Académique Documents
Professionnel Documents
Culture Documents
391 Full PDF
Transféré par
Andre Eka Putra PrakosaTitre original
Copyright
Formats disponibles
Partager ce document
Partager ou intégrer le document
Avez-vous trouvé ce document utile ?
Ce contenu est-il inapproprié ?
Signaler ce documentDroits d'auteur :
Formats disponibles
391 Full PDF
Transféré par
Andre Eka Putra PrakosaDroits d'auteur :
Formats disponibles
The British Journal of Psychiatry (2013) 202, 391393. doi: 10.1192/bjp.bp.112.
123943
Editorial
Multimorbidity and mental health: can psychiatry rise to the challenge?
Julie Langan, Stewart W. Mercer and Daniel J. Smith
Summary Multimorbidity the co-occurrence of two or more long-term conditions in an individual is highly relevant to psychiatry. Changes to training and a more integrated model of psychiatric and physical healthcare are needed in the future if we are to improve the long-term health of our patients. Declaration of interest None.
Julie Langan (pictured) is a clinical lecturer in psychiatry at the University of Glasgow; her primary research interest is the interface between psychiatric and physical health disorders. Stewart Mercer is a professor of primary care research at the University of Glasgow and national lead for research into multimorbidity within primary care in Scotland. Daniel Smith is a reader and an honorary consultant psychiatrist at the University of Glasgow.
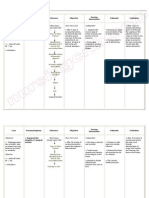
The scale of the problem and the impact of social deprivation Multimorbidity was previously considered a problem for elderly populations but recent work has found this not to be the case. A study of almost 1.8 million people within 314 primary care practices in Scotland found that more people with multimorbidity were aged below 65 than were aged above 65 and similar findings have been observed internationally.6 Socioeconomic deprivation has a strong and consistent association with multimorbidity. In the Scottish primary care study, prevalence rates of physical and mental health comorbidity were almost twice as high in the most deprived areas (11%) compared with the most affluent areas (5.9%) (Fig. 1).6 Furthermore, the onset of multimorbidity occurred up to 15 years earlier in the most deprived areas compared with the most affluent areas. This socioeconomic gradient in the association between physical and mental health will come as no surprise to general practitioners (GPs) and psychiatrists working in deprived areas of the UK an issue highlighted in the General Practitioners at the Deep End project (involving 100 general practices in the most deprived populations in Scotland),7 where a common theme was the difficulty in adequately addressing a multitude of interrelated medical, psychiatric, substance misuse and social problems in the context of limited time, limited resources and low availability of high-quality services such clinical psychology. There must be real concerns that multimorbid psychiatric patients (concentrated in more deprived areas) will not be well served by changes resulting from the new Health and Social Care Bill in England. Anxieties about the likely impact of these National Health Service (NHS) reforms on patients with physical and mental health problems are a prominent feature of the recent Kings Fund report, which highlights that the interaction between comorbidities and deprivation makes a significant contribution to generating and maintaining inequalities.3 This report urges clinical commissioning groups to prioritise the integration of physical and mental healthcare to improve both patient outcomes and longer-term productivity. Managing multimorbidity in mental health through more integrated care The care of patients with multimorbidity can be complex and may involve multiple secondary care specialists who separately liaise with the primary care team. The communication challenges this
Multimorbidity is usually defined as two or more long-term conditions co-occurring in an individual. Although the terms multimorbidity and comorbidity are often used interchangeably, comorbidity implies an index condition associated with one or more other conditions (and is thus often defined by specialists), whereas multimorbidity does not imply that any one condition is more important than another. Multimorbidity is common and is often the norm rather than the exception in those with long-term conditions.1 It is a significant and growing issue for patients, health professionals and healthcare systems worldwide. Although most individuals with long-term conditions have more than one,2 healthcare systems throughout the world are predominately organised around a single-disease approach. Multimorbidity in mental health has to date been relatively underresearched and data for how best to address the problem are limited. Here we summarise what is known about the extent of multimorbidity in psychiatric disorders and consider ways in which psychiatry might respond to the challenge.
Long-term physical health morbidity and mental illness The fact that life expectancy for those with major mental illness is 20 years less for men and 15 years less for women is a stark statistic of health inequality. The close relationship between physical and mental health outcomes has long been recognised and several recent high-profile reports have highlighted a need for much greater integration. No Health without Mental Health,2 Long-term Conditions and Mental Health,3 How Mental Illness Loses out in the NHS4 and the recent Schizophrenia Commission report The Abandoned Illness5 are a few examples. A common thread is that long-term physical conditions and mental health problems very often co-occur, act synergistically and have negative effects on levels of disability, with longer hospital stays, increased cost and increased mortality.
391
Langan et al
60 Patients with mental health disorder, %
40
Socioeconomic status 10 9 8 7 6 5 4 . 3 2 1 .
.
How should psychiatry respond?
. . . . . .
20
. . .
0 0
55
Physical health disorders, n
Fig. 1 Physical and mental health comorbidity and the association with socioeconomic status.
On the socioeconomic status scale, 1 is the most affluent and 10 the most deprived. Reproduced with permission from Barnett et al.6
presents can lead to fragmented and inconsistent care, particularly for patients with major mental illness.3 These problems are compounded by the reality that patients with mental illness and comorbid physical problems often do not receive the same level of assessment and treatment for their physical problems as patients without mental illness.8 There are likely to be opportunities in the future to improve communication between primary and secondary care, for example, by improved linking of electronic databases used for chronic disease monitoring (such as diabetes) with secondary care psychiatric databases, with a view to better sharing of information on physical health. It seems clear that we need models of care that allow a much more integrated approach to diagnosing, monitoring and treating multimorbidity in patients with mental illness, particularly in areas of social and economic deprivation. Greater integration of psychiatric services with primary care and with specialist medical services is clearly vital but evidence on how best to achieve this is limited. The World Health Organization (WHO) defines integrated care as the management and delivery of healthcare along a continuum of preventive and curative services, according to patient needs over time and across different levels of the health system. Integrated care can be cost-effective, patient-centred, equitable and locally-owned but there is also a risk that a broad continuum of integration threatens existing high-quality services. Although there is some evidence that integrated care models which include chronic disease management approaches, case management and enhanced multidisciplinary teamwork may have long-term benefits in treating multimorbidity,9 there has been no systematic evaluation of these interventions in multimorbid patients with severe mental illnesses such as schizophrenia. Collaborative care models for the management of depression involve a mental health specialist, a primary care practitioner and a case manager with, in general, good outcomes10 this tripartite model may be a useful approach for treating multimorbid mental illness but it has not yet been formally evaluated. Another potential avenue for improving the integration of physical and mental healthcare is to build on the success of liaison psychiatry services that at present are almost exclusively hospital based. One of the key recommendations from the NHS Confederations recent briefing report Liaison Psychiatry The Way Ahead is that liaison psychiatry services could be developed further to provide community-based services and training.11
Policy makers in the UK and internationally need to plan reorganisations of both mental health and physical health services in ways that can equitably address the health inequalities noted earlier. Careful attention needs to be given to how best to get mental health specialists and GPs working together effectively and whether this multimorbidity work can be incentivised, particularly in areas of social deprivation. The Royal College of General Practitioners and the Royal College of Psychiatrists have started to work together on this issue for example, with the recent publication of the Positive Cardiometabolic Health Resource (Lester UK Adaptation)12 but this is an area in need of much further development. Arguably the most pressing need is to develop interventions to reduce the extraordinarily high rates of smoking in major mental illness. In the longer term, addressing multimorbidity will have major implications for the way in which all clinicians involved with mental health as well as GPs are trained and work. The current disconnection between secondary care psychiatric services (which are focused on mental health outcomes) and primary care services, which are often not fully engaged in the physical healthcare of their patients with mental illness, needs to be addressed as a matter of urgency. In the short- to medium-term, psychiatrists should seek to improve the degree to which they engage with the physical health needs of their patients. This could obviously take many forms, including better assessment and monitoring, closer liaison with GPs, supporting and delivering exercise, weight management and smoking cessation programmes, improving antipsychotic prescribing skills and recognising the opportunities within early intervention services for addressing the long-term physical health needs of young people with major mental illness.13 Longer-term, the medical academic community should come together to design and test creative new interventions specifically for multimorbidity in mental health in order to gather the evidence for new innovations in service organisation and delivery. These interventions should be at several levels, from healthcare system changes and large-scale integrated or collaborative care models, to focused interventions in high-risk groups, such as young adults with first-episode psychosis living in deprived communities.
Conclusions Multimorbidity in mental health may be a relatively new concept for psychiatry but it is likely to become increasingly important in the future. This issue may be particularly acute for psychiatric practice in the UK, given the current recruitment crisis and the biggest health service reforms for a generation, both of which risk further inequality and disadvantage for patients with mental illness who have complex needs. Given the central role of mental illness within the multimorbidity continuum, it is our contention that psychiatrists, GPs, researchers and policy makers urgently need to discuss how best to develop and evaluate services that will improve physical, psychological and social outcomes for our patients.
Julie Langan, MRCP, MRCPsych, Stewart W. Mercer, PhD, FRCGP, Daniel J. Smith, MD, MRCPsych, Institute of Health and Wellbeing, University of Glasgow, UK. Correspondence : Daniel J. Smith, Institute of Health and Wellbeing, University of Glasgow, Mental Health and Wellbeing, Gartnavel Royal Hospital, 1055 Great Western Road, Glasgow G12 0XH, UK. Email: daniel.smith@glasgow.ac.uk First received 19 Nov 2012, accepted 4 Dec 2012
392
Multimorbidity and mental health
References
1 van den Akker M, Buntinx F, Metsemakers JFM, Roos S, Knotterus JA. Multimorbidity in general practice: prevalence, incidence, and determnants of co-occurring chronic and recurrent diseases. J Clin Epidemiol 1998; 51: 36775. Department of Health. No Health without Mental Health: A CrossGovernment Mental Health Outcomes Strategy for People of All Ages. Department of Health, 2011. The Kings Fund. Long-Term Conditions and Mental Health: The Cost of Co-Morbidities. The Kings Fund, 2012. The Centre for Economic Performances Mental Health Policy Group. How Mental Illness Loses out on the NHS. London School of Economics and Political Science, 2012. Schizophrenia Commission. The Adandoned Illness. Schizophrenia Commission Report. Rethink Mental Illness, 2012. Barnett K, Mercer SW, Norbury M, Watt G, Wyke S, Guthrie B. Epidemiology of multimorbidity and implications for health care, research, and medical education: a cross-sectional study. Lancet 2012; 380: 3743. Watt G. GPs at the deep end. Br J Gen Pract 2011; 61: 667.
8 Thornicroft G, Brohan E, Rose D, Sartorius N, Leese M. Global pattern of experienced and anticipated discrimination against people with schizophrenia: a cross-sectional survey. Lancet 2009; 373: 40815. 9 Smith SM, Soubhi H, Fortin M, Hudon C, ODowd T. Managing patients with multimorbidity: systematic review of interventions in primary care and community settings. BMJ 2012; 345: e5205. 10 Gilbody S, Bower P, Fletcher J, Richards D, Sutton AJ. Collaborative care for depression: a cumulative meta-analysis and review of longer-term outcomes. Arch Intern Med 2006; 166: 231421. 11 NHS Confederation Mental Health Network. Liaison Psychiatry The Way Ahead. Briefing 249. NHS Confederation, 2012 (http://www.nhsconfed.org/ Publications/Documents/Liaison-psychiatry-the-way-ahead.pdf). 12 Lester H, Shiers DE, Rafi I, Cooper SJ, Holt RIG. Positive Cardiometabolic Health Resource: An Intervention Framework for Patients with Psychosis on Antipsychotic Medication. Royal College of Psychiatrists, 2012 (http://www.rcpsych.ac.uk/quality/nationalclinicalaudits/schizophrenia/ nationalschizophreniaaudit/nasresources.aspx). 13 Bailey S, Gerada C, Lester H, Shiers D. The cardiovascular health of young people with severe mental illness: addressing an epidemic within an epidemic. Psychiatrist 2012; 36: 3758.
3 4
5 6
words
100
Menstrual psychosis
Ian Brockington Menstrual psychosis is a periodic illness, in which stupor, mania, confusion or other psychotic symptoms recur in rhythm with the menses. It resembles puerperal psychosis, at 1/10th its frequency. Nevertheless, psychiatrists will occasionally encounter cases, especially if they work with postpartum or bipolar women. Over 80 well-evidenced cases have been published. Occurrence before the menarche, during amenorrhoeic phases and without a pituitary, as well as after childbirth, indicate a hypothalamic origin. Action on Menstrual Psychosis, an international link between sufferers, has members from UK, USA, Australia and New Zealand. The aim is to establish national referral centres and collaborative research. Interested readers are referred to Menstrual Psychosis and the Catamenial Process. Eyry Press, 2008.
The British Journal of Psychiatry (2013) 202, 393. doi: 10.1192/bjp.bp.112.108563
393
Vous aimerez peut-être aussi
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)D'EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Évaluation : 4.5 sur 5 étoiles4.5/5 (121)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryD'EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryÉvaluation : 3.5 sur 5 étoiles3.5/5 (231)
- Grit: The Power of Passion and PerseveranceD'EverandGrit: The Power of Passion and PerseveranceÉvaluation : 4 sur 5 étoiles4/5 (588)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaD'EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaÉvaluation : 4.5 sur 5 étoiles4.5/5 (266)
- Never Split the Difference: Negotiating As If Your Life Depended On ItD'EverandNever Split the Difference: Negotiating As If Your Life Depended On ItÉvaluation : 4.5 sur 5 étoiles4.5/5 (838)
- The Little Book of Hygge: Danish Secrets to Happy LivingD'EverandThe Little Book of Hygge: Danish Secrets to Happy LivingÉvaluation : 3.5 sur 5 étoiles3.5/5 (400)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyD'EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyÉvaluation : 3.5 sur 5 étoiles3.5/5 (2259)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeD'EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeÉvaluation : 4 sur 5 étoiles4/5 (5795)
- Her Body and Other Parties: StoriesD'EverandHer Body and Other Parties: StoriesÉvaluation : 4 sur 5 étoiles4/5 (821)
- The Emperor of All Maladies: A Biography of CancerD'EverandThe Emperor of All Maladies: A Biography of CancerÉvaluation : 4.5 sur 5 étoiles4.5/5 (271)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreD'EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreÉvaluation : 4 sur 5 étoiles4/5 (1091)
- Shoe Dog: A Memoir by the Creator of NikeD'EverandShoe Dog: A Memoir by the Creator of NikeÉvaluation : 4.5 sur 5 étoiles4.5/5 (537)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceD'EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceÉvaluation : 4 sur 5 étoiles4/5 (895)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureD'EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureÉvaluation : 4.5 sur 5 étoiles4.5/5 (474)
- Team of Rivals: The Political Genius of Abraham LincolnD'EverandTeam of Rivals: The Political Genius of Abraham LincolnÉvaluation : 4.5 sur 5 étoiles4.5/5 (234)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersD'EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersÉvaluation : 4.5 sur 5 étoiles4.5/5 (345)
- Wiltshire HRT Guidance 2014Document5 pagesWiltshire HRT Guidance 2014andrewmmwilmot100% (1)
- On Fire: The (Burning) Case for a Green New DealD'EverandOn Fire: The (Burning) Case for a Green New DealÉvaluation : 4 sur 5 étoiles4/5 (74)
- The Yellow House: A Memoir (2019 National Book Award Winner)D'EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Évaluation : 4 sur 5 étoiles4/5 (98)
- The Unwinding: An Inner History of the New AmericaD'EverandThe Unwinding: An Inner History of the New AmericaÉvaluation : 4 sur 5 étoiles4/5 (45)
- Physics, Physiology and Medicine of Diving PDFDocument30 pagesPhysics, Physiology and Medicine of Diving PDFAndre Eka Putra Prakosa100% (1)
- Physics, Physiology and Medicine of Diving PDFDocument30 pagesPhysics, Physiology and Medicine of Diving PDFAndre Eka Putra Prakosa100% (1)
- Nursing Care Plan Impaire Physical MobilityDocument2 pagesNursing Care Plan Impaire Physical Mobilityderic90% (10)
- 5 - Population and SampleDocument13 pages5 - Population and SampleAndre Eka Putra Prakosa100% (1)
- Implant FailureDocument6 pagesImplant FailureNajeeb UllahPas encore d'évaluation
- NOAA Diving ManualDocument520 pagesNOAA Diving Manualdasalomon100% (5)
- Asessment Nursing Diagnosis Background Knowledge Planning Intervention Rationale EvaluationDocument3 pagesAsessment Nursing Diagnosis Background Knowledge Planning Intervention Rationale EvaluationHikari 光 Shidou50% (2)
- Health Talk On Exclusive BreastfeedingDocument14 pagesHealth Talk On Exclusive BreastfeedingPiyush DuttaPas encore d'évaluation
- A Review of Nebivolol Pharmacology and Clinical Evidence: Key PointsDocument23 pagesA Review of Nebivolol Pharmacology and Clinical Evidence: Key PointsAndre Eka Putra PrakosaPas encore d'évaluation
- The Use of Vasopressor and Inotropes in The Emergency Departement For The Treatment of ShockDocument36 pagesThe Use of Vasopressor and Inotropes in The Emergency Departement For The Treatment of ShockAndre Eka Putra PrakosaPas encore d'évaluation
- Daftar Pustaka Tumor ParotisDocument2 pagesDaftar Pustaka Tumor ParotisAndre Eka Putra PrakosaPas encore d'évaluation
- Parotid MassDocument9 pagesParotid MassAndre Eka Putra PrakosaPas encore d'évaluation
- DR - Sapta FarmasiDocument1 pageDR - Sapta FarmasiAndre Eka Putra PrakosaPas encore d'évaluation
- Nitrox Physiology OHP PDFDocument25 pagesNitrox Physiology OHP PDFAndre Eka Putra PrakosaPas encore d'évaluation
- Canmedaj00472 0105Document3 pagesCanmedaj00472 0105Andre Eka Putra PrakosaPas encore d'évaluation
- Brain Kidney Interactions in Post Traumatic Brain Death PDFDocument6 pagesBrain Kidney Interactions in Post Traumatic Brain Death PDFspeed_09Pas encore d'évaluation
- List of Clinical Studies For You To Take To Your Doctor 1Document34 pagesList of Clinical Studies For You To Take To Your Doctor 1girithaPas encore d'évaluation
- MVDocument14 pagesMVLeonardo VirginioPas encore d'évaluation
- Script For Direct Examination Of: Doctor For The AccusedDocument3 pagesScript For Direct Examination Of: Doctor For The AccusedJohn Levi P. CalinawanPas encore d'évaluation
- RC Holy Spirit - Interact Club of Holy SpiritDocument3 pagesRC Holy Spirit - Interact Club of Holy Spiritrc_holyspiritPas encore d'évaluation
- Rome Self Help QuestionnaireDocument2 pagesRome Self Help QuestionnaireebookdrPas encore d'évaluation
- The Nursing Assistant and The Care TeamDocument13 pagesThe Nursing Assistant and The Care TeamShannie PadillaPas encore d'évaluation
- PostnatalDocument99 pagesPostnatalPlain GerlPas encore d'évaluation
- 1amnktgeftag13rbb5srrbnvDocument2 pages1amnktgeftag13rbb5srrbnvwasu sheebuPas encore d'évaluation
- Gastrointestinal DiseasesDocument9 pagesGastrointestinal DiseasesJeraLdine HÜfanoPas encore d'évaluation
- 10 Import Risk Analysis: 10.1 PurposeDocument5 pages10 Import Risk Analysis: 10.1 PurposeformanitePas encore d'évaluation
- Ortho Problem Based QuestionsDocument6 pagesOrtho Problem Based QuestionsPuja Guni100% (1)
- THESIS SYNOPSIS - 2021 Government Medical College & HospitalDocument8 pagesTHESIS SYNOPSIS - 2021 Government Medical College & HospitalShreya GargPas encore d'évaluation
- Multiple Choice QuestionsDocument10 pagesMultiple Choice QuestionsDr-Sanjay SinghaniaPas encore d'évaluation
- Priority Nursing Diagnosis NutritionDocument5 pagesPriority Nursing Diagnosis NutritionAnonymous h2EnKyDbPas encore d'évaluation
- Temozolomide Adjuvant NHSDocument5 pagesTemozolomide Adjuvant NHSSyed Touseef AhmedPas encore d'évaluation
- Growth DisturbancesDocument10 pagesGrowth DisturbancesSulthana Rasiya NPas encore d'évaluation
- Pregnancy (Y)Document64 pagesPregnancy (Y)Mohamed AbbasPas encore d'évaluation
- Jurnal Fisioterapi DadaDocument11 pagesJurnal Fisioterapi DadaRosvita IndriawatiPas encore d'évaluation
- Muhs 2013 Winter Time TableDocument70 pagesMuhs 2013 Winter Time Tablepappu6600Pas encore d'évaluation
- 1907 CollegewiseallottmentsofpgmedicalafterseconndphasecounsellingDocument29 pages1907 CollegewiseallottmentsofpgmedicalafterseconndphasecounsellingkrishnaPas encore d'évaluation
- Slow Auditory Evoked Potentials (1 InterligneDocument8 pagesSlow Auditory Evoked Potentials (1 Interligner.boniver524Pas encore d'évaluation
- 2017 10Document200 pages2017 10Eduardo RomeroPas encore d'évaluation
- World Malaria Report: Years of Global Progress & ChallengesDocument300 pagesWorld Malaria Report: Years of Global Progress & ChallengesMOBA LQPas encore d'évaluation
- CHRA - Agnisyah S.P - Magister K3 FKM UIDocument24 pagesCHRA - Agnisyah S.P - Magister K3 FKM UITribuana Yogaswara BhadraPas encore d'évaluation