Académique Documents
Professionnel Documents
Culture Documents
British Consensus Guidelines IVF For Adults Surgical Pt.
Transféré par
Sandip PatilTitre original
Copyright
Formats disponibles
Partager ce document
Partager ou intégrer le document
Avez-vous trouvé ce document utile ?
Ce contenu est-il inapproprié ?
Signaler ce documentDroits d'auteur :
Formats disponibles
British Consensus Guidelines IVF For Adults Surgical Pt.
Transféré par
Sandip PatilDroits d'auteur :
Formats disponibles
The Intensive Care Society 2009
Special reports
Summary of The British Consensus Guidelines on Intravenous Fluid Therapy for Adult Surgical Patients (GIFTASUP) for comment
J Powell-Tuck, P Gosling, D Lobo, S Allison, G Carlson, M Gore, A Lewington, R Pearse, M Mythen
Starting in October 2006 the Association of Surgeons of Great Britain and Ireland, the Society of Academic and Research Surgery, BAPEN Medical, the Intensive Care Society, the Association for Clinical Biochemistry and the Renal Association, nominated core members of a steering committee who came together to establish consensus for good peri-operative fluid prescribing. Concern arose regarding a high incidence of postoperative sodium and water overload, and evidence to suggest that preventing or treating this, by more accurate fluid therapy, would improve outcome. The following recommendations (28 in total) are extracted from the complete document which can be found on the ICS website (http://www.ics.ac.uk/downloads/2008112340_GIFTASUP%20FINAL_31-10-08.pdf ). Members of the steering committee used the definitions of the Oxford Centre for Evidence-based Medicine Levels of Evidence (May 2001) accessed from http://www.cebm.net/ index.aspx?o=1025 to assign levels of evidence, each of which, after debate, was accepted unanimously. However, debate is on-going and you are encouraged to have your say. Please communicate your thoughts on this published summary to the editor of JICS who will seek response from the authors.
Recommendation 1
Due to the risk of inducing hyperchloraemic acidosis in routine practice, when crystalloid resuscitation or replacement is indicated, balanced salt solutions, eg Ringers lactate/acetate or Hartmanns solution should replace 0.9% saline, except in cases of hypochloraemia, eg from vomiting or gastric drainage. Evidence level 1b*
elective surgery, clear non-particulate oral uids should not be withheld for more than two hours prior to the induction of anaesthesia. Evidence level 1a*
Recommendation 5
In the absence of disorders of gastric emptying or diabetes, preoperative administration of carbohydrate-rich beverages 2-3 h before induction of anaesthesia may improve patient well being and facilitate recovery from surgery. It should be considered in the routine preoperative preparation for elective surgery. Evidence level 2a*
Recommendation 2
Solutions such as 4% dextrose/0.18% saline and 5% dextrose are important sources of free water for maintenance, but should be used with caution as excessive amounts may cause dangerous hyponatraemia, especially in children and the elderly. These solutions are not appropriate for resuscitation or replacement therapy except in conditions of signicant free water decit, eg diabetes insipidus. Evidence level 1b*
Recommendation 6
Routine use of preoperative mechanical bowel preparation is not benecial and may complicate intra- and post-operative management of uid and electrolyte balance. Its use should therefore be avoided whenever possible. Evidence level 1a*
Recommendation 3
To meet maintenance requirements, adult patients should receive sodium 50-100 mmol/day, and potassium 40-80 mmol/day in 1.5-2.5 litres of water by the oral, enteral or parenteral route (or a combination of routes). Additional amounts should only be given to correct decit or continuing losses. Careful monitoring should be undertaken using clinical examination, uid balance charts, and regular weighing when possible. Evidence level 5*
Recommendation 7
Where mechanical bowel preparation is used, uid and electrolyte derangements commonly occur and should be corrected by simultaneous intravenous uid therapy with Hartmanns or Ringer-lactate/acetate type solutions. Evidence level 5*
Recommendation 8
Excessive losses from gastric aspiration/vomiting should be treated preoperatively with an appropriate crystalloid solution which includes an appropriate potassium supplement. Hypochloraemia is an indication for the use of 0.9% saline,
13
Preoperative fluid management
Recommendation 4
In patients without disorders of gastric emptying undergoing
JICS Volume 10, Number 1, January 2009
Special reports
with sufcient additions of potassium and care not to produce sodium overload. Losses from diarrhoea/ileostomy/small bowel stula/ileus/obstruction should be replaced volume for volume with Hartmanns or Ringer-lactate/acetate type solutions. Saline depletion, for example due to excessive diuretic exposure, is best managed with a balanced electrolyte solution such as Hartmanns. Evidence level 5* Evidence level 2a for Hartmanns versus 0.9% saline.*
until there is no further increase in stroke volume and improvement in the clinical parameters. Evidence level for ow-based measurements: 1b* For bolus infusion: Evidence level 1b* Volume to be given: Evidence level 5 (consensus)* For suitable colloid: Evidence level 1b*
Intraoperative fluid management
Recommendation 13
In patients undergoing some forms of orthopaedic and abdominal surgery, intraoperative treatment with intravenous uid to achieve an optimal value of stroke volume should be used where possible as this may reduce postoperative complication rates and duration of hospital stay. Orthopaedic surgery: Evidence level 1b* Abdominal surgery: Evidence level 1a*
Recommendation 9
In high-risk surgical patients preoperative treatment with intravenous uid and inotropes should be aimed at achieving predetermined goals for cardiac output and oxygen delivery as this may improve survival. Evidence level 1b*
Recommendation 10
Although currently logistically difcult in many centres, preoperative or operative hypovolaemia should be diagnosed by ow-based measurements wherever possible. The clinical context should also be taken into account as this will provide an important indication of whether hypovolaemia is possible or likely. When direct ow measurements are not possible, hypovolaemia will be diagnosed clinically on the basis of pulse, peripheral perfusion and capillary rell, venous (JVP/CVP) pressure and Glasgow Coma Scale together with acid-base and lactate measurements. A low urine output can be misleading and needs to be interpreted in the context of the patients cardiovascular parameters above. Diagnosis of hypovolaemia: Evidence level 1b*
Recommendation 14
Patients undergoing non-elective major abdominal or orthopaedic surgery should receive intravenous uid to achieve an optimal value of stroke volume during and for the rst eight hours after surgery. This may be supplemented by a low dose dopexamine infusion. Evidence level 1b*
Postoperative fluid, and nutritional management
Recommendation 15
Details of uids administered must be clearly recorded and easily accessible. Evidence level 5*
Recommendation 11
Hypovolaemia due predominantly to blood loss should be treated with either a balanced crystalloid solution or a suitable colloid until packed red cells are available. Hypovolaemia due to severe inammation such as infection, peritonitis, pancreatitis or burns should be treated with either a suitable colloid or a balanced crystalloid. In either clinical scenario, care must be taken to administer sufcient balanced crystalloid and colloid to normalise haemodynamic parameters and minimise overload. The ability of critically ill patients to excrete excess sodium and water is compromised, placing them at risk of severe interstitial oedema. The administration of large volumes of colloid without sufcient free water (eg 5% dextrose) may precipitate a hyperoncotic state. Suitable colloid or crystalloid for hypovolaemia: Evidence level 1b* Administration of sufcient water: Evidence level 5*
Recommendation 16
When patients leave theatre for the ward, high dependency unit (HDU) or intensive care unit (ICU) their volume status should be assessed. The volume and type of uids given perioperatively should be reviewed and compared with uid losses in theatre including urine and insensible losses.
Recommendation 17
In patients who are euvolaemic and haemodynamically stable, a return to oral uid administration should be achieved as soon as possible.
Recommendation 18
In patients requiring continuing IV maintenance uids, these should be sodium poor and of low enough volume until the patient has returned their sodium and uid balance over the perioperative period to zero. When this has been achieved the IV uid volume and content should be those required for daily maintenance and replacement of any on-going additional losses.
Recommendation 12
When the diagnosis of hypovolaemia is in doubt and the central venous pressure is not raised, the response to a bolus infusion of 200 mL of a suitable colloid or crystalloid should be tested. The response should be assessed using the patients cardiac output and stroke volume measured by ow-based technology if available. Alternatively, the clinical response may be monitored by measurement/estimation of the pulse, capillary rell, CVP and blood pressure before and 15 minutes after receiving the infusion. This procedure should be repeated
14
Recommendation 19
The haemodynamic and uid status of those patients who fail to excrete their perioperative sodium load, and especially whose urine sodium concentration is <20 mmol/L, should be reviewed. Evidence levels for recommendations 16,17,18 & 19: 1b*
Volume 10, Number 1, January 2009 JICS
Special reports
Recommendation 20
In high-risk patients undergoing major abdominal surgery, postoperative treatment with intravenous uid and low dose dopexamine should be considered, in order to achieve a predetermined value for systemic oxygen delivery, as this may reduce postoperative complication rates and duration of hospital stay. Evidence level 1b*
Recommendation 26
Balanced electrolyte solutions containing potassium can be used cautiously in patients with AKI closely monitored on HDU or ICU, in preference to 0.9% saline. If free water is required, 5% dextrose or dextrose-saline should be used. Patients developing hyperkalaemia or progressive AKI should be switched to non-potassium containing crystalloid solutions such as 0.45% saline or 4% dextrose/0.18% saline. Ringers lactate versus 0.9% saline for patients with AKI: Evidence level 1b*
Recommendation 21
In patients who are oedematous, hypovolaemia if present must be treated, followed by a gradual persistent negative sodium and water balance based on urine sodium concentration or excretion. Plasma potassium concentration should be monitored and where necessary potassium intake adjusted. Evidence level 1b*
Recommendation 27
In patients with AKI, uid balance must be closely observed and uid overload avoided. In patients who show signs of refractory uid overload, renal replacement therapy should be considered early to mobilise interstitial oedema and correct extracellular electrolyte and acid base abnormalities. Evidence level 5*
Recommendation 22
Nutritionally depleted patients need cautious refeeding orally, enterally or parenterally, with feeds supplemented in potassium, phosphate and thiamine. Generally, and particularly if oedema is present, these feeds should be reduced in water and sodium. Though refeeding syndrome is a risk, improved nutrition will help to restore normal partitioning of sodium, potassium and water between intraand extra-cellular spaces. Evidence level 5*
Recommendation 28
Patients at risk of developing AKI secondary to rhabdomyolysis must receive aggressive uid resuscitation with an isotonic crystalloid solution to correct hypovolaemia. There is insufcient evidence to recommend the specic composition of the crystalloid. Evidence level 5*
*
Recommendation 23
Surgical patients should be nutritionally screened, and NICE guidelines for perioperative nutritional support adhered to. Care should be taken to mitigate risks of the refeeding syndrome. Evidence level 5*
For the complete document PDF including background, discussion and supporting evidence citations see: the ICS website:http://www.ics.ac.uk/downloads/2008112340_GIFTAS UP%20FINAL_31-10-08.pdf. Jeremy Powell-Tuck (Chair), Simon P Allison British
Association of Parenteral and Enteral Nutrition Medical j.powelltuck@btinternet.com
Fluid management in acute kidney injury (AKI)
Recommendation 24
Based on current evidence, higher molecular weight hydroxyethyl starch (hetastarch and pentastarch MW >200 kDa) should be avoided in patients with severe sepsis due to an increased risk of AKI. Evidence level 1b
Peter Gosling The Association for Clinical Biochemistry Dileep N Lobo BAPEN Medical and the Association of
Surgeons of Great Britain and Ireland and Society of Academic and Research Surgeons
Recommendation 25
Higher molecular weight hydroxyethyl starch (hetastarch and pentastarch MW >200 kDa) should be avoided in brain-dead kidney donors due to reports of osmotic nephrosis-like lesions. Evidence level 2b
Gordon L Carlson, Marcus Gore The Association of Surgeons of Great Britain and Ireland and Society of Academic and Research Surgeons Andrew J Lewington The Renal Association Rupert M Pearse, Monty G Mythen On behalf of the
Intensive Care Society
JICS Volume 10, Number 1, January 2009
15
Vous aimerez peut-être aussi
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)D'EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Évaluation : 4.5 sur 5 étoiles4.5/5 (121)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryD'EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryÉvaluation : 3.5 sur 5 étoiles3.5/5 (231)
- Grit: The Power of Passion and PerseveranceD'EverandGrit: The Power of Passion and PerseveranceÉvaluation : 4 sur 5 étoiles4/5 (588)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaD'EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaÉvaluation : 4.5 sur 5 étoiles4.5/5 (266)
- Never Split the Difference: Negotiating As If Your Life Depended On ItD'EverandNever Split the Difference: Negotiating As If Your Life Depended On ItÉvaluation : 4.5 sur 5 étoiles4.5/5 (838)
- The Emperor of All Maladies: A Biography of CancerD'EverandThe Emperor of All Maladies: A Biography of CancerÉvaluation : 4.5 sur 5 étoiles4.5/5 (271)
- The Little Book of Hygge: Danish Secrets to Happy LivingD'EverandThe Little Book of Hygge: Danish Secrets to Happy LivingÉvaluation : 3.5 sur 5 étoiles3.5/5 (400)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeD'EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeÉvaluation : 4 sur 5 étoiles4/5 (5794)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyD'EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyÉvaluation : 3.5 sur 5 étoiles3.5/5 (2259)
- Shoe Dog: A Memoir by the Creator of NikeD'EverandShoe Dog: A Memoir by the Creator of NikeÉvaluation : 4.5 sur 5 étoiles4.5/5 (537)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreD'EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreÉvaluation : 4 sur 5 étoiles4/5 (1090)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersD'EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersÉvaluation : 4.5 sur 5 étoiles4.5/5 (344)
- Team of Rivals: The Political Genius of Abraham LincolnD'EverandTeam of Rivals: The Political Genius of Abraham LincolnÉvaluation : 4.5 sur 5 étoiles4.5/5 (234)
- Her Body and Other Parties: StoriesD'EverandHer Body and Other Parties: StoriesÉvaluation : 4 sur 5 étoiles4/5 (821)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceD'EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceÉvaluation : 4 sur 5 étoiles4/5 (895)
- The Unwinding: An Inner History of the New AmericaD'EverandThe Unwinding: An Inner History of the New AmericaÉvaluation : 4 sur 5 étoiles4/5 (45)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureD'EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureÉvaluation : 4.5 sur 5 étoiles4.5/5 (474)
- On Fire: The (Burning) Case for a Green New DealD'EverandOn Fire: The (Burning) Case for a Green New DealÉvaluation : 4 sur 5 étoiles4/5 (74)
- Provisional Restoration Options in Implant DentistryDocument8 pagesProvisional Restoration Options in Implant Dentistrydevendra chhonkarPas encore d'évaluation
- Pain ManagementDocument175 pagesPain ManagementGusni FitriPas encore d'évaluation
- Downloads - 23032018 - Format of Affidavit and Indemnity Bond For Renewal of RegistrationDocument4 pagesDownloads - 23032018 - Format of Affidavit and Indemnity Bond For Renewal of RegistrationSandip Patil50% (8)
- The Yellow House: A Memoir (2019 National Book Award Winner)D'EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Évaluation : 4 sur 5 étoiles4/5 (98)
- Product Review EllaOne - Ulipristal AcetateDocument7 pagesProduct Review EllaOne - Ulipristal AcetateAnonymous SDUIPeqXPas encore d'évaluation
- Substance UseDocument3 pagesSubstance UseAlbert SamantePas encore d'évaluation
- IMNCIDocument31 pagesIMNCIJaya Prabha100% (2)
- 2016 Revised Standards For Clinical Dental Hygiene PracticeDocument16 pages2016 Revised Standards For Clinical Dental Hygiene PracticeElvira PurnamasariPas encore d'évaluation
- Administration of Total Parenteral Nutrition (TPN) - Adults and Children (Not NICU)Document15 pagesAdministration of Total Parenteral Nutrition (TPN) - Adults and Children (Not NICU)Giri SivaPas encore d'évaluation
- Bhakoot Dosha PDFDocument4 pagesBhakoot Dosha PDFSandip PatilPas encore d'évaluation
- Participants Manual ImnciDocument228 pagesParticipants Manual Imncishikhar100% (1)
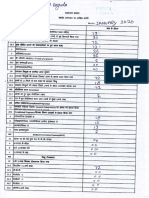
- Form A Monthly ReportDocument1 pageForm A Monthly ReportSandip PatilPas encore d'évaluation
- Nov 19bDocument1 pageNov 19bSandip PatilPas encore d'évaluation
- January 20aDocument1 pageJanuary 20aSandip PatilPas encore d'évaluation
- Obstetrical Ultrasound Report: Fetal Anatomy and StructuresDocument2 pagesObstetrical Ultrasound Report: Fetal Anatomy and StructuresSandip PatilPas encore d'évaluation
- Obstetrical Ultrasound Report: Fetal Anatomy and StructuresDocument1 pageObstetrical Ultrasound Report: Fetal Anatomy and StructuresSandip PatilPas encore d'évaluation
- Ceu Guidance Intrauterine ContraceptionDocument60 pagesCeu Guidance Intrauterine ContraceptionSandip PatilPas encore d'évaluation
- Harshada Sandip Patil 12/04/1992 OBC: Application For NCLDocument2 pagesHarshada Sandip Patil 12/04/1992 OBC: Application For NCLSandip PatilPas encore d'évaluation
- External Research ProgrammesDocument3 pagesExternal Research ProgrammesSandip PatilPas encore d'évaluation
- Village Health Nutrition Days - GuidelinesDocument28 pagesVillage Health Nutrition Days - GuidelinesSandip PatilPas encore d'évaluation
- Progestogen-Only Injectable ContraceptionDocument40 pagesProgestogen-Only Injectable ContraceptionMohamed OmerPas encore d'évaluation
- GanaDosha PDFDocument4 pagesGanaDosha PDFSandip PatilPas encore d'évaluation
- 2 Syllabus GPDocument1 page2 Syllabus GPAzhagiya SingamPas encore d'évaluation
- CEU QlairaDocument4 pagesCEU QlairaNadira RahmanPas encore d'évaluation
- General Science PDFDocument8 pagesGeneral Science PDFmrpatil186Pas encore d'évaluation
- Csir Net - General Aptitude (Part-A) : Sample TheoryDocument7 pagesCsir Net - General Aptitude (Part-A) : Sample TheorySandip PatilPas encore d'évaluation
- Letter of ExperienceDocument1 pageLetter of ExperienceSandip PatilPas encore d'évaluation
- (Family Medicine) : Dr. Sandip Ganesh PatilDocument38 pages(Family Medicine) : Dr. Sandip Ganesh PatilSandip PatilPas encore d'évaluation
- General Science PDFDocument8 pagesGeneral Science PDFmrpatil186Pas encore d'évaluation
- Curriculum Vitae 2Document3 pagesCurriculum Vitae 2Sandip PatilPas encore d'évaluation
- CEU QlairaDocument4 pagesCEU QlairaNadira RahmanPas encore d'évaluation
- Geeta: Birth Date: 12 Apr 1992 Birth Place: KalyanDocument7 pagesGeeta: Birth Date: 12 Apr 1992 Birth Place: KalyanSandip PatilPas encore d'évaluation
- Syphilis Doc Low-Res 5th JanDocument56 pagesSyphilis Doc Low-Res 5th JanSandip PatilPas encore d'évaluation
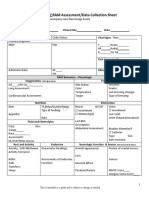
- Proforma For Iphs Facility Survey of SCDocument6 pagesProforma For Iphs Facility Survey of SCSandip PatilPas encore d'évaluation
- 5 X 5 Rmnch+aDocument2 pages5 X 5 Rmnch+aManish Chandra Prabhakar0% (1)
- Cec Ceu Statement Esmya Interactions Nov 2012Document3 pagesCec Ceu Statement Esmya Interactions Nov 2012Sandip PatilPas encore d'évaluation
- Annexure 10 Guideline On Consumption of WIFS TabletsDocument1 pageAnnexure 10 Guideline On Consumption of WIFS TabletsSandip PatilPas encore d'évaluation
- ARTIKEL9 - Jurnal Elective Birth in Twin PregnancyDocument11 pagesARTIKEL9 - Jurnal Elective Birth in Twin PregnancyFarid NurdiansyahPas encore d'évaluation
- Raw Milk For The HealthDocument7 pagesRaw Milk For The HealthviannikkkyPas encore d'évaluation
- AnencephalyDocument11 pagesAnencephalyAnironOrionPas encore d'évaluation
- Standar Keselamatan PasienDocument30 pagesStandar Keselamatan PasienraraPas encore d'évaluation
- Preliminary: Noor Ariyani Rokhmah, AnggorowatiDocument2 pagesPreliminary: Noor Ariyani Rokhmah, AnggorowatiIta NovitaPas encore d'évaluation
- Saba University: School of MedicineDocument32 pagesSaba University: School of MedicineGus LionsPas encore d'évaluation
- Surveillance Guide For Vaccine-Preventable Diseases in The WHO South-East Asia RegionDocument28 pagesSurveillance Guide For Vaccine-Preventable Diseases in The WHO South-East Asia RegionDebPas encore d'évaluation
- Novartis Vigamox-Product (API+excipient)Document15 pagesNovartis Vigamox-Product (API+excipient)auliana khusniatiPas encore d'évaluation
- Croup Diagnosis and Management 2018Document6 pagesCroup Diagnosis and Management 2018Jose Fernando DiezPas encore d'évaluation
- Weekly Home Learning Plan: Grade 8 - Quarter 2. Week 7Document3 pagesWeekly Home Learning Plan: Grade 8 - Quarter 2. Week 7Danmer Jude TorresPas encore d'évaluation
- Short Form Plan - August 2013Document3 pagesShort Form Plan - August 2013Anonymous s0QUn5CtHUPas encore d'évaluation
- Comparison of Nursing and Medical DiagnosesDocument14 pagesComparison of Nursing and Medical DiagnosesNeko NekoPas encore d'évaluation
- NCM 107Document3 pagesNCM 107Sunshine BocoPas encore d'évaluation
- A Case of Aspartate Aminotransferase MacroenzymeDocument3 pagesA Case of Aspartate Aminotransferase MacroenzymeOlfiany Laurenzia PongohPas encore d'évaluation
- Akut AbdomenDocument38 pagesAkut AbdomenAprianPas encore d'évaluation
- Welcome To Trucare Trust A Premium Alcohol & Drug Rehab CentreDocument5 pagesWelcome To Trucare Trust A Premium Alcohol & Drug Rehab CentreTrucare TrustPas encore d'évaluation
- Case PresentationDocument11 pagesCase PresentationHira Rafique100% (1)
- Pharmacology: A Career inDocument2 pagesPharmacology: A Career insnikt7863443Pas encore d'évaluation
- Philippine Institute of Traditional and Alternative Health Care (PITAHC) Board of Trustees Government RepresentativesDocument3 pagesPhilippine Institute of Traditional and Alternative Health Care (PITAHC) Board of Trustees Government Representativesallen reyesPas encore d'évaluation
- Understanding Immunomodulatory DrugsDocument4 pagesUnderstanding Immunomodulatory DrugsMark Russel Sean LealPas encore d'évaluation
- Pcod 0343021025 PDFDocument5 pagesPcod 0343021025 PDFArun AchalamPas encore d'évaluation
- UwomjDocument88 pagesUwomjjeffaguilarPas encore d'évaluation
- Biological Properties of Lemongrass An OverviewDocument1 pageBiological Properties of Lemongrass An OverviewLilia RotariPas encore d'évaluation
- Baird 2017Document20 pagesBaird 2017Jhasmyn MartinezPas encore d'évaluation