Académique Documents
Professionnel Documents
Culture Documents
Neoplasia/dysplasia Surveillance of Oral Lichen Planus in Malaysia: A Preliminary Study Using Topography Maps
Transféré par
University Malaya's Dental Sciences ResearchTitre original
Copyright
Formats disponibles
Partager ce document
Partager ou intégrer le document
Avez-vous trouvé ce document utile ?
Ce contenu est-il inapproprié ?
Signaler ce documentDroits d'auteur :
Formats disponibles
Neoplasia/dysplasia Surveillance of Oral Lichen Planus in Malaysia: A Preliminary Study Using Topography Maps
Transféré par
University Malaya's Dental Sciences ResearchDroits d'auteur :
Formats disponibles
Surveillance of Oral Lichen Planus using Topography Maps in Malaysia
RESEARCH COMMUNICATION Neoplasia/dysplasia Surveillance of Oral Lichen Planus in Malaysia: A Preliminary Study using Topography Maps
Jimie Siew Mei Lim, Sum Pei Tang, Chong Huat Siar*
Abstract
Background: Conventional methods for writing case notes detailing the progress of oral lichen planus (OLP), a precancerous condition that requires long-term surveillance, is both time-consuming and tedious for the busy clinician. Objectives: To design and perform a simple surveillance on OLP patients based on colour-coded topography mouth maps (TMM). Materials and methods: Three colour-coded TMM were employed: red for OLP in high risk oral mucosal sites, yellow for cases showing improvement and green for asymptomatic lesions at each recall visit. In this preliminary study, these were applied on 30 histologically confirmed OLP individuals attending the Oral Medicine Clinic at the Department of Oral Pathology, Oral Medicine & Periodontology, Faculty of Dentistry, University of Malaya. The sites and extent of OLP lesions were charted on either red, yellow or green TMM based on defined criteria. This surveillance evaluated OLP in relation to patients age, race, gender, underlying systemic conditions, oral habits, initial onset of OLP, oral manifestations and presence/ absence of clinically suspicious areas. Results: Study sample comprised 4 (13.3%) Malays, 9 (30.0%) Chinese and 17 (56.7%) Indians. Most OLP patients belong to the green TMM (n=14, 46.6%) group followed by red (n=11, 36.7%) and yellow (n=5, 16.7%) groups. Of the 11 cases with red TMM, rebiopsy was performed on 4 cases but no dysplasia was detected. Any local confounding factors namely periodontal disease or faulty dental restorations were managed accordingly. Conclusions: TMM is simple to use and aided the clinicians in terms of time saving and patient management. Hence, follow-up of OLP patients can be carried out more efficiently and appropriately. TMM can be used for surveillance of other oral precancerous lesions and conditions. Key Words: Oral lichen planus - precancerous lesions dysplasia - surveillance Asian Pacific J Cancer Prev, 10, 1071-1074
Introduction
Lichen planus is a chronic inflammatory autoimmune disease that can affect the skin, the oral mucosa, scalp and nails (Neville and Day, 2002; Epstein et al., 2007; Scully and Carrozzo, 2008). The disease affects 0.5-2% of the population with a predilection for females (female to male ratio of 3: 2) and a mean onset age in the fourth to fifth decade. Although considerable controversy still surrounds its status as a precancerous condition, currently, a large body of evidence favours the need for recall of these oral lichen planus (OLP) patients to screen for possible malignant transformation (Lo Muzio et al., 1998; Mattsson et al., 2002; Mignogna et al., 2001; 2006; Rad et al., 2009; Rajentheran et al., 2008; van der Meij et al., 2003). The Oral Medicine Clinic in the Department of Oral Pathology, Oral Medicine and Periodontology, Faculty of Dentistry, University of Malaya, Kuala Lumpur, Malaysia, is one of the main tertiary referral centers for oral diseases including screening for oral precancerous and cancerous lesions/conditions. It is currently served by four Oral
Medicine specialists. Although OLP is relatively uncommon in Malaysia, affecting 0.38% of the general population (Zain et al., 1997), a substantial number of patients attending the Oral Medicine clinic present with OLP. In addition, a previous study disclosed that the risk of malignant transformation of OLP in Malaysians is about 1.2% (Yaacob et al., 2002). Two of the authors (LSMJ and TSP), final year dental undergraduates undertook this study of OLP surveillance as part of their elective programme. In the course of this study, they found that compiling data on progress of OLP patients based on case notes were both tedious and timeconsuming. They then devised the use of colour-coded topography mouth maps (TMM) to chart the lesions and monitor the disease course in these patients at each review visit.
Materials and Methods
Institutional approval (Ethics No. DF OP0903/ 0021(U) was obtained prior to the commencement of this study. Selection of OLP patients was based on the
Department of Oral Pathology, Oral Medicine & Periodontology, Faculty of Dentistry, University of Malaya, Kuala Lumpur, Malaysia *For Correspondence: siarch@um.edu.my, chsiar@gmail.com Asian Pacific Journal of Cancer Prevention, Vol 10, 2009
1071
Jimie Siew Mei Lim et al
i)
ii)
iii)
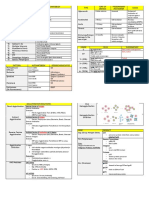
Figure 1. Oral lichen planus (OLP) surveillance using topography mouth maps (TMM). i) a, examination of patient,
b, intraoral view of patient with atrophic OLP on maxillary anterior gingiva, and c, charting of lesions on red TMM. ii) a, atrophic OLP in left buccal mucosa before treatment, b, improvement of lesion after treatment, and c, assignment of case to yellow TMM; iii), asymptomatic reticular OLP in the left buccal mucosa, and b charting in green TMM
modified World Health Organization diagnostic criteria (Rad et al, 2009). Thirty cases from the files (SCH) of the Oral Medicine Clinic, Faculty of Dentistry, University of Malaya were selected. Standard oral mucosa topography maps (Figure 1) were designed for surveillance of OLP lesions in these patients. These consisted of three colour-coded forms: red, yellow and green. Red maps were indicated for patients presenting with atrophic-erosive and plaque forms of OLP as well as for lesions in the tongue and floor of mouth. These cases were placed on a monthly recall visit. Yellow maps were assigned to those patients that showed improvement of their OLP lesions at all other oral mucosal sites except the tongue and floor of mouth and their review was on a 3-monthly basis. Green maps were for patients with asymptomatic reticular form of OLP in all other oral mucosal sites except the tongue and floor of mouth, and for OLP patients who are lesion-free. Asymptomatic cases were followed on a 6-monthly interval while lesion-free patients were seen annually. For each selected case, a pre-designed questionaire was used to obtain information of the patients past medical and dental histories, and high risk habits. This was followed by a routine extraoral and intraoral examination of the oral cavity. Charting of the lesions in the TMM was made based on consensus of all three examiners.
Results 1072
Asian Pacific Journal of Cancer Prevention, Vol 10, 2009
In our sample, there were 8 male (26.7%) and 22 female (73.3%) patients with a male to female ratio of 1:2.75. These consisted of 4 Malays (13.3%), 9 Chinese (30.0%) and 17 Indians (56.7%). Four patients represented new cases who attended the Oral Medicine clinic for the first time. For these new cases, detailed history-taking followed by clinical examination and appropriate laboratory investigations (haematology tests, swabs and smears to rule out Candida) were carried out by the Supervisor (SCH). To establish a diagnosis of OLP, incisional biopsies for histopathological examination and direct immunoflourescent studies were performed. The remaining 26 patients were histologically confirmed cases of OLP attending the Oral Medicine clinic on a regular follow-up/review visit. The maximum period of follow up for these cases was 18 years (mean duration: 3.6 years, range: 0.0 to 18.0 years). The only significant oral habit observed was betel-quid chewing for more than 30 years in one patient. A total of 62 lesions were obtained from our 30 OLP cases. The most common site involved was the gingiva (25.8%), followed by buccal mucosa (24.2%), vestibules (19.4%), tongue (14.5%), upper labial mucosa (4.8%) and lower labial mucosa (4.8%). The rest of the lesions were found on less common sites namely lips (3.2%), palate (1.6%) and floor of mouth (1.6%). The most common clinical form of OLP was the reticular type (48.4%) followed by atrophic (24.2%), plaque (14.5%), mixed (11.3%) and erosive (1.6%) forms. From the TMM charting, most OLP patients were
Surveillance of Oral Lichen Planus using Topography Maps in Malaysia
placed on green TMM (n=14, 46.7%) followed by red for 11 patients (36.7%) and yellow maps on 5 (16.7%). Of the 11 cases with red TMM, rebiopsy was performed on 4 cases but no dysplasia was detected. Any local confounding factors namely periodontal disease or faulty dental restorations were managed accordingly. In the red TMM group (n=11) placed on monthly recall visits, 6 patients attended their review appointments. Two cases showed improvement and were moved to the yellow TMM group. The other 4 cases underwent rebiopsy of their clinically suspicious lesions to rule out possibility of impending malignancy or dysplasia. In the yellow TMM group (n=5) placed on 3 monthly recall visits, 3 cases presented with residual asymptomatic reticular OLP lesions in the buccal mucosa and were moved to the green TMM group. In the green TMM group, 9 cases with asymptomatic OLP cases in non-high risk sites were placed on 6-monthly followup whereas the remaining 5 OLP patients who were lesion-free were placed on annual follow-up.
Discussion
Oral cancer is the sixth most common malignancy worldwide. In Malaysia, oral cancer remains a major health problem (Ng et al., 1985; 1986; Ng and Siar, 1992; Siar et al., 1990). It is now well established that early detection of oral precancerous and cancerous lesions/ conditions can improve the clinical outcome for patients. A previous nationwide survey on oral mucosal lesions was carried out to screen for potentially malignant oral epithelial lesions and conditions, and for the early detection of oral cancer (Zain et al, 1996; 1997). OLP was classified as a precancerous condition in this survey and accounted for 0.38% of oral mucosal lesions. In another Malaysian study based on a retrospective analysis of 77 cases of OLP, a single case of malignant transformation was reported (Yaacob et al., 2002). In consideration of the fact that majority viewed OLP as a precancerous condition, a monitoring system for OLP patients has been recommended (Mattsson et al., 2002). This is to facilitate the early diagnosis of oral cancer and thereby reducing morbidity and mortality from oral cancer arising in these patients. One suggestion is that OLP patients should have regular follow-up examinations from two to four times annually (Scully et al., 1998). Since OLP is one of the most prevalent oral mucosal lesions, a surveillance programme entails utilization of substantial economic resources, and hence, a reconsideration of the background of the need for a recall is warranted (Mattsson et al, 2002). In addition, in countries with few dentists or other oral health care providers, it is most likely difficult for any recall routines for OLP to be implemented (Warnakulasuriya and Nanayakkara, 1991). As OLP has been accepted as a precancerous condition in this Institution, follow-ups are mandatory. During each follow-up visit, the patients complaints, clinical examinations and managements were carried out by the clinicians, and the conventional method was to record these findings/ evaluations in these patients folders. Consequently a thick compilation of patients records
often accumulates. The main disadvantage of this conventional method of record keeping is that the clinicians frequently have to spend considerable time to read through these case notes. For ease of follow-ups, our study has introduced a simple and economical method for surveillance of OLP. Coloured-coded maps were utilized to classify patients according to the severity of the disease and frequency of recall visits. The advantage of this method is that it can help save the clinicians time by viewing only the mouth maps on coloured papers and obviates the need to plough through their records. As pictures can tell a thousand words, clinicians can look at the locations and descriptions of lesions at a glance, instead of spending time reading the patients records. Different colour codings will also guide a clinician to determine the frequency of follow-up needed for each case. The idea was developed based on the colours of the traffic lights. Moreover, clinicians will be able to determine the progress of patients conditions by referring to the colours of mouth maps used for every visit. Red colour mouth maps are allocated to patients that require more frequent monitoring. The red colour can easily attract a clinicians attention to follow up the patient in one months time and for re-biopsy if indicated. Patients presenting with atrophic, erosive and bullous OLP are assigned red mouth maps because it is known that these forms of OLP carry a higher risk of malignant transformation than reticular or plaque forms (Mattsson et al., 2002; van der Meij et al., 2003; Rad et al., 2009). Similarly, patients with OLP affecting the tongue and floor of mouth are assigned red mouth maps as these locations are considered high risk sites for oral cancer development. It is known that the precise location within the mouth seems to have a profound influence on the risk of malignant transformation (Napier and Speight, 2008). Potentially malignant lesions including leukoplakia are more frequently found in the buccal mucosa yet those found on the lateral borders of the tongue and floor of mouth are more frequently associated with malignant transformation to oral squamous cell carcinoma. In those cases that showed improvement in subsequent follow-ups, yellow mouth maps were used, and they will be reviewed after 3 months. Patients who have asymptomatic OLP lesions in oral mucosal sites other than the tongue or floor of mouth are placed on a 6-monthly recall visit, whereas those OLP patients who are now lesion-free are placed on a 12-monthly recall visit. In summary, this study proposed the use of colourcoded TMM to subcategorize OLP patients into those requiring one, 3, 6 or 12 monthly recall. These maps are easy to apply and overcome the need to write or read detail case notes. Its potential application for screening other oral potentially malignant lesions and conditions can be considered.
Acknowledgement
Financial assistance from the university Grants Commission, Major Research Project [32-614/2006 (SR)]
Asian Pacific Journal of Cancer Prevention, Vol 10, 2009
1073
Jimie Siew Mei Lim et al
is gratefully acknowledged. References
Epstein JB, Gorsky M, Fischer D, et al (2007). A survey of the current approaches to diagnosis and management of oral premalignant lesions. J Am Dent Assoc, 138, 1555-62. Gale N, Pilch BZ, Sidransky D (2005). Epithelial precursor lesions. In: World Health Organization Pathology & Genetics. Head and Neck Tumours, Eds Barnes L, Evenson JW, Reichart P, Sidransky D. IARC, Lyon, pp 17781. Lo Muzio L, Mignogna MD, Favia G, et al (1998). The possible association between oral lichen planus and oral squamous cell carcinoma: a clinical evaluation on 14 cases and a review of the literature. Oral Oncol, 34, 239-6. Mattsson U, Jontell M, Holmstrup P (2002). Oral lichen planus and malignant transformation: Is a recall of patients justified? Crit Rev Oral Biol, 13, 390-6. Mignogna MD, Fedele S, Lo Russo L (2006). Dysplasia/ neoplasia surveillance in oral lichen planus patients: A description of clinical criteria adopted at a single centre and their impact on prognosis. Oral Oncol, 42, 819-24. Mignogna MD, Lo Muzio L, Lo Russo L, et al (2001). Clinical guidelines in early detection of oral squamous cell carcinoma arising in oral lichen planus: a 5-year experience. Oral Oncol, 37, 262-7. Napier SS, Speight PM (2008). Natural history of potentially malignant oral epithelial lesions and conditions: An overview of the literature. J Oral Pathol Med, 37, 1-10. Neville BW, Day TA (2002). Oral cancer and precancerous lesions. CA Cancer J Clin, 52, 195-215. Ng KH, Siar CH, Ramanathan K, Murugasu P (1986). The prevalence of oral habits in 100 cases of oral squamous cell carcinomas in Malaysia. Ann Dent, 45, 7-10. Ng KH, Siar CH, Ramanathan K, Murugasu P, Chelvanayagam P (1985). Squamous cell in Malaysia - Any change? Southeast Asian J Trop Med Pub Hlth, 16, 602-6. Ng KH, Siar CH (1992). Oral cancers in Malaysia. Proc Sci Sem IMR, 90th Anniv, 103-115. Rad M, Hashemipoor MA, Mojtahedi A, et al (2009). Correlation between clinical and histopathologic diagnosis of oral lichen planus based on the modified WHO diagnostic criteria. Oral Surg Oral Med Oral Pathol Oral Radiol Endod, 107, 796800. Rajentheran R, McLean NR, Kelly CG, Reed MF, Nolan A (1999). Malignant transformation of oral lichen planus. Eur J Surg Oncol, 25, 520-3. Scully C, Beyli M, Ferreiro MC et al (1998). Update on oral lichen planus: etiopathogenesis and management. Crit Rev Oral Biol Med, 9, 86122. Scully C, Carrozzo M (2008). Oral mucosal disease: Lichen planus. Br J Oral Maxillofac Surg, 46, 15-21. Siar CH, Ng KH, Mah CF, Ling CC (1990). Oral squamous cell carcinoma in peninsular Malaysia. Asian Med J, 33, 697703. van der Meij EH, Schepman K, van der Waal I (2003). The possible premalignant character of oral lichen planus and oral lichenoid lesions: A prospective study. Oral Surg Oral Med Oral Pathol Oral Radiol Endod, 96, 164-71 Warnakulasuriya KA, Nanayakkara BG (1991). Reproducibility of an oral cancer and precancer detection program using a primary health care model in Sri Lanka. Cancer Detect Prev, 15, 331-4. Yaacob HB, Tan PL, Ngeow WC (2002). Malignancy in oral lichen planus: a review of a group from the Malaysian population. J Oral Sci, 44, 6571. Zain RB, Ikeda N, Gupta PC, et al (1999). Oral mucosal lesions associated with betel quid, areca nut and tobacco chewing habits: consensus from a workshop held in Kuala Lumpur,
Malaysia, November 25-27, 1996. J Oral Pathol Med, 28, 1-4. Zain RD, Ikeda N, Razak IA, et al (1997). A national epidemiological survey of oral mucosal lesions in Malaysia. Comm Dent Oral Epidemiol, 25, 377-83.
1074
Asian Pacific Journal of Cancer Prevention, Vol 10, 2009
Vous aimerez peut-être aussi
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeD'EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeÉvaluation : 4 sur 5 étoiles4/5 (5794)
- The Yellow House: A Memoir (2019 National Book Award Winner)D'EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Évaluation : 4 sur 5 étoiles4/5 (98)
- Influence of Object Location in Different FOVs On Trabecular Bone Microstructure Measurements of Human MandibleDocument1 pageInfluence of Object Location in Different FOVs On Trabecular Bone Microstructure Measurements of Human MandibleUniversity Malaya's Dental Sciences ResearchPas encore d'évaluation
- Multi-Unit Implant Impression Accuracy: A Review of The LiteratureDocument1 pageMulti-Unit Implant Impression Accuracy: A Review of The LiteratureUniversity Malaya's Dental Sciences ResearchPas encore d'évaluation
- A Simple Procedure For Retrieval of A Cement-Retained Implant-Supported Crown: A Case ReportDocument4 pagesA Simple Procedure For Retrieval of A Cement-Retained Implant-Supported Crown: A Case ReportUniversity Malaya's Dental Sciences ResearchPas encore d'évaluation
- Level and Determinants of Knowledge of Symptomatic Knee Osteoarthritis Among Railway Workers in MalaysiaDocument10 pagesLevel and Determinants of Knowledge of Symptomatic Knee Osteoarthritis Among Railway Workers in MalaysiaUniversity Malaya's Dental Sciences ResearchPas encore d'évaluation
- Global Search For Right Cell Type As A Treatment Modality For Cardiovascular DiseaseDocument1 pageGlobal Search For Right Cell Type As A Treatment Modality For Cardiovascular DiseaseUniversity Malaya's Dental Sciences ResearchPas encore d'évaluation
- Growth Inhibitory Response and Ultrastructural Modification of Oral-Associated Candidal Reference Strains (ATCC) by Piper Betle L. ExtractDocument7 pagesGrowth Inhibitory Response and Ultrastructural Modification of Oral-Associated Candidal Reference Strains (ATCC) by Piper Betle L. ExtractUniversity Malaya's Dental Sciences ResearchPas encore d'évaluation
- Assessment of Patients' Level of Satisfaction With Cleft Treatment Using The Cleft Evaluation ProfileDocument12 pagesAssessment of Patients' Level of Satisfaction With Cleft Treatment Using The Cleft Evaluation ProfileUniversity Malaya's Dental Sciences ResearchPas encore d'évaluation
- The Effect of Psidium Guajava and Piper Betle Extracts On The Morphology of Dental Plaque BacteriaDocument6 pagesThe Effect of Psidium Guajava and Piper Betle Extracts On The Morphology of Dental Plaque BacteriaUniversity Malaya's Dental Sciences ResearchPas encore d'évaluation
- StaphyloBase: A Specialized Genomic Resource For The Staphylococcal Research CommunityDocument9 pagesStaphyloBase: A Specialized Genomic Resource For The Staphylococcal Research CommunityUniversity Malaya's Dental Sciences ResearchPas encore d'évaluation
- Reusable Heat-Sensitive Phantom For Precise Estimation of Thermal Profile in Hyperthermia ApplicationDocument2 pagesReusable Heat-Sensitive Phantom For Precise Estimation of Thermal Profile in Hyperthermia ApplicationUniversity Malaya's Dental Sciences ResearchPas encore d'évaluation
- Prosthetic Management of Mid-Facial Defect With Magnet-Retained Silicone ProsthesisDocument2 pagesProsthetic Management of Mid-Facial Defect With Magnet-Retained Silicone ProsthesisUniversity Malaya's Dental Sciences ResearchPas encore d'évaluation
- Genomic Reconnaissance of Clinical Isolates of Emerging Human Pathogen Mycobacterium Abscessus Reveals High Evolutionary PotentialDocument10 pagesGenomic Reconnaissance of Clinical Isolates of Emerging Human Pathogen Mycobacterium Abscessus Reveals High Evolutionary PotentialUniversity Malaya's Dental Sciences ResearchPas encore d'évaluation
- Enhanced Post Crown Retention in Resin Composite-Reinforced, Compromised, Root-Filled Teeth: A Case ReportDocument6 pagesEnhanced Post Crown Retention in Resin Composite-Reinforced, Compromised, Root-Filled Teeth: A Case ReportUniversity Malaya's Dental Sciences ResearchPas encore d'évaluation
- Evaluation of The Effect of Cassia Surattensis Burm. F., Flower Methanolic Extract On The Growth and Morphology of Aspergillus NigerDocument7 pagesEvaluation of The Effect of Cassia Surattensis Burm. F., Flower Methanolic Extract On The Growth and Morphology of Aspergillus NigerUniversity Malaya's Dental Sciences ResearchPas encore d'évaluation
- Treatment of A Maxillary Dento-Alveolar Defect Using An Immediately Loaded Definitive Zygoma Implant-Retained Prosthesis With 11-Month Follow-Up: A Clinical ReportDocument5 pagesTreatment of A Maxillary Dento-Alveolar Defect Using An Immediately Loaded Definitive Zygoma Implant-Retained Prosthesis With 11-Month Follow-Up: A Clinical ReportUniversity Malaya's Dental Sciences Research100% (1)
- University of Malaya Dental Students' Attitudes Towards Communication Skills Learning: Implications For Dental EducationDocument9 pagesUniversity of Malaya Dental Students' Attitudes Towards Communication Skills Learning: Implications For Dental EducationUniversity Malaya's Dental Sciences ResearchPas encore d'évaluation
- Tooth Size Discrepancies in An Orthodontic PopulationDocument7 pagesTooth Size Discrepancies in An Orthodontic PopulationUniversity Malaya's Dental Sciences ResearchPas encore d'évaluation
- Translating The Research Diagnostic Criteria For Temporomandibular Disorders Into Malay: Evaluation of Content and ProcessDocument0 pageTranslating The Research Diagnostic Criteria For Temporomandibular Disorders Into Malay: Evaluation of Content and ProcessUniversity Malaya's Dental Sciences ResearchPas encore d'évaluation
- Talon Cusp Affecting Primary Dentition in Two Siblings: A Case ReportDocument3 pagesTalon Cusp Affecting Primary Dentition in Two Siblings: A Case ReportUniversity Malaya's Dental Sciences ResearchPas encore d'évaluation
- The Safety Zone For Mini-Implant Maxillary Anchorage in MongoloidsDocument5 pagesThe Safety Zone For Mini-Implant Maxillary Anchorage in MongoloidsUniversity Malaya's Dental Sciences ResearchPas encore d'évaluation
- Transient Loss of Power of Accommodation in 1 Eye Following Inferior Alveolar Nerve Block: Report of 2 CasesDocument5 pagesTransient Loss of Power of Accommodation in 1 Eye Following Inferior Alveolar Nerve Block: Report of 2 CasesUniversity Malaya's Dental Sciences ResearchPas encore d'évaluation
- The Antimicrobial Efficacy of Elaeis Guineensis: Characterization, in Vitro and in Vivo StudiesDocument18 pagesThe Antimicrobial Efficacy of Elaeis Guineensis: Characterization, in Vitro and in Vivo StudiesUniversity Malaya's Dental Sciences ResearchPas encore d'évaluation
- Reliability of Voxel Gray Values in Cone Beam Computed Tomography For Preoperative Implant Planning AssessmentDocument1 pageReliability of Voxel Gray Values in Cone Beam Computed Tomography For Preoperative Implant Planning AssessmentUniversity Malaya's Dental Sciences ResearchPas encore d'évaluation
- Promoting Oral Cancer Awareness and Early Detection Using A Mass Media ApproachDocument8 pagesPromoting Oral Cancer Awareness and Early Detection Using A Mass Media ApproachUniversity Malaya's Dental Sciences ResearchPas encore d'évaluation
- Stress and Its Relief Among Undergraduate Dental Students in MalaysiaDocument9 pagesStress and Its Relief Among Undergraduate Dental Students in MalaysiaJacky TangPas encore d'évaluation
- Structured Student-Generated Videos For First-Year Students at A Dental School in MalaysiaDocument8 pagesStructured Student-Generated Videos For First-Year Students at A Dental School in MalaysiaUniversity Malaya's Dental Sciences ResearchPas encore d'évaluation
- Strawberry Gingivitis As The First Presenting Sign of Wegener's Granulomatosis: Report of A CaseDocument4 pagesStrawberry Gingivitis As The First Presenting Sign of Wegener's Granulomatosis: Report of A CaseUniversity Malaya's Dental Sciences ResearchPas encore d'évaluation
- Scanning Electron Microscopic Study of Piper Betle L. Leaves Extract Effect Against Streptococcus Mutans ATCC 25175Document10 pagesScanning Electron Microscopic Study of Piper Betle L. Leaves Extract Effect Against Streptococcus Mutans ATCC 25175University Malaya's Dental Sciences ResearchPas encore d'évaluation
- Practices and Beliefs Among Malaysian Dentists and Periodontists Towards Smoking Cessation InterventionDocument7 pagesPractices and Beliefs Among Malaysian Dentists and Periodontists Towards Smoking Cessation InterventionUniversity Malaya's Dental Sciences ResearchPas encore d'évaluation
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryD'EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryÉvaluation : 3.5 sur 5 étoiles3.5/5 (231)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceD'EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceÉvaluation : 4 sur 5 étoiles4/5 (895)
- The Little Book of Hygge: Danish Secrets to Happy LivingD'EverandThe Little Book of Hygge: Danish Secrets to Happy LivingÉvaluation : 3.5 sur 5 étoiles3.5/5 (400)
- Shoe Dog: A Memoir by the Creator of NikeD'EverandShoe Dog: A Memoir by the Creator of NikeÉvaluation : 4.5 sur 5 étoiles4.5/5 (537)
- Never Split the Difference: Negotiating As If Your Life Depended On ItD'EverandNever Split the Difference: Negotiating As If Your Life Depended On ItÉvaluation : 4.5 sur 5 étoiles4.5/5 (838)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureD'EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureÉvaluation : 4.5 sur 5 étoiles4.5/5 (474)
- Grit: The Power of Passion and PerseveranceD'EverandGrit: The Power of Passion and PerseveranceÉvaluation : 4 sur 5 étoiles4/5 (588)
- The Emperor of All Maladies: A Biography of CancerD'EverandThe Emperor of All Maladies: A Biography of CancerÉvaluation : 4.5 sur 5 étoiles4.5/5 (271)
- On Fire: The (Burning) Case for a Green New DealD'EverandOn Fire: The (Burning) Case for a Green New DealÉvaluation : 4 sur 5 étoiles4/5 (74)
- Team of Rivals: The Political Genius of Abraham LincolnD'EverandTeam of Rivals: The Political Genius of Abraham LincolnÉvaluation : 4.5 sur 5 étoiles4.5/5 (234)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaD'EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaÉvaluation : 4.5 sur 5 étoiles4.5/5 (266)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersD'EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersÉvaluation : 4.5 sur 5 étoiles4.5/5 (344)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyD'EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyÉvaluation : 3.5 sur 5 étoiles3.5/5 (2259)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreD'EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreÉvaluation : 4 sur 5 étoiles4/5 (1090)
- The Unwinding: An Inner History of the New AmericaD'EverandThe Unwinding: An Inner History of the New AmericaÉvaluation : 4 sur 5 étoiles4/5 (45)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)D'EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Évaluation : 4.5 sur 5 étoiles4.5/5 (121)
- Her Body and Other Parties: StoriesD'EverandHer Body and Other Parties: StoriesÉvaluation : 4 sur 5 étoiles4/5 (821)
- Diabetik Keto AsDocument162 pagesDiabetik Keto AsayudilaPas encore d'évaluation
- Biomonitoring of 5 Flourouracil - AnyDocument23 pagesBiomonitoring of 5 Flourouracil - AnyAgus TianyPas encore d'évaluation
- General Pharmacology MCQs PDFDocument41 pagesGeneral Pharmacology MCQs PDFTaonga Zulu90% (21)
- 1.5 ProkaryotesDocument17 pages1.5 ProkaryotesKate Rashell SevillaPas encore d'évaluation
- Pediatric Cholestasis: Epidemiology, Genetics, Diagnosis, and Current ManagementDocument5 pagesPediatric Cholestasis: Epidemiology, Genetics, Diagnosis, and Current ManagementAnnisa SusiloPas encore d'évaluation
- What Is Muscle Dystrophy?Document4 pagesWhat Is Muscle Dystrophy?Ryan GoldsteinPas encore d'évaluation
- How I Treat Mixed-Phenotype Acute LeukemiaDocument10 pagesHow I Treat Mixed-Phenotype Acute LeukemiawenyinriantoPas encore d'évaluation
- POPS - Tetanus Booklet BDocument8 pagesPOPS - Tetanus Booklet BGuhanPas encore d'évaluation
- Global Rheumatoid Arthritis Drugs MarketDocument2 pagesGlobal Rheumatoid Arthritis Drugs MarketiHealthcareAnalyst, Inc.Pas encore d'évaluation
- Sci 8, 4th Periodical ExamDocument3 pagesSci 8, 4th Periodical ExamRutchie Lasque100% (1)
- ScleritisDocument3 pagesScleritisPangala NitaPas encore d'évaluation
- Chapter14 PDFDocument21 pagesChapter14 PDFsgw67Pas encore d'évaluation
- Leapotswe International School: Cambridge IGCSEDocument16 pagesLeapotswe International School: Cambridge IGCSEShepherd W NgwenyaPas encore d'évaluation
- Synthesis Paper On The Framework For Pathophysiology: EtiologyDocument4 pagesSynthesis Paper On The Framework For Pathophysiology: EtiologyTiger KneePas encore d'évaluation
- IQ Tests, IQ Scores and Human IntelligenceDocument2 pagesIQ Tests, IQ Scores and Human IntelligenceHarish PotnuriPas encore d'évaluation
- Radiation Physics and Chemistry: Emilie Brun, Cécile Sicard-RoselliDocument9 pagesRadiation Physics and Chemistry: Emilie Brun, Cécile Sicard-RoselliDavide MessinaPas encore d'évaluation
- Science 9 Assessment TestDocument4 pagesScience 9 Assessment TestMonhannah Calimbol Sumapal LimbutunganPas encore d'évaluation
- Mutations in SLC26A1 Cause Nephrolithiasis: Table S1Document7 pagesMutations in SLC26A1 Cause Nephrolithiasis: Table S1Johnny GotePas encore d'évaluation
- Introduction To Drug Discovery & Development: Dr. Humair Bin MD OmerDocument9 pagesIntroduction To Drug Discovery & Development: Dr. Humair Bin MD OmerMD. RASEL MAHMUD MIMPas encore d'évaluation
- Biology Paper 1 TZ2 HLDocument19 pagesBiology Paper 1 TZ2 HLMiriam LópezPas encore d'évaluation
- Pedigree ChartsDocument12 pagesPedigree ChartsvaughanPas encore d'évaluation
- Lettre de Corteva À La Commission Européenne Concernant Les Avis de l'EFSA Sur Le Chlorpyrifos Et Le Chlorpyrifos-Méthyl 06.09.2019Document34 pagesLettre de Corteva À La Commission Européenne Concernant Les Avis de l'EFSA Sur Le Chlorpyrifos Et Le Chlorpyrifos-Méthyl 06.09.2019LeMonde.frPas encore d'évaluation
- Cimetidine Anti Cancer Drug Reverses Tumor Immunity - Jeffrey Dach MDDocument26 pagesCimetidine Anti Cancer Drug Reverses Tumor Immunity - Jeffrey Dach MDnepretipPas encore d'évaluation
- Amare Thesis Proposal1Document39 pagesAmare Thesis Proposal1ናታኔም ናታኔምPas encore d'évaluation
- List All Biology Books CollectionDocument6 pagesList All Biology Books Collectionmbak_asyPas encore d'évaluation
- Biology End of Semister Exam June 2020Document7 pagesBiology End of Semister Exam June 2020Tavonga ShokoPas encore d'évaluation
- An Effective Solution To Optimise Health Status and Nutrient Utilisation - GUSTOR AQUADocument5 pagesAn Effective Solution To Optimise Health Status and Nutrient Utilisation - GUSTOR AQUAInternational Aquafeed magazinePas encore d'évaluation
- Environmental Enteropathy: Ahmed Laving University of NairobiDocument19 pagesEnvironmental Enteropathy: Ahmed Laving University of NairobiDauz KevinPas encore d'évaluation
- NBDE Remembered 2 New YorkDocument242 pagesNBDE Remembered 2 New YorkR MPas encore d'évaluation
- ISBB Wall Notes PDFDocument8 pagesISBB Wall Notes PDFLynx EemanPas encore d'évaluation