Académique Documents
Professionnel Documents
Culture Documents
Antib 1
Transféré par
Rimy SinghDescription originale:
Titre original
Copyright
Formats disponibles
Partager ce document
Partager ou intégrer le document
Avez-vous trouvé ce document utile ?
Ce contenu est-il inapproprié ?
Signaler ce documentDroits d'auteur :
Formats disponibles
Antib 1
Transféré par
Rimy SinghDroits d'auteur :
Formats disponibles
i n d i a n j o u r n a l o f d e n t i s t r y 4 ( 2 0 1 3 ) 2 9 e3 4
Available online at www.sciencedirect.com
journal homepage: www.elsevier.com/locate/ijd
Review Article
Antibiotics as an intracanal medicament in endodontics: A review
Neelam Mittal a, Jyoti Jain b,*
a b
Professor, Department of Conservative Dentistry & Endodontics, Faculty of Dental Sciences, I.M.S, B.H.U, Varanasi, UP, India. Postgraduate Student, Department of Conservative Dentistry & Endodontics, Faculty of Dental Sciences, I.M.S, B.H.U, Varanasi, UP, India.
article info
Article history: Received 22 October 2011 Accepted 2 March 2012 Keywords: Antibiotics Endodontics Root canal irrigation and intracanal medicament
abstract
Antibiotics are an extremely valuable addition to the armamentarium available to health practitioners for management of bacterial infections. Due to the potential risk of adverse systemic effects of systemic applications and ineffectiveness of systemic antibiotics in the necrotic pulpless tooth and the periradicular tissues, local application of antibiotics may be a more effective mode for delivering antibiotics to infected root canals. This paper reviews the applications of antibiotics and antibiotics containing medicaments in endodontics. 2012 Indian Journal of Dentistry. All rights reserved.
1.
Introduction
The role of microorganisms in development and perpetuation of pulpal and periapical diseases have clearly been demonstrated in animal models and human studies. Elimination of microorganisms from infected root canals is a complicated task. Numerous measures have been described to reduce the numbers of root canal microorganisms, including the use of various instrumentation techniques, irrigation regimens, and intracanal medicaments. There is no solid evidence in the literature that mechanical instrumentation alone results in a bacteria-free root canal system. Considering the complex anatomy of root canal pulp space, this is not surprising. On the contrary, there is in vitro and clinical evidence that mechanical instrumentation leaves signicant portions of the root canal walls untouched. Hence, complete elimination of bacteria from the root canal system by instrumentation alone
is unlikely to be achieved. Therefore, some sort of irrigation/ disinfection is necessary to kill microorganisms. Simply, chemical treatment of the root canal can be arbitrarily divided into irrigants, rinses, and inter visit medicaments. Several studies have been conducted on antibiotics as root canal irrigants and medicaments. Hence, the purpose of this article was to review the use of intracanal antibiotics during endodontic treatment and when managing traumatized teeth.
2.
History
For several decades antibiotic have been prescribed in different disciplines of medicine and dentistry.1 The rst reported local use of an antibiotic in endodontic treatment was
* Corresponding author. E-mail address: drjyoti82@gmail.com (J. Jain). 0975-962X/$ e see front matter 2012 Indian Journal of Dentistry. All rights reserved. http://dx.doi.org/10.1016/j.ijd.2012.03.002
30
i n d i a n j o u r n a l o f d e n t i s t r y 4 ( 2 0 1 3 ) 2 9 e3 4
in 1951 when Grossman used a polyantibiotic paste known as PBSC (Penicillin, Bacitracin, Streptomycin, and Caprylate sodium).2 PBSC contained penicillin to target gram-positive organisms, Bacitracin for penicillin-resistant strains, Streptomycin for gram-negative organisms, and caprylate sodium to target yeasts. Later, nystatin replaced caprylate sodium as an antifungal agent in a similar medicament and named as PBSN (penicillin, bacitracin, streptomycin, and nystatin).3
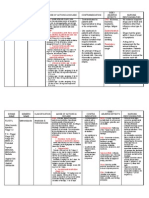
3. Antibiotics and antibiotics containing medicaments in endodontics
3.1. Ledermix paste
In 1960 Ledermix paste was developed by Schroeder and Triadan and was marketed in Europe by Lederle Pharmaceuticals in 1962.4 Ledermix is a glucocorticosteroid antibiotic compound and the development of Ledermix paste was based on the use of corticosteroid to control pain and inammation. Schroeder and Triadan initially incorporated chloramphenicol in their rst trials but when Lederle Pharmaceuticals became the manufacturer, the antibiotic was changed to demeclocycline HCl. Today, Ledermix paste remains a combination of the same tetracycline antibiotic, demeclocycline HCl (at a concentration of 3.2%), and a corticosteroid, triamcinolone acetonide (concentration 1%), in a polyethylene glycol base.4 The two therapeutic components of the Ledermix (i.e., triamcinolone and demeclocycline) are capable of diffusing through dentinal tubules and cementum to reach the periodontal and periapical tissues.5 Abbott et al. showed dentinal tubules were the major supply route of the active components to the periradicular tissues, while the apical foramen was not as signicant as a supply route.6 However, within the peripheral parts of the dentine and in the periradicular tissues, the concentration achieved through diffusion is insufcient to inactivate bacteria, especially over time.7 Heling and Pecht evaluated the efcacy of the Ledermix paste in the disinfection of dentinal tubules.8 Their ndings showed that Ledermix and 3% tetracycline in a hydrous base were effective in reducing the amount of Staphylococcus aureus in dentinal tubules after seven days of incubation and also after recontamination. They were not effective after 24 h. Abbott showed that the intradental use of the Ledermix paste and Ledermix cement is unlikely to result in any systemic side effects.9 Pierce et al. demonstrated histologically that the Ledermix eliminated experimentally induced external inammatory root resorption in vivo.10 Taylor et al. evaluated effects of Ledermix paste and Pulpdent paste on mouse broblasts and on bacteria in vitro.11 And their nding showed that Ledermix was found to reversibly inhibit mitosis while present in the concentrations range 10(-3) to 10(-6) mg/ml. Mixing with Pulpdent did not modify this antimitotic effect. Ledermix killed mouse broblasts at 10(-3) mg/ml and above, while Pulpdent killed at 1 mg/ml and above. The toxic effect of Ledermix was slightly inhibited by mixing it with Pulpdent. Thong et al. compared the effect of calcium hydroxide (Pulpdent) and Ledermix paste on periodontal healing and root resorption following replantation histomorphometrically.12 They found that periodontal ligament inammation and inammatory
root resorption were markedly inhibited by both calcium hydroxide and corticosteroid-antibiotic relative to untreated controls. Replacement resorption was lowest in the corticosteroid-antibiotic group, and signicantly more normal periodontal ligament was present in this group than in calcium hydroxide and control groups. Wong and Sae-Lim evaluated the effect of immediate intracanal Ledermix on root resorption of delayed-replanted monkey teeth.13 The positive control group was root lled and replanted after 1 h while the negative control group was root lled and replanted immediately. The negative control group produced highly signicant favorable healing and unfavorable healing as compared to the Ledermix group. The Ledermix group only showed signicantly higher occurrence of complete healing (35.46%) compared to the positive control group (16.58%), but there were no signicant differences in the inammatory root resorption and replacement resorption. Bryson et al. evaluated the effect of immediate intracanal placement of Ledermix paste (R) on healing of replanted dog teeth after extended dry times (1 h).14 Their nding showed that the Ledermix triamcinolone, and demeclocycline had statistically signicantly more favorable healing than the group lled with Gutta Percha replanted after 1-h dry time (positive control).15 There was no statistically signicant difference between the Ledermix group and the triamcinolone group, while the tetracycline group showed less favorable healing than the negative control, the Ledermix group, and the triamcinolone group. Trope evaluated the relationship of intracanal medicaments to endodontic are-ups.16 Formocresol, Ledermix, and calcium hydroxide were placed in strict sequence irrespective of the presence or absence of symptoms or radiographic signs of apical periodontitis. He found no signicant difference in the are-up rate among the three intracanal medicaments. Ehrmann et al. investigated the relationship of postoperative pain to three different medicaments placed in the root canal after a complete biomechanical debridement of the root canal system in patients presenting for emergency relief of pain.17 They found that painful teeth with acute apical periodontitis that had been dressed with Ledermix paste gave rise to less pain than that experienced by patients who had a dressing of calcium hydroxide, or no dressing at all. Kim et al. investigated the effects of the Ledermix paste as an intracanal medicament on discoloration of mature teeth, whether the discoloring effects were related to the method of application, as well as the effects of sunlight upon discoloration of mature teeth.18 Results demonstrated that after 12 weeks, sunlight exposure had caused dark gray-brown staining of the teeth in the Ledermix groups, but this did not occur when the teeth were kept in the dark. More severe staining was noted when Ledermix paste lled the pulp chamber than when the paste was restricted to below the cementoenamel junction (CEJ). They suggested that if placement of the Ledermix was restricted to below the gingival margin, such effects could be minimized. In another study, they investigated the effects of the Ledermix paste as an intracanal medicament on discoloration of mature teeth, whether the discoloring effects were related to the method of application, as well as the effects of sunlight upon discoloration of immature teeth. After 12 weeks, sunlight exposure
i n d i a n j o u r n a l o f d e n t i s t r y 4 ( 2 0 1 3 ) 2 9 e3 4
31
had caused dark gray-brown staining in the Ledermix groups but this did not occur when the teeth were kept in the dark. More severe staining was noted when Ledermix paste lled the pulp chamber than when the paste was restricted to below the CEJ and when teeth were exposed to sunlight.19 When compared to the results of a similar study using mature teeth, the results were similar but the immature teeth were more severely stained than the mature teeth. The calcium hydroxide paste caused an increase in lightness and yellowness in immature teeth.19
3.2.
Combination of Ledermix and calcium hydroxide
The combination of Ledermix paste with calcium hydroxide was advocated by Schroeder initially for the treatment of necrotic teeth with incomplete root formation.4 A 50e50 mixture of Ledermix paste and calcium hydroxide has also been advocated as an intracanal dressing in cases of infected root canals.12 It has been shown that the 50e50 mixture results in slower release and diffusion of the active components of Ledermix paste, which makes the medicament last longer in the canal.20 This in turn helps to maintain the sterility of the canal for longer and also maintains a higher concentration of all components within the canal.20 Seow showed that for Streptococcus sanguis and S. aureus, the addition of only 25% by volume of Calyxl (a calcium hydroxide in saline paste) (Otto and Co. Frankfurt, Germany) to Ledermix converted the zone of complete inhibition originally seen in Ledermix to one of only partial inhibition.21 Chu et al. compared the efcacy of disinfection of root canals with periapical radiolucencies when treated with either antibiotics/ steroid medicaments (Ledermix or Septomixine) or a calcium hydroxide paste (Calasept, Speiko, Darmstadt, Germany).22 Their nding showed that in the Ledermix group, 38 strains of bacteria were recovered. The Septomixine group had 25 strains, and the Calasept group had 25 strains. Gram-positive facultative anaerobic cocci (including staphylococci and streptococci) were more prevalent than the gram-negative obligate anaerobic rods after treatment in all three groups.
intracanal dressing.24 Following initial bacteriological sampling and routine instrumentation, clindamycin powder mixed to a paste with saline was applied for 14 days. The presence or absence of bacteria was determined in samples taken immediately after removal of the dressing, and after a period of seven days during which the canals were lled with sampling uid. The results indicated that clindamycin offered no advantage over conventional root canal dressings, such as calcium hydroxide. However, the concentration of the active drug and its ability to penetrate deeply into the root canal system was not clear. Nonetheless, the clindamycin paste was successful in eliminating bacterial growth in 21 of 25 teeth tested by the 14th day. In the four remaining teeth, Enterococci constituted the dominant ora despite antibiotic treatment. Lin et al. compared the antibacterial effect of clindamycin and tetracycline in bovine dentinal tubule model, as well as using the agar diffusion test.25 Their ndings showed that clindamycin signicantly reduced the amount of viable bacteria in each dentin layer compared with them tetracycline.
3.5.
Metronidazole
3.3.
Septomixine Forte
Septomixine Forte (Septodont, Saint- Maur, France) contains two antibiotics: Neomycin and Polymixin B sulfate. Tang et al. who demonstrated that a routine one-week application of Septomixine Forte was not effective in inhibiting residual intracanal bacterial growth between appointments.23 In addition, although the anti-inammatory (corticosteroid) agent, dexamethasone (at a concentration of 0.05%), is clinically effective, triamcinolone is considered to have less systemic side effects.
3.4.
Clindamycin
Clindamycin is effective against many of the representative endodontic pathogens, including Actinomyces, Eubacterium, Fusobacterium, Propionobacterium, Microaerophilic, Streptococci, Peptococcus, Peptostreptococcus, Veillonella, Prevotella, and Porphyromonas. Molander et al. investigated the effect of clindamycin on root canal infection when placed as an
Metronidazole is a nitroimidazole compound that exhibits a broad spectrum of activity against protozoa and anaerobic bacteria. Roche and Yoshimori investigated the activity of metronidazole against clinical isolates from odontogenic abscesses in vitro.26 Their ndings showed that metronidazole had excellent activity against anaerobes isolated from odontogenic abscesses but had no activity against aerobes. Siqueira and de Uzeda evaluated the antibacterial activity of 0.12% chlorhexidine gel, 10% metronidazole gel; calcium hydroxide plus distilled water, calcium hydroxide plus camphorated paramonochlorophenol (CPMC), and calcium hydroxide plus glycerin using agar diffusion test.27 The results revealed that calcium hydroxide/CPMC paste was effective against all bacterial strains tested. Chlorhexidine was also inhibitory to all strains. It was about as effective as calcium hydroxide/CPMC paste against most of the strains. Metronidazole also caused inhibition of growth of all obligate anaerobes tested and was more effective than calcium hydroxide/ CPMC against two strains. In another study, Lima et al. evaluated the effectiveness of chlorhexidine or antibiotics-based medications in eliminating Enterococcus faecalis biolms.28 They found there were signicant differences between the formulations tested. The association of clindamycin with metronidazole signicantly reduced the number of cells in one-day biolms. However, of all medications tested, only 2% chlorhexidine-containing medications were able to thoroughly eliminate most of both one-day and three-day E. faecalis biolm. Wang et al. evaluated the effect of metronidazole-chlorhexidine solution on treatment of chronic apical periodontitis.29 They found that the effective rate of metronidazole- chlorhexidine solution treatment was 97.6%. Yu et al. evaluated the effect of a paste made of erythromycin ethylsuccinate, metronidazole and camphorated paramonochlorophenol (CP) to sterilize the root canal.30 There nding showed that there was no signicant difference comparing erythromycin-ethylsuccinate- metronidazole-CP with formocresol (FC) in root canal sterilization. Therefore, the
32
i n d i a n j o u r n a l o f d e n t i s t r y 4 ( 2 0 1 3 ) 2 9 e3 4
irritability and poisonousness of the paste could be reduced by using erythromycin-ethylsuccinate-metronidazole-CP instead of FC. They concluded that the root canal sterilization with erythromycin-ethylsuccinate-metronidazole-CP was a safe and effective method to promote the restoration of root apex diseases. Gao et al. investigated a sustained release delivery Gutta Percha point containing metronidazole (SRDGM) for root canal disinfection, and determined the drug concentration in vitro and the time that the device maintained the effective drug concentration.31 Their ndings showed that the effective metronidazole concentration released lasted more than 10 days. On the 10th day, there was also 33.13 mg/ml metronidazole released, which was more than a minitory inhibitory concentration of metronidazole. Hoelscher et al. evaluated the antimicrobial effects of ve antibiotics (Amoxicillin, Penicillin, Clindamycin, Metronidazole, and Doxycycline) when added to Kerr Pulp Canal Sealer EWT against E. faecalis.32 They found that all mentioned antibiotics except for metronidazole, could enhance the antimicrobial efcacy of the sealer. Krithikadatta et al. evaluated the disinfection of dentinal tubules using 2% chlorhexidine gel, 2% metronidazole gel, bioactive glass (S53P4) in comparison with calcium hydroxide.33 Their nding demonstrated that the overall percentage inhibition of bacterial growth (at 200 mg and 400 mg depth) was 100% with 2% chlorhexidine gel. The inhibition of growth was moderate with 2% metronidazole gel (86.5%), followed by bioactive glass (62.8%) and calcium hydroxide (58.5%).
tract.38 Instead of the standard root canal treatment protocol and apexication, antimicrobial agents (metronidazole and ciprooxacin) were used in the canal, after which the canal was left empty. Radiographic examination showed the start of apical closure ve months after the completion of the antimicrobial protocol. Thickening of the canal wall and complete apical closure was conrmed 30 months after the treatment, indicating the revascularization potential of a young permanent tooth pulp into a bacteria-free root canal space. Takushige et al. evaluated the efcacy of polyantibiotic paste consisted of metronidazole, ciprooxacin, and minocycline, on the clinical outcome of so-called Lesion Sterilization and Tissue Repair, (LSTR) therapy in primary teeth with periradicular lesions.39 Results showed that in all cases, clinical symptoms such as gingival swelling, sinus tracts, induced dull pain, spontaneous dull pain, and pain on biting disappeared after treatment, although in four cases clinical signs and symptoms were nally resolved only after retreatment using the same procedures. Thus, gingival abscesses and stulae, if present, disappeared after a few days.
3.7.
BioPure (MTAD)
3.6.
Triple antibiotic paste
The infection of the root canal system is considered to be a polymicrobial infection, consisting of both aerobic and anaerobic bacteria. Because of the complexity of the root canal infection, it is unlikely that any single antibiotic could result in effective sterilization of the canal. More likely a combination would be needed to address the diverse ora encountered. A combination of antibiotics would also decrease the likelihood of the development of resistant bacterial strains. The combination that appears to be most effective consists of metronidazole ciprooxacin, and minocycline.34,35 Sato et al. evaluated the potential of a mixture of ciprooxacin, metronidazole and minocycline to kill bacteria in the deep layers of root canal dentine in situ.36 Results showed that no bacteria were recovered from the infected dentine of the root canal wall 24 h after application of the drug combination, except in one case in which a few bacteria were recovered. Hoshino et al. investigated the antibacterial effect of a mixture of ciprooxacin, metronidazole, and minocycline with and without the addition of rifampicin, on bacteria from infected dentine of root canal walls.37 The efcacy was also determined against bacteria of carious dentine and infected pulps, which may the precursory bacteria of infected root dentine. They found that alone, none of the drugs resulted in complete elimination of bacteria. However, in combination; these drugs were able to consistently sterilize all samples. Iwaya et al. reported a necrotic immature mandibular second premolar with periapical involvement and sinus
BioPure (Dentsply, Tulsa Dental, Tulsa, OK, USA), otherwise known as MTAD (mixture of tetracycline, acid and detergent), is a relatively new root canal irrigant, which was introduced by Torabinejad & Johnson (2003). This solution contains doxycycline (at a concentration of 3%), citric acid (4.25%) and a detergent, Polysorbate 80 (0.5%) (Torabinejad & Johnson 2003). It has been shown that MTAD is able to remove the smear layer (Torabinejad & Johnson 2003) and is effective against E. faecalis (Shabahang & Torabinejad 2003, Shabahang et al., 2003, Torabinejad et al., 2003b).40
3.8.
Side effects
The well-documented side effects to antibiotics commonly prescribed for endodontic infections are hypersensitivity reactions and drug fevers to penicillin and other beta lactam antibiotics, Pseudomembranous colitis, which occasionally occurs with clindamycin or other antibiotics, nausea, vomiting, and gastrointestinal distress common with macrolides, photosensitivity that may accompany tetracycline and renal toxicity that may be associated with the use of aminogycosides.41 Gastrointestinal side effects are common among many medications, but in particular macrolide antibiotics. Clarithromycin (such as Biaxin XL) and azithromycin are associated with less GI irritation than erythromycin.42
4.
Conclusion
The local application of antibiotics within the root canal system may be a more effective mode for delivering such drugs than systemic routes of administration. Ledermix has antiinammatory, antibacterial and antiresorptive properties, all of which help to reduce the periapical inammatory reaction including clastic-cell mediated resorption. This material has been shown to signicantly lower the incidence of inammatory and replacement resorption, and thus prompts more
i n d i a n j o u r n a l o f d e n t i s t r y 4 ( 2 0 1 3 ) 2 9 e3 4
33
favorable healing in replanted teeth. A 50:50 mixture of Ledermix paste and calcium hydroxide has been advocated as an intracanal dressing in cases of pulpless infected root canals, pulp necrosis and infection with incomplete root formation (apexication), perforations, inammatory root resorption, inammatory periapical bone resorption, and for the treatment of large periapical radiolucent lesions. Clindamycin alone or in an ethylene vinyl acetate vehicle can reduce the bacterial load inside the root canal system (including dentinal tubules) signicantly. A triple antibiotic paste consisting of metronidazole, ciprooxacin, and minocycline has been reported to be very effective in the disinfection of the root canal system. BioPure (MTAD) is effective in removing the smear layer. Among the well-documented side effects to antibiotics commonly prescribed for endodontic infections (penicillins) are hypersensitivity reactions and drug fevers.
references
1. Abbott PV. Selective and intelligent use of antibiotics in endodontics. Aust Endod J. 2000;26:30e39. 2. Grossman LI. Polyantibiotic treatment of pulpless teeth. J Am Dent Assoc. 1951;43:265e278. 3. Weine FS. Endodontic therapy. 3rd ed. Mosby; 1982. p. 325. 4. Athanassiadis B, Abbott PV, Walsh LJ. The use of calcium hydroxide, antibiotics and biocides as antimicrobial medicaments in endodontics. Aust Dent J. 2007;52:S64eS82. 5. Abbott PV. Medicaments: aids to success in endodontics. Part 1. A review of literature. Aust Dent J. 1990;35:438e448. 6. Abbott PV, Heithersay GS, Hume WR. Release and diffusion through human tooth roots in vitro of corticosteroid and tetracycline trace molecules from Ledermix paste. Endod Dent Traumatol. 1988;4:55e62. 7. Abbott PV, Hume WR, Pearman JM. Antibiotics and endodontics. Aust Dent J. 1990;35:50e60. 8. Heling I, Pecht M. Efcacy of Ledermix paste in eliminating Staphylococcus aureus from infected dentinal tubules in vitro. Endod Dent Traumatol. 1991;7:251e254. 9. Abbott PV. Systemic release of corticosteroids following intradental use. Int Endod J. 1992;25:189e191. 10. Pierce A, Heithersay G, Lindskog S. Evidence for direct inhibition of dentinoclasts by a corticosteroid/antibiotic endodontic paste. Endod Dent Traumatol. 1988;4:44e45. 11. Taylor MA, Hume WR, Heithersay GS. Some effects of Ledermix paste and Pulpdent paste on mouse broblasts and on bacteria in vitro. Endod Dent Traumatol. 1989;5:266e273. 12. Thong YL, Messer HH, Siar CH, Saw LH. Periodontal response to two intracanal medicaments in replanted monkey incisors. Dent Traumatol. 2001;17:254e259. 13. Wong KS, Sae-Lim V. The effect of intracanal Ledermix on root resorption of delayed-replanted monkey teeth. Dent Traumatol. 2002;18:309e315. 14. Bryson E, Levin L, Banchs F, Abbott PV, Trope M. Effect of immediate intracanal placement of Ledermix paste on healing of replanted dog teeth after extended dry times. Dent Traumatol. 2002;18:316e321. 15. Chen H, Teixeira FB, Ritter AL, Levin L, Trope M. The effect of intracanal antiinammatory medicaments on external root resorption of replanted dog teeth after extended extra-oral dry time. Dent Taumatol. 2008;24:74e78. 16. Trope M. Relationship of intracanal medicaments to endodontic are-ups. Endod Dent Traumatol. 1990;6:226e229.
17. Ehrmann EH, Messer HH, Adams GG. The relationship of intracanal medicaments to postoperative pain in endodontics. Int Endod J. 2003;36:868e875. 18. Kim ST, Abbott PV, McGinley P. The effects of Ledermix paste on discoloration of mature teeth. Int Endod J. 2000 May;33(3):227e232. 19. Kim ST, Abbott PV, McGinley P. The effects of Ledermix paste on discoloration of immature teeth. Int Endod J. 2000;33:233e237. 20. Abbott PV, Hume WR, Heithersay GS. Effect of combining Ledermix and calcium hydroxide pastes on the diffusion of corticosteroid and tetracycline through human tooth roots in vitro. Endod Dent Traumatol. 1989;5:188e192. 21. Seow WK. The effects of dyadic combinations of endodontic medicaments on microbial growth inhibition. Red Dent. 1990;12:292e297. 22. Chu FC, Leung WK, Tsang PC, Chow TW, Samaranayake LP. Identication of cultivable microorganisms from root canals with apical periodontitis following two-visit endodontic treatment with antibiotics/steroid or calcium hydroxide dressings. J Endod. 2005;32:17e23. 23. Tang G, Samaranayake LP, Yip HK. Molecular evaluation of residual endodontic microorganisms after instrumentation, irrigation and medication with either calcium hydroxide or Septomixine. Oral Dis. 2004;10:389e397. 24. Molander A, Dahlen G. Evaluation of the antibacterial potential of tetracycline or erythromycin mixed with calcium hydroxide as intracanal dressing against E. faecalis in vivo. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2003;96:744e750. 25. Lin S, Levin L, Peled M, Weiss EI, Fuss Z. Reduction of viable bacteria in dentinal tubules treated with clindamycin or tetracycline. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2003;96:751e756. 26. Roche Y, Yoshimori RN. In vitro activity of spiramycin and metronidazole alone or in combination against clinical isolates from odontogenic abscesses. J Antimicrob Chemother. 1997;40:353e377. 27. Siqueira Jr JF, de Uzeda M. Intracanal medicaments: evaluation of the antibacterial effects of chlorhexidine, metronidazole, and calcium hydroxide associated with three vehicles. J Endod. 1997;23:167e169. 28. Lima KC, Fava LR, Siqueira Jr JF. Susceptibilities of Enterococcus faecalis biolms to some antimicrobial medications. J Endod. 2001;27:616e619. 29. Wang ZP, Wang D, Zhang LJ, Kong L. The observation of the effect of metronidazole-chlorhexidine solution on treatment of periapical periodontitis. Shanghai Kou Qiang Yi Xue. 2003;12:244e246. 30. Yu X, Song M, Xu L. Clinical evaluation of the paste of erythromycin ethylsuccinate-metronidazole CP for root canal sterilization. Shanghai Kou Qiang Yi Xue. 2000;9:143e144. 31. Gao J, Wang ZP, Li XG, Wang D, Zhang L. The preparation and in vitro release test of sustained release delivery gutta percha point containing metronidazole. Shanghai Kou Qiang Yi Xue. 2004;13:557e560. 32. Hoelscher AA, Bahcall JK, Maki JS. In vitro evaluation of the antimicrobial effects of a root canal sealer-antibiotic combination against Enterococcus faecalis. J Endod. 2006;32:145e147. 33. Krithikadatta J, Indira R, Dorothykalyani AL. Disinfection of dentinal tubules with 2 percent chlorhexidine, 2 percent metronidazole, bioactive glass when compared with calcium hydroxide as intracanal medicaments. J Endod. 2007;33:1473e1476. 34. Windley 3rd W, Teixeira F, Levin L, Sigurdsson A, Trope M. Disinfection of immature teeth with a triple antibiotic paste. J Endod. 2005;31:439e443. 35. Trope M. Treatment of immature teeth with nonvital pulps and apical periodontitis. Endod Top. 2006;14:51e59.
34
i n d i a n j o u r n a l o f d e n t i s t r y 4 ( 2 0 1 3 ) 2 9 e3 4
36. Sato I, Ando-Kurihara N, Kota K, Iwaku M, Hoshino E. Sterilization of infected root canal dentine by topical application of a mixture of ciprooxacin, metronidazole and minocycline in situ. Int Endod J. 1996;29:118e124. 37. Hoshino E, Ando-Kurihara N, Sato I, et al. In vitro antibacterial susceptibility of bacteria taken from infected root dentine to a mixture of ciprooxacin, metronidazole and minocycline. Int Endod J. 1996;29:125e130. 38. Iwaya SI, Ikawa M, Kubota M. Revascularization of an immature permanent tooth with apical periodontitis and sinus tract. Dent Traumatol. 2001;17:185e187.
39. Takushige T, Cruz EV, Asgor Moral A, Hoshino E. Endodontic treatment of primary teeth using a combination of antibacterial drugs. Int Endod J. 2004;37:132e138. 40. Torabinejad M, Shabahang S, Aprecio R, Kettering JD. The antimicrobial effect of MTAD: an in vitro investigation. J Endodontics. 2003;29:400e403. 41. Cunha BA. Antibiotic side effects. Med Clin North Am. 2001;85:149e185. 42. Baker KA, Fotos PG. The management of odontogenic infections. A rationale for appropriate chemotherapy. Dent Clin North Am. 1994;38:689e706.
Vous aimerez peut-être aussi
- Shoe Dog: A Memoir by the Creator of NikeD'EverandShoe Dog: A Memoir by the Creator of NikeÉvaluation : 4.5 sur 5 étoiles4.5/5 (537)
- EndoDocument1 pageEndoSaca AnastasiaPas encore d'évaluation
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeD'EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeÉvaluation : 4 sur 5 étoiles4/5 (5794)
- Laureys 2013 Journal of EndodonticsDocument5 pagesLaureys 2013 Journal of EndodonticsRimy SinghPas encore d'évaluation
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceD'EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceÉvaluation : 4 sur 5 étoiles4/5 (895)
- Antibiotics in EndodonticsDocument10 pagesAntibiotics in EndodonticstarekrabiPas encore d'évaluation
- The Yellow House: A Memoir (2019 National Book Award Winner)D'EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Évaluation : 4 sur 5 étoiles4/5 (98)
- 01 - 004 An Indirect Cast Post and Core TechniqueDocument3 pages01 - 004 An Indirect Cast Post and Core TechniqueRimy Singh100% (1)
- Grit: The Power of Passion and PerseveranceD'EverandGrit: The Power of Passion and PerseveranceÉvaluation : 4 sur 5 étoiles4/5 (588)
- General DentistryDocument4 pagesGeneral DentistryRimy SinghPas encore d'évaluation
- The Little Book of Hygge: Danish Secrets to Happy LivingD'EverandThe Little Book of Hygge: Danish Secrets to Happy LivingÉvaluation : 3.5 sur 5 étoiles3.5/5 (400)
- Minimal Intervention DentistryDocument3 pagesMinimal Intervention DentistryRimy SinghPas encore d'évaluation
- The Emperor of All Maladies: A Biography of CancerD'EverandThe Emperor of All Maladies: A Biography of CancerÉvaluation : 4.5 sur 5 étoiles4.5/5 (271)
- Endodontic Insruments-1Document114 pagesEndodontic Insruments-1Rimy Singh100% (1)
- Never Split the Difference: Negotiating As If Your Life Depended On ItD'EverandNever Split the Difference: Negotiating As If Your Life Depended On ItÉvaluation : 4.5 sur 5 étoiles4.5/5 (838)
- Drug Hunt: Larr Sumalpong N22Document11 pagesDrug Hunt: Larr Sumalpong N22Larr SumalpongPas encore d'évaluation
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyD'EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyÉvaluation : 3.5 sur 5 étoiles3.5/5 (2259)
- FlagystatinDocument18 pagesFlagystatinChristian YongkyPas encore d'évaluation
- On Fire: The (Burning) Case for a Green New DealD'EverandOn Fire: The (Burning) Case for a Green New DealÉvaluation : 4 sur 5 étoiles4/5 (74)
- Regañon - Rle Case # 1Document22 pagesRegañon - Rle Case # 1Darla Janyll RegañonPas encore d'évaluation
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureD'EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureÉvaluation : 4.5 sur 5 étoiles4.5/5 (474)
- High Risk PregnancyDocument5 pagesHigh Risk Pregnancygracie_greys5755Pas encore d'évaluation
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryD'EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryÉvaluation : 3.5 sur 5 étoiles3.5/5 (231)
- Clinical Aspects Fluor Albus of Female and Treatment: Literature ReviewDocument11 pagesClinical Aspects Fluor Albus of Female and Treatment: Literature ReviewDafit VdayPas encore d'évaluation
- Team of Rivals: The Political Genius of Abraham LincolnD'EverandTeam of Rivals: The Political Genius of Abraham LincolnÉvaluation : 4.5 sur 5 étoiles4.5/5 (234)
- Parasites Life CycleDocument12 pagesParasites Life CyclebretonPas encore d'évaluation
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaD'EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaÉvaluation : 4.5 sur 5 étoiles4.5/5 (266)
- Neospark-Performance Through ExcellenceDocument1 pageNeospark-Performance Through ExcellenceEssam Abd AlRahmanPas encore d'évaluation
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersD'EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersÉvaluation : 4.5 sur 5 étoiles4.5/5 (345)
- Drug Drug Interactions 2Document133 pagesDrug Drug Interactions 2joo saadPas encore d'évaluation
- Chemotherapy of Protozoal InfectionsDocument34 pagesChemotherapy of Protozoal InfectionsSri RamPas encore d'évaluation
- The Unwinding: An Inner History of the New AmericaD'EverandThe Unwinding: An Inner History of the New AmericaÉvaluation : 4 sur 5 étoiles4/5 (45)
- Central Nervous System: Drug of Choices Notes - Kent Andrei Paelma Bsn-2FDocument22 pagesCentral Nervous System: Drug of Choices Notes - Kent Andrei Paelma Bsn-2FOfficially RandomPas encore d'évaluation
- CPG - Antimicrobial - Antibiotics in Periodontal TherapyDocument8 pagesCPG - Antimicrobial - Antibiotics in Periodontal TherapyTrue GeminiPas encore d'évaluation
- 3.2. QuantificationDocument80 pages3.2. QuantificationBrhanu belayPas encore d'évaluation
- Vulvovaginal Candidiasis and Bacterial VaginosisDocument16 pagesVulvovaginal Candidiasis and Bacterial VaginosisAdnanda Maulan100% (1)
- Chemotherapy For Protozoal InfectionsDocument32 pagesChemotherapy For Protozoal InfectionsJia YingPas encore d'évaluation
- Emnc 4 North Drug StudyDocument12 pagesEmnc 4 North Drug StudyFrancesca Aurea MagumunPas encore d'évaluation
- Dailymed - Nlm.nih - Gov METRONIDAZOLEDocument16 pagesDailymed - Nlm.nih - Gov METRONIDAZOLELip StickPas encore d'évaluation
- Antibiotic Use in Dog, Cat and HumanDocument20 pagesAntibiotic Use in Dog, Cat and Humankhangsiean89Pas encore d'évaluation
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreD'EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreÉvaluation : 4 sur 5 étoiles4/5 (1090)
- Bsava Protect PosterDocument1 pageBsava Protect PosterNilamdeen Mohamed ZamilPas encore d'évaluation
- Drug StudyDocument7 pagesDrug Studykakienz100% (7)
- Double Anaerobic Coverage Guideline AgainstDocument2 pagesDouble Anaerobic Coverage Guideline AgainstioanaPas encore d'évaluation
- Local Drug Delivery in PeriodonticsDocument40 pagesLocal Drug Delivery in PeriodonticsruchaPas encore d'évaluation
- Housejob GuideDocument11 pagesHousejob GuideSam James100% (1)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)D'EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Évaluation : 4.5 sur 5 étoiles4.5/5 (121)
- Vaginitis: Diagnosis and Treatment: Barry L. Hainer, MD, and Maria V. Gibson, MD, PHDDocument9 pagesVaginitis: Diagnosis and Treatment: Barry L. Hainer, MD, and Maria V. Gibson, MD, PHDMonika PuspitasariPas encore d'évaluation
- VaginitisDocument20 pagesVaginitisgpicaulyPas encore d'évaluation
- Tinidazole Is An AntiDocument6 pagesTinidazole Is An AntiNoi Maya Anggrita SariPas encore d'évaluation
- Metronidazole Vaginosis-1992Document4 pagesMetronidazole Vaginosis-1992maryPas encore d'évaluation
- Drugs RevDocument84 pagesDrugs RevdeasyPas encore d'évaluation
- Drug Study - Tamiflu, FlagylDocument2 pagesDrug Study - Tamiflu, Flagylmark_gain100% (1)
- Pharm SimpleNursing PDFDocument192 pagesPharm SimpleNursing PDFDacanay M.A.Pas encore d'évaluation
- Her Body and Other Parties: StoriesD'EverandHer Body and Other Parties: StoriesÉvaluation : 4 sur 5 étoiles4/5 (821)
- Basic and Essential PharmacologyDocument75 pagesBasic and Essential PharmacologyIorjiim WaltersPas encore d'évaluation