Académique Documents
Professionnel Documents
Culture Documents
A Study On Ventilator Associated Pneumonia in
Transféré par
Al MuzakkiDescription originale:
Titre original
Copyright
Formats disponibles
Partager ce document
Partager ou intégrer le document
Avez-vous trouvé ce document utile ?
Ce contenu est-il inapproprié ?
Signaler ce documentDroits d'auteur :
Formats disponibles
A Study On Ventilator Associated Pneumonia in
Transféré par
Al MuzakkiDroits d'auteur :
Formats disponibles
NATIONAL JOURNAL OF MEDICAL RESEARCH print ISSN: 2249 4995eISSN: 2277 8810
ORIGINAL ARTICLE
A STUDY ON VENTILATOR ASSOCIATED PNEUMONIA IN PEDIATRIC AGE GROUP IN A TERTIARY CARE HOSPITAL, VADODARA
Modi Payal P1, Javadekar Tanuja B2, Nanda Sandeep3, Pandya Neelam N3
1Tutor, 2Prof.
& Head, 3Assistant Professor, Department of Microbiology, Medical College Baroda, Baroda
Correspondence: Dr. Payal Modi, Email: Payal_2304@yahoo.co.in
ABSTRACT
Introduction: Approximately 10-28% of critical care patients develop Ventilator Associated Pneumonia (VAP). It increases length of stay in ICU up to 28% and each incidence ofVentilator-associated pneumonia(VAP) is estimated to generate an increased cost of 6000-22000. Mortality rate is 24%-71%. Objectives: To determine the incidence rate, bacteriological profile and antibiotic sensitivity pattern of ventilatorassociated pneumonia in pediatric intensive care unit (PICU) & Neonatal intensive care unit(NICU) Methods: In this study total 125 patients of pediatric age group admitted in ICU & put on ventilator at SSGH from November 2010 to November 2011 were enrolled. After the clinical confirmation according to CDC criteria, the endotracheal secretion were collected and processed as per standard microbiological methods and antibiotic sensitivity pattrn of each were recorded. Results: Of total 125 samples 58 samples were positive. Most common Organism isolated are Klebseilla spp.(35%), Acinetobactor spp.(26%), Psedomonas spp.(15%),other enterobactriacae(13%), Gram positive cocci(8%) and candida spp(3%). Among the isolates for Gram Negative Bacilli Imipenem and Vancomycin for Gram Positive Cocci is recommended. Conclusion: Among the isolates for Gram Negative Bacilli Imipenem and Vancomycin for Gram Positive Cocci is recommended Key words: ventilator associated pneumonia, CDC guidelines of VAP, Endotracheal aspirate culture INTRODUCTION Approximately 10-28% of critical care patients develop VAP1. It increases length of stay in ICU up to 28% and each incidence ofVentilator-associated pneumonia(VAP) is estimated to generate an increased cost of 6000-220001. Mortality rate is 24%-71%2 VAP is the second most common cause of the nosocomial infection after urinary tract infection among pediatric and neonatal intensive care unit (NICU) patients.3 Infants mechanically ventilated in the NICU are at a particularly high risk of developing Ventilator-associated pneumonia because of poor host factors, severe underlying diseases, prolonged use of mechanical ventilation, inadequate pulmonary toilet and extensive use of invasive devices and procedures4 VAP is defined as nosocomial pneumonia in mechanically ventilated patients that develops with in 48 hours or more , after initiation of mechanical ventilation . The pneumonia was neither present nor incubating at the time of intubation.5 This study was conducted to determine the incidence rate, bacteriological profile and antibiotic sensitivity pattern of ventilator-associated pneumonia in pediatric intensive care unit (PICU) & Neonatal intensive care unit(NICU) in a teaching hospital. METHODOLOGY Study area and Duration: This study is carried out at Department of Microbiology, in S.S.G.Hospital, from November 2010 to November 2011. Study sample: The review of literature showed prevalence of VAP in 0-12 years of age group was around 30%10-14. In our study we expected prevalence to be around 50%. With the Type-I error fixed at 0.01 and typeII error at 0.10, we found sample size 83 , using MEDCALC software version 11.5.0. As this
Page 318
Volume 2Issue 3July Sept 2012
NATIONAL JOURNAL OF MEDICAL RESEARCH print ISSN: 2249 4995eISSN: 2277 8810
study starts from November 2010 to November 2011, total 125 pediatric patients who were kept on mechanical ventilator were enrolled. Study population: All children below 12 years of age kept on mechanical ventilation & admitted in Intramural NICU (patient directly admitted in NICU, S.S.G.Hospital), Extramural NICU (patients reffered from other hospital) and PICU included in study population. Inclusion criteria: Patients aged between 0-12 years; Patients admitted in Intensive Care Unit or transferred to the unit from paediatric wards for any medical conditions/complications; Patients kept on mechanical ventilator for >48 hours. Exclusion criteria: Patients already having pneumonia at the time of ICU admission and Patients who developed pneumonia in the first 48 hours of mechanical ventilation. For the diagnosis of VAP Criteria of Centers for Disease Control and Prevention (CDC)7 was used. Radiology signs: Two or more serial radiographs with at least one of the following - new or progressi ve and persistent Infiltrate - consolidation - cavitation chest
transported aseptically to the laboratory within one hour of collection. Sample collected at night was stored at 4 degree centigrade overnight and send to the laboratory by 10 am next day morning. Endotracheal aspirate culture were collectedbefore putting the patient on ventilation and also after 48 hrs of ventilaton, received in our department. Samples were processed as per the standard methods.Specimens are taken prior to start next scheduled antibiotic dose.In case of Endotracheal aspirate culture, >106 cfu/ml was considered significant for the diagnosis of VAP. After achiving the growth sensitivity was also done as per CLSI(Clinical and Laboratory Standard Institute) guidelines. RESULTS Incidence of VAP in present study was 46.4%.( From 125 samples, 54 samples showed monomicrobial growth while only 4 samples showed polymicrobial growth and 67 samples were showing no growth.) Maximum number of patients having VAP belongs to early neonatal age group ( 0-7 days) that is 73%(91) and followed by 1-12 years of age group 12%(15) followed by infants of age group 8% (10)and lastly late neonatal age group 7%(9) Table 1: Different organisms isolated in this study Name of Organism Klebseilla spp. Acinetobacter spp. E.coli Pseudomonas spp. Proteus spp. Providentia spp. Morgenella Enterococcus Coagulase Negative Staphylococcus Staphylococcus aureus Candida spp. No. of isolates (n=62) (%) 22 (35.5) 16 (25.8) 5 (8.1) 9 (14.5) 1 (1.6) 1 (1.6) 1 (1.6) 2 (3.2) 2 (3.2) 1 (1.6) 2 (3.2)
Clinical signs: At least 1 of the following: -fever (temperature > 38 C) -leukopenia (< 4000 WBC) or leukocytosis (> 12000 WBC) - altered mental status, for adults 70 years or older, with no other recognized cause Plus at least 2 of the following - new onset of purulent sputum, or change in character of sputum - increased respiratory secretions, or increased suctioning requirements new-onset or worsening cough, or dyspnea, or tachypnea - rales or bronchial sounds - worsening gas exchange - increased oxygen requirements Microbiological criteria: At least one of the following: - positive growth in blood culture not related to another source of infection - positive quantitative culture from broncho alveolar lavage (> 104) or protected specimen brushing (> 103) - five percent or more of cells with intracellular bacteria on direct microscopic examination of Gram-stained bronchoalveolar lavage fluid - histopathological evidence of pneumonia As for the diagnosis we are following CDC guidelines9 clinical criteria are satisfied and after than evaluation of microbiological criteria is done. After proper hand washing and wearing sterile gloves before suctioning, the endotracheal aspirates were collected from the endotracheal tube with the help of sterile Deles mucous trap. The specimen collected was immediately
Volume 2Issue 3July Sept 2012
Follow up of the patients, from whom the samples were isolated, revealed 65 (52.0%) patient died in the hospital while remaining 60 (48.0%) patients either discharges or DAMA (Discharge Against Medical Advice) or transferred to wards or absconded) DISCUSSION & CONCLUSION There are very few studies on VAP in pediatric age group. Incidence varies in different studies10-14. Such large variation in incidence is due to case-mix differences, differences in the diagnostic criteria used, the variable sensitivity and specificity of the available diagnostic tests, lack of gold standard test for diagnosis of VAP, condition of ICU, nursing care, variability in
Page 319
NATIONAL JOURNAL OF MEDICAL RESEARCH print ISSN: 2249 4995eISSN: 2277 8810
the presence of Hospital flora, Policy of Hospital for fumigation of ICU, care and maintenance of various equipments ( warmer, ventilator machine) and in
different studies difference in age group (neonates, infants & children).
Table 2: Antibiotic sensitivity pattern of Gram Negative Bacilli Klebseilla spp. Acinetobacter spp. E.coli (n=5) (%) Proteii gp. (n=3) (n=22) (%) (n=16) (%) (%) Amika 13 (60) 7 (41) 3 (50) 3 (100) Genta 3 (13) 2 (14) 1 (13) 1 (33) CTX 4 (18) 2 (10) 1 (25) 1 (33) Imi * 21 (93) 16 (100 ) 5(100) 3 (100) Ampi +sulb 4 (20) 2 (10 ) 2 (38) 0 (0) Pipera 5 (22) 2 (14) 2 (38) 0 (0) Pipera + Tazo 8 (38) 3 (21) 3 (50) 1 (33) Oflox 9 (42) 5 (31) 3 (50) 3 (100) Netil 9 (40) 2 (14) 1 (13) 0 (0) Cipro 10 (47) 4 (28) 3 (50) 0 (0) Tobra 9 (42) 4 (24) 1 (25) 0 (0) Gati 12 (53) 13 (79) 5(100) 3 (100) Amika Amikacin, Genta- Gentamycin, CTX- Cefotaxime, Imi-Imipenem, Ampi+Sulb- Ampicillin+Sulbectum, Pipera- Piperacillin, Pipera+Tazo-Piperacillin+Tazobactum, Oflox-Ofloxacin, Netil-Netilmycin, CiproCiprofloxacin, Tobra-Tobramycin, Gati- Gatifloxacin (* good sensitivity) Table 3 Antibiotic sensitivity of Gram Positive Cocci. Antibiotic Enterococc Coagulas Staphy.aure us Spp. e Neg us (n=1) (%) (n=2) (%) Staphy. (n=22) (%) Cefazolin 1 (50) 1 (50) 1 (100) Chloramphenic 1 (50) 1 (50) 1 (100) ol Erythromycin 1 (50) 1 (50) 1 (100) Vancomycin* 2 (100) 2 (100) 1 (100) Cefotaxime* 2 (100) 2 (100) 1 (100) Ciprofloxacin* 2 (100) 2 (100) 1 (100) Ofloxacin* 2 (100) 2 (100) 1 (100) Penicillin 1 (50) 1 (50) 1 (100) Amoxycillin + 1 (50) 1 (50) 1 (100) Clavulanic acid Cloxacillin 1 (50) 1 (50) 1 (100) Oxacillin 1 (50) 1 (50) 1 (100) Linezolid* 2 (100) 2 (100) 1 (100) *Good sensitivity In summary, ventilator-associated pneumonia (VAP) is a leading cause of morbidity and mortality in ICU patients, leading to lengthened ICU and hospital stays and higher health care costs16-17. VAP continues to be an important challenge to the critical care physician and is the most common nosocomial acquired infection among patients with acute respiratory failure. It is difficult to diagnose accurately, and a high index of suspicion is required. The mortality caused by VAP increases if it is caused by resistant bacteria.Since some clinical interventions increase the development of VAP, clinical guidelines for the treatment of VAP should be developed, pediatricians should understand its
Volume 2Issue 3July Sept 2012
Antibiotic
epidemiology and participate in control measures, by reducing the risk of cross-contamination during mechanical ventilation, preventing colonization and aspiration. Table 4: Antibiotic sensitivity of Psuedomonas Antibiotic Piperacillin Piperacillin + Tazoactum Cabencillin Amikacin Ticarcilli+ Clavlunic acid Cefazidime Imipenem* Polymyxin B* Lomefloxacin Ciprofloxacin Ofloxacin Tobramycin *Good sensitivity RECOMMENDATION Good management strategies for VAP like adequate infection control practices and better nursing care, early and accurate diagnosis and more specific antimicrobial use may significantly improve patients outcome. If VAP is suspected empirical antibiotics, in combination of Vancomycin (for gram positive organism including MRSA(Methicillin Resistant S. aureus)), imipenem (for pseudomonas) and aminoglycosides or imipenem (for gram negative organisms) should be given immediately. Although bacteriological sampling is important, it should not significantly delay the start of treatment. As the appropriateness of the initial antibiotic regimen is a
Page 320
Psuedomonas 4 (43) 4 (43) 3 (29) 7 (78) 3 (29) 4 (43) 8 (86) 8 (86) 4 (43) 5 (57) 4 (43) 5 (50)
NATIONAL JOURNAL OF MEDICAL RESEARCH print ISSN: 2249 4995eISSN: 2277 8810
vital determinant of outcome, microbiological advice should be sought. There is an increasing prevalence of MRSA and multidrug resistant pathogens in late onset Table 5: Common organisms isolated in various studies Various Studies Shalini Tripathi et al.3 Anucha A et al.15 Alexis M. Elward et al.12 Elizabeth Foglia et al.7 Witaya Petdachai et al.4 Ramya Srinivasan et al.14 Present study LIMITATIONS There was a limitation in the sampling procedures used to obtain microbiologic specimens from the small respiratory tract in our study, in that invasive techniques to distinguish infection from colonization are not practical or feasible and may be harmful in small infants. They can impair blood-gas exchange, delay treatment, and lead to sepsis. So the techniques which are more sensitive and specific like BAL(Broncho Alveolar Lavage), B-PSB (BlindProtected Specimen Brushing), NB-PSB(Non BlindProtected Specimen Brushing), MINI BAL could not be possible which is possible in higher age group. Though pediatric studies were very few, most of the data are available for only adult patients. REFERANCES
1. Acharya Hwad. Ventilator Associated Pneumonia - An Overview. British Hournal of Medical Practitioners. [Review]. 2009;2(2):16-9. Richard Scott. Ventilator-Associated Pnuemonia. Arch Intern Med. [Review]. 2000;160:1926-36. Shalini Tripathi, Amita Jain, Neera Kohli. Study Of Ventilator Associated Pneumonia In Neonatal Intensive Care Unit : Charecterisitcs, Risk Factors and Outcome. Internel Journal of Medical Update. [Original]. 2010;5(1):12-9. Petdachai W. Ventilator Associated Pneumonia In A Newborn Intensive Care Unit. Journal of Peadiatrics. 2004;35(3):724 to 9. Noyal Mariya Joseph SS, Tarun Kumar Dutta, Ashok Shankar Badhe, Desdemona Rasitha, Subhash Chandra Parija. Ventilator-Associated Pneumonia In A Tertiary Care Hospital In India : Role Of Multi-Drug Resistant Pathogens. JIPMER, Pondicherry, India. [Original]. 2010;4(4):218-25. Park DR. The Microbiology Of Ventilator-Associated Pnuemonia. Respiratory Care. 2005;50(6):742-65.
VAP, and antimicrobial therapy should take account of this. Subsequent microbiological findings should be used to tailor antibiotic therapy.
Organisms isolated (%) Pseudo Monas E. coli Klebsiella Acinetobacter Proteii. gp 11% 23% 33% 18% NM 10% 7% 31% 12% 7.7% 29.4% 3% 14% NM NM 38.4% NM 23% NM NM 38.2% NM 27.3% 25.4% NM 2.6% 10.3% NM NM NM 15% 8% 35% 26% 6%
7.
GPC Candida 10% 3% 12% 2% 21% 9% 23% NM 3.6% NM 33% 2.3% 8% 3%
Elizabath Foglia MDMaAE. Ventilator-Associated Pneumonia In Neonatal And Pediatric Intensive Care Unit Patients. Clinical Microbiology Reviews. [Review]. 2007;20(3):409-25. J.C.Overall J, and M.R.Britt. Nosocomial Infection In A Newborn Intensive Care Unit. Results of 41 month study. NEngl J Med. 1976;294:1310-6. CDC. Ventilator-Associated Pnuemonia (VAP) Event. CDC guidelines.6-1 TO 6-14. Fagon JCaJ-Y. Ventilaor-Associated Pneumonia. American Journal of Respiratory and Critical Care Medicine. [State of Art]. 2002;165:867-903. Tejada Artigas A BDS, Chacon Valles E, Munoz Marco J, Villuendas Uson MC, Figueras P, Suarez FJ, Hernandez A. Risk factors for nosocomial pneumonia in critically ill trauma patients. Crit Care Med. 2001;29:304-9. Alexis M. Elward, Victoria J. Fraser. Ventilator-Associated Pneumonia In Pediatric Intensive Care Unit Patients : Risk Factors And Outcomes. Pediatrics. 2002;109(5):757-62. Markowicz P WM, Djedaini K, Cohen Y, Chastre J, Delclaux C,, Merrer J HB, Veber B, Fontaine A, et al. . Multicenter prospective study of ventilator-associated pneumonia during acute respiratory distress syndrome. ATS Journal. 2000;161:1942-8. Srinivasan R, Asselin J, Gildengorin G, Wiener-Kronish J, Flori HR. A prospective study of ventilator-associated pneumonia in children. Pediatrics 2009;123:1108-1115. Anucha Apisarnathanarak; Aaron Hamvas, Margaret A.Olsen, J.Fraser, MD. Ventilator-Associated Pneumonia In Extremely Preterm Neonates In A Neonatal Intensive Care Unit : Characteristics, Risk Factors And Outcomes. Pediatrics. 2003;112(6):1283-8 Fagon J, Chastre J, Hance A, et al. Nosocomial pneumonia in ventilated patients: a cohort study evaluatingattributable mortality and hospital stay. AmJ Med 1993; 94: 281-8. Fagon JY, Chastre J, Vaugnat A, Trouillet JL, Novara A, Gibert C. Nosocomial pneumonia and mortalityamong patients in intensive care units. JAMA 996; 275: 866-9
8.
9. 10.
11.
12.
13.
2. 3.
14.
15.
4. 5.
16.
17.
6.
Volume 2Issue 3July Sept 2012
Page 321
Vous aimerez peut-être aussi
- Klebsiella PDFDocument4 pagesKlebsiella PDFOscarEduardoPas encore d'évaluation
- Journal Read ChiaDocument14 pagesJournal Read ChiaChris Tine ChiaPas encore d'évaluation
- Vap NicuDocument8 pagesVap NicuWiwit ClimberPas encore d'évaluation
- Neonatal PneumoniaDocument8 pagesNeonatal PneumoniaAde Gustina SiahaanPas encore d'évaluation
- Minor Diagnostic Factors in Ventilator Associated Pneumonia in ChildrenDocument9 pagesMinor Diagnostic Factors in Ventilator Associated Pneumonia in ChildrenmariskaPas encore d'évaluation
- VAP Incidence, Risk Factors and Bacteria in PICUDocument6 pagesVAP Incidence, Risk Factors and Bacteria in PICURabiatul 'raney' AdawiyahPas encore d'évaluation
- Neocon 2017Document71 pagesNeocon 2017Jasleen KaurPas encore d'évaluation
- Risk Factor TaiwanDocument5 pagesRisk Factor TaiwanMira ApriliaPas encore d'évaluation
- ADW Presentasi - Epidemiologi VAP Hippi 2023Document30 pagesADW Presentasi - Epidemiologi VAP Hippi 2023ERIE YUWITA SARIPas encore d'évaluation
- Risk Factors for Suppurative Complications in Children with PneumoniaDocument6 pagesRisk Factors for Suppurative Complications in Children with PneumoniaWilson LeccaPas encore d'évaluation
- Carraro 2013 RSBMTV 46 N 2 P 161Document5 pagesCarraro 2013 RSBMTV 46 N 2 P 161Emerson CarraroPas encore d'évaluation
- Microbiological Profile of Bronchoalveolar Lavage in Patients With Nosocomial Pneumonia in Neonatal Intensive Care UnitDocument4 pagesMicrobiological Profile of Bronchoalveolar Lavage in Patients With Nosocomial Pneumonia in Neonatal Intensive Care UnitIJAR JOURNALPas encore d'évaluation
- 209 Full PDFDocument8 pages209 Full PDFAngga PratamaPas encore d'évaluation
- JCDR 10 SC06Document6 pagesJCDR 10 SC06YANPas encore d'évaluation
- CAPDocument21 pagesCAPLoids IgnacioPas encore d'évaluation
- Ventilator Associated Pneumonia: Incidence, Profile and Outcome in Pediatric Intensive Care Unit of Tertiary Care CentreDocument5 pagesVentilator Associated Pneumonia: Incidence, Profile and Outcome in Pediatric Intensive Care Unit of Tertiary Care CentreJoaquín SosaPas encore d'évaluation
- Clinical Presentation and Laboratory Features in Pediatric Typhoid Fever Patient Susceptibility To First-Line Antibiotic TherapyDocument10 pagesClinical Presentation and Laboratory Features in Pediatric Typhoid Fever Patient Susceptibility To First-Line Antibiotic TherapySuci ZahraniPas encore d'évaluation
- AygunDocument5 pagesAygunotheasPas encore d'évaluation
- Oseltamivir For Coronavirus Illness:: ResearchDocument6 pagesOseltamivir For Coronavirus Illness:: ResearchellaPas encore d'évaluation
- Jurnal 2Document12 pagesJurnal 2zingioPas encore d'évaluation
- Effect of Reusing Suction Catheters On The Occurrence of Pneumonia in ChildrenDocument9 pagesEffect of Reusing Suction Catheters On The Occurrence of Pneumonia in ChildrenSitti Rosdiana YahyaPas encore d'évaluation
- Critical Care InfectionDocument15 pagesCritical Care InfectionTito Ahmad RizkiawanPas encore d'évaluation
- Covid Ihu 2 1 PDFDocument28 pagesCovid Ihu 2 1 PDFSayed MachfudPas encore d'évaluation
- Covid Ihu 2 1 PDFDocument28 pagesCovid Ihu 2 1 PDFhlim_13Pas encore d'évaluation
- Original Article: Evaluation of Microbial Flora in Chronic Tonsillitis and The Role of TonsillectomyDocument5 pagesOriginal Article: Evaluation of Microbial Flora in Chronic Tonsillitis and The Role of TonsillectomyAmril BillahmarPas encore d'évaluation
- Mortality in Typhoid Intestinal Perforation-A Declining TrendDocument3 pagesMortality in Typhoid Intestinal Perforation-A Declining Trendaura009Pas encore d'évaluation
- Candidiasis in PICUDocument6 pagesCandidiasis in PICUMeirinda HidayantiPas encore d'évaluation
- Lau 2015Document25 pagesLau 2015tifanny carolinaPas encore d'évaluation
- Neonatal Pneumonia Incidence and Outcomes in BangladeshDocument6 pagesNeonatal Pneumonia Incidence and Outcomes in BangladeshAnonymous Us5v7C6QhPas encore d'évaluation
- A Prospective, Randomized Study of Ventilator-Associated Pneumonia in Patients Using A Closed vs. Open Suction SystemDocument7 pagesA Prospective, Randomized Study of Ventilator-Associated Pneumonia in Patients Using A Closed vs. Open Suction SystemFebri Nick Daniel SihombingPas encore d'évaluation
- BJC 2017154Document8 pagesBJC 2017154Altair CamargoPas encore d'évaluation
- Covid NiñosDocument9 pagesCovid NiñosPaola ZuluagaPas encore d'évaluation
- Streptococcus Pneumoniae Carriage, Resistance and Serotypes Among Jordanian Children From Wadi Al Seer District, JordanDocument8 pagesStreptococcus Pneumoniae Carriage, Resistance and Serotypes Among Jordanian Children From Wadi Al Seer District, JordanInternational Medical PublisherPas encore d'évaluation
- Hospital-Acquired Pneumonia in Critically Ill Children: Incidence, Risk Factors, Outcome and Diagnosis With Insight On The Novel Diagnostic Technique of Multiplex Polymerase Chain ReactionDocument7 pagesHospital-Acquired Pneumonia in Critically Ill Children: Incidence, Risk Factors, Outcome and Diagnosis With Insight On The Novel Diagnostic Technique of Multiplex Polymerase Chain ReactionadhitiaPas encore d'évaluation
- Persistence and Complex Evolution of Fluoroquinolone-Resistant Streptococcus Pneumoniae CloneDocument7 pagesPersistence and Complex Evolution of Fluoroquinolone-Resistant Streptococcus Pneumoniae CloneMark ReinhardtPas encore d'évaluation
- Endocervical Polyps in High Risk Human Papillomavirus InfectionsDocument4 pagesEndocervical Polyps in High Risk Human Papillomavirus InfectionsGLAYZA CLARITOPas encore d'évaluation
- Predictors of Urinary Tract Infection Among Febrile Children Attending at Bugando Medical Centre Northwestern, TanzaniaDocument7 pagesPredictors of Urinary Tract Infection Among Febrile Children Attending at Bugando Medical Centre Northwestern, TanzaniaInternational Medical PublisherPas encore d'évaluation
- Journal of Pediatric Sciences: Diphtheria: Is It Really OUT?Document5 pagesJournal of Pediatric Sciences: Diphtheria: Is It Really OUT?ayuPas encore d'évaluation
- Detection of Typhoid CarriersDocument6 pagesDetection of Typhoid CarriersClarestaPas encore d'évaluation
- 2 Dümichen2012Document6 pages2 Dümichen2012Sergio SampaioPas encore d'évaluation
- En 13Document8 pagesEn 13Bruna CarvalhoPas encore d'évaluation
- Typhoid JournalDocument7 pagesTyphoid JournalRegina AyediaPas encore d'évaluation
- Jurnal Kritis ICU Bundle Vap PneumoniaDocument6 pagesJurnal Kritis ICU Bundle Vap PneumoniaAdzkia PintaPas encore d'évaluation
- Ak 2011Document6 pagesAk 2011bouchra8blsPas encore d'évaluation
- Marneffei: Cytological Diagnosis of Penicillium InfectionDocument5 pagesMarneffei: Cytological Diagnosis of Penicillium InfectionAnonymous oQtve4oPas encore d'évaluation
- Bacterial Tonsillar Microbiota and Antibiogram in Recurrent TonsillitisDocument5 pagesBacterial Tonsillar Microbiota and Antibiogram in Recurrent TonsillitisResianaPutriPas encore d'évaluation
- Nosocomial Pneumonia in AdultsDocument28 pagesNosocomial Pneumonia in AdultsAndrie WigunaPas encore d'évaluation
- Antimicrobial Susceptibility Among Pathogens Isolated in Early-Versus Late-Onset Ventilator-Associated PneumoniaDocument10 pagesAntimicrobial Susceptibility Among Pathogens Isolated in Early-Versus Late-Onset Ventilator-Associated PneumoniaJeremy CPas encore d'évaluation
- Abdul CadarDocument4 pagesAbdul CadarVitta Kusma WijayaPas encore d'évaluation
- Ebn RespiDocument17 pagesEbn RespilablabkurmPas encore d'évaluation
- 6 Original CandiduriaDocument7 pages6 Original CandiduriaHarnadi WonogiriPas encore d'évaluation
- Use and Quality of Point-Of-Care Microscopy Urine Culture and Susceptibility Testing For Urinalysis in General PracticeDocument9 pagesUse and Quality of Point-Of-Care Microscopy Urine Culture and Susceptibility Testing For Urinalysis in General Practicemicrobehunter007Pas encore d'évaluation
- EwswsawnDocument5 pagesEwswsawnProbioticsAnywherePas encore d'évaluation
- TurquiaDocument8 pagesTurquiaanselmopesquisa2769Pas encore d'évaluation
- Clinical Predictors of Radiographic Abnormalities Among Infants With Bronchiolitis in A Paediatric Emergency DepartmentDocument5 pagesClinical Predictors of Radiographic Abnormalities Among Infants With Bronchiolitis in A Paediatric Emergency Departmentnavali rahmaPas encore d'évaluation
- Typhoid Immunization Strategy for Children in PakistanDocument24 pagesTyphoid Immunization Strategy for Children in Pakistanmoon1312Pas encore d'évaluation
- Comparative Study of Levofloxacin and Amoxycillin/clavulanic Acid in Adults With Mild-To-Moderate Community-AcquiredDocument9 pagesComparative Study of Levofloxacin and Amoxycillin/clavulanic Acid in Adults With Mild-To-Moderate Community-Acquiredjuloc34Pas encore d'évaluation
- VAP Diagnosis 2009Document8 pagesVAP Diagnosis 2009Illham Setiawan SulistioPas encore d'évaluation
- Pediatric Tuberculous Pleural EffusionDocument5 pagesPediatric Tuberculous Pleural EffusionAnnisa SasaPas encore d'évaluation
- Hipertensi PBLDocument41 pagesHipertensi PBLAl MuzakkiPas encore d'évaluation
- Daftar PustakaDocument2 pagesDaftar PustakaAl MuzakkiPas encore d'évaluation
- Kul. Gagal JantungDocument28 pagesKul. Gagal JantungAl MuzakkiPas encore d'évaluation
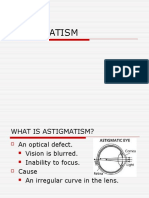
- ASTIGMATISM (Lucas Vigneaux) FinalDocument11 pagesASTIGMATISM (Lucas Vigneaux) FinalAl MuzakkiPas encore d'évaluation
- Paliatif CareDocument13 pagesPaliatif CareAl MuzakkiPas encore d'évaluation
- Unlock-Induction ANSE10 WMDocument8 pagesUnlock-Induction ANSE10 WMAl MuzakkiPas encore d'évaluation
- Jijin 140725134811 Phpapp01Document52 pagesJijin 140725134811 Phpapp01Al MuzakkiPas encore d'évaluation
- TSWJ2014 270120Document6 pagesTSWJ2014 270120Al MuzakkiPas encore d'évaluation
- Journal Rockey MountainDocument4 pagesJournal Rockey MountainAl MuzakkiPas encore d'évaluation
- Activate Win8 Via KMS (WORKING!) (12!12!2012) (UPDATED+SUPPORT) (ProWMC Permanent Activation Added) - Windows 8 - 7pm TechDocument9 pagesActivate Win8 Via KMS (WORKING!) (12!12!2012) (UPDATED+SUPPORT) (ProWMC Permanent Activation Added) - Windows 8 - 7pm TechAl MuzakkiPas encore d'évaluation
- Clin Gui EncephalitisDocument9 pagesClin Gui EncephalitisAl MuzakkiPas encore d'évaluation
- AktifasiDocument1 pageAktifasiAl MuzakkiPas encore d'évaluation
- Enable .NET Framework 3.... Iew To Run ApplicationsDocument12 pagesEnable .NET Framework 3.... Iew To Run ApplicationsAl MuzakkiPas encore d'évaluation
- Patient Risk Factors Best Practices SsiDocument9 pagesPatient Risk Factors Best Practices SsiAl MuzakkiPas encore d'évaluation
- Activate Win8 Via KMS (WORKING!) (12!12!2012) (UPDATED+SUPPORT) (ProWMC Permanent Activation Added) - Windows 8 - 7pm TechDocument9 pagesActivate Win8 Via KMS (WORKING!) (12!12!2012) (UPDATED+SUPPORT) (ProWMC Permanent Activation Added) - Windows 8 - 7pm TechAl MuzakkiPas encore d'évaluation
- JADWAL OPERASI INSTALASI BEDAH SENTRAL RSUD dr. ZAINOEL ABIDIN BANDA ACEHDocument27 pagesJADWAL OPERASI INSTALASI BEDAH SENTRAL RSUD dr. ZAINOEL ABIDIN BANDA ACEHAl MuzakkiPas encore d'évaluation
- Activate Win8 Via KMS (WORKING!) (12!12!2012) (UPDATED+SUPPORT) (ProWMC Permanent Activation Added) - Windows 8 - 7pm TechDocument9 pagesActivate Win8 Via KMS (WORKING!) (12!12!2012) (UPDATED+SUPPORT) (ProWMC Permanent Activation Added) - Windows 8 - 7pm TechAl MuzakkiPas encore d'évaluation
- CDC - Ventilator-Associated Pneumonia (VAP) EventDocument13 pagesCDC - Ventilator-Associated Pneumonia (VAP) EventAl MuzakkiPas encore d'évaluation
- SuisseMed Company ProfileDocument60 pagesSuisseMed Company ProfileCarepro AsiaPas encore d'évaluation
- Test Bank For Understanding The Essentials of Critical Care Nursing 2nd Edition Kathleen Ouimet Perrin Carrie Edgerly MacleodDocument9 pagesTest Bank For Understanding The Essentials of Critical Care Nursing 2nd Edition Kathleen Ouimet Perrin Carrie Edgerly MacleodFelix Guy100% (26)
- Medical Vocabulary: Part of Speech AdjDocument11 pagesMedical Vocabulary: Part of Speech Adjhisamol956Pas encore d'évaluation
- Algorithm For COVID19 Referral and TriageDocument1 pageAlgorithm For COVID19 Referral and Triagejeffrey ordonezPas encore d'évaluation
- Empanelment On 19.10Document8 pagesEmpanelment On 19.10api-3832244100% (1)
- Mind Invaders - Dave HuntDocument331 pagesMind Invaders - Dave Huntinfomih70100% (2)
- Pressure Ulcer Assessment and Treatment (PDFDrive)Document88 pagesPressure Ulcer Assessment and Treatment (PDFDrive)Amna AliPas encore d'évaluation
- ICU Prophylaxis ChecklistDocument41 pagesICU Prophylaxis ChecklistBharti NaraPas encore d'évaluation
- CS HF Directory 2018 Print PDFDocument80 pagesCS HF Directory 2018 Print PDFAt Day's WardPas encore d'évaluation
- Urinary Tract Infections 2021 UpdateDocument14 pagesUrinary Tract Infections 2021 UpdateSandy GaresPas encore d'évaluation
- 7.2post Resus Algorithms 1Document1 page7.2post Resus Algorithms 1Massimo Di BenedettoPas encore d'évaluation
- Procalcitonin Guided Antibiotic TherapyDocument20 pagesProcalcitonin Guided Antibiotic TherapyhziglamPas encore d'évaluation
- Sample: Reading Sub-Test - Question Paper: Parts B & CDocument16 pagesSample: Reading Sub-Test - Question Paper: Parts B & CSajana Thulung100% (1)
- Gandaki Medical College: Teaching Hospital & Research Centre Pvt. LTDDocument2 pagesGandaki Medical College: Teaching Hospital & Research Centre Pvt. LTDSushant AcharyaPas encore d'évaluation
- Critical care patients' psychosocial problemsDocument5 pagesCritical care patients' psychosocial problemsSaif Ahmed jubarPas encore d'évaluation
- PICU NICU OrientationDocument8 pagesPICU NICU OrientationSony PrabowoPas encore d'évaluation
- ProspectusDocument64 pagesProspectusIMRANPas encore d'évaluation
- ABC Hospital OverviewDocument12 pagesABC Hospital OverviewKrishna100% (1)
- Policy - Document LIC TusharDocument54 pagesPolicy - Document LIC Tusharwaghtushar1212Pas encore d'évaluation
- Vol 4 DBR EPC AIIMS GKPR - 21.01.2018Document234 pagesVol 4 DBR EPC AIIMS GKPR - 21.01.2018Shyam SinghPas encore d'évaluation
- Evaluation of Antimicrobial Activity of a Natural Fogging SolutionDocument16 pagesEvaluation of Antimicrobial Activity of a Natural Fogging SolutionednisoPas encore d'évaluation
- Musallam 2018Document7 pagesMusallam 2018Koup NuPas encore d'évaluation
- Trauma TriageDocument34 pagesTrauma TriageMonica FalconePas encore d'évaluation
- Covid-19 Supporting Nurses' Psychological and Mental HealthDocument10 pagesCovid-19 Supporting Nurses' Psychological and Mental HealthIka JuitaPas encore d'évaluation
- ResumeDocument3 pagesResumeapi-383804230Pas encore d'évaluation
- Close, OpenDocument7 pagesClose, OpenNoeRhul M-lhati OelfhaPas encore d'évaluation
- VAP Prevention StrategiesDocument6 pagesVAP Prevention StrategiesCGKN BanyuwangiPas encore d'évaluation
- Rajiv Gandhi University of Health Sciences, Bangalore, KarnatakaDocument17 pagesRajiv Gandhi University of Health Sciences, Bangalore, KarnatakayashramawatPas encore d'évaluation
- 22PG MATH-plus-Rationale-Journal-of-Intensive-Care-Medicine-Dec2020Document22 pages22PG MATH-plus-Rationale-Journal-of-Intensive-Care-Medicine-Dec2020Barbara RowePas encore d'évaluation
- Nursing Students Experiences in Critical Care Course A Qualitative StudyDocument7 pagesNursing Students Experiences in Critical Care Course A Qualitative StudyEkoArsetyantoPas encore d'évaluation