Académique Documents
Professionnel Documents
Culture Documents
Cascade Koagulasi
Transféré par
Ratih ArianitaDescription originale:
Copyright
Formats disponibles
Partager ce document
Partager ou intégrer le document
Avez-vous trouvé ce document utile ?
Ce contenu est-il inapproprié ?
Signaler ce documentDroits d'auteur :
Formats disponibles
Cascade Koagulasi
Transféré par
Ratih ArianitaDroits d'auteur :
Formats disponibles
In a normal individual, coagulation is initiated within 20 seconds after an injury occurs to the blood vessel damaging the endothelial
cells. Platelets immediately form a haemostatic plug at the site of injury. This is called primary haemostasis. Secondary haemostasis then follows plasma components called coagulation factors respond (in a complex cascade) to form fibrin strands which strengthen the platelet plug. Contrary to popular belief, coagulation from a cut on the skin is not initiated by air or drying out, but by platelets adhering to and activated by collagen in the blood vessel endothelium. The activated platelets then release the contents of their granules, these contain a variety of substances that stimulate further platelet activation and enhance the haemostatic process. The use of adsorbent chemicals, such as zeolite, and other haemostatic agents is also being explored for use in sealing severe injuries quickly.
Primary haemostasis
Primary haemostasis is initiated when platelets adhere, using a specific platelet collagen receptor glycoprotein Ia/IIa, to collagen fibers in the vascular endothelium. This adhesion is mediated by von Willebrand factor (vWF), which forms links between the platelet glycoprotein Ib/IX/V and collagen fibrils. The platelets are then activated and release the contents of their granules into the plasma, in turn activating other platelets and white blood cells. The platelets undergo a change in their shape which exposes a phospholipid surface for those coagulation factors that require it. Fibrinogen links adjacent platelets by forming links via the glycoprotein IIb/IIIa. In addition, thrombin activates platelets.
Secondary haemostasis
The coagulation cascade
The coagulation cascade of secondary hemostasis has two pathways, the Contact Activation pathway (formerly known as the Intrinsic Pathway) and the Tissue Factor pathway (formerly known as the Extrinsic pathway) that lead to fibrin formation. It was previously thought that the coagulation cascade consisted of two pathways of equal importance joined to a common pathway. It is now known that the primary pathway for the initiation of blood coagulation is the Tissue Factor pathway. The pathways are a series of reactions, in which a zymogen of a serine protease and its glycoprotein co-factor are activated to become active components that then catalyze the next reaction in the cascade. Coagulation factors are generally indicated by Roman numerals, with a lowercase a appended to indicate an active form, ultimately resulting in cross-linked fibrin. The coagulation factors are serine proteases (enzymes) except FVIII and FV which are glycoproteins. The serine proteases act by cleaving other proteins at specific sites. Factor XIII is a transglutaminase. Protein C is also a serine protease. The coagulation factors circulate as inactive zymogens. The coagulation cascade can be summarised as follows: 1. Tissue Factor pathway: the main role of the tissue factor pathway is to generate a "thrombin burst," thrombin being the single most important constituent of the coagulation cascade in terms of its feedback activation roles. FVIIa circulates in a higher amount than any other activated coagulation factor and following damage to the blood vessel endothelium Tissue Factor (TF) is released, this then forms a complex with FVIIa (TF-FVIIa) this activates FIX and FX. FVII itself is activated by thrombin, FXIa, plasmin, FXII and FXa. The activation of FXa by TF-FVIIa is almost immediately inhibited by tissue factor pathway inhibitor (TFPI). FXa and its co-factor FVa form the prothombinase complex which activates prothrombin to thrombin.
Thrombin then activates other components of the coagulation cascade, including FV and FVII (which activates FXI which in turn activates FIX), and activates and releases FVIII from being bound to vWF. FVIIIa is the co-factor of FIXa and together they form the "tenase" complex which activates FX and so the cycle continues. 2. Contact Activation pathway: There is formation of the primary complex on collagen by high molecular weight kininogen (HMWK), prekallikrein and FXII (Hageman factor). Prekallikrein is converted to kallikrein and FXII becomes FXIIa. FXIIa converts FXI into FXIa. Factor XIa activates FIX, which with its co-factor FVIIIa form the tenase complex which activates FX to FXa. The minor role that the contact activation pathway has in initiating clot formation can be illustrated by the fact that patients with severe deficiencies of FXII, HMWK and prekallikrein do not have a bleeding disorder. 3. Thrombin Thrombin has a large array of functions. Its primary role is the conversion of fibrinogen to fibrin, the building block of a haemostatic plug. In addition, it activates Factors VIII and V and their inhibitor protein C (in the presence of thrombomodulin), and it activates Factor XIII, which forms covalent bonds that crosslink the fibrin polymers that form from activated monomers. Following activation by the contact factor or tissue factor pathways the coagulation cascade is maintained in a prothrombotic state by the continued activation of FVIII and FIX to form the tenase complex, until it is down regulated by the anticoagulant pathways.
Cofactors and inhibitors
Various substances are required for the proper functioning of the coagulation cascade: Calcium and phospholipid (a platelet membrane constituent) are required for the tenase and prothrombinase complexes to function. Calcium mediates the binding of the complexes via the terminal gamma-carboxy residues on FXa and FIXa to the phospholipid surfaces expressed by platelets. Calcium is also required at other points in the coagulation cascade. Vitamin K is an essential factor to a hepatic gamma-glutamyl carboxylase that adds a carboxyl group to glutamic acid residues on factors II, VII, IX and X, as well as Protein S, Protein C and Protein Z. Deficiency of vitamin K (e.g. in malabsorption), use of inhibiting anticoagulants (warfarin, acenocoumarol and phenprocoumon) or disease (cirrhosis, hepatocellular carcinoma) impairs the function of the enzyme and leads to the formation of PIVKA's (proteins formed in vitamin K absence) this causes partial or non gamma carboxylation and affects the coagulation factors ability to bind to expressed phospholipid. Three mechanisms keep the coagulation cascade in check. Abnormalities can lead to an increased tendency toward thrombosis: Protein C is an important co-factor inhibitor, which degrades the co-factors FVa and FVIIIa. It is activated by thrombin with thrombomodulin and requires its co-enzyme Protein S to function. Quantitative or qualitative deficiency of either may lead to thrombophilia (a tendency to develop thrombosis). Impaired action of Protein C (activated Protein C resistance), for example by having the "Leiden" variant of Factor V or high levels of FVIII also may lead to a thrombotic tendency. Antithrombin is a serine protease inhibitor (serpin) that degrades the serine proteases; thrombin and FXa, as well as FXIIa, and FXIa. It is constantly active, but its adhesion to these factors is increased by the presence of heparan sulfate (a glycosaminoglycan)
or the administration of heparins (different heparinoids increase affinity to F Xa, F IIa, or both). Quantitative or qualitative deficiency of antithrombin (inborn or acquired, e.g. in proteinuria) leads to thrombophilia. Tissue factor pathway inhibitor (TFPI) inhibits F VIIa-related activation of F IX and F X after its original initiation.
Testing of coagulation
Numerous tests are used to assess the function of the coagulation system: Common: aPTT, INR (PT), TCT, bleeding time, D-dimer Other: mixing test (whether an abnormality corrects if the patient's plasma is mixed with normal plasma), antiphosholipid antibodies, coagulation factor assays, genetic tests (eg. factor V Leiden, prothrombin mutation G20210A), dilute Russell viper venom test (dRVVT), platelet function tests, thromboelastography (TEG) or thromboelastometry (ROTEG). The contact factor pathway is initiated by activation of the "contact factors" of plasma, and can be measured by the activated partial thromboplastin time (aPTT) test. The Tissue factor pathway is initiated by release of "tissue factor" (a specific cellular lipoprotein), and can be measured by the prothrombin time (PT) test. This is reported as an INR value when used for the dosing of oral anticoagulants such as warfarin. The quantatative and qualitative screening of fibrinogen is measured by the thrombin time (TCT). Measurement of the exact amount of fibrinogen present in the blood is generally done using the Clauss method for fibrinogen testing. Many analysers are capable of measuring a "derived fibrinogen" level from the graph of the Prothrombin time clot. If a coagulation factor is part of the contact or tissue factor pathway, a deficiency of that factor will affect only one of the tests: thus hemophilia A, a deficiency of factor VIII, which is part of the contact factor pathway, results in an abnormally prolonged aPTT test but a normal PT test. The exceptions are prothrombin, fibrinogen and some variants of FX which can only be detected by either aPTT or PT. Deficiencies of fibrinogen (quantitative or qualitative) will affect all screening tests.
Disorders of hemostasis
Disorders of the platelet and vessel wall *Immune thrombocytopenic purpura (ITP) *Thrombotic thrombocytopenic purpura (TTP) *Hemolytic-uremic syndrome (HUS) *Glanzmann's thrombasthenia *Bernard-Soulier syndrome (abnormal glycoprotein Ib-IX-V complex) *Storage pool disorders *Paroxysmal nocturnal hemoglobinuria *Gray platelet syndrome: deficient alpha granules. *Delta storage pool deficiency: deficient dense granules. Disorders of coagulation and thrombosis
*Disseminated intravascular coagulation *Factor deficiencies **Hemophilia A (Factor VIII deficiency) **Hemophilia B (Factor IX deficiency, "Christmas disease") **Hemophilia C (Factor XI deficiency, mild bleeding tendency) **Von Willebrand disease (the most common bleeding disorder) *Factor inhibitors Disorders predisposing to thrombosis (see: hypercoagulability) *Heparin-induced thrombocytopenia and thrombosis ("white clot syndrome") *Antiphospholipid syndrome **Lupus anticoagulant **Anticardiolipin antibody *Factor V Leiden *Prothrombin mutation *Protein C deficiency *Protein S deficiency *Antithrombin deficiency *Abnormally raised levels of Factor VIII and Factor XI
Coagulation factors
Coagulation factors and related substances Number and/or name I (fibrinogen) II (prothrombin) Tissue factor Calcium V (proaccelerin, labile factor) VI VII (stable factor) VIII (antihemophilic factor) IX (Christmas factor) X (Stuart-Prower factor) XI (plasma thromboplastin antecedent) XII (Hageman factor) XIII (fibrin-stabilizing factor) von Willebrand factor prekallikrein high molecular weight kininogen (HMWK) fibronectin Function Forms clot (fibrin) Its active form (IIa) activates I, V, VII, XIII, protein C, platelets Co-factor of VIIa (formerly known as factor III) Required for coagulation factors to bind to phospholipid (formerly known as factor IV) Co-factor of X with which it forms the prothrombinase complex Unassigned old name of Factor Va Activates IX, X Co-factor of IX with which it forms the tenase complex Activates X: forms tenase complex with factor VIII Activates II: froms prothrombinase complex with factor V Activates XII, IX and prekallikrein Activates prekallikrein and fibrinolysis Crosslinks fibrin Binds to VIII, mediates platelet adhesion Activates XII and prekallikrein; cleaves HMWK Supports reciprocal activation of XII, XI, and prekallikrein Mediates cell adhesion
antithrombin III heparin cofactor II protein C protein S protein Z Protein Z-related protease inhibitor (ZPI) plasminogen alpha 2-antiplasmin tissue plasminogen activator (tPA) urokinase plasminogen activator inhibitor1 (PAI1) plasminogen activator inhibitor2 (PAI2) cancer procoagulant
Inhibits IIa, Xa, and other proteases; Inhibits IIa, cofactor for heparin and dermatan sulfate ("minor antithrombin") Inactivates Va and VIIIa Cofactor for activated protein C (APC, inactive when bound to C4b-binding protein) Mediates thrombin adhesion to phospholipids and stimulates degradation of factor X by ZPI Degrades factors X (in presence of protein Z) and XI (independently) Converts to plasmin, lyses fibrin and other proteins Inhibits plasmin Activates plasminogen Activates plasminogen Inactivates tPA & urokinase (endothelial PAI) Inactivates tPA & urokinase (placental PAI) Pathological factor X activator linked to thrombosis in cancer
History
Theories on the coagulation of blood have existed since antiquity. Physiologist Johannes Mller (1801-1858) described fibrin, the substance of a thrombus. Its soluble precursor, fibrinogen, was thus named by Rudolf Virchow (1821-1902), and isolated chemically by Prosper Sylvain Denis (1799-1863). Alexander Schmidt suggested that the conversion from fibrinogen to fibrin was the result of an enzymatic process, and labeled the hypothetical enzyme "thrombin" and its precursor "prothrombin"Shapiro SS. Treating thrombosis in the 21st century. N Engl J Med 2003;349:1762-4. PMID 14585945.. Platelets were identified in 1865, and their function was elucidated by Giulio Bizzozero in 1882Brewer DB. Max Schultze (1865), G. Bizzozero (1882) and the discovery of the platelet. Br J Haematol 2006;133:251-8. DOI [10.1111/j.1365-2141.2006.06036.x].. The theory that thrombin was generated by the presence of tissue factor and calcium was consolidated by Paul Morawitz in 1905. At this stage, it was known that thrombokinase/thromboplastin (factor III) was released by damaged tissues, reacting with prothrombin (II), which, together with calcium (IV), formed thrombin, which converted fibrinogen into fibrin (I)Giangrande PL. Six characters in search of an author: the history of the nomenclature of coagulation factors. Br J Haematol 2003;121:703-12. PMID 12780784.. The remainder of the biochemical factors in the process of coagulation were largely discovered in the 20th century. A first clue as to the actual complexity of the system of coagulation was the discovery of proaccelerin (initially and later called Factor V) by Paul Owren (1905-1990) in 1947. He also
postulated that its function was the generation of accelerin (Factor VI), which later turned out to be the activated form of V (or Va); hence, VI is not now in active use. Factor VII (also known as serum prothrombin conversion accelerator or proconvertin, precipitated by barium sulfate) was discovered in a young female patient in 1949 and 1951 by different groups. Factor VIII turned out to be deficient in the clinically recognised but etiologically elusive hemophilia A; it was identified in the 1950s and is alternatively called antihemophilic globulin due to its capability to correct hemophilia A. Factor IX was discovered in 1952 in a young patient with hemophilia B named Stephen Christmas (1947-1993). His deficiency was described by Dr. Rosemary Biggs and Professor R.G. MacFarlane in Oxford, UK. The factor is hence called Christmas Factor or Christmas Eve Factor. Christmas lived in Canada, and campaigned for blood transfusion safety until succumbing to transfusion-related AIDS at age 46. An alternative name for the factor is plasma thromboplastin component, given by an independent group in California. Hageman factor, now known as factor XII, was identified in 1955 in an asymptomatic patient with a prolonged bleeding time named of John Hageman. Factor X, or Stuart-Prower factor, followed, in 1956. This protein was identified in a Ms. Audrey Prower of London, who had a lifelong bleeding tendency. In 1957, an American group identified the same factor in a Mr. Rufus Stuart. Factors XI and XIII were identified in 1953 and 1961, respectively. The usage of Roman numerals rather than eponyms or systematic names was agreed upon during annual conferences (starting in 1955) of hemostasis experts. This committee evolved into the present-day International Committee on Thrombosis and Hemostasis (ICTH). Assignment of numerals ceased in 1963 after the naming of Factor XIII. The names Fletcher Factor and Fitzgerald Factor were given to further coagulation-related proteins, namely prekallikrein and high molecular weight kininogen respectively. Factors III and VI are unassigned, as thromboplastin was never identified, and actually turned out to consist of ten further factors, and accelerin was found to be activated Factor V. All mammals have an extremely closely related blood coagulation process, using a combined cellular and serine protease process. In fact, it is possible for any mammalian coagulation factor to "cleave" its equivalent target in any other mammal. The only nonmammalian animal that uses serine proteases for blood coagulation is the Horseshoe Crab.
Vous aimerez peut-être aussi
- CoagulationDocument3 pagesCoagulationHerho-nyl CesPas encore d'évaluation
- Biochemistry of The Blood Coagulation SystemDocument4 pagesBiochemistry of The Blood Coagulation Systemabc007200100% (1)
- Hemostasis, Hemorrhagic Disorders and ThrombosisDocument114 pagesHemostasis, Hemorrhagic Disorders and ThrombosisZeePas encore d'évaluation
- Articulo PDFDocument11 pagesArticulo PDFmartin najeraPas encore d'évaluation
- ClottingDocument25 pagesClottingAtalabi AdebusolaPas encore d'évaluation
- Labmed33 0948Document6 pagesLabmed33 0948VKTNPas encore d'évaluation
- Introduction To Blood CoagulationDocument22 pagesIntroduction To Blood Coagulationemman_abzPas encore d'évaluation
- Hemostasis: in The NeonateDocument5 pagesHemostasis: in The NeonateMorales Eli PediatraPas encore d'évaluation
- Haemostasis: Dr. Ali ElhassanDocument45 pagesHaemostasis: Dr. Ali ElhassanMohja JaberPas encore d'évaluation
- Secondary HemostasisDocument12 pagesSecondary HemostasisMariella DinglePas encore d'évaluation
- Coagulation Cascade: Thrombin Act On Fibrinogen and Convert It To Fibrin To Form Fibrin ClotDocument23 pagesCoagulation Cascade: Thrombin Act On Fibrinogen and Convert It To Fibrin To Form Fibrin ClotSawsan Z. JwaiedPas encore d'évaluation
- HemostasisDocument14 pagesHemostasisGowtham SelvarajPas encore d'évaluation
- 1-4 Hemostasis, Surgical Bleeding and TransfusionDocument17 pages1-4 Hemostasis, Surgical Bleeding and TransfusionRobin Tolentino100% (3)
- Coagulation and Hemostasis - Part 2Document33 pagesCoagulation and Hemostasis - Part 2Raghad SonríoPas encore d'évaluation
- Hemostatic Physiology: Mansyur Arif Dept. of Clinical Pathology Faculty of Medicine, Hasanuddin University, MakassarDocument66 pagesHemostatic Physiology: Mansyur Arif Dept. of Clinical Pathology Faculty of Medicine, Hasanuddin University, MakassarilhamaminsyaputraPas encore d'évaluation
- Hemostatic Physiology: Presented byDocument68 pagesHemostatic Physiology: Presented byDitha FadhilaPas encore d'évaluation
- Sarthak Mechanism of Blood ClottingDocument42 pagesSarthak Mechanism of Blood ClottingVishal MishraPas encore d'évaluation
- Hemost. & Coag - PhysiologyDocument40 pagesHemost. & Coag - PhysiologyImam Muhamad RissandyPas encore d'évaluation
- Cascadeeee KoagulasiDocument3 pagesCascadeeee Koagulasiv noviantihyPas encore d'évaluation
- Unit IV HemostasisDocument49 pagesUnit IV Hemostasisalshads957Pas encore d'évaluation
- HaemostasisDocument8 pagesHaemostasisKe ShPas encore d'évaluation
- SGD 20 - HemostasisDocument8 pagesSGD 20 - HemostasisJohn RayPas encore d'évaluation
- Biochem Hemostatis and ThrombosisDocument54 pagesBiochem Hemostatis and ThrombosischayChay gapolPas encore d'évaluation
- 33-Hemostasis and Coagulation ProfileDocument40 pages33-Hemostasis and Coagulation ProfileOsman Mohamed MuhumedPas encore d'évaluation
- Hema 2 AssignmentDocument3 pagesHema 2 AssignmentErnest CañosPas encore d'évaluation
- Hemostasis, Clotting, EctDocument33 pagesHemostasis, Clotting, Ectblessing akataPas encore d'évaluation
- Bleeding DisordersDocument27 pagesBleeding DisordersIliana América AlarcónPas encore d'évaluation
- Blood Vessels and Endothelial CellsDocument4 pagesBlood Vessels and Endothelial CellsJemmy FandriPas encore d'évaluation
- Hemostasis and Blood CoagulationDocument11 pagesHemostasis and Blood CoagulationRinta MoonPas encore d'évaluation
- Intrinsic PathwayDocument4 pagesIntrinsic PathwayAsish GeiorgePas encore d'évaluation
- Hemostasis ReviewerDocument14 pagesHemostasis ReviewerDayledaniel SorvetoPas encore d'évaluation
- The Coagulation CascadeDocument8 pagesThe Coagulation Cascade8pvz96ktd9Pas encore d'évaluation
- HemostasisDocument20 pagesHemostasisTULSI SHARMAPas encore d'évaluation
- Hemostasis: Overview of Normal Hemostasis 3Document23 pagesHemostasis: Overview of Normal Hemostasis 3Joce Maripangui100% (1)
- Essentials of Anticoagulation in Hemodialysis: Core CurriculumDocument12 pagesEssentials of Anticoagulation in Hemodialysis: Core CurriculumKavidu KeshanPas encore d'évaluation
- Have Half-Lives in The Range 2 - 6 H. Lovenox Is 4.5 Hours. The Anticoagulant Effect ofDocument37 pagesHave Half-Lives in The Range 2 - 6 H. Lovenox Is 4.5 Hours. The Anticoagulant Effect ofkellixgPas encore d'évaluation
- Clinical Anesthesiolog1 BLOODDocument14 pagesClinical Anesthesiolog1 BLOODIsra JavedPas encore d'évaluation
- Società Federata Anmvi: in Collaborazione ConDocument5 pagesSocietà Federata Anmvi: in Collaborazione ConMuhammad Arslan GillPas encore d'évaluation
- Chapter 34 Reviewer From Katzung's Basic & Clinical PharmacologyDocument6 pagesChapter 34 Reviewer From Katzung's Basic & Clinical PharmacologyAimee Redor100% (1)
- Disseminated Intravascular Coagulation: Dr. Abhineet PG Registrar Dept of Transfusion Medicine and ImmunohematologyDocument60 pagesDisseminated Intravascular Coagulation: Dr. Abhineet PG Registrar Dept of Transfusion Medicine and ImmunohematologyAbhineet SalvePas encore d'évaluation
- Blood Coagulation: The Clotting CascadesDocument5 pagesBlood Coagulation: The Clotting CascadesNorrifhan Akmal IsmailPas encore d'évaluation
- Hemostasis: /coagulationDocument80 pagesHemostasis: /coagulationLeonardo Adi BestPas encore d'évaluation
- Schemi 1-2Document7 pagesSchemi 1-2lucaPas encore d'évaluation
- Normal HemostasisDocument34 pagesNormal Hemostasisمصطفي خندقاويPas encore d'évaluation
- He Most As IsDocument22 pagesHe Most As IsFiras Nazih Bou DiabPas encore d'évaluation
- Primary HemostasisDocument10 pagesPrimary HemostasisMariella DinglePas encore d'évaluation
- Physiology of CoagulationDocument44 pagesPhysiology of CoagulationXee JayPas encore d'évaluation
- Coagulation disorders-MS1Document46 pagesCoagulation disorders-MS1Chamika Huruggamuwa100% (1)
- Fisiologi Hemostasis Dan FibrinolisisDocument45 pagesFisiologi Hemostasis Dan FibrinolisisBesth To Frynce HutabaratPas encore d'évaluation
- Overview of Hemostasis - UpToDateDocument50 pagesOverview of Hemostasis - UpToDateTrung LêPas encore d'évaluation
- Clotting FactorsDocument7 pagesClotting FactorsDjdjjd SiisusPas encore d'évaluation
- Coagulation of BloodDocument16 pagesCoagulation of BloodMoner ManushPas encore d'évaluation
- Normal HaemostasisDocument36 pagesNormal HaemostasisReem EshraPas encore d'évaluation
- Coagulation ReviewDocument6 pagesCoagulation ReviewRobins DhakalPas encore d'évaluation
- ThromboelastographyDocument39 pagesThromboelastographyMarcelliaPas encore d'évaluation
- Hemostasis - MechanismDocument5 pagesHemostasis - MechanismАнна КатраженкоPas encore d'évaluation
- Blood ClottingDocument68 pagesBlood ClottingRevina AmaliaPas encore d'évaluation
- A New Understanding of The Coagulation ProcessDocument6 pagesA New Understanding of The Coagulation Processwuryan dewiPas encore d'évaluation
- Platelet Protocols: Research and Clinical Laboratory ProceduresD'EverandPlatelet Protocols: Research and Clinical Laboratory ProceduresPas encore d'évaluation
- Trading SecretsDocument99 pagesTrading SecretsGary100% (3)
- Lease of Playground To A SchoolDocument2 pagesLease of Playground To A SchoolSutapaPas encore d'évaluation
- Catalogue Maltep en PDFDocument88 pagesCatalogue Maltep en PDFStansilous Tatenda NyagomoPas encore d'évaluation
- Disruptive Strategy Final Paper Company ProfilesDocument2 pagesDisruptive Strategy Final Paper Company ProfilesHumberto Jose Arias BarrosPas encore d'évaluation
- Intensive Care Fundamentals: František Duška Mo Al-Haddad Maurizio Cecconi EditorsDocument278 pagesIntensive Care Fundamentals: František Duška Mo Al-Haddad Maurizio Cecconi EditorsthegridfanPas encore d'évaluation
- Sow English Year 4 2023 2024Document12 pagesSow English Year 4 2023 2024Shamien ShaPas encore d'évaluation
- Due Process of LawDocument2 pagesDue Process of Lawjoe100% (4)
- Grammar Summary Unit 8Document2 pagesGrammar Summary Unit 8Luana Suarez AcostaPas encore d'évaluation
- The Impact of Eschatology and ProtologyDocument48 pagesThe Impact of Eschatology and ProtologyJuan SteinPas encore d'évaluation
- Amazon PrimeDocument27 pagesAmazon PrimeMohamedPas encore d'évaluation
- Proximity Principle of DesignDocument6 pagesProximity Principle of DesignSukhdeepPas encore d'évaluation
- Technical Activities: Ken Goldberg, VP Technical Activities Spring 2007, ICRA, RomeDocument52 pagesTechnical Activities: Ken Goldberg, VP Technical Activities Spring 2007, ICRA, RomeWasim Ahmad KhanPas encore d'évaluation
- 750 Famous Motivational and Inspirational QuotesDocument53 pages750 Famous Motivational and Inspirational QuotesSaanchi AgarwalPas encore d'évaluation
- KNOLL and HIERY, The German Colonial Experience - IntroDocument6 pagesKNOLL and HIERY, The German Colonial Experience - IntroGloria MUPas encore d'évaluation
- Written Test 4-Book 3Document2 pagesWritten Test 4-Book 3Vinícius MoreiraPas encore d'évaluation
- Bond - Chemical Bond (10th-11th Grade)Document42 pagesBond - Chemical Bond (10th-11th Grade)jv peridoPas encore d'évaluation
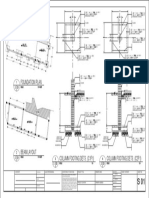
- Foundation Plan: Scale 1:100 MTSDocument1 pageFoundation Plan: Scale 1:100 MTSJayson Ayon MendozaPas encore d'évaluation
- Nutrition Science by B Srilakshmi PDFDocument6 pagesNutrition Science by B Srilakshmi PDFRohan Rewatkar46% (35)
- Internship Report Aqib 2Document11 pagesInternship Report Aqib 2Usman SheikhPas encore d'évaluation
- All About Me - RubricDocument3 pagesAll About Me - Rubricapi-314921155Pas encore d'évaluation
- Gonzales v. PennisiDocument15 pagesGonzales v. Pennisimceline19Pas encore d'évaluation
- Schedule 1 Allison Manufacturing Sales Budget For The Quarter I Ended March 31 First QuarterDocument16 pagesSchedule 1 Allison Manufacturing Sales Budget For The Quarter I Ended March 31 First QuarterSultanz Farkhan SukmanaPas encore d'évaluation
- Halai Entu: Kohhrana Thuhril (Sermon) Chungchang - IiDocument4 pagesHalai Entu: Kohhrana Thuhril (Sermon) Chungchang - IiRollick LalnuntluangaPas encore d'évaluation
- MDL ChallanDocument1 pageMDL ChallanPratik V PaliwalPas encore d'évaluation
- Course: Business Communication Course Code: COM 402 Submitted To: Mr. Nasirullah Khan Submission Date: 12Document18 pagesCourse: Business Communication Course Code: COM 402 Submitted To: Mr. Nasirullah Khan Submission Date: 12Wahaj noor SiddiquePas encore d'évaluation
- Odyssey Marine Exploration, Inc. v. The Unidentified, Shipwrecked Vessel or Vessels - Document No. 3Document11 pagesOdyssey Marine Exploration, Inc. v. The Unidentified, Shipwrecked Vessel or Vessels - Document No. 3Justia.comPas encore d'évaluation
- CWWDocument2 pagesCWWmary joy martinPas encore d'évaluation
- Gremath Set8-1Document48 pagesGremath Set8-1uzairmetallurgistPas encore d'évaluation
- Oblicon NotesDocument14 pagesOblicon NotesCee Silo Aban100% (1)
- Safety Management in Coromandel FertilizerDocument7 pagesSafety Management in Coromandel FertilizerS Bharadwaj ReddyPas encore d'évaluation