Académique Documents
Professionnel Documents
Culture Documents
Emergency Drugs
Transféré par
Roland Mark Rodel LagosCopyright
Formats disponibles
Partager ce document
Partager ou intégrer le document
Avez-vous trouvé ce document utile ?
Ce contenu est-il inapproprié ?
Signaler ce documentDroits d'auteur :
Formats disponibles
Emergency Drugs
Transféré par
Roland Mark Rodel LagosDroits d'auteur :
Formats disponibles
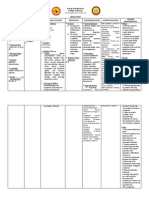
ROLAND MARK RODEL DUMAGPI LAGOS DRUG DATA Generic Name: PROCAINAMIDE Trade Name: Pronestyl Patients Dose:
n/a Minimum Dose: 100mg IVTT q 5mins Maximum Dose: 600mg IVTT q 60mins Availability: Solution Route of Administration: IV, IM CLASSIFICATION Therapeutic: Antiarrhythmics (class IA) Pregnancy Risk Category: C MECHANISM OF ACTION Decrease myocardial exitability. Slows conduction velocity. May depress myocardial contractility Therapeutic: Suppression of arrhythmias. Onset: immediate Peak: 25 - 60 mins Duration: 3 4 hrs Half-Life: 2.5 4.7 hrs INDICATION General: Treatment of a wide variety of ventricular and atrial arrhythmias, including: Atrial premature contractions, Premature ventricular contractions, Ventricular tachycardia, Paroxysmal atrial tachycardia. Maintenance of normal sinus rhythm after conversion from atrial fibrillation or flutter ADVERSE/SIDE EFFECTS Contraindicated in CNS: hypersensitivity; AV block; Seizures, dizziness, Myasthenia gravis; confusion Hypersinsitiviity to tarrazine (FDC yellow dye CV: asystole, heart #5; present in some oral block, ventricular products) arrhythmias, hypotension Use catiously in known suspected CNS disorder, GI: renal impairment. diarrhea, anorexia, bitter taste, nausea, Drug Interaction: vomiting May have additive or antagonistic effects with Derm: other antiarryhtmics. rashes Additive neurologic toxicity (confusion, seizures) with lidocaine. Antihypertensives and nitrates may potentiate hypotensive effect. Potentiates neuromuscular blocking agents. May partially antagonize the therapeutic effects of anticholinesterase agents in myasthenia gravis. CONTRADICATION NURSING RESPONSIBILITIES Before: Check doctors order. Review drug preparation. Assess for clients heart rate. Inform therapeutic effect. Check venoclysis patency. During: Observe rights of administration. Administer drug on time. Monitor BP closely during administration. Assess for patients hypersensitivity. Inform patient of the possible adverse/side effects of drug. After: Monitor bowel elimination. Check Lab values leukocytes, eosinophils and platelets. Advise patient to report for allergic reactions. Advised to avoid activity that requires mental alertness. Notify health care professionals if no improvement w/in a few days.
Source: Deglin J. H., Vallerand A. H. (2008). Daviss Drug Guide for Nurses. (11th ed., pp. 1008 1010) 1915 Arch Street Philadelphia, PA 19103: F.A Davis Company. DOI: www.fadavis.com
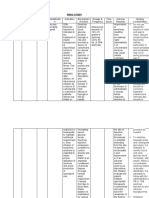
ADVERSE/SIDE NURSING RESPONSIBILITIES EFFECTS Generic Name: Therapeutic: Contraindicated in CNS: Before: HYDRALAZINE Antihypertensive hypersensitivity; Some dizziness, drowsiness, Check doctors order. rpoducts contain tartazine headache Review drug preparation. Trade Name: and should be avoided in Assess for clients heart rate. Apresoline patients with known CV: tachycardia, agina, Inform therapeutic effect. Pharmacologic intolerance. arrhythmias, edema, Check venoclysis patency. Patients Dose: Vasodilator orthostatic During: n/a Use cautiously in hypotension Observe rights of Pregnancy Risk Cardiovascular or administration. Minimum Dose: Category: cerebrovascular disease; GI: Administer drug on time. 5mg C Severe renal and hepatic diarrhea, nausea, Monitor BP closely during fisease (dose modification vomiting administration. Maximum Dose: Onset: may be necessary); Assess for patients 40mg 5 - 20 mins hypersensitivity. Drug Interaction: Inform patient of the possible Availability: Peak: Increase hypotension with adverse/side effects of drug. Tablets, Injection, 15 - 30 mins acute ingestion of alcohol, After: Solution other antihypertensives, or Monitor BUN results. Duration: nitrates. MAO inhibitors Monitor liver function. Route of Administration: 2 6 hrs may exaggerate Arrange for pyridoxine if patient IV, IM, PO hypotension. May decrease develops symptoms of peripheral Half-Life: pressor response to neuritis. 2 8 hrs epinephrine. NSAIDS may Advised to avoid activity that decrease antihypertensive requires mental alertness. response. Notify health care professionals if no improvement w/in a few days. th Source: Deglin J. H., Vallerand A. H. (2008). Daviss Drug Guide for Nurses. (11 ed., pp. 633 635) 1915 Arch Street Philadelphia, PA 19103: F.A Davis Company. DOI: www.fadavis.com DRUG DATA CLASSIFICATION CONTRADICATION
MECHANISM OF INDICATION ACTION Direct-acting General: peripheral arteriolar Moderate to severe vasodilator. hypertension (with a diuretic). Unlabeled Therapeutic: uses: CHF unresponsive Lowering of blood to conventional therapy pressure in with digoxin and hypertensive diuretics patients and decreased afterload in patients with CHF.
DRUG DATA Generic Name: HYDROCORTISONE SOIUM SUCCINATE
CLASSIFICATION Therapeutic: Antiasthmatics, corticosteroid
Before: Check doctors order. Review drug preparation. Assess for clients heart rate. Trade Name: Inform therapeutic effect. A-hydroCort, Solu-Cortef Check venoclysis patency. Pharmacologic Therapeutic: Use cautiously in chronic During: Patients Dose: corticosteroids Suppression of treatment Observe rights of n/a inflammation and CV: hypertension administration. Pregnancy Risk modification of the Drug Interaction: Administer drug on time (before Minimum Dose: Category: normal immune Increase isk of hypokalemia GI: 9AM to mimic normal diurnal 4mg C response. with thiazide and loop Peptic ulceration, corticosteroid levels). diuretics, or amphotericin anorexia, nausea, Monitor BP closely during Maximum Dose: Onset: B. Hypokalemia may vomiting administration. 10mg rapid increase risk of digoxin Assess for patients toxicity. hypersensitivity. Availability: Peak: Inform patient of the possible Tablets, Injection, unknown adverse/side effects of drug. Solution After: Duration: Monitor BP hourly. Route of Administration: unknown No virus vaccine for patients IV, IM, PO taking this medication. Half-Life: Provide antacids before meals 1.5 2 hrs to prevent peptic ulcer. Advised to avoid activity that requires mental alertness. Notify health care professionals if no improvement w/in a few days. Source: Deglin J. H., Vallerand A. H. (2008). Daviss Drug Guide for Nurses. (11th ed., pp. 350 357) 1915 Arch Street Philadelphia, PA 19103: F.A Davis Company. DOI: www.fadavis.com
MECHANISM OF ACTION Replace endogenous cortisol in deficiency states. Have potent mineralocorticoid activity.
INDICATION General: Management adrenocortical insufficiency.
CONTRADICATION Contraindicated in active of untreated infections (maybe used in patients being treated for some forms of meningitits).
ADVERSE/SIDE EFFECTS CNS: Depression, euphoria, headache, increased intracranial pressure, personality change, psychoses, restlessness
NURSING RESPONSIBILITIES
DRUG DATA Generic Name: ISOSORBIDE MONONITRATE Trade Name: Apo-ISMN, IMDUR Patients Dose: n/a Minimum Dose: 2.5mg Maximum Dose: 5mg Availability: Tablets, Injection, Solution Route of Administration: IV, IM, PO
CLASSIFICATION Therapeutic: antianginals
Pharmacologic nitrates Pregnancy Risk Category: C
MECHANISM OF ACTION Produce vasodilation (venous greater than arterial). Decrease left ventricular enddiastolic pressure and left ventricular endvolume(preload). Net effect is reduced myocardial oxygen consumption. Increase coronary blood flow by dilating coronary arteries and improving collateral flow to ischemic regions. Therapeutic: Relief and prevention of angina attacks Onset: unknown Peak: unknown Duration: 12 hrs
INDICATION General: Acute treatment of angina attacks (SL only). Prophylactic management of angina pectoris. Treatment of chronic CHF(unlabeled)
ADVERSE/SIDE EFFECTS Contraindicated in CNS: hypersensitivity; Dizziness, headache concurrent use of sildenafil, vardenafil or CV: hypotension, tadalafil. tachycardia, paradoxic bradycardia, syncope Use cautiously in volume depleted patients; right GI: ventricular infarction; nausea, vomiting hypertrophic cardiomyopathy CONTRADICATION Drug Interaction: Concurrent use of sildenafil, tadalafil, or vardenafil may result in significant and potentially fatal hypotension.
NURSING RESPONSIBILITIES Before: Check doctors order. Review drug preparation. Assess for clients heart rate. Inform therapeutic effect. Check venoclysis patency. During: Observe rights of administration. Administer drug on time. Monitor BP closely during administration. Assess for patients pain. Inform patient of the possible adverse/side effects of drug. After: Monitor BP and heart rate hourly. Assess for patients pain levels. bedrest. Advised to avoid activity that requires mental alertness. Notify health care professionals if no improvement w/in a few days.
Half-Life: 5 hrs Source: Deglin J. H., Vallerand A. H. (2008). Daviss Drug Guide for Nurses. (11th ed., pp. 707 708) 1915 Arch Street Philadelphia, PA 19103: F.A Davis Company. DOI: www.fadavis.com
DRUG DATA Generic Name: MAGNESIUM SULFATE Trade Name: Elin Magnesium Sulfate Patients Dose: n/a Minimum Dose: 1 - 6g /day Maximum Dose: 8 12g / day Availability: Tablets, Injection, Solution Route of Administration: IV, IM, PO
CLASSIFICATION Therapeutic: Mineral and electrolyte repalcements / supplements
MECHANISM OF ACTION Essential for the activity of many enzymes. Plays an important role in neurotransmission and muscular excitability.
INDICATION General: Treatment/prevention of hypomagnesemia. Treatment of hypertension. Anticonvulsant associated severe eclampsia, preeclampsia, or acute nephritis.
Pharmacologic Therapeutic: Mineral/electrolytes Replacements in deficiency states. Pregnancy Risk Resolution of Category: eclampsia. D Onset: immediate Peak: unknown Duration: 30 mins Half-Life: unknown
ADVERSE/SIDE EFFECTS Contraindicated in CNS: hypermagnesemia; Drowsiness hypocalcemia; Anuria; Hear block; Respi: decreased respiratory rate Use cautiously in any degree of renal CV: arrhythmias, insufficiency; Digitalized bradycardia, patients. hypotension CONTRADICATION Drug Interaction: GI: Potentiate calcium channel diarrhea blockers and neuromuscular blocking agents.
NURSING RESPONSIBILITIES Before: Check doctors order. Review drug preparation. Assess for clients heart rate. Inform therapeutic effect. Check venoclysis patency. During: Observe rights of administration. Administer drug on time. Monitor BP closely during administration. Assess for patients pain. Inform patient of the possible adverse/side effects of drug. After: Monitor BP and heart rate hourly. Monitor for Ca, Mg, K levels. Monitor for renal function. Advised to avoid activity that requires mental alertness. Notify health care professionals if no improvement w/in a few days.
Source: Deglin J. H., Vallerand A. H. (2008). Daviss Drug Guide for Nurses. (11th ed., pp. 768 357) 1915 Arch Street Philadelphia, PA 19103: F.A Davis Company. DOI: www.fadavis.com
DRUG DATA Generic Name: MEPERIDINE
CLASSIFICATION Therapeutic: Opiod analgesics
Before: Check doctors order. Review drug preparation. Trade Name: Assess for clients heart rate. Demerol Inform therapeutic effect. Pharmacologic Check venoclysis patency. Patients Dose: Opiod agonists Use cautiously in head During: n/a trauma; increased ICP; Observe rights of Pregnancy Risk severe renal, hepatic or EENT: blurred vision, administration. Minimum Dose: Category: Therapeutic: pulmonary disease diplopia, miosis. Administer drug on time. 50mg c Decrease in severity Monitor BP closely during of pain. Drug Interaction: Resp: respiratory administration. Maximum Dose: Potentiate calcium channel depression. Assess for patients pain. 150mg Onset: blockers and Inform patient of the possible immediate neuromuscular blocking CV: hypotension, adverse/side effects of drug. Availability: agents. bradycardia. After: Tablets, Injection, Peak: Instruct to change position Solution 5 7 mins GI: constipation, slowly. nausea, vomiting. Instruct to lie down when Route of Administration: Duration: feeling nauseated. IV, IM, PO 2 3 hrs Monitor for renal function. Advised to avoid activity that Half-Life: requires mental alertness. 2.5 4 hrs Notify health care professionals if no improvement w/in a few days. th Source: Deglin J. H., Vallerand A. H. (2008). Daviss Drug Guide for Nurses. (11 ed., pp. 784 357) 1915 Arch Street Philadelphia, PA 19103: F.A Davis Company. DOI: www.fadavis.com
MECHANISM OF ACTION Binds to opiate receptor in the CNS. Alters the perception of and response to painful stimuli, while producing generalized CNS depression.
INDICATION General: Moderate or severe pain (alone or with nonopiod agent). Anesthesia adjunct.
CONTRADICATION Contraindicated in hypersensitivity; hypersensitivity to bisulfites (some injectable products)
ADVERSE/SIDE EFFECTS CNS: SEIZURES, confusion, sedation, dysphoria, euphoria, floating feeling, hallucinations, headache, unusual dreams.
NURSING RESPONSIBILITIES
DRUG DATA Generic Name: METOCLOPRAMIDE Trade Name: Apo-Metoclop, Clopra Patients Dose: n/a Minimum Dose: 5mg Maximum Dose: 10mg Availability: Tablets, Injection, Solution Route of Administration: IV, IM, PO
CLASSIFICATION Therapeutic: antiemetics
Pregnancy Risk Category: B
MECHANISM OF ACTION Blocks dopamine receptors in chemoreceptor trigger zone of the CNS. Stimulates motility of the upper GI tract and accelerates gastric emptying.
INDICATION
CONTRADICATION Contraindicated in hypersensitivity; hypersensitivity to bisulfites (some injectable products) Use cautiously in head trauma; increased ICP; severe renal, hepatic or pulmonary disease Drug Interaction: Potentiate calcium channel blockers and neuromuscular blocking agents.
General: Prevention of chemotherapy-induced emesis. Treatment of postsurgical and diabetic gastric stasis. Facilitation of small bowel intubation in radiographic procedures. Therapeutic: Management of Decreased nausea esophagealreflux. and vomiting. Treatment and Decreased prevention of symptoms of gastric postoperative nausea stasis. and vomiting when nasogastric suctioning is Onset: undesirable. Unlabeled 1 3 min uses: Treatment of hiccups. Adjunct Peak: management of immediate migraine headaches. Duration: 1 2 hrs Half-Life: 2.5 6 hrs
ADVERSE/SIDE EFFECTS CNS: drowsiness, extrapyramidal reactions, restlessness, NEUROLEPTIC MALIGNANT SYNDROME, anxiety, depression, irritability, tardive dyskinesia. CV: arrhythmias (supraventricular tachycardia, bradycardia), hypertension, hypotension. GI: constipation, diarrhea, dry mouth, nausea.
NURSING RESPONSIBILITIES Before: Check doctors order. Review drug preparation. Assess for clients heart rate. Inform therapeutic effect. Check venoclysis patency. During: Observe rights of administration. Administer drug on time. Monitor BP closely during administration. Assess for patients pain. Inform patient of the possible adverse/side effects of drug. After: Instruct to change position slowly. Instruct to lie down when feeling nauseated. Keep diphenhydramine injection ready. Advised to avoid activity that requires mental alertness. Notify health care professionals if no improvement w/in a few days.
Source: Deglin J. H., Vallerand A. H. (2008). Daviss Drug Guide for Nurses. (11th ed., pp. 810 812) 1915 Arch Street Philadelphia, PA 19103: F.A Davis Company. DOI: www.fadavis.com
DRUG DATA Generic Name: MIDAZOLAM Trade Name: Dormicum Patients Dose: n/a Minimum Dose: 1mg Maximum Dose: 3.5mg Availability: Tablets, Injection, Solution Route of Administration: IV, IM, PO
CLASSIFICATION Therapeutic: Antianiety agents
Pharmacologic: benzodiazepines
MECHANISM OF ACTION Acts at many levels of the CNS to produce generalized CNS depression. Effects may be mediatedby GABA, an inhibitory neurotransmitter. Therapeutic: Short-term sedation. Postoperative amnesia. Onset: 1 3 min Peak: immediate Duration: 1 2 hrs Half-Life: 2.5 6 hrs
INDICATION General: Provides sedation/ anxiolysis/ amnesia during therapeutic, diagnostic, or radiographic procedures (conscious sedation). Aids in the induction of anesthesia and as part of balanced anesthesia. As a continuous infusion, provides sedation of mechanically ventilated patients during anesthesia or in a critical care setting, Status epilepticus.
Pregnancy Risk Category: B
ADVERSE/SIDE EFFECTS Contraindicated in: CNS: agitation, Hypersensitivity; drowsiness, excess Crosssensitivity with other sedation, headache. benzodiazepinesmay occur; Shock; Comatose patients EENT: blurred vision. or those with pre-existing CNS depression; Resp: APNEA, Uncontrolled severe pain; LARYNGOSPASM, Products containing benzyl RESPIRATORY alcohol should not be used DEPRESSION, in neonates; bronchospasm, coughing. Use Cautiously in: Pulmonary disease; CHF; CV: CARDIAC ARREST, Renal impairment; Severe arrhythmias. hepatic impairment; Obese pediatric patients GI: hiccups, nausea, (calculate dose on the vomiting. Chronicbasis of ideal body weight); CONTRADICATION Drug Interaction: Increase CNS depression with alcohol, inantihistamines, opioid analgesics, and other sedative/hypnotics (midazolam dose by30 50% if used concurrently).
NURSING RESPONSIBILITIES Before: Check doctors order. Review drug preparation. Assess for clients heart rate. Inform therapeutic effect. Check venoclysis patency. During: Observe rights of administration. Administer drug on time. Monitor BP closely during administration. Assess for patients pain. Inform patient of the possible adverse/side effects of drug. After: Instruct to change position slowly. monitor IV site for extravasation. Arrange to reduce dose if given opion analgesics. Advised to avoid activity that requires mental alertness. Notify health care professionals if no improvement w/in a few days.
Source: Deglin J. H., Vallerand A. H. (2008). Daviss Drug Guide for Nurses. (11th ed., pp. 822 825) 1915 Arch Street Philadelphia, PA 19103: F.A Davis Company. DOI: www.fadavis.com
DRUG DATA Generic Name: MORPHINE
CLASSIFICATION Therapeutic: Antianiety agents
Before: Check doctors order. Review drug preparation. Trade Name: Assess for clients heart rate. none Inform therapeutic effect. Pharmacologic: Check venoclysis patency. Patients Dose: benzodiazepines During: n/a Observe rights of Use Cautiously in: Head EENT: blurred vision, administration. Minimum Dose: Therapeutic: trauma; Increased diplopia,miosis. Administer drug on time. 5mg Pregnancy Risk Decrease in severity intracranial pressure; Monitor BP closely during Category: of pain. Severe renal, hepatic, or Resp: RESPIRATORY administration. Maximum Dose: B pulmonary disease; DEPRESSION. Assess for patients pain. 20mg Onset: Hypothyroidism; Adrenal Inform patient of the possible rapid insufficiency; History of CV: hypotension, adverse/side effects of drug. Availability: substance abuse; bradycardia. After: Tablets, Injection, Peak: Instruct to change position Solution 20 mins Drug Interaction: GI: constipation, slowly. Use with extreme caution nausea, vomiting. monitor IV site for Route of Administration: Duration: in patients extravasation. IV, IM, PO 4 5 hrs receiving MAO inhibitors Arrange to reduce dose if given within 14 days prior (may opion analgesics. Half-Life: result in unpredictable, Advised to avoid activity that 2 4 hrs severe reactionsdecrease requires mental alertness. initial dose of morphine to Notify health care professionals 25% of usual dose). if no improvement w/in a few days. Source: Deglin J. H., Vallerand A. H. (2008). Daviss Drug Guide for Nurses. (11th ed., pp. 843 847) 1915 Arch Street Philadelphia, PA 19103: F.A Davis Company. DOI: www.fadavis.com
MECHANISM OF ACTION Binds to opiate receptors in the CNS. Alters the perception of and response to painful stimuli while producing generalized CNS depression.
INDICATION
CONTRADICATION
General: Contraindicated in: Severe Pain. Pulmonary Hypersensitivity; Some edema. Pain Associated products contain with MI. tartrazine, bisulfites, or alcohol and should be avoided in patients with known hypersensitivity.
ADVERSE/SIDE EFFECTS CNS: confusion, sedation, dizziness, dysphoria, euphoria, floating feeling, hallucinations, headstartache, unusual dreams.
NURSING RESPONSIBILITIES
DRUG DATA Generic Name: MORPHINE Trade Name: none Patients Dose: n/a Minimum Dose: 0.5mg Maximum Dose: 2.2mg Availability: Tablets, Injection, Solution Route of Administration: IV, IM, PO
CLASSIFICATION Therapeutic: Antianginals, antihypertensive
Pharmacologic: Calcium channel blockers
MECHANISM OF ACTION Inhibits the transport of calcium into myocardial and vascular smooth muscle cells, resulting in inhibition of excitationcontraction coupling and subsequent contraction. Therapeutic: Systemic vasodilation resulting in decreased blood pressure. Coronary vasodilation resulting in decreased frequency and severity of attacks of angina. Onset: Within min Peak: 45 mins Duration: 50 hrs Half-Life: 2 4 hrs
INDICATION General: Management of: Hypertension, Angina pectoris, Vasospastic (Prinzmetals) angina. Unlabeled buses: Management of CHF.
CONTRADICATION Contraindicated in: Hypersensitivity; Sick sinus syndrome; 2nd- or 3rddegree AV block (unless an artificial pacemaker is in place); BP <90mmHg; Advanced aortic stenosis. Use Cautiously in: Severe hepatic impairment
Pregnancy Risk Category: c
Before: Check doctors order. Review drug preparation. Assess for clients heart rate. Inform therapeutic effect. Check venoclysis patency. During: Observe rights of administration. Administer drug on time. Use Cautiously in: Severe EENT: blurred vision, Monitor BP closely during hepatic impairment (dose disturbed equilibrium, administration. reduction recommended); epistaxis, tinnitus. Assess for patients pain. Inform patient of the possible Drug Interaction: Resp: cough, dyspnea, adverse/side effects of drug. Additive hypotensionmay shortness of breath. After: occur when used Instruct to change position concurrently with fentanyl, CV: ARRHYTHMIAS, slowly. other antihypertensives, CHF, peripheral monitor IV site for nitrates, acute ingestion of edema, bradycardia, extravasation. alcohol, or quinidine. chest pain, Arrange to reduce dose if given Antihypertensive effects hypotension, opion analgesics. may beby concurrent use Advised to avoid activity that of NSAIDs. Concurrent use requires mental alertness. with beta blockers, digoxin Notify health care professionals if no improvement w/in a few days.
ADVERSE/SIDE EFFECTS CNS: abnormal dreams, anxiety, confusion, dizziness, drowsiness, headache, jitteriness, nervousness, psychiatric disturbances, weakness.
NURSING RESPONSIBILITIES
Source: Deglin J. H., Vallerand A. H. (2008). Daviss Drug Guide for Nurses. (11th ed., pp. 879 881) 1915 Arch Street Philadelphia, PA 19103: F.A Davis Company. DOI: www.fadavis.com
Vous aimerez peut-être aussi
- Drug StudyDocument5 pagesDrug StudyRai D. MacapantonPas encore d'évaluation
- The Cardiovascular System ReviewDocument18 pagesThe Cardiovascular System ReviewDanisha Reeves100% (1)
- HNN215 Drug Diary GuideDocument10 pagesHNN215 Drug Diary GuideMaddison MitchellPas encore d'évaluation
- Emergency Drugs Crash CartDocument14 pagesEmergency Drugs Crash CartEricson SomeraPas encore d'évaluation
- Management of diabetic ketoacidosis: principles of management in the first hourDocument13 pagesManagement of diabetic ketoacidosis: principles of management in the first hourAzim Abd RazakPas encore d'évaluation
- 25 Cardiovascular DiseaseDocument35 pages25 Cardiovascular DiseaseBramantyo NugrosPas encore d'évaluation
- Common Emergency DrugsDocument58 pagesCommon Emergency Drugshatem alsrour84% (19)
- UFO Midwest Magazine April2011Document16 pagesUFO Midwest Magazine April2011Jimi HughesPas encore d'évaluation
- Er DrugsDocument15 pagesEr DrugsDays AniarPas encore d'évaluation
- Common Emergency DrugsDocument48 pagesCommon Emergency Drugshady920100% (1)
- ER DRUGS AT A GLANCEDocument3 pagesER DRUGS AT A GLANCEmyleneacar100% (3)
- Prepared By: Madi, Krister: Salvador, Ma. Grace BSN-4ADocument36 pagesPrepared By: Madi, Krister: Salvador, Ma. Grace BSN-4ATap Tap100% (2)
- DrugcardsDocument70 pagesDrugcards2liter100% (2)
- CardDocument2 pagesCardAngeline EspinasPas encore d'évaluation
- Emergency DrugsDocument11 pagesEmergency Drugsthenursingcorner96% (24)
- Drug Study For PneumoniaDocument15 pagesDrug Study For PneumoniaPrincess Pauline Abrasaldo100% (1)
- 37 Operational Emergency and Abnormal ProceduresDocument40 pages37 Operational Emergency and Abnormal ProceduresLucian Florin ZamfirPas encore d'évaluation
- Medical Surgical Nursing Common Drugs and Its AntidotesDocument2 pagesMedical Surgical Nursing Common Drugs and Its AntidotesJhannPas encore d'évaluation
- Crash Cart Drugs: A Review of Medications Used in Cardiac ArrestDocument23 pagesCrash Cart Drugs: A Review of Medications Used in Cardiac ArrestKristiina MakinenPas encore d'évaluation
- 24 Emergency DrugsDocument7 pages24 Emergency DrugsApple BelicanPas encore d'évaluation
- Drug Study On Emergency DrugsDocument14 pagesDrug Study On Emergency Drugsjcarysuitos100% (4)
- Eating and HealingDocument19 pagesEating and HealingMariana CoriaPas encore d'évaluation
- Oxytocin Nursing Care Guide: Uses, Side Effects & ResponsibilitiesDocument10 pagesOxytocin Nursing Care Guide: Uses, Side Effects & ResponsibilitiesCieLouie Cauilan-DomingoPas encore d'évaluation
- Emergency Drugs: Cardiac Drugs Atropine SulfateDocument14 pagesEmergency Drugs: Cardiac Drugs Atropine SulfateJayvee Montoya-Pujante100% (1)
- Emergency Pharmacology Drugs GuideDocument5 pagesEmergency Pharmacology Drugs GuideAce RegellanaPas encore d'évaluation
- Emergency DrugsDocument15 pagesEmergency Drugsjheverly123100% (1)
- Digoxin Drug CardDocument1 pageDigoxin Drug CardMahsa Ahmadzadeh100% (2)
- Medication CardsDocument5 pagesMedication CardsAndrew Harrison Lewis0% (1)
- Emergency Drugs: (A Drug Study)Document13 pagesEmergency Drugs: (A Drug Study)Marichu BajadoPas encore d'évaluation
- Pathways-Childrens Ministry LeaderDocument16 pagesPathways-Childrens Ministry LeaderNeil AtwoodPas encore d'évaluation
- Arcelor Mittal - Bridges PDFDocument52 pagesArcelor Mittal - Bridges PDFShamaPas encore d'évaluation
- StrokeDocument17 pagesStrokeMirza Shaharyar BaigPas encore d'évaluation
- Anes Drugs TableDocument20 pagesAnes Drugs TableKathleen Grace ManiagoPas encore d'évaluation
- MINI CP Angina PectorisDocument11 pagesMINI CP Angina Pectorisyasira100% (1)
- Drug Study Er MedsDocument12 pagesDrug Study Er MedsJerald S. OlaloPas encore d'évaluation
- BiperidenDocument3 pagesBiperidenKaren T. Celetaria100% (1)
- CefuroximeDocument6 pagesCefuroximetrinkets0914Pas encore d'évaluation
- Hypertensive Crisis PathoDocument4 pagesHypertensive Crisis PathoJanelle Dela CruzPas encore d'évaluation
- Adult Immediate Post Cardiac Arrest Care Algorithm 2015 UpdateDocument1 pageAdult Immediate Post Cardiac Arrest Care Algorithm 2015 UpdateRyggie Comelon0% (1)
- Er-Drug StudyDocument41 pagesEr-Drug Studyrc_lacampuinganyahooPas encore d'évaluation
- Syringe Driver / Syringe Pump: By: Lacsamana, Joan Noemy CDocument6 pagesSyringe Driver / Syringe Pump: By: Lacsamana, Joan Noemy CMr. Christian ParabuacPas encore d'évaluation
- Isosorbide NitratesDocument3 pagesIsosorbide Nitratesapi-3797941Pas encore d'évaluation
- Drug StudyDocument3 pagesDrug StudyKwin SaludaresPas encore d'évaluation
- EpinephrineDocument1 pageEpinephrineKathrina IoannouPas encore d'évaluation
- Head InjuryDocument5 pagesHead InjuryJames Jayson Liberto100% (3)
- IV Fluid CalculationDocument7 pagesIV Fluid Calculationemyjones0% (1)
- Neurogenic ShockDocument11 pagesNeurogenic Shocklulu voxPas encore d'évaluation
- Drug Cards (PDF Library)Document5 pagesDrug Cards (PDF Library)Jim Stewart0% (2)
- AtivanDocument1 pageAtivanSheri490Pas encore d'évaluation
- Narrative PathophysiologyDocument18 pagesNarrative PathophysiologyNica Georgelle Maniego SamontePas encore d'évaluation
- FlagylDocument3 pagesFlagylAdrianne BazoPas encore d'évaluation
- Cardiac Arrhythmias Drug AmiodaroneDocument7 pagesCardiac Arrhythmias Drug AmiodaroneMarie Angeline ManzanoPas encore d'évaluation
- Ischemic Heart DiseaseDocument8 pagesIschemic Heart Diseaseiri_balPas encore d'évaluation
- Drug Class:: Prototype (Generic/Trade) : Eskalith, LithobidDocument1 pageDrug Class:: Prototype (Generic/Trade) : Eskalith, LithobidAaLona Robinson100% (2)
- Non-Variceal Upper GI Bleeding GuideDocument34 pagesNon-Variceal Upper GI Bleeding GuideChe Ainil ZainodinPas encore d'évaluation
- Pathophysiology ErDocument3 pagesPathophysiology ErAlexa A. AldayPas encore d'évaluation
- A Simple Guide to Abdominal Aortic Aneurysm, Diagnosis, Treatment and Related ConditionsD'EverandA Simple Guide to Abdominal Aortic Aneurysm, Diagnosis, Treatment and Related ConditionsPas encore d'évaluation
- For Drug Recitation 1Document33 pagesFor Drug Recitation 1Abigail LonoganPas encore d'évaluation
- Drug StudyDocument17 pagesDrug StudyKenneth ManalangPas encore d'évaluation
- Amlodipine, Vit.b Complex, CombiventDocument6 pagesAmlodipine, Vit.b Complex, CombiventErickson Caisido GarciaPas encore d'évaluation
- VIII. Drug StudyDocument11 pagesVIII. Drug StudyCharlayne AnnePas encore d'évaluation
- Drug 25Document17 pagesDrug 25carol_gigliotti24100% (1)
- Drug-Study MethyldopaDocument4 pagesDrug-Study MethyldopamayangernszPas encore d'évaluation
- Drug Study No.1 Brand Name: Paracetamol Generic Name: Tempra Classification: Anti-Infectives Dosage: 100mg, 1ml Drops q4hrDocument7 pagesDrug Study No.1 Brand Name: Paracetamol Generic Name: Tempra Classification: Anti-Infectives Dosage: 100mg, 1ml Drops q4hrMary EnsomoPas encore d'évaluation
- Medication Worksheet: (You Will Need To Make Additional Copies of This Form)Document2 pagesMedication Worksheet: (You Will Need To Make Additional Copies of This Form)mcarter402100% (1)
- Badminton Lesson 1 4 - 5 Grade: TH THDocument31 pagesBadminton Lesson 1 4 - 5 Grade: TH THLoxcey LopezPas encore d'évaluation
- Rivalry and Central PlanningDocument109 pagesRivalry and Central PlanningElias GarciaPas encore d'évaluation
- Hilton 5-29 Case SolutionDocument4 pagesHilton 5-29 Case SolutionPebbles RobblesPas encore d'évaluation
- Module 5 Communication & Change MGT - HS Planning & Policy Making ToolkitDocument62 pagesModule 5 Communication & Change MGT - HS Planning & Policy Making ToolkitKristine De Luna TomananPas encore d'évaluation
- Modification Adjustment During Upgrade - Software Logistics - SCN WikiDocument4 pagesModification Adjustment During Upgrade - Software Logistics - SCN Wikipal singhPas encore d'évaluation
- Lignan & NeolignanDocument12 pagesLignan & NeolignanUle UlePas encore d'évaluation
- Purp Com Lesson 1.2Document2 pagesPurp Com Lesson 1.2bualjuldeeangelPas encore d'évaluation
- Research of William Wells at HarvardDocument10 pagesResearch of William Wells at HarvardARGHA MANNAPas encore d'évaluation
- BILL of Entry (O&A) PDFDocument3 pagesBILL of Entry (O&A) PDFHiJackPas encore d'évaluation
- Data Sheet FC SIDocument2 pagesData Sheet FC SIAndrea AtzeniPas encore d'évaluation
- Service: Audi A6 1998Document256 pagesService: Audi A6 1998Kovács EndrePas encore d'évaluation
- Extraform RsDocument47 pagesExtraform RsCarlos David Duran AvilaPas encore d'évaluation
- CONNECTIFYDocument3 pagesCONNECTIFYAbhishek KulshresthaPas encore d'évaluation
- EE114-1 Homework 2: Building Electrical SystemsDocument2 pagesEE114-1 Homework 2: Building Electrical SystemsGuiaSanchezPas encore d'évaluation
- Government of The Punjab Primary & Secondary Healthcare DepartmentDocument3 pagesGovernment of The Punjab Primary & Secondary Healthcare DepartmentYasir GhafoorPas encore d'évaluation
- BE 510 Business Economics 1 Problem Set 5 SolutionsDocument5 pagesBE 510 Business Economics 1 Problem Set 5 SolutionsCreative Work21stPas encore d'évaluation
- Matador - : Medical Advanced Training in An Artificial Distributed EnvironmentDocument25 pagesMatador - : Medical Advanced Training in An Artificial Distributed EnvironmentNauman ChaudaryPas encore d'évaluation
- KG ResearchDocument257 pagesKG ResearchMuhammad HusseinPas encore d'évaluation
- Biotechnology Eligibility Test (BET) For DBT-JRF Award (2010-11)Document20 pagesBiotechnology Eligibility Test (BET) For DBT-JRF Award (2010-11)Nandakumar HaorongbamPas encore d'évaluation
- Teacher Commitment and Dedication to Student LearningDocument8 pagesTeacher Commitment and Dedication to Student LearningElma Grace Sales-DalidaPas encore d'évaluation
- Mapeflex Pu50 SLDocument4 pagesMapeflex Pu50 SLBarbara Ayub FrancisPas encore d'évaluation
- Evolution BrochureDocument4 pagesEvolution Brochurelucas28031978Pas encore d'évaluation
- Climate Change in Bryce CanyonDocument8 pagesClimate Change in Bryce CanyonClaire CrisePas encore d'évaluation
- SCIENCE 5 PERFORMANCE TASKs 1-4 4th QuarterDocument3 pagesSCIENCE 5 PERFORMANCE TASKs 1-4 4th QuarterBALETE100% (1)
- VFD ManualDocument187 pagesVFD ManualgpradiptaPas encore d'évaluation