Académique Documents
Professionnel Documents
Culture Documents
Computer-Assisted Navigational Surgery in Oral and Maxillofacial Surgery
Transféré par
Vikas VatsDescription originale:
Titre original
Copyright
Formats disponibles
Partager ce document
Partager ou intégrer le document
Avez-vous trouvé ce document utile ?
Ce contenu est-il inapproprié ?
Signaler ce documentDroits d'auteur :
Formats disponibles
Computer-Assisted Navigational Surgery in Oral and Maxillofacial Surgery
Transféré par
Vikas VatsDroits d'auteur :
Formats disponibles
Atlas Oral Maxillofacial Surg Clin N Am 13 (2005) 4149
Computer-Assisted Navigational Surgery in Oral and Maxillofacial Surgery
Arnulf Baumann, MD, DMD*, Kurt Schicho, DSc, Clemens Klug, MD, Arne Wagner, MD, DMD, Rolf Ewers, MD, DMD
University Hospital of Cranio-Maxillofacial and Oral Surgery, Medical University of Vienna, AKH, Wa hringer Gu rtel 18-20, 1090 Vienna, Austria
The development of computer-assisted navigational surgery has made tremendous progress since the rst application of a computer-aided navigation system in a neurosurgical procedure by Watanabe [1] in the late 1980s. Computer-assisted surgery (CAS) is now in widespread use in neurosurgery, orthopedics, and ear, nose, and throat procedures. In oral and maxillofacial surgery, this technique has been applied in dental implantology for the correction of posttraumatic deformities, arthroscopy of the temporomandibular joint, tumor surgery, and removal of foreign bodies. CAS allows an interactive operative application of CT and MRI scan data, which assists the surgeon during the operative procedure. Therefore, distances and relationships between important anatomic structures can be better evaluated with this technique. Computer-assisted surgery also provides the possibilities of performing less invasive approaches and passing through a preoperative simulated and planned procedure more easily and precisely.
Workow for navigation procedures To apply navigational surgery, the patient must rst be prepared with reference markers. The markers are necessary for registration of the patient in the navigation system. Reference markers can be inserted in an occlusion splint or as microscrews in the bone. It has been shown that using screws as markers will give the best accuracy. The diagnostic workup by CT or MRI scan is performed with these reference markers in position. Diagnostic images Computer-assisted navigational surgery needs CT and MRI scans in high quality. All of the following steps in planning and operative navigation are based on CT and MRI data in threedimensional (3D) computer models. Planning and simulation For simulation and planning, virtual three-dimensional graphics software should be available to allow interactive manipulation, for example in positioning implants according prosthodontic
This work was supported by Grant P-12489 Med from the Austrian Science Foundation (FWF) and by CMF Vienna. * Corresponding author. E-mail address: arnulf.baumann@akh-wien.ac.at (A. Baumann). 1061-3315/05/$ - see front matter 2005 Elsevier Inc. All rights reserved. doi:10.1016/j.cxom.2004.10.002
oralmaxsurgeryatlas.theclinics.com
42
BAUMANN et al
requirements. Limitations in the interactive manipulation may require additional planning tools, such as a stereolithographic (SL) model. Operative procedure Before starting the operation, the patient must be registered or calibrated using the reference markers (screws or an occlusion splint). Also, the surgical instrument (eg, a drill for implant insertion) must be calibrated relative to the bone. Calibration is performed by sensors attached to the handpiece and to the patient. For this procedure, the optoelectric tracking system with light-emitting diodes is used. The optoelectric tracking system gives better accuracy and stability of the navigation system in comparison with the electromagnetic tracking system, because the magnetic eld will be distorted by the motor of the drill. Two examples explain the current technique and possibilities of computer-assisted navigational surgery in oral and maxillofacial surgery. In these two procedures, the authors used dierent methods for registration, planning, and intraoperative navigation. Computer-assisted navigation in posttraumatic zygomatic correction Posttraumatic malposition of the zygomatic bone may cause atness of the malar prominence, orbita dystopia with functional symptoms such as diplopia, or a reduced mouth opening. Surgical correction can be performed either by onlay grafts in a matter of camouage or by an osteotomy of the zygomatic complex. The disadvantage of camouage is that many symptoms of posttraumatic zygomatic deformity still remain. Therefore, Freihofer and Borstlap [2] and Cohen and Kawamoto [3] suggest a complete osteotomy of the zygomatic bone. However, nding the right position of the zygomatic complex to correct facial asymmetry is the most difcult part in the operation because of limited access, even though a coronal approach is used. The change of the anatomic landmarks makes this procedure more difcult than in a fresh zygomatic fracture. The patient presented with several secondary camouage corrections that had been performed for primary treatment of a right communicated zygomatic fracture. Nevertheless, the patient was not satised with the aesthetic outcome (Fig. 1). For the correction procedure, we used a combination of CAS with an SL model, and for the registration procedure we used an occlusion splint with inserted reference markers. Preoperative planning Diagnostic data For planning and simulation of the zygomatic osteotomy, we used an SL model. The SL model was fabricated with the occlusion splint according to the CT data and showed the 3D skeletal structure very precisely. In Fig. 2, different views of the skeletal structure show the lowered right infraorbital rim and the atness in the right zygomatic prominence. The SL model was adapted for preoperative treatment planning and also for preoperative registration by using a special occlusion splint. The splint was supplied with marker spheres (at a diameter of 1 mm), and these reference markers were visible in the CT slices. To transfer the marker points to the 3D model, additional horizontal connection bars were added to the surface of the SL model, as seen in Fig. 2. During the production of the SL model, a dened space in the bars was spared, and this space was later lled with 1-mm diameter steel globules (see Fig. 2B). This transfer of the occlusion splint allows registering or calibrating the 3D model in the navigation system. Surgical planning According to SL model analysis, the decisions for locating the osteotomy lines were determined, and the surgical procedure was simulated on the SL model. The right position of the zygomatic bone was found by comparison with the uninjured side, and the osteotomized segment was xed with miniplates. These miniplates were later used for xation of the bone.
COMPUTER-ASSISTED NAVIGATIONAL SURGERY
43
Fig. 1. The patient presented after undergoing several corrections of a right communicated fracture of the zygoma. The right orbit is lowered (orbita dystopia), and the right malar prominence is missing.
Additionally the osteotomy gaps can be visualized directly, which gives the surgeon additional information such as how much bone must be excised for the elevation of the zygomatic complex during the surgery (Fig. 3). Registration of the SL model After the surgical planning, the bent miniplates were removed from the model, and the zygomatic was repositioned in its preoperative situation. A sensor was attached to the model for registration in the navigation system. All reference markers were touched consecutively with a pointer, and the corresponding points were touched on the computer screen. After registration of the SL model, the drill holes were recorded with the pointer, and the coordinates were stored in the computer (Fig. 4). Surgical procedure Registration of the patient Registration of the patient in the navigation system was carried out by using reference markers on the occlusion splint (Fig. 5). Then the splint was removed, and the saved coordinates of the drill holes from the SL model were navigated and marked on the patient by the drill. The osteotomy lines were marked.
Fig. 2. SL model of the patient in Fig.1. (A) Anteroposterior view shows the orbita dystopia and the reconstructed orbital oor. Skeletal asymmetry in the malar prominence can be better seen in the caudal projection (B). The arrow (B) shows the space for the insertion of the reference markers. These locations correspond to the reference markers in the occlusion splint of the patient.
44
BAUMANN et al
Fig. 3. Postoperative SL model showing anteroposterior (A) and caudal (B) views. The zygoma was xed by using miniplates in the right position. Miniplates were already removed for sterilization.
Osteotomy After exposure by buccal, transconjunctival, and lateral eyebrow incisions, the zygomatic bone was osteotomized. Fig. 6 shows the osteotomy at the zygomaticofrontal location and the prepared, navigated drill holes for the osteosynthesis plate. After mobilization, the prebent plates were xed in the navigated screw holes, and the zygomatic was repositioned according to the curvature of the plate. In addition, orbital oor reconstruction was performed, with a bone graft from the mandible. The clinical outcome resulted in an improvement of the zygomatic position and symmetry in the orbital region (Fig. 7). Disadvantages of computer-assisted surgery in zygomatic correction The navigation system is expensive and time consuming, and there are dierent types of navigation systems available. The authors used the Treon system (Medtronic, Inc, Minneapolis, MN). Marmulla and Niederdellmann [4] used a different navigational system for a similar procedure. They used the Surgical Segment Navigator (SSN) system [Marmulla (inventor); Carl Zeiss, Oberkochen, Germany]. In the SSN system, one frame is xed at the skull and the other one at the osteotomized zygomatic complex. The osteotomized bone is then navigated to the right position. This technique needs more dissection and limits space during zygomatic xation with miniplates. Advantages of computer-assisted surgery in zygomatic correction The planned surgical correction can be better transformed with assistance from the navigation system. CAS may also allow performing a less invasive procedure. The three
Fig. 4. Registration of the screw holes with the pointer at the SL model. Screw holes are shown at the zygomaticofrontal region (arrow).
COMPUTER-ASSISTED NAVIGATIONAL SURGERY
45
Fig. 5. The patient is registered intraoperatively by using the reference markers on the occlusion splint.
incisions (enoral, transconjunctival, and lateral brow incision) that the present authors used in this case were adequate for performing the osteotomy and nding the right position of the zygomatic bone. The prebent plates reduced the operation time. Improvement in 3D software development may shorten preoperative planning time and the navigation procedure itself. Computer-assisted navigation in dental implantology Dental implantology may be another application for computer-assisted navigation surgery. The use of presently available commercial software allows for planning the procedure more easily. CAS may help to insert implants more precisely and will provide higher safety against nerve damage or injury of adjacent teeth. A typical workow for navigated insertion of dental implants in the maxilla is described using a patient case history. Preoperative planning Diagnostic data The CT scan was performed after insertion of microscrews in the maxilla. The screws were used as reference markers for the registration and the navigation (Fig. 8A).
Fig. 6. Intraoperative view of the zygomaticofrontal region. The arrow marks the navigated position of the planned screw position. The bone slice must be removed for the later elevation of the zygoma.
46
BAUMANN et al
Fig. 7. The caudal view shows the change of the zygoma prominence in the preoperative (A) view and after zygoma correction (B). The yellow line through the pupil also marks the change of the orbita dystopia.
Planning After importing the CT data and drawing the dental arc, the implants were positioned according to prosthodontic aspects. For planning and navigation, the authors used the software program of the Virtual Implant System (Artma Medical Technologies AG, Vienna, Austria). This program runs on Apple computers (Apple Inc., Cupertino, California). The implants were selected from a menu on the computer screen and positioned by drag and drop using the mouse. In various 2D and 3D renderings, the position, angulations, and lengths of the implants were dened (see Fig. 8BD). In a case of implantation in the mandible, the alveolar nerve must rst be drawn or marked in the CT scan to recognize the various distances to this critical area.
Surgical procedure Registration of the patient The patient was registered by markers on the upper jaw. To trace the position of the drill relative to the bone, a navigation sensor was mounted to the patient at the anterior nasal spine, and another sensor was mounted to the handpiece of the drill (Fig. 9).
Fig. 8. (A) Axial CT scan with inserted screws as reference markers (arrows). (AD) Preoperative planning of implant positions and orientation in the maxilla with the Virtual Implant Navigator.
COMPUTER-ASSISTED NAVIGATIONAL SURGERY
47
Fig. 9. Operation site. Navigation sensors are attached to the patient and to the handpiece of the dental drill.
Implantation During the surgical procedure, the actual position of the drill was continuously displayed in relation to the preplanned (optimal) positions of the implants (Fig. 10). The position and angulation of the drill were visible directly on the screen and could be corrected immediately. Fig. 11 shows, for example, the situation in which the drill was in the implant cavity but the angulation and the depth of the drill were not completely correct to the planned situation. Parallelization could be achieved by minimal angulation of the drill. Clinical outcome Postoperative CT scans showed a high degree of correspondence between the postoperative implant position and the planned position (Fig. 12) [5].
Fig. 10. Position of the drill is shown relative to the preplanned implant position.
48
BAUMANN et al
Fig. 11. Intraoperative screens. Various 2D and 3D visualizations are available.
Disadvantages of computer-assisted surgery in dental implantology The available equipment is expensive, and planning and performing this procedure take more time than a conventional implant insertion procedure. In addition to the Virtual Implant System, the authors also used VISIT (Birkfellner, Center for Biomedical Engineering and Physics, Medical University, Vienna, Austria) software for planning and navigation of the implants [6]. This system runs on the SGI work station (SGI, Mountain View, CA). Advantages of computer-assisted surgery in dental implantology Dental implants can be positioned optimally considering functional and prosthodontic aspects. Necessary changes during the surgical procedure can be more easily performed by computer-assisted navigational surgery in comparison with conventional planning with the splint method. Planning changes such as additional or fewer implants or using other implant diameters can be undertaken at any time during the intervention. Also, for the mandible, nerve injury can be avoided, and operative safety is increased.
Fig. 12. Comparison of the planned (top) and postoperative (bottom) implant position in the CT scan. (From Ewers R, Schicho K, Truppe M, et al. Computer-aided navigation in dental implantology: 7 years of clinical experience. J Oral Maxillofac Surg 2004;62:32934; with permission.)
COMPUTER-ASSISTED NAVIGATIONAL SURGERY
49
Using navigated implantology, unfavorable mechanical loading may be avoided. Unfavorable mechanical loading can lead to peri-implant bone atrophy and early loss of the implant [7]. Because of the better preoperative planning and precise implant insertion, bone-demanded implant insertion can be avoided. In addition to surgical applications, computer navigated surgery also may be useful for teaching demonstrations and for teleconsultation.
Summary Computer-assisted navigational surgery oers the possibility to translate a preplanned procedure better into the operating room. However the costs for the navigation systems are very high, and the time for preparation for the surgery is longer in comparison with conventional technique. However, the navigation procedure gives more security, particularly in complex cases, and also may result in a better clinical outcome for the patient. Further development of software programs may reduce the preoperative planning time and time spent during the operation.
Further readings
Birkfellner W, Solar P, Gahleitner A, et al. In-vitro assessment of a registration protocol for image guided implant dentistry. Clin Oral Implants Res 2001;12:6978. Grunert P, Darabi K, Espinosa J, et al. Computer-aided navigation in neurosurgery. Neurosurg Rev 2003;26:7399. Hassfeld S, Mu hling J. Computer assisted oral and maxillofacial surgery - a review and assessment of technology. Int J Oral Maxillofac Surg 2001;30:213. Klein M, Hein A, Lueth T, et al. Robot-assisted placement of craniofacial implants. Int J Oral Maxillofac Implants 2003; 18:7128. Meyer U, Wiesmann HP, Runte C, et al. Evaluation of accuracy of insertion of dental implants and prosthetic treatment by computer-aided navigation in minipigs. Br J Oral Maxillofac Surg 2003;41:1028. Wanschitz F, Birkfellner W, Watzinger F, et al. Evaluation of accuracy of computer-aided intraoperative positioning of endosseous oral implants in the edentulous mandible. Clin Oral Implants Res 2002;13:5964. Watzinger F, Wagner A, Enislidis G, et al. Computer aided navigation in secondary reconstruction of posttraumatic deformities of the zygoma. J Craniomaxillofac Surg 1997;25:198202.
References
[1] Watanabe E, Watanabe T, Manaka S, et al. Three-dimensional digitizer (Neuronavigator): new equipment for computed tomography-guided stereotaxic surgery. Surg Neurol 1987;27:5437. [2] Freihofer HPM, Borstlap WA. Reconstruction of the zygomatic area: a comparison between osteotomy and onlay techniques. J Craniomaxillofac Surg 1989;17:2438. [3] Cohen SR, Kawamoto HK. Analysis and results of treatment of established posttraumatic facial deformities. Plast Reconstr Surg 1992;90:57484. [4] Marmulla R, Niederdellmann H. Surgical planning of computer-assisted reposition osteotomies. Plast Reconstr Surg 1999;104:93844. [5] Ewers R, Schicho K, Truppe M, et al. Computer-aided navigation in dental implantology: 7 years of clinical experience. J Oral Maxillofac Surg 2004;62:32934. [6] Birkfellner W, Huber K, Larson A, et al. A modular software system for computer-aided surgery and its application in oral implantology. IEEE Trans Med Imaging 2000;19:61620. [7] Hobkirk JA, Havthoulas TK. The incidence of mandibular deformation, implant numbers, and loading position on detected forces in abutments supporting xed implant superstructures. J Prosthet Dent 1998;80:16974.
Vous aimerez peut-être aussi
- Implant SeminarDocument62 pagesImplant SeminarDr. Abdulsalam Awas Dental CenterPas encore d'évaluation
- Computer-Assisted Craniomaxillofacial Surgery: Sean P. EdwardsDocument18 pagesComputer-Assisted Craniomaxillofacial Surgery: Sean P. Edwardshasan nazzalPas encore d'évaluation
- Three Dimensional Imaging in DentistryDocument26 pagesThree Dimensional Imaging in Dentistrydorasani99Pas encore d'évaluation
- Small Pox: A Child Infected With SmallpoxDocument5 pagesSmall Pox: A Child Infected With SmallpoxJavee_Viccent__5618Pas encore d'évaluation
- Somniferous Poisons: DR M. Malleswari Asso. Prof Nri Medical CollegeDocument58 pagesSomniferous Poisons: DR M. Malleswari Asso. Prof Nri Medical CollegeSudheera RachamallaPas encore d'évaluation
- Pharmacology Neurotropic Drugs 2015Document44 pagesPharmacology Neurotropic Drugs 2015Migz BrosasPas encore d'évaluation
- Rhinoplasty Dissection ManualDocument185 pagesRhinoplasty Dissection ManualVikas Vats100% (3)
- Triage in Polytauma: Prof. Dr. A. Chandrasekaran M.S., PH.D.Document73 pagesTriage in Polytauma: Prof. Dr. A. Chandrasekaran M.S., PH.D.ShrutiPas encore d'évaluation
- Dealing With Shift Work and FatigueDocument14 pagesDealing With Shift Work and FatigueA. AkbariPas encore d'évaluation
- Color Atlas of Temporomandibular Joint Surgery - QuinnDocument248 pagesColor Atlas of Temporomandibular Joint Surgery - QuinnAnonymous LnWIBo1G100% (2)
- AppendectomyDocument8 pagesAppendectomyDark AghanimPas encore d'évaluation
- An Investigatory Project ProposalDocument13 pagesAn Investigatory Project ProposalJeg B. Israel Jr.Pas encore d'évaluation
- GlossitisDocument7 pagesGlossitisLjubomirErdoglija100% (3)
- Clinical Maxillary Sinus Elevation SurgeryD'EverandClinical Maxillary Sinus Elevation SurgeryDaniel W. K. KaoPas encore d'évaluation
- Acute Effects of Radiation InjuryDocument8 pagesAcute Effects of Radiation InjuryVikas VatsPas encore d'évaluation
- A Surgical Planning and Guidance System For High Tibial OsteotomyDocument11 pagesA Surgical Planning and Guidance System For High Tibial OsteotomyKiran Kumar KalyanamPas encore d'évaluation
- 2018 - Optimizing Accuracy in Computer-Guided Implant Surgery WithDocument5 pages2018 - Optimizing Accuracy in Computer-Guided Implant Surgery WithLenny GrauPas encore d'évaluation
- Image Guided Oral Implantology and Its Application in The Placement of Zygoma ImplantsDocument12 pagesImage Guided Oral Implantology and Its Application in The Placement of Zygoma ImplantsDenisa CorneaPas encore d'évaluation
- DownloadDocument22 pagesDownloadhasan nazzalPas encore d'évaluation
- Cat e ImplantesDocument5 pagesCat e ImplantesBlas García GarcíaPas encore d'évaluation
- Cirugia Asistida Por ComputadoraDocument18 pagesCirugia Asistida Por ComputadoraPaola Alexandra LaguadoPas encore d'évaluation
- Cohen2019 Atualização Sobre Os Aspectos Atuais Da Imagem Orbital .Tomografia Computadorizada, Ressonância Magnética e UltrassonografiaDocument11 pagesCohen2019 Atualização Sobre Os Aspectos Atuais Da Imagem Orbital .Tomografia Computadorizada, Ressonância Magnética e Ultrassonografiaana clara scopelPas encore d'évaluation
- Implant Planning and Placement Using Optical Scanning and Cone Beam CT TechnologyDocument6 pagesImplant Planning and Placement Using Optical Scanning and Cone Beam CT TechnologyPraveen Raj ThakurPas encore d'évaluation
- An Automated Pelvic Bone Geometrical Feature Measurement Utilities On CT ScanningDocument7 pagesAn Automated Pelvic Bone Geometrical Feature Measurement Utilities On CT ScanningInternational Organization of Scientific Research (IOSR)Pas encore d'évaluation
- Implant OlogyDocument14 pagesImplant OlogyAya M RashidiPas encore d'évaluation
- Three-Dimensional Facial Simulation in BDocument10 pagesThree-Dimensional Facial Simulation in BVLAKORADOSPas encore d'évaluation
- FacialSurgery MMVR2005Document3 pagesFacialSurgery MMVR2005Mohamed AhmedPas encore d'évaluation
- 2019 - Yeung Et Al - Accuracy and Precision of 3d-Printed Implant Surgical Guideswith Different Implant Systems An in Vitro StudyDocument8 pages2019 - Yeung Et Al - Accuracy and Precision of 3d-Printed Implant Surgical Guideswith Different Implant Systems An in Vitro StudyRafael FedaltoPas encore d'évaluation
- From Implant Planning To Surgical Execution An Integrated Approach For Surgery in Oral ImplantologyDocument10 pagesFrom Implant Planning To Surgical Execution An Integrated Approach For Surgery in Oral ImplantologyDenisa CorneaPas encore d'évaluation
- Accuracy of Implant Placement With A Esterolitografia PDFDocument8 pagesAccuracy of Implant Placement With A Esterolitografia PDFSamuel Flores CalderonPas encore d'évaluation
- AJODO-2013 Bae 143 6 893Document9 pagesAJODO-2013 Bae 143 6 893player osamaPas encore d'évaluation
- Radiological Templates and Cad/Cam Surgical Guides-A Literature ReviewDocument37 pagesRadiological Templates and Cad/Cam Surgical Guides-A Literature ReviewMaqbul AlamPas encore d'évaluation
- 10 1016@j Prosdent 2019 05 027Document8 pages10 1016@j Prosdent 2019 05 027OctavioJose DuarteFrenkyPas encore d'évaluation
- Periodontal Plastic Surgery For Esthetic Crown LengtheningDocument4 pagesPeriodontal Plastic Surgery For Esthetic Crown LengtheningAbdelrahman GalalPas encore d'évaluation
- Accuracy of Using Computer-Aided Rapid Prototyping Templates For Mandible Reconstruction With An Iliac Crest GraftDocument9 pagesAccuracy of Using Computer-Aided Rapid Prototyping Templates For Mandible Reconstruction With An Iliac Crest GraftHương LanPas encore d'évaluation
- Intelligent X-Ray Based Training System For Pedicle Screw Placement in Lumbar VertebraeDocument7 pagesIntelligent X-Ray Based Training System For Pedicle Screw Placement in Lumbar VertebraeCatalina Sorina ParfenePas encore d'évaluation
- 3D Jaw Modeling and AnimationDocument7 pages3D Jaw Modeling and AnimationOral SurgeonPas encore d'évaluation
- Mandibular Surgery Technologic and Technical Improvements - 2014 - Oral and Maxillofacial Surgery Clinics of North AmericaDocument35 pagesMandibular Surgery Technologic and Technical Improvements - 2014 - Oral and Maxillofacial Surgery Clinics of North AmericaGabriela Lizbeth ArmentaPas encore d'évaluation
- Three-Dimensional Navigation-Guided Percutaneous Screw Fixation For Nondisplaced and Displaced Pelvi-Acetabular Fractures in A Major Trauma CentreDocument9 pagesThree-Dimensional Navigation-Guided Percutaneous Screw Fixation For Nondisplaced and Displaced Pelvi-Acetabular Fractures in A Major Trauma CentrePierre MartzPas encore d'évaluation
- Moamen M Sarhan Evaluation of The Accuracy of ImplantDocument8 pagesMoamen M Sarhan Evaluation of The Accuracy of ImplantHayley NicPas encore d'évaluation
- Rahim Ov 2011Document11 pagesRahim Ov 2011Muslikah IkaPas encore d'évaluation
- Resume C-ArmDocument4 pagesResume C-Armp27838121011Pas encore d'évaluation
- FullMouthImplant SupportedRehabilitationDocument5 pagesFullMouthImplant SupportedRehabilitationSherif HamdyPas encore d'évaluation
- Seminario 6. Implant Placement Accuracy Using Dynamic NavigationDocument8 pagesSeminario 6. Implant Placement Accuracy Using Dynamic NavigationLenny GrauPas encore d'évaluation
- Comparison Ofthree Facebowsemiadjustable Articulator2233Document6 pagesComparison Ofthree Facebowsemiadjustable Articulator2233Brijesh MaskeyPas encore d'évaluation
- Virtual Surgical Planning in Craniofacial Surgery: Harvey Chim, MBBS Nicholas Wetjen, MD Samir Mardini, MDDocument8 pagesVirtual Surgical Planning in Craniofacial Surgery: Harvey Chim, MBBS Nicholas Wetjen, MD Samir Mardini, MDR KPas encore d'évaluation
- Efficacy of Implant Placement With Surgical Guides in T 2022 Advances in OraDocument6 pagesEfficacy of Implant Placement With Surgical Guides in T 2022 Advances in OraГне ДзжPas encore d'évaluation
- Preoperative Radiologic Planning of Implant Surgery in Compromised PatientsDocument14 pagesPreoperative Radiologic Planning of Implant Surgery in Compromised PatientskochikaghochiPas encore d'évaluation
- Obturator 2023Document7 pagesObturator 2023Dina AbdelmoezPas encore d'évaluation
- Intraoperative Imaging in Orbital Reconstruction: How Does It Affect The Position of The Implant?"Document6 pagesIntraoperative Imaging in Orbital Reconstruction: How Does It Affect The Position of The Implant?"quetmauhamPas encore d'évaluation
- Ecr2011 C-1038Document12 pagesEcr2011 C-1038guilhermeytoPas encore d'évaluation
- Accuracy of Surgical Positioning of Orthodontic Miniscrews With A Computer-Aided Design and Manufacturing TemplateDocument10 pagesAccuracy of Surgical Positioning of Orthodontic Miniscrews With A Computer-Aided Design and Manufacturing TemplateDONGXU LIUPas encore d'évaluation
- Radiological Templates and Cad/Cam SURGICAL GUIDES. A Literature ReviewDocument11 pagesRadiological Templates and Cad/Cam SURGICAL GUIDES. A Literature ReviewMaqbul AlamPas encore d'évaluation
- Use of Computer Navigation in Orthopedic OncologyDocument8 pagesUse of Computer Navigation in Orthopedic OncologyFrontiersPas encore d'évaluation
- Journal of Oral Biology and Craniofacial Research: U. Vignesh, Divya Mehrotra, Dichen, Vaibhav Anand, Debraj HowladerDocument7 pagesJournal of Oral Biology and Craniofacial Research: U. Vignesh, Divya Mehrotra, Dichen, Vaibhav Anand, Debraj Howladerlowjy119411Pas encore d'évaluation
- Mock SurgeryDocument7 pagesMock SurgeryElegant Dental clinicPas encore d'évaluation
- ASME IMECE2019 CuttingGuides RevisedDocument7 pagesASME IMECE2019 CuttingGuides Revisedalexis jonathanPas encore d'évaluation
- Establishing Orbital Floor Symmetry To Support Mirror Imaging in Computer-Aided Reconstruction of The Orbital FloorDocument3 pagesEstablishing Orbital Floor Symmetry To Support Mirror Imaging in Computer-Aided Reconstruction of The Orbital FloorМихаил КуликовPas encore d'évaluation
- DocumentDocument9 pagesDocumentSuma_DewiPas encore d'évaluation
- Harvard Digital Full ArchDocument6 pagesHarvard Digital Full ArchAmit SadhwaniPas encore d'évaluation
- Conebeam CT of The Head and Neck, Part 2: Clinical ApplicationsDocument8 pagesConebeam CT of The Head and Neck, Part 2: Clinical ApplicationshaneefmdfPas encore d'évaluation
- Ankle-Foot Orthosis Made by 3D Printing TechniqueDocument7 pagesAnkle-Foot Orthosis Made by 3D Printing Techniquejose diazPas encore d'évaluation
- Klatt 2013Document4 pagesKlatt 2013Sung Soon ChangPas encore d'évaluation
- Guided Transplantation TeethDocument6 pagesGuided Transplantation TeethDrMarkHoganPas encore d'évaluation
- Eth 28049 02Document126 pagesEth 28049 02raku2121Pas encore d'évaluation
- Park 2012Document6 pagesPark 2012Yassin SalahPas encore d'évaluation
- Navigation FessDocument5 pagesNavigation FessAravind NooneyPas encore d'évaluation
- Advanced Applications of Cone Beam Computed Tomography in OrthodonticsDocument15 pagesAdvanced Applications of Cone Beam Computed Tomography in Orthodonticsaung NaingmyoPas encore d'évaluation
- Three-Dimensional Cone Beam Computed Tomography Analysis of Temporomandibular Joint Response To The Twin-Block Functional ApplianceDocument12 pagesThree-Dimensional Cone Beam Computed Tomography Analysis of Temporomandibular Joint Response To The Twin-Block Functional AppliancealejandroPas encore d'évaluation
- Jomi 5004Document8 pagesJomi 5004Fernando Ari del CorroPas encore d'évaluation
- Alternative Method For Fabrication of Power ArmDocument2 pagesAlternative Method For Fabrication of Power ArmVikas VatsPas encore d'évaluation
- Evoked PotentialDocument6 pagesEvoked PotentialVikas VatsPas encore d'évaluation
- Facial AnatomyDocument11 pagesFacial AnatomySneha SthaPas encore d'évaluation
- Vestibuloplasty With Skin Grafting and Lowering of The-HandoutDocument6 pagesVestibuloplasty With Skin Grafting and Lowering of The-HandoutVikas VatsPas encore d'évaluation
- Pikos-Mandibluar Block Autografts For Alveolar Ridge AugmentationDocument17 pagesPikos-Mandibluar Block Autografts For Alveolar Ridge AugmentationVikas VatsPas encore d'évaluation
- BJOMS 2011. Technical Note. Use of Methylene Blue For Precise Peripheral Ostectomy of Keratocystic Odontogenic TumourDocument2 pagesBJOMS 2011. Technical Note. Use of Methylene Blue For Precise Peripheral Ostectomy of Keratocystic Odontogenic TumourVikas Vats100% (1)
- HN 03-2011 Submadibular Salivary Gland Transfer PDFDocument7 pagesHN 03-2011 Submadibular Salivary Gland Transfer PDFVikas VatsPas encore d'évaluation
- 1545 1569 (2000) 037 0243:amouof 2.3.co 2Document5 pages1545 1569 (2000) 037 0243:amouof 2.3.co 2Vikas VatsPas encore d'évaluation
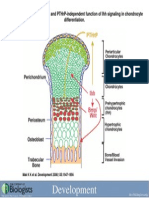
- Development 2008 Jun 135 (11) 1947-56, Fig. 7.Document1 pageDevelopment 2008 Jun 135 (11) 1947-56, Fig. 7.Vikas VatsPas encore d'évaluation
- 4 Circulation Disorders PDFDocument69 pages4 Circulation Disorders PDFSetiawan SukmadjaPas encore d'évaluation
- Pelvix Organ ProlapsDocument5 pagesPelvix Organ ProlapskazugawaPas encore d'évaluation
- Metastases Bone DiseaseDocument59 pagesMetastases Bone Diseasemuhammad rustamPas encore d'évaluation
- Asthma Treatment GuidlineDocument56 pagesAsthma Treatment GuidlineEsther OdumanyePas encore d'évaluation
- User Guide For The Participant Use Data File: American College of Surgeons National Surgical Quality Improvement ProgramDocument40 pagesUser Guide For The Participant Use Data File: American College of Surgeons National Surgical Quality Improvement Programbobobobo12341212Pas encore d'évaluation
- CGHS Rates 2014 - Nagpur1Document58 pagesCGHS Rates 2014 - Nagpur1RajatPas encore d'évaluation
- Blood Cells LabDocument7 pagesBlood Cells LabKameron WardPas encore d'évaluation
- Reading - Age With Moderate DehydrationDocument8 pagesReading - Age With Moderate DehydrationSophia IbuyanPas encore d'évaluation
- Ascorbic Acid (Vitamin C) - Side Effects, Interactions, Warning, Dosage & UsesDocument4 pagesAscorbic Acid (Vitamin C) - Side Effects, Interactions, Warning, Dosage & UsesMuhammad ZuhriPas encore d'évaluation
- Parasitology - TrematodesDocument16 pagesParasitology - TrematodesMarlex SuanPas encore d'évaluation
- Lifetree Gut Relax, An Ayurvedic Health SupplementDocument13 pagesLifetree Gut Relax, An Ayurvedic Health SupplementLifetree WorldPas encore d'évaluation
- Levonorgestrel Emergency Contraception: (Plan B or Generic Equivalent)Document2 pagesLevonorgestrel Emergency Contraception: (Plan B or Generic Equivalent)AdityaWijayaPas encore d'évaluation
- JIA - Information For TeachersDocument4 pagesJIA - Information For TeachersragingreaderPas encore d'évaluation
- LT 2 Members: Raazia Jalil, Ali Amjad & Ali Raza: Project 2 Doctors InterviewDocument3 pagesLT 2 Members: Raazia Jalil, Ali Amjad & Ali Raza: Project 2 Doctors InterviewfatimaPas encore d'évaluation
- 2017 Spine CPT Code Changes: Kim Pollock, RN, MBA, CPC, CMDPDocument4 pages2017 Spine CPT Code Changes: Kim Pollock, RN, MBA, CPC, CMDPZakariaAwaludinPas encore d'évaluation
- UNEP Directory March 2021Document34 pagesUNEP Directory March 2021Perera KusalPas encore d'évaluation
- Mycobacterial Infections Hcu Aug 2016 PDFDocument5 pagesMycobacterial Infections Hcu Aug 2016 PDFumarPas encore d'évaluation
- Pengaruh Aromaterapi Inhalasi Terhadap Penurunan Nilai Kecemasan Pasien Gagal Ginjal Kronik Yang Menjalani HemodialisaDocument6 pagesPengaruh Aromaterapi Inhalasi Terhadap Penurunan Nilai Kecemasan Pasien Gagal Ginjal Kronik Yang Menjalani HemodialisaevangelinePas encore d'évaluation
- 2012.tips For Healthy LivingDocument2 pages2012.tips For Healthy LivingNoelia Conca FrancésPas encore d'évaluation
- India's 1 Health Management LabDocument14 pagesIndia's 1 Health Management LabAjay Kumar dasPas encore d'évaluation
- Toronto Cataract ConferenceDocument6 pagesToronto Cataract ConferenceDee Margaux SantiagoPas encore d'évaluation
- Imaging For Neuro-Ophthalmic and Orbital Disease - A ReviewDocument24 pagesImaging For Neuro-Ophthalmic and Orbital Disease - A ReviewMashhoor AlfayezPas encore d'évaluation