Académique Documents
Professionnel Documents
Culture Documents
Jurnal Kardiologi 1
Transféré par
Idi Nagan RayaDescription originale:
Titre original
Copyright
Formats disponibles
Partager ce document
Partager ou intégrer le document
Avez-vous trouvé ce document utile ?
Ce contenu est-il inapproprié ?
Signaler ce documentDroits d'auteur :
Formats disponibles
Jurnal Kardiologi 1
Transféré par
Idi Nagan RayaDroits d'auteur :
Formats disponibles
Am J Cardiovasc Dis 2013;3(2):71-78 www.AJCD.
us /ISSN:2160-200X/AJCD1302001
Original Article Lone aspiration thrombectomy without stenting in young patients with ST elevation myocardial infarction
Gohar Jamil1, Mujgan Jamil2, Ahmed Abbas1, Swapna Sainudheen1, Sadek Mokahal1, Anwer Qureshi1
1
Division of Cardiology, Tawam Hospital, PO Box 15258, Al Ain, United Arab Emirates; 2Department of Internal Medicine, Tawam Hospital, PO Box 15258, Al Ain, United Arab Emirates Received February 6, 2013; Accepted April 3, 2013; Epub June 10, 2013; Published June 15, 2013 Abstract: Plaque rupture with thrombotic occlusion without severe underlying coronary atherosclerosis is frequently observed during primary percutaneous coronary intervention (pPCI) for ST-segment elevation myocardial infarction (STEMI). These lesions are stented even if post thrombectomy mild underlying coronary artery disease (CAD) is noted. The value of mechanical thrombus aspiration alone lone aspiration thrombectomy (LAT) without stenting is not well studied. We present a retrospective analysis of patients receiving LAT as the only pPCI therapy for STEMI. Between January 2008 and March 2012, 202 young patients underwent pPCI for acute STEMI at our institution. From this group 10 patients had LAT as definitive therapy. LAT was favored if post thrombectomy minimal underlying CAD was noted, and concerns regarding long term treatment cost and compliance with dual antiplatelet therapy (DAPT) was an issue. All patients received ASA, clopidogrel, heparin and eptifibatide. DAPT was maintained for at least 1 month. One patient was lost to follow-up. At one month, all remaining 9 patients were free of MACE. At six weeks one patient had recurrent STEMI after abruptly discontinuing all his medications. Re-occlusion at the site of prior plaque rupture was stented, and treatment compliance was urged. Short term follow up at 2 months available for 5 patients and 2 years for 3 patients revealed no adverse consequences, the remaining patients had returned to their home countries. Conclusion: In selected young patients presenting with acute STEMI, LAT without balloon angioplasty or stenting is feasible and is associated with favorable short and long-term outcome. Keywords: Aspiration thrombectomy, percutaneous coronary intervention, angioplasty, ST-segment elevation myocardial infarction, young patients, coronary artery disease
Introduction Myocardial infarction in patients less than 50 years is uncommon. It usually presents as single vessel disease with thrombotic occlusion at the site of endothelial erosion or plaque rupture [1-4]. PCI is an effective and preferred method for restoring epicardial blood flow in acute MI [5, 6]. Distal embolization of atherothrombotic material in the infarct related artery (IRA) before and during PCI is associated with more extensive myocardial infarction, possibility of a no reflow phenomenon and higher mortality [7]. To avert these complications manual thrombus aspiration before stenting of IRA is advised [8, 9]. Following thrombosuction, however, stenting of underlying diseased coronary segment is undertaken irrespective of residual atherosclerotic disease. Randomized trials of acute MI have not addressed the question of manual
thrombus aspiration without stenting. This approach is infrequently reported in literature [10-16]. and no specific guidelines are available. In recent publications [17, 18]. Thrombus aspiration alone may be a viable option in patients presenting with STEMI or rescue angioplasty. Tawam Hospital is a regional tertiary care hospital situated in Al Ain, UAE. It serves a heterogeneous population with substantial number of expatriates originating from South East Asia and the Far East. In this latter group, presentation with MI is at a significantly younger age. Predisposition for this early presentation of symptomatic CAD is not well understood. Management of these patients is affected by cost considerations, compliance issues and fragmented follow up care. Considering these socioeconomic factors, which significantly
Lone aspiration thrombectomy without stenting
Table 1. Baseline Characteristics of Patients
Patients (n=10) Male (female) Age (mean SD) Smoking History Diabetes Mellitus Family History Hypercholesterolemia Hypertension Previous CAD Polycythemia 9 (1) 36.3 6 2 1 4 1 0 1
Table 2. Cardiac Biomarkers, Lipids and LV Function
Diagnostic Test Peak CPK Peak troponin (mean SD) LDL-C mg/dl (mean SD) HDL-C mg/dl (mean SD) Triglyceride mg/dl (mean SD) LVEF (%) at discharge (mean SD) Mean Value (+/-SD) 2586.6 65.1 142.3 (+/-51.04) 36.3 (+/-11.05) 218.8 (+/-134.66) 55 (+/-5.9)
of re-occlusion. Lesions that were deemed favorable for aspiration only were in non-tortuous and non-calcified vessels with no residual lesion or mild residual stenosis (< 40%) with smooth angiographic appearance of the vessel lumen and restoration of TIMI-3 flow. Noninfracted vessels being angiographically normal were additional reassuring information for a low total atherosclerotic burden. The decision to avoid stenting was based on preference of treating cardiologist. High-risk patients or lesions assessed to be complex, calcified or in a tortuous vessel, or more than mild stenosis post thrombus extraction were determined to be unsuitable for lone thrombosuction. Procedure Access was obtained through right radial artery. Diagnostic angiography was performed with 5 French (Fr) radial TIG catheter (Terumo Medical, Somerset, NJ). JR and XB guide-catheters (Cordis Corporation Miami Lakes FL) were used for PCI. BMW guidewire (Abbott Vascular Santa Clara CA) was successfully used in all instances. Export catheters (6F) (Medtronic vascular Incorporation, Santa Rosa, CA) were used for thrombus aspiration. Intra coronary Adenosine, Nicardipine, or Nitroprusside was used in six cases to manage slow or no reflow due to large thrombus burden. Adjuvant treatment All patients received loading dose of aspirin 300 mg, clopidogrel 600 mg, heparin 5000 units bolus followed by heparin infusion and eptifibatide prior to coronary intervention. Heparin infusion was maintained for 48 hrs targeting PTT between 50-70. Eptifibatide was infused for 18-24 hours. High dose aspirin at 300 mg daily and clopidogrel 75 mg daily was maintained for the first 4 weeks with reduction in aspirin dose to 100 mg thereafter. Other treatment included beta-blockers, high dose statin and ACE-I. To ensure early compliance patient received first month of treatment free of any additional cost upon hospital discharge. Follow up Follow up information was gathered during office visit, telephone contact and review of
Total cholesterol mg/dl (mean SD) 211.5 (+/-58.77)
impact treatment compliance and outcome, we have managed these patients selectively with thrombus aspiration alone without stenting of IRA, if post thrombectomy minimal or no residual atherosclerotic disease was present on angiography. In this retrospective analysis of our experience with mechanical thrombus aspiration alone in 10 patients with a mean age of 36.3 years we discuss major adverse cardiovascular events (MACE) during short term and long term follow up and the problem with treatment compliance and fragmented care. Materials and methods Identification of studied patients Between January 2008 and March 2012, 202 patients younger than 50 years of age underwent primary PCI for acute STEMI at our institution. In this group 10 patients (5%) were treated with mechanical thrombus aspiration alone. Criteria for lone thrombosuction Lone thrombosuction was performed if residual lesion was felt by the operator to be at low risk
72
Am J Cardiovasc Dis 2013;3(2):71-78
Lone aspiration thrombectomy without stenting
Table 3. Age, Ethnicity, BMI and Vessel Characteristics Pre and Post PCI
Patient Age Asian No (years) Race 1 35 South East 2 30 South East 3 39 South East 4 41 South East 5 38 South East 6 41 South East 7 30 South East 8 29 Middle East 9 48 Far East 10 32 Middle East BMI (mean 24.98) 24.3 25.3 21.4 19.8 27.1 28.9 21.4 24.8 23.9 32.9 Stenosis before/ after Lone Throm- other IRA bus Aspiration vessels LAD 80/20% Normal LAD 70/40% OM 100/40% TIMI flow before PCI 2 TIMI flow after PCI 3 3 3 3 3 3 3 3 3 3 Intracoronary adenosine NicardipineNitroprusside 0 1 1 1 1 1 1 0 0 0
Normal 2 Normal 0 D1/ 0 RCA Normal 2 Normal 0 Normal 0 Normal 0 Normal 0 Normal 2
LCX 100/40% LAD 90/30% RCA 100/mild LAD 100/30% RCA 100/40% LAD 100/10% RCA 90/0%
electronic medical record. Any adverse cardiovascular event or compliance issue was appropriately documented. Statistical analysis All analysis was performed on Epi info version 3.5.3 software package. Results Baseline characteristics Clinical characteristics are summarized in Table 1 These patients had no prior history of CAD. The mean age for the group was 36.3 years. Nine patients were male. Cigarette smoking was documented in six patients, hyperlipidemia in four, diabetes in two and hypertension in one. Hypercoaguable state due to polycythemia was diagnosed in one. Strong family history of premature coronary artery disease was present in one as shown in Table 1 . Routine diagnostic studies Routine diagnostic studies revealed a moderate sized myocardial infarction. Overall LV systolic function was mildly reduced. Significant
dyslipidemia was present at admission as shown in Table 2. Coronary angiography In Table 3 each patient is represented detailing age, ethnicity and BMI. Corresponding angiographic characteristic of the IRA for each patient, success following Lone thrombus aspiration and use of adjuvant intracoronary medications is detailed. Seven patients originated from South East Asia, one from Far East and two were of Middle Eastern origin. The mean BMI for the group was 25. Left anterior descending (LAD) artery was the culprit artery in five, right coronary artery (RCA) in three and left circumflex (LCX) in two patients respectively. Prior to any mechanical intervention TIMI 0 flow was noted in six patients while the rest had TIMI 2 flow in culprit vessel. Post thrombosuction TIMI 3 flow was restored in all patients. Six patients received intracoronary adenosine, Nicardipine or Nitroprusside for slow flow phenomena. Post thrombus aspiration all patient had either no visible lesion or less than 40% residual stenosis. The non culprit vessels were angiographically normal in nine out of ten patients with one patient having non obstructive disease in first diagonal (D1) and RCA. Am J Cardiovasc Dis 2013;3(2):71-78
73
Lone aspiration thrombectomy without stenting
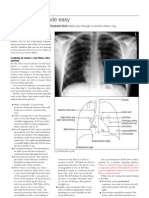
Figure 1. A: Total occlusion of LAD; (B) Clot retrieved by export catheter; (C) Post LAT angiogram shows less than 40% stenosis; (D) Angiogram 6 weeks later confirms vessel patency.
Clinical outcome One patient did not return for specified follow up at 4 weeks. No MACE was noted in the other 9 patients at 4 weeks. Patient #8 (29 years old smoker), underwent pre discharge coronary CT angiogram, which showed moderate (50-69%) residual stenosis. He stopped all medications five weeks post discharge and presented a week thereafter with STEMI. Re-occlusion of RCA at the same site of previous plaque rupture was confirmed on angiogram. The culprit lesion was stented and he was re-counseled regarding treatment compliance. Repeat invasive
angiography for chest pain in patient #9, 6 weeks after initial hospitalization confirmed vessel patency with minimal residual lesion and TIMI 3 flow as shown in Figure 1 . Subsequent follow up was available in 5 patients (three patients returned to their home countries) at two months and in 3 patients at 1 year and 2 years after their index MI as presented in Figure 2. Discussion In acute STEMI intra-luminal thrombus is seen in 90% patients [19]. Distal embolization in
74
Am J Cardiovasc Dis 2013;3(2):71-78
Lone aspiration thrombectomy without stenting
Figure 2. Clinical follow up and outcome.
STEMI occurs in approximately 15% cases and is associated with no reflow [20, 21] reduced angiographic success, reduced ST segment resolution, larger infarct size and higher mortality [3]. Thrombus aspiration is an effective adjunctive therapy to prevent distal embolization and is recommended in patients with STEMI undergoing mechanical revascularization [22, 23]. Despite the clinical [24], and angiographic [25, 26] benefit, the response to thrombus aspiration is variable [27]. Majority of acute myocardial infarctions occur in the setting of thrombotic occlusion of coronary artery subsequent to plaque rupture and less frequently from thrombus associated with 75
plaque erosion. The underlying atherosclerotic plaque is mostly not obstructive [28, 29]. Intracoronary thrombus can be treated with embolic protection devices, mechanical thrombectomy [9]. or manual aspiration. Results were not conclusive regarding their usefulness in earlier trials and meta-analysis [24, 26, 30, 31]. The TAPAS trial [9] brought manual thrombectomy into the mainstream, and showed mortality reduction at one-year follow-up. Thrombus aspiration in this and other studies was an effective adjunctive therapy to prevent distal embolization [22, 23]. The above emphasizes the concept that intracoronary thrombus, not plaque burden is the Am J Cardiovasc Dis 2013;3(2):71-78
Lone aspiration thrombectomy without stenting
cause of vessel obstruction, and lone thrombectomy may be enough in selected cases. In our series we show the short-term safety and feasibility of lone thrombectomy without stenting of the infarct related artery when TIMI 3 flow has been established and a non-significant residual lesion is present. Appropriate selection of patients for this approach is important, as we have previously outlined. Early compliance with prescribed treatment, in particular dual antiplatelet therapy is likely important. This approach is cost effective, avoids problems inherent with coronary stenting and the need for long-term dual antiplatelet therapy. Study limitations This study has the inherent limitation of a retrospective chart review. The small number of patients and inconsistent follow up influences our observations. Treatment decisions were based on angiographic appearance post thrombectomy. Additional information from Intravascular ultrasound (IVUS) may have confirmed our visual estimate of mild residual atherosclerosis. During follow up assessment objective reevaluation of plaque progression was not done. Functional testing or coronary CTA may have been insightful. Conclusion The presented cases demonstrate the effectiveness of manual thrombus aspiration in restoring TIMI 3 flow. It also confirms the safety and feasibility of thrombus aspiration alone in selected young patients with acute ST elevation myocardial infarction. Additional evaluation of plaque progression with functional testing or coronary CTA may be useful. Disclaimers of conflict of interest None.
Address correspondence to: Dr. Gohar Jamil, Tawam Hospital, PO Box 15258, Al Ain, UAE. Phone: 00971501398358; Fax: 0097137672560; E-mail goharjamil@gmail.com [9] [6] [2] [3] Falk E, Shah PK, Fuster V. Coronary Plaque disruption. Circulation 1995; 92: 657-671. Farb A, Burke AP, Tang AL, Liang TY, Mannan P, Smialek J, Virmani R. Coronary plaque erosion without rupture into a lipid core. A frequent cause of coronary thrombosis in sudden coronary death. Circulation 1996; 93: 1354-1363. Van der Wal AC, Becker AE, van der Loos CM, Das PK. Site of initial rupture or erosion of thrombosed coronary atherosclerotic plaques is characterized by an inflammatory process irrespective of the dominant morphology. Circulation 1994; 89: 36-44. Antman EM, Anbe DT, Armstrong PW, Bates ER, Green LA, Hand M, Hochman JS, Krumholz HM, Kushner FG, Lamas GA, Mullany CJ, Ornato JP, Pearle DL, Sloan MA, Smith SC Jr, Alpert JS, Anderson JL, Faxon DP, Fuster V, Gibbons RJ, Gregoratos G, Halperin JL, Hiratzka LF, Hunt SA, Jacobs AK; American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Writing Committee to Revise the 1999 Guidelines for the Management of Patients With Acute Myocardial Infarction). ACC/AHA guidelines for the management of patients with ST-elevation myocardial infarction--executive summary: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Writing Committee to Revise the 1999 Guidelines for the Management of Patients With Acute Myocardial Infarction). Circulation 2004; 110: 588-636. Keeley EC, Boura JA, Grines CL. Primary angioplasty versus intravenous thrombolytic therapy for acute myocardial infarction: a quantitative review of 23 randomised trials. Lancet 2003; 361: 13-20. Henriques JP, Zijlstra F, Ottervanger JP, de Boer MJ, van t Hof AW, Hoorntje JC, Suryapranata H. Incidence and clinical significance of distal embolization during primary angioplasty for acute myocardial infarction. Eur Heart J 2002; 23: 1112-1117. Svilaas T, Vlaar PJ, van der Horst IC, Diercks GF, de Smet BJ, van den Heuvel AF, Anthonio RL, Jessurun GA, Tan ES, Suurmeijer AJ, Zijlstra F. Thrombus aspiration during primary percutaneous coronary intervention. N Engl J Med 2008; 358: 557-567. Vlaar PJ, Svilaas T, van der Horst IC, Diercks GF, Fokkema ML, de Smet BJ, van den Heuvel AF, Anthonio RL, Jessurun GA, Tan ES, Suurmeijer AJ, Zijlstra F. Cardiac death and reinfarction after 1 year in the Thrombus Aspiration during Percutaneous coronary intervention in Acute myocardial infarction Study (TAPAS): a 1-year follow-up study. Lancet 2008; 371: 19151920.
[4]
[5]
[7]
[8]
References
[1] Davies MJ, Thomas A. Thrombosis and acute coronary lesions in sudden cardiac ischemic death. N Engl J Med 1984; 310: 1137-1140.
76
Am J Cardiovasc Dis 2013;3(2):71-78
Lone aspiration thrombectomy without stenting
[10] Talarico GP, Burzotta F, Trani C, Porto I, Leone AM, Niccoli G, Coluccia V, Schiavoni G, Crea F. Thrombus aspiration without additional ballooning or stenting to treat selected patients with ST-elevation myocardial infarction. J Invasive Cardiol 2010; 22: 489-492. [11] Sakai K, Inoue K, Nobuyoshi M. Aspiration thrombectomy of a massive thrombotic embolus in acute myocardial infarction caused by coronary embolism. Int Heart J 2007; 48: 387392. [12] Hajek P, Alan D, Vejvoda J, Linhartova K, Shapa P. Hajsmannova Z, Veselka J, Treatment of a large Left main coronary artery thrombus by aspiration thrombectomy. J Thromb Thrombolysis 2009; 27: 352-354. [13] Kotooka N, Otsuka Y, Yasuda S, Morii I, Kawamura A, Miyazaki S. Three cases of acute myocardial infarction due to coronary embolism. Treatment using a thrombus aspiration device. Jpn Heart J 2004; 45: 861-866. [14] Wilson AM, Ardehali R, Brinton TJ, Yeung AC, Vagelos R. Successful removal of a paradoxical coronary embolus using an aspiration catheter. Nat Clin Pract Cardiovasc Med 2006; 3: 633-636. [15] Fokkema ML, Vlaar PJ, Svilaas T. Thrombus aspiration as definitive mechanical intervention for ST-elevation myocardial infarction: a report of five cases. J Invasive Cardiol 2008; 20: 242244. [16] Avaramides D, Raisakis K, Matsakas E. Acute inferior ST-segment elevation myocardial infarction treated with primary angioplasty using only a Pronto aspiration catheter. J Invasive Cardiol 2008; 20: E177-9. [17] Kramer MC, Verouden NC, Li X, Koch KT, van der Wal AC, Tijssen JG, de Winter RJ. Thrombus aspiration alone during primary percutanous coronary intervention as definitive treatment in acute ST-elevation myocardial infarction. Catheter Cardiovasc Interv 2012; 79: 860867. [18] Jamil G, Ouda H, Jamil M, Qureshi A. Mechanical thrombectomy alone as a definite therapy for rescue angioplasty. BMJ Case Rep 2013; 2013. [19] DeWood MA, Spores J, Notske R, Mouser LT, Burroughs R, Golden MS, Lang HT. Prevalence of total coronary occlusion during the early hours of transmural myocardial infarction. N Engl J Medicine 1980; 303: 897-902. [20] Sakuma T, Leong-Poi H, Fisher NG, Goodman NC, Kaul S. Further insights into the no-reflow phenomenon after primary angioplasty in acute myocardial infarction: the role of microthromboemboli. J Am Soc Echocardiogr 2003; 16: 15-21. [21] Niccoli G, Burzotta F, Galiuto L, Crea F. Myocardial no-reflow in humans. J Am Coll Cardiol 2009; 54: 281-292. [22] Kushner FG, Hand M, Smith SC Jr, King SB 3rd, Anderson JL, Antman EM, Bailey SR, Bates ER, Blankenship JC, Casey DE Jr, Green LA, Hochman JS, Jacobs AK, Krumholz HM, Morrison DA, Ornato JP, Pearle DL, Peterson ED, Sloan MA, Whitlow PL, Williams DO. 2009 focused updates: ACC/AHA guidelines for the management of patients with ST-elevation myocardial infarction (updating the 2004 guideline and 2007 focused update) and ACC/AHA/SCAI guidelines on percutaneous coronary intervention (updating the 2005 guideline and 2007 focused update) a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol 2009; 54: 2205-2241. [23] Van de Werf F, Bax J, Betriu A, Blomstrom-Lundqvist C, Crea F, Falk V, Filippatos G, Fox K, Huber K, Kastrati A, Rosengren A, Steg PG, Tubaro M, Verheugt F, Weidinger F, Weis M; ESC Committee for Practice Guidelines (CPG). Management of acute myocardial infarction in patients presenting with persistent ST-segment elevation: the Task Force on the Management of ST-Segment Elevation Acute Myocardial Infarction of the European Society of Cardiology. Eur Heart J 2008; 29: 2909-2945. [24] Burzotta F, De Vita M, Gu YL, Isshiki T, Lefvre T, Kaltoft A, Dudek D, Sardella G, Orrego PS, Antoniucci D, De Luca L, Biondi-Zoccai GG, Crea F, Zijlstra F. Clinical impact of thrombectomy in acute ST-elevation myocardial infarction: an individual patient-data pooled analysis of 11 trials. Eur Heart J 2009; 30: 2193-2203. [25] Burzotta F, Trani C, Romagnoli E, Mazzari MA, Rebuzzi AG, De Vita M, Garramone B, Giannico F, Niccoli G, Biondi-Zoccai GG, Schiavoni G, Mongiardo R, Crea F. Manual thrombus-aspiration improves myocardial reperfusion: the randomized evaluation of the effect of mechanical reduction of distal embolization by thrombusaspiration in primary and rescue angioplasty (REMEDIA) trial. J Am Coll Cardiol 2005; 46: 371-376. [26] De Luca G, Dudek D, Sardella G, Marino P, Chevalier B, Zijlstra F. Adjunctive manual thrombectomy improves myocardial perfusion and mortality in patients undergoing primary percutaneous coronary intervention for ST-elevation myocardial infarction: a meta-analysis of randomized trials. Eur Heart J 2008; 29: 3002-3010. [27] Burzotta F, Trani C, Romagnoli E, Belloni F, Biondi-Zoccai GG, Mazzari MA, De Vita M, Giannico F, Garramone B, Niccoli G, Rebuzzi AG, Mongiardo R, Schiavoni G, Crea F. A pilot study
77
Am J Cardiovasc Dis 2013;3(2):71-78
Lone aspiration thrombectomy without stenting
with a new, rapid-exchange, thrombus-aspirating device in patients with thrombus-containing lesions: the Diver C.E. study. Catheter Cardiovasc Interv 2006; 67: 887-893. [28] Falk E. Plaque rupture with severe pre-existing stenosis precipitating coronary thrombosis. Characteristics of coronary atherosclerotic plaques underlying fatal occlusive thrombi. Br Heart J 1983; 50: 127-134. [29] Vetrovec GW, Cowley MJ, Overton H, Richardson DW. Intracoronary thrombus in syndromes of unstable myocardial ischemia. Am Heart J 1981; 102: 1202-1208. [30] Bavery AA, Kumbhani DJ, Bhatt DL. Role of adjunctive thrombectomy and embolic protection devices in acute myocardial infarction: a comprehensive meta-analysis of randomized trials. Eur Heart J 2008; 29: 2989-3001. [31] Ali A, Cox D, Dib N, Brodie B, Berman D, Gupta N, Browne K, Iwaoka R, Azrin M, Stapleton D, Setum C, Popma J; AIMI Investigators. Rheolytic thrombectomy with percutaneous coronary intervention for infarct size reduction in acute myocardial infarction: 30-day results from a multicenter randomized study. J Am Coll Cardiol 2006; 48: 244-252.
78
Am J Cardiovasc Dis 2013;3(2):71-78
Vous aimerez peut-être aussi
- Chest X Rays Made EasyDocument3 pagesChest X Rays Made EasyHaluk AlibazogluPas encore d'évaluation
- Cara Membaca Foto Thoraks Yang BaikDocument2 pagesCara Membaca Foto Thoraks Yang BaikIdi Nagan RayaPas encore d'évaluation
- Cara Membaca Foto Thoraks Yang BaikDocument2 pagesCara Membaca Foto Thoraks Yang BaikIdi Nagan RayaPas encore d'évaluation
- Identitas Subjektif Objektif Assessment TerapiDocument1 pageIdentitas Subjektif Objektif Assessment TerapiIdi Nagan RayaPas encore d'évaluation
- TiroidDocument14 pagesTiroidIdi Nagan RayaPas encore d'évaluation
- Acute Liver Failure Gagal Hati AkutDocument12 pagesAcute Liver Failure Gagal Hati AkutIdi Nagan Raya100% (1)
- Lad ADocument5 pagesLad AIdi Nagan RayaPas encore d'évaluation
- Jadwal Case Jadwal CodDocument2 pagesJadwal Case Jadwal CodAndy LoakPas encore d'évaluation
- Backgroun 1Document3 pagesBackgroun 1Idi Nagan RayaPas encore d'évaluation
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeD'EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeÉvaluation : 4 sur 5 étoiles4/5 (5794)
- The Little Book of Hygge: Danish Secrets to Happy LivingD'EverandThe Little Book of Hygge: Danish Secrets to Happy LivingÉvaluation : 3.5 sur 5 étoiles3.5/5 (400)
- Shoe Dog: A Memoir by the Creator of NikeD'EverandShoe Dog: A Memoir by the Creator of NikeÉvaluation : 4.5 sur 5 étoiles4.5/5 (537)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceD'EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceÉvaluation : 4 sur 5 étoiles4/5 (895)
- The Yellow House: A Memoir (2019 National Book Award Winner)D'EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Évaluation : 4 sur 5 étoiles4/5 (98)
- The Emperor of All Maladies: A Biography of CancerD'EverandThe Emperor of All Maladies: A Biography of CancerÉvaluation : 4.5 sur 5 étoiles4.5/5 (271)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryD'EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryÉvaluation : 3.5 sur 5 étoiles3.5/5 (231)
- Never Split the Difference: Negotiating As If Your Life Depended On ItD'EverandNever Split the Difference: Negotiating As If Your Life Depended On ItÉvaluation : 4.5 sur 5 étoiles4.5/5 (838)
- Grit: The Power of Passion and PerseveranceD'EverandGrit: The Power of Passion and PerseveranceÉvaluation : 4 sur 5 étoiles4/5 (588)
- On Fire: The (Burning) Case for a Green New DealD'EverandOn Fire: The (Burning) Case for a Green New DealÉvaluation : 4 sur 5 étoiles4/5 (73)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureD'EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureÉvaluation : 4.5 sur 5 étoiles4.5/5 (474)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaD'EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaÉvaluation : 4.5 sur 5 étoiles4.5/5 (266)
- The Unwinding: An Inner History of the New AmericaD'EverandThe Unwinding: An Inner History of the New AmericaÉvaluation : 4 sur 5 étoiles4/5 (45)
- Team of Rivals: The Political Genius of Abraham LincolnD'EverandTeam of Rivals: The Political Genius of Abraham LincolnÉvaluation : 4.5 sur 5 étoiles4.5/5 (234)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyD'EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyÉvaluation : 3.5 sur 5 étoiles3.5/5 (2259)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreD'EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreÉvaluation : 4 sur 5 étoiles4/5 (1090)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersD'EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersÉvaluation : 4.5 sur 5 étoiles4.5/5 (344)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)D'EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Évaluation : 4.5 sur 5 étoiles4.5/5 (121)
- Her Body and Other Parties: StoriesD'EverandHer Body and Other Parties: StoriesÉvaluation : 4 sur 5 étoiles4/5 (821)
- Periodontal Probing and Techniques JCDocument58 pagesPeriodontal Probing and Techniques JCAbhay TandonPas encore d'évaluation
- Impact of Digital Media On Sleep Pattern Disturbance in Medical and Nursing StudentsDocument10 pagesImpact of Digital Media On Sleep Pattern Disturbance in Medical and Nursing StudentsValarmathiPas encore d'évaluation
- (HSO) Medical Examination FormDocument1 page(HSO) Medical Examination FormKrizel LagundiPas encore d'évaluation
- Senile Cataract (Age-Related Cataract) : Practice Essentials, Background, PathophysiologyDocument6 pagesSenile Cataract (Age-Related Cataract) : Practice Essentials, Background, PathophysiologyadliahghaisaniPas encore d'évaluation
- Valvular Heart Disease 2Document46 pagesValvular Heart Disease 2Topea BogdanPas encore d'évaluation
- Life - Line ECMO Sell - Sheet ECMO FEB22 1 WebDocument2 pagesLife - Line ECMO Sell - Sheet ECMO FEB22 1 WebJavier Dario Cifuentes SandovalPas encore d'évaluation
- Heart BNHADocument13 pagesHeart BNHAX OloGyPas encore d'évaluation
- Jocelyn JanniDocument2 pagesJocelyn Janniapi-271982945Pas encore d'évaluation
- Patient Care Management Human Anatomy With Answer KeyDocument7 pagesPatient Care Management Human Anatomy With Answer KeyMarylyn Grass RootPas encore d'évaluation
- Bathing Your Baby: When Should Newborns Get Their First Bath?Document5 pagesBathing Your Baby: When Should Newborns Get Their First Bath?Glads D. Ferrer-JimlanoPas encore d'évaluation
- SOP For Cleaning of Ultrasound Probes in Trust Imaging Departments PDFDocument2 pagesSOP For Cleaning of Ultrasound Probes in Trust Imaging Departments PDFShinta Vivoy21Pas encore d'évaluation
- A Case Study of Wastewater Reclamation and Reuse in Hebei Province in China: Feasibility Analysis and Advanced Treatment DiscussionDocument2 pagesA Case Study of Wastewater Reclamation and Reuse in Hebei Province in China: Feasibility Analysis and Advanced Treatment DiscussionShalynn XiePas encore d'évaluation
- FAQ Mid Day MealsDocument7 pagesFAQ Mid Day Mealsvikramhegde87Pas encore d'évaluation
- List of Shelters in The Lower Mainland, June 2007Document2 pagesList of Shelters in The Lower Mainland, June 2007Union Gospel Mission100% (1)
- Sports NutritionDocument254 pagesSports NutritionrodriguezdiazPas encore d'évaluation
- Appendix 26 - SSG Prejoining Ship Check ListDocument1 pageAppendix 26 - SSG Prejoining Ship Check ListEliza's Soothing SoundsPas encore d'évaluation
- NCFAS TWB Trauma-Report (2015)Document19 pagesNCFAS TWB Trauma-Report (2015)Christian Olmos VarasPas encore d'évaluation
- Dapagli Ozin Treatment For Type 2 Diabetes: A Systematic Review and Meta-Analysis of Randomized Controlled TrialsDocument18 pagesDapagli Ozin Treatment For Type 2 Diabetes: A Systematic Review and Meta-Analysis of Randomized Controlled TrialsVictoria Maya ChyntiaPas encore d'évaluation
- Takaful MaybankDocument4 pagesTakaful MaybankSHAPas encore d'évaluation
- A Portfolio For Work Immersion Business Enterprise SimulationDocument17 pagesA Portfolio For Work Immersion Business Enterprise SimulationnicPas encore d'évaluation
- SSB201 Group Assigment 1 - Design ThinkingDocument3 pagesSSB201 Group Assigment 1 - Design ThinkingLe CuongPas encore d'évaluation
- GHGK SDocument48 pagesGHGK SAnonymous Syr2mlPas encore d'évaluation
- Application Letter Nurse AideDocument2 pagesApplication Letter Nurse AideOliver Ian ReposoPas encore d'évaluation
- Division of Blood Transfusion Services: Ministry of Health and Family WelfareDocument40 pagesDivision of Blood Transfusion Services: Ministry of Health and Family WelfareKirandragonPas encore d'évaluation
- Level 2 Unit 39 Assist in The Administration of MedicationDocument7 pagesLevel 2 Unit 39 Assist in The Administration of MedicationSzabolcs LehotaPas encore d'évaluation
- BBB Month 10 Workout LogDocument8 pagesBBB Month 10 Workout LogLi SaPas encore d'évaluation
- LUS HSE FM4 455 005.01 Audit Gap Analysis ChecklistDocument10 pagesLUS HSE FM4 455 005.01 Audit Gap Analysis ChecklistRichu PaliPas encore d'évaluation
- Aldinga Bay's Coastal Views April 2014Document48 pagesAldinga Bay's Coastal Views April 2014Aldinga BayPas encore d'évaluation
- Teenagers Eating HabitsDocument3 pagesTeenagers Eating HabitsMaria Jose Sanz0% (1)
- DizzinessDocument65 pagesDizzinessעידית בנימיןPas encore d'évaluation