Académique Documents
Professionnel Documents
Culture Documents
Logan's Pharmacology Handy Notes PDF
Transféré par
tadiwanashe loganTitre original
Copyright
Formats disponibles
Partager ce document
Partager ou intégrer le document
Avez-vous trouvé ce document utile ?
Ce contenu est-il inapproprié ?
Signaler ce documentDroits d'auteur :
Formats disponibles
Logan's Pharmacology Handy Notes PDF
Transféré par
tadiwanashe loganDroits d'auteur :
Formats disponibles
LOGANS PHARMACOLOGY HANDY NOTES
1ST EDITION 2013
Tadiwanashe logan;tadiwanashe2@ovi.com
HARARE INSTITUTE OF TECHNOLOGY | DEPARTMENT OF PHARMACY
1. A Textbook of Clinical Pharmacology and Therapeutics FIFTH EDITION 2. Vander et al's Human Physiology: the mechanisms of body function 9th Edition
Acetylcholine Acetylcholine (ACh) is a major neurotransmitter in the peripheral nervous system at the neuromuscular junction and in the brain. Fibers that release ACh are called cholinergic fibres. The cell bodies of the brains cholinergic neurons are concentrated in relatively few areas, but their axons are widely distributed. Acetylcholine (ACh) is synthesized from choline and acetyl coenzyme A in the cytoplasm of synaptic terminals and stored in synaptic vesicles. After it is released and activates receptors on the postsynaptic membrane, the concentration of ACh at the postsynaptic membrane is reduced (thereby stopping receptor activation) by the enzyme acetylcholinesterase. This enzyme is located on the pre- and postsynaptic membranes and rapidly destroys ACh, releasing choline and acetate. The choline is then transported back into the presynaptic axon terminals where it is reused in the synthesis of new ACh. The ACh concentration at the receptors is also reduced by simple diffusion away from the synapse and eventual breakdown of the molecule by an enzyme in the blood. One biological weapon, the nerve gas Sarin, inhibits acetylcholinesterase, causing a build-up of ACh in the synaptic cleft. This results in over-stimulation of postsynaptic ACh receptors, rapidly making them insensitive and inducing paralysis. There are two types of ACh receptors, and they are distinguished by their responsiveness to two different drugs. Recall that although a receptor is considered specific for a given ligand,
such as ACh, most receptors will recognize natural or synthetic compounds that contain some degree of chemical similarity to that ligand. Some ACh receptors respond not only to acetylcholine but to the drug nicotine and, therefore, have come to be known as nicotinic receptors. The nicotinic receptor is an excellent example of a receptor that itself contains an ion channel (I. e., a ligand-gated channel); in this case the channel is selective for both sodium and potassium ions. Nicotinic receptors are present at the neuromuscular junction and, as will be covered in Chapter 9, several nicotinic receptor antagonists are toxins that induce ++paralysis. Nicotinic receptors in the brain are important in cognitive functions. For example, one cholinergic sys-tem that employs nicotinic receptors plays a major role in attention, learning, and memory by reinforcing the ability to detect and respond to meaningful stimuli. Neurons associated with the ACh system degenerate in people with Alzheimers disease, a brain disease that is usually age-related and is the most common cause of declining intellectual function in late life. Alzheimers disease affects 10 to 15 percent of people over age 65, and 50 percent of people over age 85. Because of the de-generation of cholinergic neurons, this disease is associated with a decreased amount of ACh in certain areas of the brain and even the loss of the postsynaptic neurons that would have responded to it. These defects and those in other neurotransmitter systems that are affected in this disease are related to the declining language and perceptual abilities, confusion, and memory loss that characterize Alzheimers victims. The exact causes of this degeneration are unknown. The other type of cholinergic receptor is stimulated not only by acetylcholine but by the mushroom poison muscarine; therefore, these are called muscarinic receptors. These receptors couple with G proteins, which then alter the activity of a number of different enzymes and ion channels. They are prevalent at cholinergic synapses in the brain and at junctions of neurons that innervate several glands and organs, notably the heart.
Biogenic Amines The biogenic amines are small charged molecules that are synthesized from amino acids and contain an amino group (RNH2). The most common biogenic amines are dopamine, norepinephrine, serotonin, and histamine. Epinephrine, another biogenic amine, is not a common neurotransmitter in the central nervous sys-tem but is the major hormone secreted by the adrenal medulla. Norepinephrine is an important neurotransmitter in both the central and peripheral components of the nervous system.
Catecholamines Dopamine, norepinephrine (NE), and epinephrine all contain a catechol ring (a six-carbon ring with two adjacent hydroxyl groups) and an amine group; thus they are called catecholamines. The catecholamines are formed from the amino acid tyrosine and share the same two initial steps in their synthetic path-way (Figure 633). Synthesis of catecholamines be-gins with the uptake of tyrosine by the axon terminals
and its conversion to another precursor, L-dihydroxy-phenylalanine (L-dopa) by the rate-limiting enzyme in the pathway, tyrosine hydroxylase. Depending on the enzymes present in the terminals, any one of the three catecholamines may ultimately be released. Synthesis and release of the catecholamines are strongly modulated by auto receptors on the presynaptic terminals. After activation of the receptors on the postsynaptic cell, the catecholamine concentration in the synaptic cleft declines, mainly because the catecholamine is actively transported back into the axon terminal by a membrane transporter protein. The catecholamine neurotransmitters are also broken down in both the extracellular fluid and the axon terminal by enzymes such as monoamine oxidase (MAO).MAO inhibitors increase the amount of norepinephrine and dopamine in a synapse by slowing their metabolic degradation. They are used in the treatment of diseases such as depression and anxiety. Within the central nervous system, the cell bodies of the catecholamine-releasing neurons lie in parts of the brain called the brainstem and hypothalamus. Although relatively few in number, their axons branch greatly and may go to virtually all parts of the brain and spinal cord. During the early experiments on norepinephrine and epinephrine, norepinephrine was mistakenly taken to be epinephrine, and epinephrine was called by its British name adrenaline. Consequently, nerve fibres that release epinephrine or norepinephrine came to be called adrenergic fibres. Norepinephrine-releasing fibres are also called noradrenergic.
There are two major classes of receptors for norepinephrine and epinephrine: alpha-adrenergic receptors and beta-adrenergic receptors (these are also called alpha-adrenoceptors and betaadrenoceptors). All catecholamines receptors are metabotropic, that is, they act by initiating metabolic processes that affect cellular function. As such, they all use second messengers to transfer a signal from the surface of the cell to the cytoplasm. Beta-adrenoceptors act via stimulatory G proteins to increase cAMP in the postsynaptic cell. There are three subclasses of beta-receptors, beta 1, beta 2, and beta 3, which function in different ways in different tissues (see Table 613). Alpha-adrenoceptors exist in two sub-classes, alpha 1 and alpha 2. They act presynaptically to inhibit norepinephrine release (alpha 2) or postsynaptically to either stimulate or inhibit activity at different types of potassium channels (alpha 1). The subclasses of alpha- and beta-receptors are distinguished by the drugs that influence them and their secondmessenger systems
Serotonin While not a catecholamine, serotonin (5-hydroxytryptamine, or 5-HT) is an important biogenic amine. It is produced from tryptophan, an essential amino acid. Its effects generally have a slow onset, indicating that it works as a neuromodulator. Serotonin-releasing neurons in-nervate virtually every structure in the brain and spinal cord and operate via at least 16 different receptor types In general, serotonin has an excitatory effect on pathways that are involved in the control of muscles, and an inhibitory effect on pathways that mediate sensations. The activity of serotonergic neurons is lowest or absent during sleep and highest during states of alert wakefulness. In addition to their contributions to motor activity and sleep, serotonergic pathways also function in the regulation of food intake, reproductive behaviour, and emotional states such as mood and anxiety. Serotonin reuptake blockers such as fluoxetine are thought to aid in the treatment of depression by inactivating the 5-HT transporter and increasing the synaptic concentration of the neurotransmitter. Interestingly, such drugs are often associated with decreased appetite. This is one example of how the use of reuptake inhibitors for a specific neurotransmitterone with widespread actionscan cause numerous unwanted side effects. The drug lysergic acid diethylamide (LSD) is thought to block serotonin receptors in the brain, thereby preventing normal serotonergic neurotransmission. However, it is not clear how this action produces the intense visual hallucinations that are produced by ingestion of this drug. Serotonin is also present in many nonneural cells (for example, blood platelets and certain cells of the immune system and digestive tract). In fact, the brain contains only 1 to 2 percent of the bodys serotonin and other conditions of low oxygen availability. The NMDA receptor is the site of action of a number of mind-altering drugs, such as phencyclidine (PCP, angel dust). GABA (gamma-aminobutyric acid) and the amino acid glycine are the major inhibitory neurotransmitters in the central nervous system. (GABA is not one of the 20 amino acids used to build proteins, but because it is a modified form of glutamate, it is classified with the amino acid neurotransmitters.) With few exceptions, GABA neurons in the brain are small interneurons that dampen activity within a neural circuit. Postsynaptically, GABA may bind to ionotropic or metabotropic receptors. The ionotropic receptor increases chloride flux into the cell, resulting in hyperpolarization of the postsynaptic membrane. In addition to the GABA binding site, this receptor has several additional binding sites for other compounds, including steroids, barbiturates, and benzodiazepines. Benzodiazepine drugs such as Valium reduce anxiety, guard against seizures, and induce sleep by increasing chloride flux through the GABA receptor.
GABA (gamma-aminobutyric acid) -Aminobutyric acid (GABA) acts as an inhibitory neurotransmitter by opening chloride channels that lead to hyper-polarization and suppression of epileptic discharges. In addition to the receptor site for GABA, the GABA receptorchannel complex includes benzodiazepine and barbiturate recognition sites which can potentiate GABA anti-epileptic activity. Vigabatrin (vinyl--aminobutyric acid) irreversibly inhibits GABA transaminase, the enzyme that inactivates GABA. The resulting increase in synaptic GABA probably explains its anti-epileptic activity. Glutamate is an excitatory neurotransmitter. A glutamate receptor, the N-methyl-D-aspartate (NMDA) receptor, is important in the genesis and propagation of high-frequency discharges. Lamotrigine inhibits glutamate release and has anticonvulsant activity
Histamine Histamine is widely distributed in the body and is derived from the decarboxylation of histidine. It is concentrated in mast-cell and basophil granules. The highest concentrations are found in the lung, nasal mucous membrane, skin, stomach and duodenum (i.e. at interfaces between the body and the outside environment). Histamine is liberated by several basic drugs (usually when these are given in large quantities intravenously), including tubocurarine, morphine, codeine, vancomycin and suramin. Its an inflammatory mediator secreted mainly by mast cells; acts on microcirculation to cause vasodilation and increased permeability to protein. Histamine has a powerful vasodilator effect on the arterioles and, like bradykinin, has the ability to increase greatly capillary porosity, allowing leakage of both fluid and plasma protein into the tissues. In many pathological conditions, the intense arteriolar dilation and increased capillary porosity produced by histamine cause tremendous quantities of fluid to leak out of the circulation into the tissues, inducing edema. The local vasodilatory and edema-producing effects of histamine are especially prominent during allergic reactions.
We have two classes of histamine receptors, H1-RECEPTORS In humans, stimulation of H1 receptors causes dilatation of small arteries and capillaries, together with increased permeability, which leads to formation of oedema. Histamine induces vascular endothelium to release nitric oxide, which causes vasodilatation and lowers systemic blood pressure. Inhaled histamine induces bronchospasm. In foetal vessels (e.g. the umbilical artery), histamine causes vasoconstriction. Histamine contributes to the triple response to mechanical stimulation of the skin which consists of localized pallor, which gives way to a wheal (localized oedema caused by increased vessel permeability and attributable to histamine) surrounded by a more distant and slowly developing flare (due to arteriolar dilatation via an axon-reflex mechanism and involving tachykinins such as substance P, rather than histamine). Local injection of histamine causes itching and sometimes pain due to stimulation of peripheral nerves. Inhaled histamine is used as a challenge to determine bronchial hyperreactivity and assist in the diagnosis of asthma. H2- AND H3-RECEPTORS H2 receptors are principally concerned with the stimulation of gastric acid release found on parietal cells, which stimulate acid secretion. An example of an H2 receptor antagonist is cimetidine. Their contribution to most vascular responses is minor, but some (e.g. in the pulmonary vasculature) are H2 -receptor mediated. H3 receptors are involved in neurotransmission. Sympathomimetic Drugs that facilitate or increase activity within the sympathetic nervous system. Amphetamines, Phencyclidine, and cocaine.
Vous aimerez peut-être aussi
- Shoe Dog: A Memoir by the Creator of NikeD'EverandShoe Dog: A Memoir by the Creator of NikeÉvaluation : 4.5 sur 5 étoiles4.5/5 (537)
- Grit: The Power of Passion and PerseveranceD'EverandGrit: The Power of Passion and PerseveranceÉvaluation : 4 sur 5 étoiles4/5 (587)
- Barriers To Communication: L L L L L L L L L LDocument1 pageBarriers To Communication: L L L L L L L L L Ltadiwanashe loganPas encore d'évaluation
- Eapm-Final Draft ReportDocument59 pagesEapm-Final Draft Reporttadiwanashe loganPas encore d'évaluation
- Visiual CommDocument3 pagesVisiual Commtadiwanashe loganPas encore d'évaluation
- Colorimetric Determination of pHDocument26 pagesColorimetric Determination of pHtadiwanashe loganPas encore d'évaluation
- Malaria MefloquineDocument12 pagesMalaria Mefloquinetadiwanashe loganPas encore d'évaluation
- Eapm-Final Draft ReportDocument59 pagesEapm-Final Draft Reporttadiwanashe loganPas encore d'évaluation
- Eclampsia and Its ManagementDocument2 pagesEclampsia and Its Managementtadiwanashe loganPas encore d'évaluation
- Timetable May 2012 2nd Semester Second Draft AmendedDocument7 pagesTimetable May 2012 2nd Semester Second Draft Amendedtadiwanashe loganPas encore d'évaluation
- PMC - Issues Affecting Adoption of Personalized MedicineDocument6 pagesPMC - Issues Affecting Adoption of Personalized Medicinetadiwanashe loganPas encore d'évaluation
- 2013-10 Personalised Medicine enDocument33 pages2013-10 Personalised Medicine entadiwanashe loganPas encore d'évaluation
- Hit Student HandbookDocument11 pagesHit Student Handbooktadiwanashe loganPas encore d'évaluation
- Alcohols HITDocument12 pagesAlcohols HITtadiwanashe loganPas encore d'évaluation
- General Info On PharmacopoeiasDocument7 pagesGeneral Info On Pharmacopoeiastadiwanashe loganPas encore d'évaluation
- Rhe OlogyDocument7 pagesRhe Ologytadiwanashe loganPas encore d'évaluation
- 261 PHT Slids Powder, Granuls, Caps, SuppDocument28 pages261 PHT Slids Powder, Granuls, Caps, SuppNaveenbabu SoundararajanPas encore d'évaluation
- AldehydesDocument11 pagesAldehydestadiwanashe loganPas encore d'évaluation
- General Pharmacology (Pharmacodynamics - II)Document34 pagesGeneral Pharmacology (Pharmacodynamics - II)tadiwanashe loganPas encore d'évaluation
- 7 Reaction Oof HydrocarbonDocument11 pages7 Reaction Oof Hydrocarbontadiwanashe loganPas encore d'évaluation
- Protein Sequence AnalysisDocument44 pagesProtein Sequence Analysistadiwanashe loganPas encore d'évaluation
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceD'EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceÉvaluation : 4 sur 5 étoiles4/5 (890)
- The Yellow House: A Memoir (2019 National Book Award Winner)D'EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Évaluation : 4 sur 5 étoiles4/5 (98)
- The Little Book of Hygge: Danish Secrets to Happy LivingD'EverandThe Little Book of Hygge: Danish Secrets to Happy LivingÉvaluation : 3.5 sur 5 étoiles3.5/5 (399)
- On Fire: The (Burning) Case for a Green New DealD'EverandOn Fire: The (Burning) Case for a Green New DealÉvaluation : 4 sur 5 étoiles4/5 (73)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeD'EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeÉvaluation : 4 sur 5 étoiles4/5 (5794)
- Never Split the Difference: Negotiating As If Your Life Depended On ItD'EverandNever Split the Difference: Negotiating As If Your Life Depended On ItÉvaluation : 4.5 sur 5 étoiles4.5/5 (838)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureD'EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureÉvaluation : 4.5 sur 5 étoiles4.5/5 (474)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryD'EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryÉvaluation : 3.5 sur 5 étoiles3.5/5 (231)
- The Emperor of All Maladies: A Biography of CancerD'EverandThe Emperor of All Maladies: A Biography of CancerÉvaluation : 4.5 sur 5 étoiles4.5/5 (271)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreD'EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreÉvaluation : 4 sur 5 étoiles4/5 (1090)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyD'EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyÉvaluation : 3.5 sur 5 étoiles3.5/5 (2219)
- Team of Rivals: The Political Genius of Abraham LincolnD'EverandTeam of Rivals: The Political Genius of Abraham LincolnÉvaluation : 4.5 sur 5 étoiles4.5/5 (234)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersD'EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersÉvaluation : 4.5 sur 5 étoiles4.5/5 (344)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaD'EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaÉvaluation : 4.5 sur 5 étoiles4.5/5 (265)
- The Unwinding: An Inner History of the New AmericaD'EverandThe Unwinding: An Inner History of the New AmericaÉvaluation : 4 sur 5 étoiles4/5 (45)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)D'EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Évaluation : 4.5 sur 5 étoiles4.5/5 (119)
- Her Body and Other Parties: StoriesD'EverandHer Body and Other Parties: StoriesÉvaluation : 4 sur 5 étoiles4/5 (821)
- Immunomodulatory and Growth Performance Effects of Ginsemg ExtractsDocument13 pagesImmunomodulatory and Growth Performance Effects of Ginsemg ExtractsOliver TalipPas encore d'évaluation
- Year 5 Word Puzzle 2023Document2 pagesYear 5 Word Puzzle 2023SJK (CINA) CHUNG WAH-CM4 KPM-SK-PKPPas encore d'évaluation
- The NKTI Medical Laboratory: National Kidney and Transplant InstituteDocument1 pageThe NKTI Medical Laboratory: National Kidney and Transplant InstituteMalagant EscuderoPas encore d'évaluation
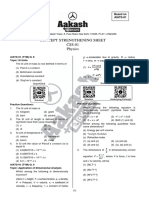
- Concept Strengthening Sheet (CSS-01) Based On AIATS-01 RMDocument19 pagesConcept Strengthening Sheet (CSS-01) Based On AIATS-01 RMB54 Saanvi SinghPas encore d'évaluation
- Writing An Organic Chemistry Filename: Writing An Organic Chemistry Lab ReportDocument6 pagesWriting An Organic Chemistry Filename: Writing An Organic Chemistry Lab ReportNikon SinghPas encore d'évaluation
- General Biology 2 NotesDocument97 pagesGeneral Biology 2 NotesMacky NohayPas encore d'évaluation
- A Conversation Explaining BiomimicryDocument6 pagesA Conversation Explaining Biomimicryapi-3703075100% (2)
- Beckman ProtocolDocument34 pagesBeckman ProtocolIonut NeagaPas encore d'évaluation
- Pforams@Mikrotax - Globigerinoides ConglobatusDocument2 pagesPforams@Mikrotax - Globigerinoides ConglobatusAhmad Lumban GaolPas encore d'évaluation
- Structure of Crystals WebexDocument22 pagesStructure of Crystals WebexmareasanthaPas encore d'évaluation
- Growing Wild MushroomsDocument50 pagesGrowing Wild Mushroomsviki90% (10)
- Gender and Human Evolution PDFDocument49 pagesGender and Human Evolution PDFSimio PensantePas encore d'évaluation
- Microb Monitor 2 Instructions UseDocument5 pagesMicrob Monitor 2 Instructions UseArluky NovandyPas encore d'évaluation
- Genetic Algorithm Based PID Control Tuning For A Model BioreactorDocument13 pagesGenetic Algorithm Based PID Control Tuning For A Model BioreactorertyucbPas encore d'évaluation
- Nervous System Assessment GuideDocument11 pagesNervous System Assessment Guideaderonke bello100% (2)
- Do Genes Determine Champions?Document6 pagesDo Genes Determine Champions?mensrea0Pas encore d'évaluation
- Fourtee: Echinoderms and HemichordatesDocument20 pagesFourtee: Echinoderms and HemichordatesMaharani Putri Chania100% (1)
- Immunology Mid-ExamDocument11 pagesImmunology Mid-ExamNgMinhHaiPas encore d'évaluation
- A Conceptual Framework of Consumer Food Choice Behaviour: CEFAGE-UE Working Paper 2009/06Document26 pagesA Conceptual Framework of Consumer Food Choice Behaviour: CEFAGE-UE Working Paper 2009/06Krishnendu Kizhakedathu SudhakaranPas encore d'évaluation
- ASEA Athletics VT StudyDocument5 pagesASEA Athletics VT Studyalien asterixPas encore d'évaluation
- Effects of Hypotonic, Isotonic & Hypertonic SolutionsDocument19 pagesEffects of Hypotonic, Isotonic & Hypertonic SolutionsTanesh SelvarajuPas encore d'évaluation
- MIB7Document6 pagesMIB7BLPas encore d'évaluation
- General Biology 1 Module 6Document19 pagesGeneral Biology 1 Module 6Vienne MonroidPas encore d'évaluation
- Dunhan R.A. Aquaculture and Fisheries BiotechnologyDocument385 pagesDunhan R.A. Aquaculture and Fisheries BiotechnologyAleksey DubinPas encore d'évaluation
- Chemistry I TheoryDocument2 pagesChemistry I Theory17roopa2010Pas encore d'évaluation
- Mcqs For LabDocument30 pagesMcqs For LabkhubaidPas encore d'évaluation
- The Paper Doctor TEXTODocument101 pagesThe Paper Doctor TEXTOondasdeforma67% (3)
- Subtotal and Total Thyroidectomy: AuthorDocument10 pagesSubtotal and Total Thyroidectomy: AuthorAgustina TambingPas encore d'évaluation
- Cell Division All PDF (Marked Book, Digest & Guide)Document108 pagesCell Division All PDF (Marked Book, Digest & Guide)sseam851Pas encore d'évaluation
- 2013 Taruka Mammalian SpeciesDocument12 pages2013 Taruka Mammalian SpeciesabrunomirandacPas encore d'évaluation