi DegenPas encore d'évaluation
- Prevalence of Burkholderia Mallei in Equids of Remount Depot, Sargodha, PakistanDocument6 pagesPrevalence of Burkholderia Mallei in Equids of Remount Depot, Sargodha, PakistanMuhammad Naeem IqbalPas encore d'évaluation
- MHFA For SchoolsDocument45 pagesMHFA For SchoolsLING KUOK LIMPas encore d'évaluation
- Max Medic Plan 2Document1 pageMax Medic Plan 2Premkumar NadarajanPas encore d'évaluation
- NK 48InjuryCategoryPackagesDocument4 pagesNK 48InjuryCategoryPackagesJD Health Services TirupatturPas encore d'évaluation
- ANGIOSARCOMA pdf3 PDFDocument9 pagesANGIOSARCOMA pdf3 PDFعبدالعزيز عماد محمودPas encore d'évaluation
- Medical PalmistryDocument5 pagesMedical PalmistryvivekpatelbiiPas encore d'évaluation
- Lights and ShadowsDocument5 pagesLights and Shadowsweeeeee1193Pas encore d'évaluation
- Anita Wagh-8-3-99-944 PDFDocument5 pagesAnita Wagh-8-3-99-944 PDFbutlesrPas encore d'évaluation
- Iligan Medical Center College Research PaperDocument9 pagesIligan Medical Center College Research PaperRyan Sulog PangantingPas encore d'évaluation
- SUMMATIVE English8Document4 pagesSUMMATIVE English8Therese LlobreraPas encore d'évaluation
- Pelvic Fracture Case StudyDocument48 pagesPelvic Fracture Case StudyYves BasanPas encore d'évaluation
- Gavi - 2015 Country TA RFIDocument20 pagesGavi - 2015 Country TA RFIDeepakSinghPas encore d'évaluation
- Msds Uq160 enDocument5 pagesMsds Uq160 enAnnalisa GiammòPas encore d'évaluation
- Job Shadowing PresentationDocument12 pagesJob Shadowing Presentationapi-462381810Pas encore d'évaluation
- ResumeDocument2 pagesResumeapi-281248740Pas encore d'évaluation
- Course Profile - HIRARC - 1 DAYDocument4 pagesCourse Profile - HIRARC - 1 DAYRizal de silvaPas encore d'évaluation
- Interview Marsha SarverDocument3 pagesInterview Marsha Sarverapi-326930615Pas encore d'évaluation
- Harga Prolanis (Data Dari Apotek Online)Document74 pagesHarga Prolanis (Data Dari Apotek Online)Orin Tri WulanPas encore d'évaluation
- Recall GuidelinesDocument31 pagesRecall GuidelinesSandy PiccoloPas encore d'évaluation
- Risk Assessment - TemplateDocument10 pagesRisk Assessment - TemplateJohn KalvinPas encore d'évaluation
- Talent MappingDocument18 pagesTalent MappingSoumya RanjanPas encore d'évaluation
- Love Life: How to Raise Your Standards, Find Your Person, and Live Happily (No Matter What)D'EverandLove Life: How to Raise Your Standards, Find Your Person, and Live Happily (No Matter What)Évaluation : 3 sur 5 étoiles3/5 (1)
- Summary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedD'EverandSummary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedÉvaluation : 4.5 sur 5 étoiles4.5/5 (82)
- ADHD is Awesome: A Guide to (Mostly) Thriving with ADHDD'EverandADHD is Awesome: A Guide to (Mostly) Thriving with ADHDÉvaluation : 5 sur 5 étoiles5/5 (3)
- LIT: Life Ignition Tools: Use Nature's Playbook to Energize Your Brain, Spark Ideas, and Ignite ActionD'EverandLIT: Life Ignition Tools: Use Nature's Playbook to Energize Your Brain, Spark Ideas, and Ignite ActionÉvaluation : 4 sur 5 étoiles4/5 (404)
- The Age of Magical Overthinking: Notes on Modern IrrationalityD'EverandThe Age of Magical Overthinking: Notes on Modern IrrationalityÉvaluation : 4 sur 5 étoiles4/5 (32)
- Think This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BeD'EverandThink This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BeÉvaluation : 2 sur 5 étoiles2/5 (1)
- Manipulation: The Ultimate Guide To Influence People with Persuasion, Mind Control and NLP With Highly Effective Manipulation TechniquesD'EverandManipulation: The Ultimate Guide To Influence People with Persuasion, Mind Control and NLP With Highly Effective Manipulation TechniquesÉvaluation : 4.5 sur 5 étoiles4.5/5 (1412)
- By the Time You Read This: The Space between Cheslie's Smile and Mental Illness—Her Story in Her Own WordsD'EverandBy the Time You Read This: The Space between Cheslie's Smile and Mental Illness—Her Story in Her Own WordsPas encore d'évaluation
- The Ritual Effect: From Habit to Ritual, Harness the Surprising Power of Everyday ActionsD'EverandThe Ritual Effect: From Habit to Ritual, Harness the Surprising Power of Everyday ActionsÉvaluation : 4 sur 5 étoiles4/5 (4)
- Raising Mentally Strong Kids: How to Combine the Power of Neuroscience with Love and Logic to Grow Confident, Kind, Responsible, and Resilient Children and Young AdultsD'EverandRaising Mentally Strong Kids: How to Combine the Power of Neuroscience with Love and Logic to Grow Confident, Kind, Responsible, and Resilient Children and Young AdultsÉvaluation : 5 sur 5 étoiles5/5 (1)
- Summary: Outlive: The Science and Art of Longevity by Peter Attia MD, With Bill Gifford: Key Takeaways, Summary & AnalysisD'EverandSummary: Outlive: The Science and Art of Longevity by Peter Attia MD, With Bill Gifford: Key Takeaways, Summary & AnalysisÉvaluation : 4.5 sur 5 étoiles4.5/5 (42)
- The Body Keeps the Score by Bessel Van der Kolk, M.D. - Book Summary: Brain, Mind, and Body in the Healing of TraumaD'EverandThe Body Keeps the Score by Bessel Van der Kolk, M.D. - Book Summary: Brain, Mind, and Body in the Healing of TraumaÉvaluation : 4.5 sur 5 étoiles4.5/5 (266)
- The Comfort of Crows: A Backyard YearD'EverandThe Comfort of Crows: A Backyard YearÉvaluation : 4.5 sur 5 étoiles4.5/5 (23)
- The Obesity Code: Unlocking the Secrets of Weight LossD'EverandThe Obesity Code: Unlocking the Secrets of Weight LossÉvaluation : 4 sur 5 étoiles4/5 (6)
- The Diabetes Code: Prevent and Reverse Type 2 Diabetes NaturallyD'EverandThe Diabetes Code: Prevent and Reverse Type 2 Diabetes NaturallyÉvaluation : 4.5 sur 5 étoiles4.5/5 (4)
- Mindset by Carol S. Dweck - Book Summary: The New Psychology of SuccessD'EverandMindset by Carol S. Dweck - Book Summary: The New Psychology of SuccessÉvaluation : 4.5 sur 5 étoiles4.5/5 (328)
- Hearts of Darkness: Serial Killers, The Behavioral Science Unit, and My Life as a Woman in the FBID'EverandHearts of Darkness: Serial Killers, The Behavioral Science Unit, and My Life as a Woman in the FBIÉvaluation : 4 sur 5 étoiles4/5 (20)
- The Courage Habit: How to Accept Your Fears, Release the Past, and Live Your Courageous LifeD'EverandThe Courage Habit: How to Accept Your Fears, Release the Past, and Live Your Courageous LifeÉvaluation : 4.5 sur 5 étoiles4.5/5 (254)
- Dark Psychology & Manipulation: Discover How To Analyze People and Master Human Behaviour Using Emotional Influence Techniques, Body Language Secrets, Covert NLP, Speed Reading, and Hypnosis.D'EverandDark Psychology & Manipulation: Discover How To Analyze People and Master Human Behaviour Using Emotional Influence Techniques, Body Language Secrets, Covert NLP, Speed Reading, and Hypnosis.Évaluation : 4.5 sur 5 étoiles4.5/5 (110)
- Critical Thinking: How to Effectively Reason, Understand Irrationality, and Make Better DecisionsD'EverandCritical Thinking: How to Effectively Reason, Understand Irrationality, and Make Better DecisionsÉvaluation : 4.5 sur 5 étoiles4.5/5 (39)
- When the Body Says No by Gabor Maté: Key Takeaways, Summary & AnalysisD'EverandWhen the Body Says No by Gabor Maté: Key Takeaways, Summary & AnalysisÉvaluation : 3.5 sur 5 étoiles3.5/5 (2)
- Cult, A Love Story: Ten Years Inside a Canadian Cult and the Subsequent Long Road of RecoveryD'EverandCult, A Love Story: Ten Years Inside a Canadian Cult and the Subsequent Long Road of RecoveryÉvaluation : 4 sur 5 étoiles4/5 (46)
- Dark Psychology: Learn To Influence Anyone Using Mind Control, Manipulation And Deception With Secret Techniques Of Dark Persuasion, Undetected Mind Control, Mind Games, Hypnotism And BrainwashingD'EverandDark Psychology: Learn To Influence Anyone Using Mind Control, Manipulation And Deception With Secret Techniques Of Dark Persuasion, Undetected Mind Control, Mind Games, Hypnotism And BrainwashingÉvaluation : 4 sur 5 étoiles4/5 (1138)