Académique Documents
Professionnel Documents
Culture Documents
Bone Development
Transféré par
Jordan TingsonCopyright
Formats disponibles
Partager ce document
Partager ou intégrer le document
Avez-vous trouvé ce document utile ?
Ce contenu est-il inapproprié ?
Signaler ce documentDroits d'auteur :
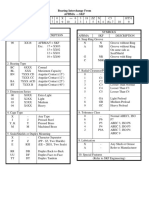
Formats disponibles
Bone Development
Transféré par
Jordan TingsonDroits d'auteur :
Formats disponibles
1. Bone Development a. Osteogenesis (Ossification)- bone tissue formation b. Stages i.
Bone formation- begins in the 2nd month of development ii. Postnatal bone growth- until early adulthood 1. After adolescence iii. Bone remodeling and repair- lifelong 2. Two Types of Ossification a. Intramembranous Ossification (Inside membrane) i. Membrane bone develops from fibrous membrane ii. Forms flat bones, e.g. clavicles(collarbones) and cranial bones b. Endochondral Ossification (forms inside cartilage) i. Cartilage( endochondral) bones form by replacing hyaline cartilage ii. Forms most of rest of skeleton 3. Endochondral Ossifications a. Uses Hyaline Cartilage models b. Requires breakdown of hyaline cartilage prior to ossification c. Dont walk around after birth because hyaline cartilage in epiphysis of long bones has not calcified. They are too soft and cannot support weight d. Long bones grow in length via epiphyseal plate cartilage 4. Postnatal Bone Growth a. Interstitial growth: i. Increase length of long bones ii. Endochondral Ossification b. Appositional growth i. Increase thickness and remodeling of all bones by osteoblasts and osteoclasts on bone surfaces ii. Intramembranous ossification 5. Growth in Length of Long Bones a. Epiphyseal plate cartilage organizes into four important functional zones: i. Proliferation (growth) ii. Hypertrophic iii. Calcification iv. Ossification (osteogenic) 6. Hormonal Regulation of Bone Growth a. Growth hormone stimulates epiphyseal plate activity b. Thyroid hormone modulates activity of growth hormone c. Testosterone and estrogens (at puberty) i. Promote adolescent growth spurts ii. End growth by inducing epiphyseal plate closure
iii. Osteoclasts destroy bones to reshape bone to adapt to the lengthening of bones 1. It resorbs the bone 7. Bone Deposit a. Occurs where bone is injured or added strength is needed b. Requires a diet rich in protein; vitamins C, D, and A; calcium; phosphorus; magnesium; and manganese c. Sites of new matrix deposit are revealed by the i. Osteoid seam 1. Unmineralized name of matrix ii. Calcification front 1. The abrupt transmission zone between the osteoid seam and the older mineralized bone 8. Bone Resorption a. Osteoclasts secrete i. Lysosomal enzymes (digest organic matrix) 1. Acid hydrolases a. Breaks down substances by adding water ii. Acids (convert calcium salts into soluble forms) b. Dissolved matrix is transcytosed across osteoclasts, enters interstitial fluid and then blood c. Gets inorganic substance into blood 9. Control of Remodeling a. What controls continual remodeling of bone? i. Hormonal mechanisms that maintain calcium homeostasis in the blood ii. Mechanical and gravitational forces 10. Hormonal Control of Blood Ca2+ a. Calcium is necessary for i. Transmissions of nerve impulses ii. Muscle contraction iii. Blood coagulation iv. Secretion by glands and nerve cells v. Cell division b. Primarily controlled by parathyroid hormone (PTH) i. Drop in Blood Ca2+ levels ii. Parathyroid glands release PTH iii. PTH stimulates osteoclasts to degrade bone matrix and release Ca2+ iv. Rise in in Blood Ca2+ levels c. May be affected to a lesser extent by calcitonin i. Rise in Blood Ca2+ levels
ii. Parafollicular cells of thyroid release calcitonin iii. Osteoblasts deposit calcium salts iv. Drop in Blood Ca2+ levels d. Leptin has also been shown to influence bone density by inhibiting osteoblasts 11. Response to mechanical Stress a. Wolffs Law: A bone grows or remodels in response or demands placed upon it b. Observations supporting Wolffs Law i. Handedness (right or left handed) results in bone of one upper limb being thicker and stronger ii. Curved bones are thickest where they are most likely to buckle iii. Trabeculae form along lines of stress iv. Large, bony projections occur where heavy, active muscles attach c. Young guys shouldnt play heavy contact sports because we risk the separation of the epiphyseal plate because the hyaline cartilage is soft 12. Classification of Bone Fractures a. Bone fractures may be classified by four either/or classifications: i. Position of bone ends after fracture: 1. Nondisplaced- ends retain normal position 2. Displaced- ends out of normal alignment ii. Completeness of the break 1. Complete- Broken all the way through 2. Incomplete- not broken all the way through iii. Orientation to the break of the long axis of the bone 1. Linear- parallel to the long axis of the bone 2. Transverse- perpendicular to the long axis of the bone iv. Whether or not bone ends penetrate skin 1. Compound (open)- bone ends penetrate skin 2. Simple (closed)- bone ends dont penetrate skin 13. Common types of fractures a. Location b. External appearance c. Nature of break 14. Stages in the healing of a bone fracture a. Hematoma forms i. Hematoma- localized collection of loose blood outside blood vessel, can form bruises ii. This is why bruising occurs where bones are broken b. Fibrocartilaginous callus forms i. Phagocytic cells clear debris ii. Osteoblasts begin forming spongy bone within one week
iii. Fibroblasts secrete collagen fibers to connect bone ends iv. Mass of tissue repair is not called fibrocartilaganous callus 1. Fibrocartilaganous callus is why movement may feel awkward or bone cannot resist to as much tension as before while bone is still not fully repaired because the callus isnt as hard as bone c. Bony Callus formation i. New trabeculae form a bony (hard) callus ii. Bony callus formation continues until firm union is formed in ~2 months d. Bone remodeling i. In response to mechanical stressors over several months ii. Final structure resembles original 15. Common Types of Fractures a. Comminuted i. Bone fragments into three or more pieces ii. Particularly common in the aged, whose bones are more brittle b. Spiral i. Ragged break occurs when excessive twisting forces are applied to a bone ii. Common sports fracture c. Depressed i. Broken bone portion is pressed inward ii. Typical of skull fracture d. Compression i. Bone is crushed ii. Common in porous bones (i.e., osteoporotic bones) subjected to extreme traumas, as in falls e. Epiphyseal i. Epiphysis separates from the diaphysis along the epiphyseal plate ii. Tends to occur where cartilage cells are dying and calcification of the matrix is occurring f. Greenstick i. Bone breaks incompletely, much in the way a green twig breaks. Only one side of the shaft breaks; the other side bends ii. Common in children, whose bones have relatively more organic matrix and are more flexible that those of adults 16. Homeostatic Imbalances a. Osteomalacia and rickets i. Calcium salts not deposited ii. Rickets (childhood disease) causes bowed legs and other bone deformations iii. Cause: Vitamin D deficiency or insufficient dietary calcium
b. Osteoporosis i. Loss of bone mass- bone resorption outpaces deposit ii. Spongy bone of spine and neck of femur become most susceptible to fracture iii. Causes 1. Lack of estrogen, calcium, or Vitamin D; petite body form; immobility; low levels of TSH; 17. Osteoperosis: Treatment and prevention a. Calcium, vitamin D, and fluoride supplements b. Increase weight bearing exercises throughout life c. Hormone (estrogen) replacement therapy (HRT) slows bone loss d. Some drugs (Fosamax, SERMs, and statins) increase bone mineral density 18. Pagets disease a. Excessive haphazard bone formation and breakdown, usually in spine, femur, pelvis, or skull b. Pagetic bone has a very high ratio of spongy bone to compact bone and reduced mineralization i. Results in a softer bone that is more susceptible to tension and compression which could result in chronic fractures and broken bones c. Unknown cause (probably viral) d. Treatments include calcitonin and bisphosphonates 19. Developmental Aspects of Bone a. Embryonic skeleton ossifies predictably so fetal age is easily determined from X rays or Sonograms b. At birth, most long bones are well ossified (except long bones) c. Nearly all bones completely ossified at age 25 i. We stop growing d. Bone mass decreases in age beginning in 4th decade e. Rate of loss determined by genetics and environmental factors f. In old age, resorption predominates i. Which could lead to osteoperosis
Vous aimerez peut-être aussi
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeD'EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeÉvaluation : 4 sur 5 étoiles4/5 (5794)
- Chapter 1 Chemical FoundationsDocument4 pagesChapter 1 Chemical FoundationsJordan TingsonPas encore d'évaluation
- Shoe Dog: A Memoir by the Creator of NikeD'EverandShoe Dog: A Memoir by the Creator of NikeÉvaluation : 4.5 sur 5 étoiles4.5/5 (537)
- 1 Pes2160Spr2011PreLab5Document4 pages1 Pes2160Spr2011PreLab5Jordan TingsonPas encore d'évaluation
- Lecture 9 Pulmonary FundamentalspdfDocument9 pagesLecture 9 Pulmonary FundamentalspdfJordan TingsonPas encore d'évaluation
- The Yellow House: A Memoir (2019 National Book Award Winner)D'EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Évaluation : 4 sur 5 étoiles4/5 (98)
- Lecture10Physiological Responses To Aerobic TrainingpdfDocument4 pagesLecture10Physiological Responses To Aerobic TrainingpdfJordan TingsonPas encore d'évaluation
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceD'EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceÉvaluation : 4 sur 5 étoiles4/5 (895)
- Lecture11-Aerobic Endurance Exercise TrainingDocument5 pagesLecture11-Aerobic Endurance Exercise TrainingJordan TingsonPas encore d'évaluation
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersD'EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersÉvaluation : 4.5 sur 5 étoiles4.5/5 (344)
- Lecture6Strength TrainingDocument8 pagesLecture6Strength TrainingJordan TingsonPas encore d'évaluation
- The Little Book of Hygge: Danish Secrets to Happy LivingD'EverandThe Little Book of Hygge: Danish Secrets to Happy LivingÉvaluation : 3.5 sur 5 étoiles3.5/5 (399)
- Chem162 MolecularGeometryDocument1 pageChem162 MolecularGeometryJordan TingsonPas encore d'évaluation
- Grit: The Power of Passion and PerseveranceD'EverandGrit: The Power of Passion and PerseveranceÉvaluation : 4 sur 5 étoiles4/5 (588)
- Full Court Dribble TestDocument3 pagesFull Court Dribble TestJordan TingsonPas encore d'évaluation
- The Emperor of All Maladies: A Biography of CancerD'EverandThe Emperor of All Maladies: A Biography of CancerÉvaluation : 4.5 sur 5 étoiles4.5/5 (271)
- Exp 11 - Crystal StructureDocument3 pagesExp 11 - Crystal StructureJordan TingsonPas encore d'évaluation
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaD'EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaÉvaluation : 4.5 sur 5 étoiles4.5/5 (266)
- Dulce Nombre de Maria Cathedral-BasilicaDocument8 pagesDulce Nombre de Maria Cathedral-BasilicaJordan TingsonPas encore d'évaluation
- Never Split the Difference: Negotiating As If Your Life Depended On ItD'EverandNever Split the Difference: Negotiating As If Your Life Depended On ItÉvaluation : 4.5 sur 5 étoiles4.5/5 (838)
- Mozart Fantasy in D MinorDocument4 pagesMozart Fantasy in D MinorASertavis100% (3)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryD'EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryÉvaluation : 3.5 sur 5 étoiles3.5/5 (231)
- Basics of Population EducationDocument4 pagesBasics of Population EducationLAILANIE DELA PENAPas encore d'évaluation
- Islam and Civilization (Analysis Study On The History of Civilization in Islam) Muhammad Hifdil IslamDocument18 pagesIslam and Civilization (Analysis Study On The History of Civilization in Islam) Muhammad Hifdil IslamLoveth KonniaPas encore d'évaluation
- On Fire: The (Burning) Case for a Green New DealD'EverandOn Fire: The (Burning) Case for a Green New DealÉvaluation : 4 sur 5 étoiles4/5 (73)
- The Process: by Andy ZoppeltDocument4 pagesThe Process: by Andy ZoppeltMark Stephen HuBertPas encore d'évaluation
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureD'EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureÉvaluation : 4.5 sur 5 étoiles4.5/5 (474)
- Nomenclatura SKFDocument1 pageNomenclatura SKFJuan José MeroPas encore d'évaluation
- Team of Rivals: The Political Genius of Abraham LincolnD'EverandTeam of Rivals: The Political Genius of Abraham LincolnÉvaluation : 4.5 sur 5 étoiles4.5/5 (234)
- Para Lec CombinedDocument83 pagesPara Lec CombinedClent Earl Jason O. BascoPas encore d'évaluation
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyD'EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyÉvaluation : 3.5 sur 5 étoiles3.5/5 (2259)
- Influence of Aesthetics Attributes of Brand Web Pages On Customer Brand EngagementDocument22 pagesInfluence of Aesthetics Attributes of Brand Web Pages On Customer Brand EngagementNOOR AKMA AIDAPas encore d'évaluation
- Underground Equipment SelectionDocument44 pagesUnderground Equipment SelectionCherotich Silas cheboseiPas encore d'évaluation
- IBM BladeCenter S RedBookDocument36 pagesIBM BladeCenter S RedBookGuillermo García GándaraPas encore d'évaluation
- DP November 2017 Examination Schedule en PDFDocument4 pagesDP November 2017 Examination Schedule en PDFSuperlucidoPas encore d'évaluation
- Paper-Czechowski-Slow-strain-rate Stress Corrosion Testing of Welded Joints of Al-Mg AlloysDocument4 pagesPaper-Czechowski-Slow-strain-rate Stress Corrosion Testing of Welded Joints of Al-Mg Alloysjavo0128Pas encore d'évaluation
- The Unwinding: An Inner History of the New AmericaD'EverandThe Unwinding: An Inner History of the New AmericaÉvaluation : 4 sur 5 étoiles4/5 (45)
- Liftchain (LC2A) Catalog AirHoistDocument10 pagesLiftchain (LC2A) Catalog AirHoisteduardshark100% (1)
- Management of DredgedExcavated SedimentDocument17 pagesManagement of DredgedExcavated SedimentMan Ho LamPas encore d'évaluation
- Valdez, Shenny RoseDocument3 pagesValdez, Shenny Roseyeng botzPas encore d'évaluation
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreD'EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreÉvaluation : 4 sur 5 étoiles4/5 (1090)
- Colour FastnessDocument37 pagesColour FastnessSivakumar K100% (1)
- EDS-A-0101: Automotive Restricted Hazardous Substances For PartsDocument14 pagesEDS-A-0101: Automotive Restricted Hazardous Substances For PartsMuthu GaneshPas encore d'évaluation
- 12-Week Off-Season Training Programme Junior Rugby (U18 - U21)Document5 pages12-Week Off-Season Training Programme Junior Rugby (U18 - U21)LeBron JamesPas encore d'évaluation
- Indoor Air Quality Standard Procedures - 2014 RevDocument12 pagesIndoor Air Quality Standard Procedures - 2014 RevFioriAmeliaHathawayPas encore d'évaluation
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)D'EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Évaluation : 4.5 sur 5 étoiles4.5/5 (120)
- Bardonna MenuDocument16 pagesBardonna MenuFarley ElliottPas encore d'évaluation
- English2 Q2 Summative Assessment 4 2Document4 pagesEnglish2 Q2 Summative Assessment 4 2ALNIE PANGANIBANPas encore d'évaluation
- SMC VM Eu PDFDocument66 pagesSMC VM Eu PDFjoguvPas encore d'évaluation
- Iodide and Bromide Ions in Brackish Water, Seawater, and Brines D 3869 - 04Document12 pagesIodide and Bromide Ions in Brackish Water, Seawater, and Brines D 3869 - 04stevgonPas encore d'évaluation
- 2017 Classification of Periodontal and Peri-Implant Diseases and Conditions. Decision Making Algorithms For Clinical PracticeDocument40 pages2017 Classification of Periodontal and Peri-Implant Diseases and Conditions. Decision Making Algorithms For Clinical PracticebbPas encore d'évaluation
- Test7 PointersDocument16 pagesTest7 PointersPratibha DwivediPas encore d'évaluation
- Clinical Reviews: The Management of Children With Gastroenteritis and Dehydration in The Emergency DepartmentDocument13 pagesClinical Reviews: The Management of Children With Gastroenteritis and Dehydration in The Emergency DepartmentRina Dewi AnggraeniPas encore d'évaluation
- Free Electron TheoryDocument8 pagesFree Electron TheoryNeelam KapoorPas encore d'évaluation
- 1n5711 RF Detector Diode 70v PIV DatasheetDocument3 pages1n5711 RF Detector Diode 70v PIV DatasheetgordslaterPas encore d'évaluation
- Skincare Routine Order Cheat SheetDocument10 pagesSkincare Routine Order Cheat SheetYel Salenga100% (3)
- Tips For A Healthy PregnancyDocument2 pagesTips For A Healthy PregnancyLizaPas encore d'évaluation
- Her Body and Other Parties: StoriesD'EverandHer Body and Other Parties: StoriesÉvaluation : 4 sur 5 étoiles4/5 (821)
- Compiled LecsDocument24 pagesCompiled LecsNur SetsuPas encore d'évaluation
- AIR Conditioner: Owner'S ManualDocument52 pagesAIR Conditioner: Owner'S Manualashley diazPas encore d'évaluation