Académique Documents
Professionnel Documents
Culture Documents
Achieving Developmental Milestones
Transféré par
drustagiTitre original
Copyright
Formats disponibles
Partager ce document
Partager ou intégrer le document
Avez-vous trouvé ce document utile ?
Ce contenu est-il inapproprié ?
Signaler ce documentDroits d'auteur :
Formats disponibles
Achieving Developmental Milestones
Transféré par
drustagiDroits d'auteur :
Formats disponibles
Clinical Case Report
Achieving developmental milestones in a chronically ill patient
By Michaelene P. Jansen, RN, C, PhD, FNP, C, GNP-BC
Cystic fibrosis (CF) has traditionally been considered a childhood disease since most patients did not live past adolescence. Recently, statistics show that the average lifespan of an individual with CF is 37 years.1 Longer life expectancy is attributed to improved airway clearance techniques, early intervention, adequate nutrition, and bilateral lung transplantation.2 Given the longer life expectancy, patients expect to fulfill normal developmental roles, such as parenthood. Preconception care is particularly important in the CF population to insure positive outcomes for the mother and infant. Case study A.C., a 26-year-old female with known CF and pancreatic insufficiency, presented at the adult pulmonary clinic on December 12 for an interval visit. Over the past 2 years her pulmonary function had decreased significantly. She worked 6 hours a day as an evening supervisor at a retail store. Her spirometry readings showed a forced vital capacity (FVC) of 1.98 liters (54%), a forced expired volume in 1 second (FEV1) of 0.98 liter (34%) and an absolute ratio (FEV1/FVC) of 50%. Airway clearance techniques included vest therapy twice daily; 7% saline 4 mL twice daily; dornase alfa 2.5 mg inhaled daily; azithromycin 250 mg/day. She reported that she had two positive home pregnancy tests. A urine pregnancy test confirmed her pregnancy. She thought that she was www.tnpj.com
only 2 or 3 weeks pregnant. She and her husband decided to continue the pregnancy. A high-risk pregnancy referral was initiated. On February 8, A.C. returned with increased cough and sputum production. She lost 3 pounds. Her FVC was 1.82 liters (50%). Her FEV1 decreased to 0.76 liter (26%). She was unable to follow through with her high-risk prenatal evaluation because her husband had recently changed jobs and did not have outpatient insurance coverage until March 1. She estimated that she was now 10 weeks pregnant. She was admitted to the hospital for I.V. antibiotics. Her sputum was positive for pseudomonas and methicillin sensitive staphylococcus aureus. Given her pregnancy, I.V. meropenem 2 grams I.V. every 8 hours and inhaled colistin 75 mg twice daily were started. Meropenem (Merrem I.V.) is a beta lactam broad spectrum antibiotic
ing A.C.s high risk for death intrapartum or immediately postpartum, due to large change in cardiac output, cardiovascular physiology, and fluid shifts during labor and delivery, which could precipitate cardiovascular collapse. However, a maternal echocardiogram did not show any pulmonary artery hypertension. A.C. was seen in the pulmonary clinic on March 12 for follow-up of her pulmonary status. Although she was now covered by insurance she still had not scheduled a high-risk prenatal exam. Her spirometry improved to FVC 1.8 liters or 49%; FEV1 0.9 liter or 30%. Her oxygen saturation was 90% on room air. Oxygen was started at 1 liter/nasal cannula (nc). A.C.s weight was 120 pounds. A high-risk prenatal visit was scheduled. A.C. was admitted to the hospital on April 2 with increased dyspnea re-
Preconception care is particularly important in the CF population to insure positive outcomes for the mother and infant.
effective in treating pseudomonas infections. Colistin is polymixin antibiotic that has been used frequently for pseudomonas infections in CF.3 It was approved for infectious diseases for use in pregnancy as an inhaled substance. A consult for inpatient high-risk prenatal care was initiated. A vaginal ultrasound confirmed a viable fetus with gestational age 17 weeks and 2 days. Concern was expressed regardquiring oxygen at 2 liters/minute. Admission spirometry showed a FVC of 1.58 liters (43%); a FEV1 of 0.66 liter (23%), and a FEV1/FVC of 43%. She decreased her work hours to 4 hours a day to devote more time to her health. Her weight was 122 pounds. She was started on 2 weeks of I.V. meropenem and inhaled colistin. The high-risk pregnancy team was contacted, and the patient was
The Nurse Practitioner April 2009 11
Clinical Case Report
On June 23, A.C. returned for follow-up reporting that she delivered a healthy boy on June 12, weighing 6 pounds, 1 ounce. He had been in the Neonatal Intensive Care Unit for almost 2 weeks and was scheduled to be discharged within the next 48 hours. She had not been able to utilize her CF vest for airway clearance, and had been using a handheld positive pressure device without any inhaled bronchodilators or dornase alfa. She reported increased cough, dyspnea, and fatigue. Her sputum was a thick green without hemoptysis. Her weight was 116 pounds, body mass index (BMI) 21.2. She had not been able to utilize any oxygen during the previous 2 weeks, as she did not have any portable oxygen tanks. Her FVC was 1.83 liters (50%), FEV1, 0.98 liter, (33%), and FEV1/FVC 53%. Blood glucose levels fluctuated between 80 and 300 mg/dL. Although A.C. was trying to breastfeed, she opted to use tobramycin and meropenem for I.V. antibiotic therapy because she previously had better results with this combination. She agreed to discard her breast milk for the duration of antibiotics. On July 14, A.C. returned for follow-up and brought her son along. She continued to utilize oxygen at 1 to 2 liters/minute via nc as well as the airway clearance devices. She felt better and her son was sleeping 4 hours at a time allowing her to get more rest. Her parents continued to help out. Her weight was 112 pounds, BMI 20.5. Her spirometry readings were FVC 1.84 liters (50%), FEV1 0.95 liter (32%), and FEV1/FVC 51.6%. Discussion This case presentation involves a complex case of a young woman with a serious chronic illness desiring to have normal life and development. Preconception care and careful planning of a pregnancy would have been www.tnpj.com
Definitions
CF Cystic fibrosis is a genetic disease caused by a mutation of the cystic fibrosis transmembrane conductance regulator gene. FVC Forced vital capacity is the amount of air that can be expired following maximum inspiration. It is measured in liters, and a percentage is provided comparing actual and predicted values. A decrease in FVC may indicate restrictive lung disease. Normal FVC: 80%-120%. FEV1 Forced expiratory volume in 1 second is the amount of air that that can be exhaled in 1 second. It is measured in liters and a percentage is provided comparing actual and predicted values. A decreased FEV1 may indicate obstructive lung disease. Normal: FEV1 80%-120% Mild CF: FEV1 > 70% Moderate CF: FEV1 = 40%-70% Severe CF: FEV1 < 40% FEV1/FVC The absolute ratio between the amount of air that can be expired in 1 second and the total amount of air that can be forcibly expired. A normal ratio is between 75% and 80%. CF Vest A vibratory vest used to provide airway clearance. Patients use the vest at various settings to loosen lung secretions two to four times a day. Dornase alfa A recombinant human DNase developed to degrade the large amount of free DNA that accumulates within mucus of CF patients, decreasing the viscosity and improving airway clearance. Dornase alfa is an inhaled substance that is used once or twice a day as part of airway clearance therapy.3 Hypertonic saline (7%) saline 7% saline is a hypertonic solution that is inhaled twice daily to increase the hydration of airway surface liquid as a method of improving mucus clearance.3 Azithromycin A macrolide antibiotic that is used for its antimicrobial and anti-inflammatory properties. Chronic use of azithromycin (250 mg/day or 500 mg three times/ week) has been shown to improve lung function and reduce exacerbations.3 Positive pressure device A handheld device that provides positive pressure so that when a patient exhales through the device, oscillations in airway pressure loosen the mucus in the airways.
seen as an inpatient with a full evaluation on the day of discharge at the high-risk prenatal center. On May 21, A.C. returned to the clinic. She was 31 weeks pregnant, and was seeing the high-risk prenatal specialist every 1 to 2 weeks. She was diagnosed with gestational diabetes and was started on insulin. She quit work and utilized oxygen at 1 liter/minute via nc at all times. Her FVC was 1.87 liters (51%); FEV1 0.98 liter (33%), and FEV1/FVC (52%). Her weight was 129 pounds.
12 The Nurse Practitioner Vol. 34, No. 4
A.C. returned to clinic on June 9 following a prenatal visit. Her cough had increased, and was now producing tan sputum. She was using oxygen at 2 liters/minute at night. She reported that the high-risk prenatal team felt that she was doing well and had no immediate concerns. She was slightly more dyspneic. Spirometry showed a FVC of 1.96 liters (54%), a FEV1 of 1.02 liters (35%), and a FEV1/FVC of 52%. Her healthcare providers anticipated that she would need one more round of I.V. antibiotics prior to delivery.
Clinical Case Report
extremely beneficial; however, this did not occur since the pregnancy was unplanned. Several issues come to light in examining this case, including ethical decision making, treatment options, and nutrition and lifestyle choices.4 Ethical decision making Although A.C. and her husband were not planning a pregnancy at the time of conception, they were faced with the decision whether or not to terminate the pregnancy in its early stages. Given A.C.s steady decline in pulmonary function over the past 2 years, the pregnancy posed a high risk for further decline in A.C.s pulmonary status. Prior to her pregnancy, discussions had been undertaken to proceed with an evaluation for lung transplantation. The healthcare team had concerns that she would continue her current rate of decline further if she allowed the pregnancy to progress. Following through with the transplant evaluation may have served as a safety net if A.C.s condition had severely declined during the pregnancy. The high-risk prenatal team had had concerns related to her morbidity and mortality due to cardiovascular changes that occur with pregnancy. Evidence on pregnancy outcomes in patients with CF is minimal and does not clearly demonstrate that pregnancy affects the course of CF.5 One study found that women with severe pulmonary impairment tend to deliver lower weight babies, and that there is no evidence to determine prospectively which women with CF will tolerate pregnancy.6 There were several times throughout this pregnancy where A.C. was faced with the decision to continue or terminate the pregnancy. The healthcare teams made it clear that they would fully support any decision she made. www.tnpj.com Treatment options Aggressive airway management was initiated to maintain adequate pulmonary function to A.C. as well as to the fetus. Supplemental oxygen was required early in the pregnancy. Adequate oxygenation was a major concern for the high-risk prenatal team as well. Early prenatal care was intermittent, due to A.C.s lack of insurance coverage in addition to the distance to the high-risk prenatal center. The high-risk prenatal service was a separate healthcare organization from the CF center, which required frequent communication. Treatment options for CF exacerbations were limited based on allergies, pregnancy, and organisms cultured. When possible, her providers adhered to the Cystic Fibrosis Foundation guidelines for lung health maintenance.3 Inhaled colistin was continued throughout A.C.s pregnancy to reduce the probability of pseudomonas infection. Although the goal to get A.C. to 36 weeks was not reached, she did deliver at 33 weeks. One of the key variables was A.C.s decision to quit working and focus on rest, airway clearance, and maintaining oxygen saturation more than 90%. Nutrition Adequate nutrition and weight gain were a priority for A.C. as she was below her ideal body weight at the time of her pregnancy. Pancreatic insufficiency and vitamin deficiency are consequences of CF, as well as important variables in food absorption and weight gain.7,8 Additional nutritional requirements of pregnancy added an additional challenge for gaining the appropriate weight for fetal development. Upon confirmation of pregnancy, the high-risk prenatal team was contacted and A.C.s ABDEK vitamins were switched to prenatal vitamins with added folic acid. Supplemental nutrition was added twice daily. Close monitoring by nutritional services was key to weight gain during the pregnancy. A.C.s weight 2 weeks postpartum was the same as her weight in December. A multidisciplinary challenge Pregnancy in an individual with a life threatening chronic illness presents many challenges to the healthcare team. A multidisciplinary approach, as well as ongoing communication between the various healthcare providers was key; especially when early prenatal care was intermittent. The ongoing challenge for A.C. is to maintain her pulmonary function in the postpartum period. The balance of caring for her infant, maintaining adequate nutrition and sleep for herself, and finding time for airway clearance will continue to be a challenge for her.4,5
REFERENCES
1. Cystic Fibrosis Foundation Patient Registry. 2005 Annual Data Report to the Center Directors. Bethesda, MD: Cystic Fibrosis Foundation; 2005. 2. Farrell PM, Rosenstein BJ, White TB, et al. Guidelines for diagnosis of cystic fibrosis in newborns through older adults: cystic fibrosis foundation consensus report. J Pediatr. 2008;153:S4-S14. 3. Flume PA, OSullivan BP, Robinson KA, et al. Cystic fibrosis pulmonary guidelines. Chronic medications for maintenance of lung health. Am J Respir Crit Care Med. 2007;176:957-969. 4. Wexler ID, Johannesson M, Edenborough FP, et al. Pregnancy and chronic progressive pulmonary disease. AJRCCM. 2007;175:300-305. 5. McMullen AH, Pasta DJ, Frederick PD, et al. Impact of pregnancy on women with cystic fibrosis. Chest. 2006;129:706-711. 6. Cheng EY, Goss CH, McKone EF, et al. Aggressive prenatal care results in successful fetal outcomes in CF women. J Cyst Fibrosis. 2006;5(2):8591. 7. Lai HC, Shoff SM. Classification of malnutrition in cystic fibrosis: implications for evaluation and benchmarking clinical practice performance. Am J Clin Nutr. 2008;88:161-166. 8. Stallings VA, Stark LJ, Robinson KA, et al. Evidence-based practice recommendations for nutrition-related management of children and adults with cystic fibrosis and pancreatic insufficiency: results of a systematic review. J Am Diet Assoc. 2008;108:832-839. Dr. Michaelene P. Jansen is a nurse practitioner in the adult pulmonary clinic at the University of Wisconsin Hospital and Clinics, Madison. The University of Wisconsin is an approved Adult Cystic Fibrosis Center.
The Nurse Practitioner April 2009 13
Vous aimerez peut-être aussi
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeD'EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeÉvaluation : 4 sur 5 étoiles4/5 (5794)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreD'EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreÉvaluation : 4 sur 5 étoiles4/5 (1090)
- Never Split the Difference: Negotiating As If Your Life Depended On ItD'EverandNever Split the Difference: Negotiating As If Your Life Depended On ItÉvaluation : 4.5 sur 5 étoiles4.5/5 (838)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceD'EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceÉvaluation : 4 sur 5 étoiles4/5 (895)
- Grit: The Power of Passion and PerseveranceD'EverandGrit: The Power of Passion and PerseveranceÉvaluation : 4 sur 5 étoiles4/5 (588)
- Shoe Dog: A Memoir by the Creator of NikeD'EverandShoe Dog: A Memoir by the Creator of NikeÉvaluation : 4.5 sur 5 étoiles4.5/5 (537)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersD'EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersÉvaluation : 4.5 sur 5 étoiles4.5/5 (344)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureD'EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureÉvaluation : 4.5 sur 5 étoiles4.5/5 (474)
- Her Body and Other Parties: StoriesD'EverandHer Body and Other Parties: StoriesÉvaluation : 4 sur 5 étoiles4/5 (821)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)D'EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Évaluation : 4.5 sur 5 étoiles4.5/5 (121)
- The Emperor of All Maladies: A Biography of CancerD'EverandThe Emperor of All Maladies: A Biography of CancerÉvaluation : 4.5 sur 5 étoiles4.5/5 (271)
- The Little Book of Hygge: Danish Secrets to Happy LivingD'EverandThe Little Book of Hygge: Danish Secrets to Happy LivingÉvaluation : 3.5 sur 5 étoiles3.5/5 (399)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyD'EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyÉvaluation : 3.5 sur 5 étoiles3.5/5 (2259)
- The Yellow House: A Memoir (2019 National Book Award Winner)D'EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Évaluation : 4 sur 5 étoiles4/5 (98)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaD'EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaÉvaluation : 4.5 sur 5 étoiles4.5/5 (266)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryD'EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryÉvaluation : 3.5 sur 5 étoiles3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnD'EverandTeam of Rivals: The Political Genius of Abraham LincolnÉvaluation : 4.5 sur 5 étoiles4.5/5 (234)
- On Fire: The (Burning) Case for a Green New DealD'EverandOn Fire: The (Burning) Case for a Green New DealÉvaluation : 4 sur 5 étoiles4/5 (73)
- The Unwinding: An Inner History of the New AmericaD'EverandThe Unwinding: An Inner History of the New AmericaÉvaluation : 4 sur 5 étoiles4/5 (45)
- New Blank TemplateDocument11 pagesNew Blank TemplateAmine MoutaqiPas encore d'évaluation
- Top Questions Asked About SAFe ExamsDocument2 pagesTop Questions Asked About SAFe ExamsdrustagiPas encore d'évaluation
- Change Log TemplateDocument3 pagesChange Log TemplatedrustagiPas encore d'évaluation
- Storyboard 0Document1 pageStoryboard 0drustagiPas encore d'évaluation
- Appreciation Cards v.1.0Document2 pagesAppreciation Cards v.1.0drustagiPas encore d'évaluation
- APG Design and Development 2015Document7 pagesAPG Design and Development 2015John RajeshPas encore d'évaluation
- SDC Course OutlineDocument3 pagesSDC Course OutlinedrustagiPas encore d'évaluation
- Agile Scrum at Glance BaselineDocument1 pageAgile Scrum at Glance BaselinedrustagiPas encore d'évaluation
- SMC Class ScheduleDocument1 pageSMC Class ScheduledrustagiPas encore d'évaluation
- 6 Six Sigma Roadmap RevDocument20 pages6 Six Sigma Roadmap RevJuan PabloPas encore d'évaluation
- Describe and Compare Below The Changes Requested To Current Product Features/requirementsDocument1 pageDescribe and Compare Below The Changes Requested To Current Product Features/requirementsdrustagiPas encore d'évaluation
- Set Project Priorities - ToCDocument4 pagesSet Project Priorities - ToCdrustagiPas encore d'évaluation
- Scrum Master Certification (SMC™) Course OutlineDocument1 pageScrum Master Certification (SMC™) Course OutlinedrustagiPas encore d'évaluation
- Leanmap FREE Six Sigma Tool OverviewDocument2 pagesLeanmap FREE Six Sigma Tool OverviewdrustagiPas encore d'évaluation
- Updated Agile - KanbanDocument25 pagesUpdated Agile - Kanbandrustagi100% (1)
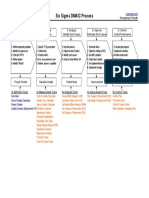
- Leanmap FREE Six Sigma DMAIC ProcessDocument1 pageLeanmap FREE Six Sigma DMAIC ProcessdrustagiPas encore d'évaluation
- Six Sigma Fact SheetDocument4 pagesSix Sigma Fact SheetMarcus Skookumchuck VanniniPas encore d'évaluation
- FBD, Fmea, ParetoDocument5 pagesFBD, Fmea, ParetodrustagiPas encore d'évaluation
- A Solution Template To Help in Hypothesis TestingDocument3 pagesA Solution Template To Help in Hypothesis TestingdrustagiPas encore d'évaluation
- Lean Vs Six SigmaDocument23 pagesLean Vs Six SigmaSiddharth ChakkarwarPas encore d'évaluation
- PDSA History Ron MoenDocument9 pagesPDSA History Ron MoenAli Shah100% (1)
- MAW KitDocument3 pagesMAW KitdrustagiPas encore d'évaluation
- Quality Management Gurus TheoriesDocument6 pagesQuality Management Gurus TheoriesSyafiqah RedzwanPas encore d'évaluation
- A Solution Template To Help in Hypothesis TestingDocument3 pagesA Solution Template To Help in Hypothesis TestingdrustagiPas encore d'évaluation
- Quality Management Gurus TheoriesDocument6 pagesQuality Management Gurus TheoriesSyafiqah RedzwanPas encore d'évaluation
- Sample Chartered Accountant ResumeDocument5 pagesSample Chartered Accountant ResumedrustagiPas encore d'évaluation
- PDSA History Ron MoenDocument9 pagesPDSA History Ron MoenAli Shah100% (1)
- The Benefits of PDCADocument2 pagesThe Benefits of PDCAdrustagiPas encore d'évaluation
- Who Are The TOP Quality GurusDocument8 pagesWho Are The TOP Quality GurusdrustagiPas encore d'évaluation
- Chartered Accountant Resume Sample - Best FormatDocument4 pagesChartered Accountant Resume Sample - Best FormatdrustagiPas encore d'évaluation