Académique Documents
Professionnel Documents
Culture Documents
Hyperglycaemia and Adverse Pregnancy Outcome (HAPO) Study: Associations With Maternal Body Mass Index
Transféré par
dr.vidhyaTitre original
Copyright
Formats disponibles
Partager ce document
Partager ou intégrer le document
Avez-vous trouvé ce document utile ?
Ce contenu est-il inapproprié ?
Signaler ce documentDroits d'auteur :
Formats disponibles
Hyperglycaemia and Adverse Pregnancy Outcome (HAPO) Study: Associations With Maternal Body Mass Index
Transféré par
dr.vidhyaDroits d'auteur :
Formats disponibles
DOI: 10.1111/j.1471-0528.2009.02486.x www.bjog.
org
Epidemiology
Hyperglycaemia and Adverse Pregnancy Outcome (HAPO) Study: associations with maternal body mass index
HAPO Study Cooperative Research Group*
Correspondence: Dr BE Metzger, Northwestern University Feinberg School of Medicine, Endocrinology, 645 North Michigan Avenue, Suite 530-22, Chicago, IL 60611, USA. Email: bem@northwestern.edu Accepted 6 December 2009. Published Online 20 January 2010.
Objective To determine whether higher maternal body mass index
(BMI), independent of maternal glycaemia, is associated with adverse pregnancy outcomes.
Design Observational cohort study. Setting Fifteen centres in nine countries. Population Eligible pregnant women. Methods A 75-g 2-hour oral glucose tolerance test (OGTT) was
delivery (before 37 weeks) and percentage of body fat >90th percentile.
Results Among 23 316 blinded participants, with control for maternal glycaemia and other potential confounders, higher maternal BMI was associated (odds ratio [95% condence interval] for highest {42.0 kg/m2} versus lowest {<22.6 kg/m2} BMI categories) with increased frequency of birthweight >90th percentile (3.52 [2.485.00]) and percentage of body fat >90th percentile (3.28 [2.284.71]), caesarean section (2.23 [1.662.99]), cord C-peptide >90th percentile (2.33 [1.583.43]) and preeclampsia (14.14 [9.4421.17]). Preterm delivery was less frequent with higher BMI (0.48 [0.310.74]). Associations with fetal size tended to plateau in the highest maternal BMI categories. Conclusion Higher maternal BMI, independent of maternal
performed between 24 and 32 weeks of gestation in all participants. Maternal BMI was calculated from height and weight measured at the OGTT. Fetal adiposity was assessed using skinfold measurements and percentage of body fat was calculated. Associations between maternal BMI and pregnancy outcomes were assessed using multiple logistic regression analyses, with adjustment for potential confounders.
Main outcome measures Predened primary outcomes were
birthweight >90th percentile, primary caesarean section, clinical neonatal hypoglycaemia and cord serum C-peptide >90th percentile. Secondary outcomes included pre-eclampsia, preterm
glycaemia, is strongly associated with increased frequency of pregnancy complications, in particular those related to excess fetal growth and adiposity and to pre-eclampsia.
Keywords Birthweight, body mass index, fetal hyperinsulinism,
hyperglycaemia, large for gestational age.
Please cite this paper as: HAPO Study Cooperative Research Group. Hyperglycaemia and Adverse Pregnancy Outcome (HAPO) Study: associations with maternal body mass index. BJOG 2010;117:575584.
Introduction
Maternal overweight and obesity are associated with increased risks of adverse pregnancy outcomes, in particular maternal complications such as hypertensive disorders of pregnancy,1 gestational diabetes24 and maternal mortality.5 Fetal or neonatal complications including stillbirth,6 birth defects,7 macrosomia3,8 and shoulder dystocia9 also occur more frequently in babies born to obese women but ndings are more variable for other putative complica*For full list of authors please refer to the Supporting information.
tions such as preterm delivery2,3,10 and early neonatal death.9,10 Obesity is also associated with an increased risk of diabetes both during and outside pregnancy. Previous reports do not allow a clear separation of the relative importance of obesity per se and hyperglycaemia as contributors to increased risks of adverse pregnancy complications because of unavoidable methodological weaknesses. In some reports routine screening for hyperglycaemia was not undertaken,2,3 whereas in others the approach to screening was not outlined.2 In studies which explicitly report glucose screening of the entire cohort, detailed analyses of the
2010 The Authors Journal compilation RCOG 2010 BJOG An International Journal of Obstetrics and Gynaecology
575
McIntyre et al.
prevalence of gestational diabetes in overweight and obese women were not reported.11,12 Furthermore, in none of the previous studies were glucose results blinded from women or their caregivers. This may have inuenced both clinical decision-making and ascertainment of pregnancy outcomes. The Hyperglycemia and Adverse Pregnancy Outcome (HAPO) study was designed primarily to assess the effects of mild hyperglycaemia on pregnancy outcomes.13,14 Glucose results were blinded from women and caregivers, except where results fell outside predetermined ranges.14 The HAPO study previously demonstrated relationships between fasting and postload glucose concentrations measured during a third-trimester 75-g oral glucose tolerance test (OGTT) and pregnancy outcomes, including fetal size, adiposity and hyperinsulinism. These were only modestly attenuated after correction for other factors, including maternal body mass index (BMI).14,15 For the current analysis, our hypothesis was that higher maternal BMI is associated with adverse pregnancy outcomes and neonatal adiposity independent of other factors, including maternal glycaemia.
mined from an ultrasound performed between 6 and 24 weeks of gestation. Final expected date of delivery was also determined from ultrasound if: (1) gestational dating from last menstrual period differed from ultrasound dating by more than 5 days, when the ultrasound was performed between 6 and 13 weeks, or (2) if dating differed by more than 10 days when the ultrasound was performed between 14 and 24 weeks.
Oral glucose tolerance test
All participants underwent a standard 75-g OGTT between 24 and 32 weeks of gestation (as close to 28 weeks as possible). Blood pressure was measured at the OGTT visit using standardised procedures and calibrated equipment. Data concerning smoking and alcohol use, rst-degree family history of diabetes and hypertension and demographic data were collected using standardised questionnaires. Race/ethnicity was self-identied by participants. A sample for random plasma glucose was collected at 3437 weeks of gestation as a safety measure to identify cases with hyperglycaemia above a predened threshold.
Glucose analysis and unblinding
Methods
The HAPO study was an international, multicentre epidemiological study conducted at 15 centres in nine countries. Methods have been reported elsewhere.13,14 The study was approved by the local institutional review board at each centre. All participants gave written informed consent and the study was overseen by an external Data Monitoring Committee.
Participants
All pregnant women at each centre were eligible to participate unless they had one or more exclusion criteria: age <18 years, planning to deliver at another hospital, date of last menstrual period not certain and no ultrasound estimation from 6 to 24 weeks of gestation available, unable to complete the OGTT by 32 weeks of gestation, multiple pregnancy, conception using gonadotrophin ovulation induction or by in vitro fertilisation, glucose testing before recruitment or a diagnosis of diabetes during this pregnancy, diabetes antedating pregnancy requiring treatment with medication, participation in another study which may interfere with HAPO, known to be human immunodeciency virus-positive or to have hepatitis B or C virus infection, before participation in HAPO, or inability to converse in the languages used in eld centre forms without the aid of an interpreter.13 Gestational age and expected date of delivery were determined from the date of the last menstrual period, if the participant was certain of her dates. If uncertain, expected date of delivery was deter-
Aliquots of fasting and 2-hour OGTT and random plasma glucose samples were analysed at eld centre laboratories. Values were unblinded if fasting plasma glucose exceeded 5.8 mmol/l, if 2-hour OGTT plasma glucose exceeded 11.1 mmol/l, if random plasma glucose was 8.9 mmol/l or if any plasma glucose value was <2.5 mmol/l. Otherwise, women, caregivers and HAPO Study staff (except laboratory personnel) remained blinded to glucose values. To avoid the confounding effects of centre-to-centre analytical variation, aliquots of all OGTT specimens were analysed at the HAPO Central Laboratory and those results are used here. Only women whose results remained blinded, with no additional glucose testing outside the HAPO protocol, are included in these analyses.
Maternal height and weight
The primary objective measurements of maternal height and weight, used to calculate BMI in this report, were obtained at the OGTT visit. Height was measured twice to the nearest 0.5 cm with a stadiometer or wall-mounted measuring tape with shoes removed and the participants head facing forward in the horizontal plane. If the results differed by more than 1.0 cm, the measurements were repeated. Weight was measured twice to the nearest 0.1 kg on a scale calibrated each day with a 10-kg weight. Outer garments and shoes were removed and a third weight measurement was taken if the results of the rst two measurements differed by more than 0.5 kg. Recalled maternal pre-pregnancy weight was also recorded, but is not the primary focus of this report because of its inherent
576
2010 The Authors Journal compilation RCOG 2010 BJOG An International Journal of Obstetrics and Gynaecology
HAPO BMI and perinatal outcomes
subjectivity and the absence of data for 1966 participants (8.4%). No centre provided specic interventions to participants based on weight or BMI.
Prenatal care and delivery
Prenatal care and timing of delivery were determined by standard eld centre practice. No eld centre arbitrarily delivered babies before full term or routinely performed caesarean delivery at a specied maternal or gestational age.
Neonatal care and anthropometrics
After delivery, infants received customary routine care. Neonatal anthropometrics were obtained within 72 hours of delivery and included weight, length and skinfold thickness at three sites (ank, subscapular, triceps). Measurement and quality control procedures have been described elsewhere.15 Medical records were abstracted to obtain data regarding maternal and newborn course.
Primary and secondary outcomes
The four prespecied primary outcomes were birthweight above the 90th percentile for gestational age, primary caesarean delivery, clinical neonatal hypoglycaemia and cord serum C-peptide above the 90th percentile (fetal hyperinsulinaemia). Secondary outcomes were preterm delivery (before 37 weeks of gestation), shoulder dystocia or birth injury, need for more intensive neonatal care, hyperbilirubinaemia and pre-eclampsia. The 90th percentiles for gestational age (3044 weeks only) were determined using quantile regression analyses for each of eight newborn genderethnic groups (Caucasian or Other, Black people, Hispanic, Asian), with adjustment for gestational age, eld centre and parity (0, 1, 2+). A newborn was considered to have a birthweight >90th percentile if the birthweight was greater than the estimated 90th percentile for the babys gender, gestational age, ethnicity, eld centre and maternal parity. Otherwise, the newborn was considered to have a birthweight 90th percentile.
Neonatal adiposity
Additional measures of neonatal adiposity included percentage of body fat >90th percentile and sum of skinfolds >90th percentile for gestational age. Fat mass was calculated from birthweight, length and ank skinfold using an equation derived from measurements of total body electrical conductivity.16 The percentage of body fat was calculated as 100 fat mass/birthweight.
continuous variable in multiple logistic regression analyses. For categorical analyses, maternal BMI was divided into six categories. Category limits were chosen to match the recommended pre-pregnancy BMI categories of <18.5 (underweight), 18.524.9 (normal range), 25.029.9 (overweight), 30.034.9 (obese class I), 35.039.9 (obese class II) and 40.0 (obese class III).17 The comparable category limits for BMI at the OGTT were obtained from a regression of OGTT BMI on pre-pregnancy BMI and gestational age at the OGTT, and yielded the following categories at 28 weeks of gestation: <22.6, 22.628.4, 28.532.9, 33.0 37.4, 37.541.9, 42.0. To assess whether or not the log of the odds of each outcome was linearly related to BMI, we added squared terms for BMI for each outcome to assess whether there were signicant quadratic associations (see below). For each outcome, two logistic models (I and II) were t. Model I included adjustment for centre or for the variables used in estimating the 90th percentiles for birthweight, percentage of fat and sum of skinfolds for gestational age (gender, ethnicity, centre and parity). In addition, Model I included adjustment for multiple potential confounders, including age, height, smoking, alcohol use, family history of diabetes, gestational age at the OGTT, babys gender, parity (0, 1, 2+) (except primary caesarean delivery), and hospitalisation before delivery (except pre-eclampsia), and family history of hypertension and maternal urinary tract infection (pre-eclampsia only). Model II added fasting glucose and mean arterial pressure to Model I, because of the potential for these variables, with their known associations with BMI, to be in the causal pathway of the associations of BMI with outcomes. Squared terms for age, fasting glucose and mean arterial pressure were prescreened for possible inclusion in models that included only centre; that is without BMI or other covariates; these terms were included in Model I and/or II when statistically signicant (see below). Squared terms for glucose, age, BMI and mean arterial pressure were considered statistically signicant for P 0.001 for all outcomes, except neonatal hypoglycaemia and shoulder dystocia/birth injury, where P 0.05 was used because of the smaller numbers of babies with these outcomes. Because the squared term for BMI was statistically signicant for several of the outcomes indicating nonlinear associations, only the categorical results are reported here. All analyses were conducted in sas version 9.1 (SAS Institute Inc., Cary, NC, USA) or Stata 10.0 (StataCorp, College Station, TX, USA). All reported P-values are twosided and were not adjusted for multiple testing.
Statistical analyses
Descriptive statistics include mean and standard deviation for continuous variables and numbers and percentages for categorical variables. For associations of maternal BMI with outcomes BMI was considered as both a categorical and
Results
Table 1 shows the characteristics of mothers and babies in the HAPO study and the overall frequencies of some
2010 The Authors Journal compilation RCOG 2010 BJOG An International Journal of Obstetrics and Gynaecology
577
McIntyre et al.
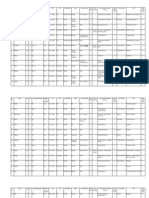
Table 1. Characteristics of hyperglycemia and adverse pregnancy outcome (HAPO) study participants and frequency of outcomes Maternal characteristics Age (years) Pre-pregnancy body mass index (kg/m2) (self-reported weight) Body mass index (kg/m2)* Mean arterial pressure (mmHg)* Fasting plasma glucose (mmol/l)*,** 1-hour plasma glucose (mmol/l)*,** 2-hour plasma glucose (mmol/l)*,** Gestational age (weeks)* N 23 316 21 324 23 316 23 316 23 316 23, 316 23 316 23 316 N 1581 1612 5282 12 233 1655 3271 N 23 23 22 19 12 316 267 601 322 003 N Mean 39.4 3,292 49.7 11.3 51.5 % Mean 29.2 23.9 27.7 80.9 4.5 7.5 6.2 27.8 % 6.8 6.9 22.7 52.5 7.1 14.0 SD 1.7 529 2.4 3.7 SD 5.8 5.0 5.1 8.3 0.4 1.7 1.3 1.8
Prenatal smoking (any) Prenatal alcohol use (any) Family history of diabetes Parity (prior delivery 20 weeks) Prenatal urinary tract infection Hospitalisation prior to delivery Newborn characteristics Gestational age (weeks) Birthweight (g) Length (cm) Body fat (%) Sex (male) Obstetric outcomes Caesarean section delivery Primary Repeat Hypertension Chronic hypertension Gestational hypertension Pre-eclampsia
pre-pregnancy weight, the corresponding mean pre-pregnant BMI was 23.9 kg/m2 and the correlation with the BMI at the OGTT visit was 0.918. The mean (SD) difference in BMI from pre-pregnancy to 28 weeks of gestation was +3.6 (2.0) kg/m2, varying from +3.9 (1.6) in those with prepregnancy BMI <18.5 kg/m2 to +1.7 (2.9) in those with pre-pregnancy BMI 35.0 kg/m2. The eld-centre-adjusted correlations of BMI at the OGTT with fasting, 1-hour and 2-hour glucose were 0.312, 0.197 and 0.154, respectively. The effects of including maternal 1-hour and 2-hour glucose results, in addition to fasting glucose in Model II adjustments, were examined for all outcomes reported here. These further adjustments resulted in little change in any of the odds ratios. Hence, we present the results with adjustment for fasting glucose alone.
Maternal BMI and primary outcomes
The relationships between maternal BMI at the OGTT and the prespecied primary outcomes are presented in Table 2. The frequency of birthweight >90th percentile was greater with higher maternal BMI with some reduction in the incremental effects seen in the highest BMI categories. Even after full Model II adjustments, the odds ratios for the four highest BMI categories were all >3.0 The frequency of primary caesarean section was also greater with higher BMI with an odds ratio of approximately 2.5 or greater for the two highest BMI categories after Model I adjustment. With additional adjustment for fasting glucose and mean arterial pressure, these two odds ratios were somewhat attenuated. The frequency of clinical neonatal hypoglycaemia showed some tendency to rise with higher maternal BMI, but none of the odds ratios were signicantly different from 1.0 when fully adjusted in Model II. Neonatal hyperinsulinaemia, measured by cord C-peptide >90th percentile, was also positively associated with maternal BMI with odds ratios over 3.0 in the highest three categories in Model I. These odds ratios were attenuated in Model II, but were still 1.9.
3731 1792 582 1370 1116
16.0 7.7 2.5 5.9 4.8
*Measured at the OGTT visit. **For glucose to mg/dl, multiply by 18. Babies with gestational age 3644 weeks at birth. Hypertension present before 20 weeks which did not progress to pre-eclampsia was classied as chronic hypertension. After 20 weeks of gestation, hypertension disorders in pregnancy were categorised according to International Society for the Study of Hypertension (ISSHP) guidelines.31 Pre-eclampsia, systolic blood pressure (BP) 140 mmHg and/or diastolic BP 90 mmHg on two or more occasions a minimum of 6 hours apart and proteinuria of 1+ dipstick or 300 mg/24 hours. If the criteria for elevated BP but not proteinuria were met, this was classied as gestational hypertension.
Maternal BMI and secondary outcomes
Table 3 shows the relationships between maternal BMI and the prespecied secondary outcomes. The frequency of preterm delivery was signicantly lower with higher maternal BMI in Model II. Pre-eclampsia was present in only 11.7% of cases of preterm delivery. Shoulder dystocia and birth injury were much less common events (overall frequency 1.3%). Their frequency was signicantly higher than in the referent group for maternal BMI categories spanning the range from 28.5 to 37.4, both in Model I and Model II, but was not signicantly increased in the highest two BMI categories, in part because of the small number of events in these two categories.
obstetric outcomes. (More detailed information is presented in a previous publication14) The mean age of participants was 29.2 years, and the mean maternal BMI at the OGTT was 27.7 kg/m2. For the 21 350 participants with a recalled
578
2010 The Authors Journal compilation RCOG 2010 BJOG An International Journal of Obstetrics and Gynaecology
HAPO BMI and perinatal outcomes
Table 2. Relationship between maternal body mass index (BMI) at the oral glucose tolerance test (OGTT) and primary outcomes BMI (kg/m2) N # % Model I OR 95% CI Model II OR 95% CI
Birthweight >90th percentile*,** <22.6 2974 115 22.628.4 11 934 981 28.532.9 5127 644 33.037.4 2064 308 37.541.9 735 112 42.0 383 61 Total 23 217 2221 Primary caesarean section <22.6 2809 356 22.628.4 10 868 1814 28.532.9 4438 916 33.037.4 1707 404 37.541.9 609 152 42.0 301 89 Total 20 732 3731 Clinical neonatal hypoglycaemia, <22.6 2978 75 22.628.4 11 938 225 28.532.9 5123 99 33.037.4 2068 50 37.541.9 737 18 42.0 383 13 Total 23 227 480 Cord serum C-peptide >90th percentile, <22.6 2633 123 22.628.4 10 317 731 28.532.9 4355 448 33.037.4 1683 232 37.541.9 599 83 42.0 298 54 Total 19 885 1671
3.9 8.2 12.6 14.9 15.2 15.9 9.6 12.7 16.7 20.6 23.7 25.0 29.6 18.0 2.5 1.9 1.9 2.4 2.4 3.4 2.1 4.7 7.1 10.3 13.8 13.9 18.1 8.4
1.00 2.24 3.62 4.43 4.52 4.55
1.842.74 2.954.45 3.545.55 3.435.96 3.256.36
1.00 2.17 3.31 3.89 3.80 3.52
1.782.65 2.684.10 3.074.93 2.845.08 2.485.00
1.00 1.27 1.78 2.26 2.46 3.20
1.121.44 1.542.04 1.912.67 1.963.07 2.414.25
1.00 1.17 1.48 1.75 1.78 2.23
1.031.33 1.281.71 1.472.08 1.412.25 1.662.99
1.00 0.81 0.89 1.08 1.19 1.74
0.621.07 0.641.22 0.741.58 0.692.04 0.933.26
1.00 0.76 0.73 0.82 0.82 1.11
0.581.01 0.521.03 0.541.23 0.471.45 0.582.15
1.00 1.46 2.18 3.11 3.04 4.30
1.191.79 1.752.71 2.443.97 2.234.15 2.986.20
1.00 1.29 1.66 2.13 1.90 2.33
1.051.58 1.322.08 1.652.75 1.372.63 1.583.43
N, total number in the BMI category; #, number in the BMI category with the outcome; %, proportion in the BMI with the outcome. BMI category limits at the OGTT were chosen to match the recommended pre-pregnancy categories of <18.5 (underweight), 18.524.9 (normal range), 25.029.9 (overweight), 30.034.9 (obese class I), 35.039.9 (obese class II), and 40.0 (obese class III). *Ninetieth percentiles for gestational age (3044 weeks only) were determined using quantile regression analyses for each of eight newborn genderethnic groups (Caucasian or Other, Black people, Hispanic, Asian), with adjustment for gestational age, eld centre and parity (0, 1, 2 +). A newborn was considered to have a birthweight >90th percentile if the birthweight was greater than the estimated 90th percentile for the babys gender, gestational age, ethnicity, eld centre, and maternal parity. Otherwise, the newborn was considered to have a birthweight 90th percentile. **Model I: Adjusted for the variables used in estimating 90th percentiles, age, height and gestational age at the OGTT, smoking, alcohol use, hospitalisation before delivery, any family history of diabetes. Model II: Model I adjustment + fasting plasma glucose and mean arterial pressure. Model I: Adjusted for eld centre, age, gender, smoking, alcohol use, hospitalisation before delivery, any family history of diabetes, gestational age and maternal height at the OGTT. Model II: Model I adjustment + fasting plasma glucose and mean arterial pressure. Clinical neonatal hypoglycaemia was dened as present if there was notation of neonatal hypoglycaemia in the medical record and there were symptoms and/or treatment with a glucose infusion or a local laboratory report of a glucose value 1.7 mmol/l in the rst 24 hours and/or 2.5 mmol/l after the rst 24 hours after birth. Same Models as for primary caesarean delivery except parity was added. 90th percentile of the values for the total HAPO sample. Same Models as for primary caesarean delivery except that parity and cord glucose were added.
The associations of maternal BMI with neonatal hyperbilirubinaemia and intensive neonatal care were positive in Model I. Few categories showed signicant associations for these outcomes after Model II adjustment.
The frequency of pre-eclampsia showed a strong linear relationship with increasing maternal BMI. Women in the highest BMI category had an odds ratio >18.0 for pre-eclampsia, which was somewhat attenu-
2010 The Authors Journal compilation RCOG 2010 BJOG An International Journal of Obstetrics and Gynaecology
579
McIntyre et al.
Table 3. Relationship between maternal body mass index (BMI) at the oral glucose tolerance test (OGTT) and secondary outcomes BMI (kg/m2)* N # % Model I OR 95% CI Model II OR 95% CI
Preterm delivery (<37 weeks)* <22.6 2989 22.628.4 11 986 28.532.9 5143 33.037.4 2075 37.541.9 739 42.0 384 Total 23 316 Shoulder dystocia/birth injury* <22.6 2978 22.628.4 11 938 28.532.9 5123 33.037.4 2068 37.541.9 737 42.0 383 Total 23 227 Hyperbilirubinaemia*,** <22.6 2978 22.628.4 11 938 28.532.9 5123 33.037.4 2068 37.541.9 737 42.0 383 Total 23 227 Intensive neonatal care*, <22.6 2978 22.628.4 11 938 28.532.9 5123 33.037.4 2068 37.541.9 737 42.0 383 Total 23 227 Pre-eclampsia <22.6 2893 22.628.4 11 289 28.532.9 4574 33.037.4 1739 37.541.9 596 42.0 273 Total 21 364
251 768 366 127 67 29 1608 21 145 87 40 11 7 311 286 1033 372 150 61 28 1930 268 924 373 175 81 34 1855 58 368 293 197 119 81 1116
8.4 6.4 7.1 6.1 9.1 7.6 6.9 0.7 1.2 1.7 1.9 1.5 1.8 1.3 9.6 8.7 7.3 7.3 8.3 7.3 8.3 9.0 7.7 7.3 8.5 11.0 8.9 8.0 2.0 3.3 6.4 11.3 20.0 29.7 5.2
1.00 0.79 0.88 0.73 1.13 0.88
0.680.92 0.741.05 0.580.92 0.841.51 0.581.33
1.00 0.72 0.69 0.50 0.70 0.48
0.620.84 0.570.83 0.390.64 0.510.95 0.310.74
1.00 1.51 1.95 2.09 1.51 1.72
0.952.42 1.193.21 1.203.62 0.713.21 0.714.16
1.00 1.52 1.96 2.09 1.50 1.67
0.952.43 1.183.28 1.173.73 0.693.28 0.674.16
1.00 1.09 1.21 1.30 1.62 1.49
0.941.26 1.021.44 1.041.62 1.202.20 0.982.26
1.00 1.06 1.09 1.10 1.32 1.15
0.911.23 0.911.31 0.881.39 0.961.80 0.751.77
1.00 1.09 1.24 1.43 1.98 1.51
0.941.27 1.041.49 1.161.78 1.492.61 1.022.23
1.00 1.07 1.13 1.22 1.61 1.15
0.911.25 0.931.36 0.971.53 1.202.15 0.771.73
1.00 1.66 3.25 6.01 11.13 18.77
1.252.21 2.414.37 4.398.22 7.8615.76 12.6727.81
1.00 1.56 2.85 5.01 8.92 14.14
1.172.08 2.113.85 3.646.89 6.2512.73 9.4421.17
N, total number in the BMI category; #, number in the BMI category with the outcome; %, proportion in the BMI with the outcome. BMI category limits at the OGTT were chosen to match the recommended pre-pregnancy categories of <18.5 (underweight), 18.524.9 (normal range), 25.029.9 (overweight), 30.034.9 (obese class I), 35.039.9 (obese class II), and 40.0 (obese class III). *Model I: Adjusted for eld centre, age, gender, parity, smoking, alcohol use, hospitalisation before delivery, any family history of diabetes, gestational age and maternal height at the OGTT. Model II: Model I adjustment + fasting plasma glucose and mean arterial pressure. **Hyperbilirubinaemia was dened by treatment with phototherapy after birth, at least one laboratory report of a bilirubin level of 342 lmol/l or more, or readmission for hyperbilirubinaemia. Intensive neonatal care was dened as admission to any type of unit for care more intensive than normal newborn care and lasting more than 24 hours or as death of the baby or transfer to another hospital. Data were excluded for admissions that were only for possible sepsis and sepsis was ruled out, observation, or feeding problems. Model I deleted hospitalisation before delivery and added maternal urinary tract infection and family history of hypertension. Model II deleted mean arterial pressure.
580
2010 The Authors Journal compilation RCOG 2010 BJOG An International Journal of Obstetrics and Gynaecology
HAPO BMI and perinatal outcomes
ated by Model II adjustment but was still greater than 14.0.
Neonatal adiposity
Consistent with the primary outcome of birthweight >90th percentile, both percentage of body fat and sum of skinfolds >90th percentile were more frequent with higher maternal BMI (Table 4). This conrms that these babies were not only large, but that they also had increased fat deposits. As seen for birthweight >90th percentile, odds ratios are somewhat attenuated in the highest BMI categories with Model II adjustment.
Other outcomes
There was no relationship between maternal BMI and the occurrence of major congenital malformations or perinatal mortality, either in unadjusted or adjusted analyses.
Discussion
In conjunction with the results of the primary analysis of the HAPO study,14 this report demonstrates that both maternal BMI and glycaemia have strong, independent associations with a range of clinically important pregnancy outcomes. Neither the participants glycaemic status nor her BMI was a target for active therapy in the HAPO
cohort, removing a major source of potential confounding that was present in previous reports. Parental size and infant birthweight are related through genetic and environmental mechanisms, with the stronger relationship between maternal and fetal size believed to represent contributions of the intrauterine environment.18 Our results demonstrate that increasing maternal BMI contributes to this effect independently of variations in glycaemic exposure. In addition to the strong relationship with birthweight >90th percentile, maternal BMI was also strongly related to fetal adiposity and hyperinsulinaemia, even after adjustment for maternal glycaemia. This highlights the potential importance of other nutrients including triglycerides, free fatty acids and amino acids19 and potentially of total caloric intake. Fetal beta cells may have been programmed to increase insulin secretion much earlier in pregnancy before the OGTT.20 Other factors associated with maternal obesity, such as altered concentrations of adipocytokines and other inammatory markers and changes in physical activity, may also play a role in determining fetal size and adiposity.21 Associations with fetal growth tended to plateau at the highest levels of maternal BMI, suggesting that a maximal inuence is present before the mothers BMI is categorised as class II or III obesity or that other factors limiting growth (e.g. increased frequency of pre-eclampsia) come
Table 4. Relationship between maternal body mass index (BMI) at the oral glucose tolerance test (OGTT) and neonatal adiposity BMI (kg/m2) N # % Model I OR 95% CI Model II OR 95% CI
Per cent body fat >90th percentile* <22.6 2513 113 22.628.4 9962 817 28.532.9 4230 544 33.037.4 1701 258 37.541.9 604 104 42.0 317 56 Total 19 327 1892 Sum of skinfolds >90th percentile* <22.6 2515 113 22.628.4 9978 814 28.532.9 4256 531 33.037.4 1714 268 37.541.9 607 84 42.0 319 53 Total 19 389 1863
4.5 8.2 12.9 15.2 17.2 17.7 9.8 4.5 8.2 12.5 15.6 13.8 16.6 9.6
1.00 1.91 3.15 3.82 4.45 4.48
1.562.34 2.553.88 3.034.82 3.345.91 3.176.34
1.00 1.81 2.77 3.19 3.51 3.28
1.482.23 2.223.44 2.504.08 2.614.74 2.284.71
1.00 1.84 2.93 3.83 3.33 4.06
1.512.26 2.383.62 3.044.83 2.474.49 2.865.77
1.00 1.70 2.42 2.94 2.36 2.63
1.382.08 1.953.01 2.303.75 1.723.23 1.823.81
N, total number in the BMI category; #, number in the BMI category with the outcome; %, proportion in the BMI with the outcome. BMI category limits at the OGTT were chosen to match the recommended pre-pregnancy categories of <18.5 (underweight), 18.524.9 (normal range), 25.029.9 (overweight), 30.034.9 (obese class I), 35.039.9 (obese class II), and 40.0 (obese class III). *Dened based on gender, ethnicity, eld centre, gestational age (3644 weeks only), parity using the same methods as for birthweight >90th percentile (see footnote to Table 2). Model I: Adjusted for the variables used in estimating 90th percentiles, age, height and gestational age at the OGTT, smoking, alcohol use, hospitalisation before delivery, any family history of diabetes. Model II: Model I adjustment + fasting plasma glucose and mean arterial pressure.
2010 The Authors Journal compilation RCOG 2010 BJOG An International Journal of Obstetrics and Gynaecology
581
McIntyre et al.
into play at very high levels of BMI. Similar ndings have been reported in obese and severely obese women diagnosed with gestational diabetes.22 Increased frequency of caesarean section with increasing BMI has been noted in previous reports.3,23 This was conrmed in HAPO and found to be independently related to BMI and glycaemic status. This has important practical and health economic implications24 in view of the rising prevalence of obesity in women of child-bearing age.25,26 Maternal BMI was strongly associated with both increased fetal size and adiposity and with pre-eclampsia. This is a paradox because pre-eclampsia is expected to be associated with smaller babies. However, only a small proportion of pregnancies in all BMI categories except the two highest categories developed pre-eclampsia. Other factors, such as substrate supply, may be dominant determinants of fetal growth in the overweight or obese gravida. The plateau in fetal size noted at the highest levels of maternal BMI may partly reect the higher prevalence of pre-eclampsia in these women as 2030% of these groups experienced pre-eclampsia. Preterm delivery was less frequent with higher BMI, consistent with other large studies.3,10 This contrasts with the greater risk of preterm delivery that was found with rising plasma glucose14 and again suggests that alternative mechanisms contribute to pregnancy complications of obesity. The greater frequency of pre-eclampsia might have been predicted to lead to higher rates of preterm delivery in more obese women, but among HAPO participants preeclampsia occurred in only 11.7% of those with preterm delivery. Maternal BMI was not associated with malformations or perinatal mortality, but HAPO was not designed or powered to examine such relationships. Although presence of a known congenital anomaly was not an exclusion criterion, it is unlikely that such women would have been recruited. Major strengths of the HAPO data include careful and standardised documentation of maternal characteristics and pregnancy outcomes in a large, multinational, ethnically diverse group of pregnant women. Strict blinding of maternal glycaemia and the absence of any specic interventions within the study population help to reduce bias. Some limitations should be noted. We hypothesise that maternal BMI inuences pregnancy outcomes primarily through its association with maternal adiposity. However, BMI measured in the third trimester is less closely correlated with maternal fat mass than BMI measured in early pregnancy.27 Lean mothers tend to gain more (and obese mothers less) weight from the pre-pregnancy period to the third trimester (in accordance with current guidelines).28 This observation, conrmed in the HAPO cohort, may have attenuated differences between BMI groups but would not produce false-positive ndings. Maternal height and
weight were not blinded to participants or their caregivers. This may have inuenced clinical decisions, especially regarding mode of delivery. A number of other factors that we did not evaluate in the HAPO Study, for example dietary intake (both calories and nutrient composition), physical activity and/or maternal weight gain are also potentially associated with birthweight, fetal adiposity and hyperinsulinaemia. A single measure of fasting plasma glucose at about 28 weeks of gestation is not a complete surrogate for time and dietary-related integrated glycaemia; however, it is strongly and independently related to the primary and most of the secondary outcomes of the HAPO Study.14,15 We cannot conclude that there is a causal relationship between increased maternal BMI and the adverse outcomes reported, although this would be consistent with both the current data and previous reports.8 We are unable to offer a pathophysiological explanation for the relationship between increased BMI and adverse pregnancy outcomes, but can conclude that mechanisms separate from, or in addition to, the association of hyperglycaemia and obesity are likely to play a role. Differences in supply of other substrates, as well as the inammatory state associated with increased BMI, may contribute to adverse pregnancy outcomes. Despite the clear association of obesity with adverse pregnancy outcomes, a recent systematic review has noted that there is minimal evidence to support any specic treatment strategy.29 One small randomised controlled trial has shown that caloric restriction during pregnancy can reduce weight gain and markers of insulin resistance, but reported no difference in major pregnancy outcomes.30 In conclusion, higher maternal BMI is strongly related to adverse pregnancy outcomes, especially those related to fetal size, adiposity and hyperinsulinism and to pre-eclampsia. It is, however, inversely related to premature delivery. These associations are independent of maternal glycaemia and other potential confounding factors. The pathophysiological mechanisms linking obesity to adverse pregnancy outcomes remain poorly dened and warrant further research. Increasing prevalence of maternal obesity in many countries will place an increasing burden on healthcare resources. Prevention and optimal treatment of maternal obesity have the potential to substantially reduce adverse fetal and maternal pregnancy outcomes.
Disclosure of interests
None of the members of the Writing Group report a conict of interest.
Contribution to authorship
These individuals formed the Writing Group: HD McIntyre, BE Metzger, LP Lowe, AR Dyer, P Catalano, ER Trimble, B Persson, JJN Oats, M Hod, DR Hadden, DR Coustan.
582
2010 The Authors Journal compilation RCOG 2010 BJOG An International Journal of Obstetrics and Gynaecology
HAPO BMI and perinatal outcomes
Members of the HAPO Study Cooperative Research Group are listed in the Supporting Information Appendix S1.
Details of ethics approval
The Clinical Coordinating Center for this study undergoes annual ethics approval by the Northwestern University Ofce for the Protection of Research Subjects as Protocol # 0353-001. On 17 April 2009 it was approved for the period 8 May 2009 through to 7 May 2010.
Funding
The study was funded by grants R01-HD34242 and R01HD34243 from the National Institute of Child Health and Human Development and the National Institute of Diabetes, Digestive, and Kidney Diseases, by the National Center for Research Resources (M01-RR00048, M01-RR00080), and by the American Diabetes Association. Support has also been provided to local eld centres by Diabetes UK (RD04/0002756), Kaiser Permanente Medical Center, KK Womens and Childrens Hospital, Mater Mothers Hospital, Novo Nordisk, the Myre Sim Fund of the Royal College of Physicians of Edinburgh, and the Howard and Carol Bernick Family Foundation.
Supporting information
The following supplementary materials are available for this article: Appendix S1. List of authors. Additional Supporting Information may be found in the online version of this article. Please note: Wiley-Blackwell are not responsible for the content or functionality of any supporting materials supplied by the authors. Any queries (other than missing material) should be directed to the corresponding author for the article. j
References
1 OBrien TE, Ray JG, Chan WS. Maternal body mass index and the risk of preeclampsia: a systematic overview. Epidemiology 2003;14:36874. 2 Callaway LK, Prins JB, Chang AM, McIntyre HD. The prevalence and impact of overweight and obesity in an Australian obstetric population. Med J Austr 2006;184:569. 3 Sebire NJ, Jolly M, Harris JP, et al. Maternal obesity and pregnancy outcome: a study of 287,213 pregnancies in London. Int J Obes Relat Metab Disord 2001;25:117582. 4 Chu SY, Callaghan WM, Kim SY, et al. Maternal obesity and risk of gestational diabetes mellitus. Diabetes Care 2007;30:2070 6. 5 CEMACH. Why mothers die. The Sixth Report into Maternal Deaths in the United Kingdom. London: RCOG Press, 2004. 6 Chu SY, Kim SY, Lau J, et al. Maternal obesity and risk of stillbirth: a metaanalysis. Am J Obstet Gynecol 2007;197:2238.
7 Stothard KJ, Tennant PW, Bell R, Rankin J. Maternal overweight and obesity and the risk of congenital anomalies: a systematic review and meta-analysis. J Am Med Assoc 2009;301:63650. 8 Catalano PM, Ehrenberg HM. The short- and long-term implications of maternal obesity on the mother and her offspring. BJOG 2006;113:112633. 9 Cedergren MI. Maternal morbid obesity and the risk of adverse pregnancy outcome. Obstet Gynecol 2004;103:21924. 10 Cnattingius S, Bergstrom R, Lipworth L, Kramer MS. Prepregnancy weight and the risk of adverse pregnancy outcomes. N Engl J Med 1998;338:14752. 11 Sermer M, Naylor CD, Farine D, et al. The Toronto Tri-Hospital Gestational Diabetes Project. A preliminary review. Diabetes Care 1998;21(Suppl. 2):B3342. 12 Schmidt MI, Duncan BB, Reichelt AJ, et al. Gestational diabetes mellitus diagnosed with a 2-h 75-g oral glucose tolerance test and adverse pregnancy outcomes. Diabetes Care 2001;24: 11515. 13 HAPO Study Cooperative Research Group. The Hyperglycemia and Adverse Pregnancy Outcome (HAPO) Study. Int J Gynecol Obstet 2002;78:6977. 14 HAPO Study Cooperative Research Group. Hyperglycemia and adverse pregnancy outcomes. N Engl J Med 2008;358:19912002. 15 HAPO Study Cooperative Research Group. Hyperglycemia and Adverse Pregnancy Outcome (HAPO) Study: associations with neonatal anthropometrics. Diabetes 2009;58:4539. 16 Catalano PM, Thomas AJ, Avallone DA, Amini SB. Anthropometric estimation of neonatal body composition. Am J Obstet Gynecol 1995;173:117681. 17 World Health Organization. Obesity: Preventing and Managing the Global Epidemic. Geneva, Switzerland: World Health Organization; 2000, WHO technical report series 894. 18 Grifths LJ, Dezateux C, Cole TJ. Differential parental weight and height contributions to offspring birthweight and weight gain in infancy. Int J Epidemiol 2007;36:1047. 19 Schaefer-Graf UM, Graf K, Kulbacka I, et al. Maternal lipids as strong determinants of fetal environment and growth in pregnancies with gestational diabetes mellitus. Diabetes Care 2008;31:185863. 20 Carpenter MW, Canick JA, Star J, Carr SR, Burke ME, Shahinian K. Fetal hyperinsulinism at 1420 weeks and subsequent gestational diabetes. Obstet Gynecol 1996;87:8993. 21 Ramsay JE, Ferrell WR, Crawford L, Wallace AM, Greer IA, Sattar N. Maternal obesity is associated with dysregulation of metabolic, vascular, and inammatory pathways. J Clin Endocrinol Metab 2002;87:42317. 22 Yogev Y, Langer O. Pregnancy outcome in obese and morbidly obese gestational diabetic women. Eur J Obstet Gynecol Reprod Biol 2008;137:216. 23 Chu SY, Kim SY, Schmid CH, et al. Maternal obesity and risk of cesarean delivery: a meta-analysis. Obes Rev 2007;8:38594. 24 Chu SY, Bachman DJ, Callaghan WM, et al. Association between obesity during pregnancy and increased use of health care. N Engl J Med 2008;358:144453. 25 Kim SY, Dietz PM, England L, Morrow B, Callaghan WM. Trends in pre-pregnancy obesity in nine states, 19932003. Obesity (Silver Spring) 2007;15:98693. 26 Heslehurst N, Ells LJ, Simpson H, Batterham A, Wilkinson J, Summerbell CD. Trends in maternal obesity incidence rates, demographic predictors, and health inequalities in 36,821 women over a 15-year period. BJOG 2007;114:18794. 27 Sewell MF, Huston-Presley L, Amini SB, Catalano PM. Body mass index: a true indicator of body fat in obese gravidas. J Reprod Med 2007;52:90711.
2010 The Authors Journal compilation RCOG 2010 BJOG An International Journal of Obstetrics and Gynaecology
583
McIntyre et al.
28 Schieve LA, Cogswell ME, Scanlon KS. Maternal weight gain and preterm delivery: differential effects by body mass index. Epidemiology 1999;10:1417. 29 Dodd JM, Crowther CA, Robinson JS. Dietary and lifestyle interventions to limit weight gain during pregnancy for obese or overweight women: a systematic review. Acta Obstet Gynecol Scand 2008;87: 7026. 30 Wolff S, Legarth J, Vangsgaard K, Toubro S, Astrup A. A randomized trial of the effects of dietary counseling on gestational weight
gain and glucose metabolism in obese pregnant women. Int J Obes (Lond) 2008;32:495501. 31 Brown MA, Lindheimer MD, de Swiet M, Van Assche A, Moutquin JM. The classication and diagnosis of the hypertensive disorders of pregnancy: statement from the International Society for the Study of Hypertension in Pregnancy (ISSHP). Hypertens Pregnancy 2001;20: IXXIV.
584
2010 The Authors Journal compilation RCOG 2010 BJOG An International Journal of Obstetrics and Gynaecology
Vous aimerez peut-être aussi
- Complementary and Alternative Medical Lab Testing Part 10: ObstetricsD'EverandComplementary and Alternative Medical Lab Testing Part 10: ObstetricsPas encore d'évaluation
- Risk Factors For Fetal Macrosomia: The Importance of A Positive Oral Glucose Challenge TestDocument7 pagesRisk Factors For Fetal Macrosomia: The Importance of A Positive Oral Glucose Challenge TestKhuriyatun NadhifahPas encore d'évaluation
- Hapo Study GDMDocument6 pagesHapo Study GDMRaul Garcia Salas CastilloPas encore d'évaluation
- Gestationaldiabetes Mellitus: Emily D. Szmuilowicz,, Jami L. Josefson,, Boyd E. MetzgerDocument15 pagesGestationaldiabetes Mellitus: Emily D. Szmuilowicz,, Jami L. Josefson,, Boyd E. Metzgerjose ricardo escalante perezPas encore d'évaluation
- Scientific Advisory Committee Opinion Paper 23: 1. BackgroundDocument5 pagesScientific Advisory Committee Opinion Paper 23: 1. BackgroundNatia DemetradzePas encore d'évaluation
- OGTT and Adverse Outcome 2020Document10 pagesOGTT and Adverse Outcome 2020Nuraida baharuddinPas encore d'évaluation
- Gestiational DMDocument6 pagesGestiational DMTiara AnggianisaPas encore d'évaluation
- Jurnal Hiperemesis GravidarumDocument6 pagesJurnal Hiperemesis GravidarumArief Tirtana PutraPas encore d'évaluation
- J of Obstet and Gynaecol - 2011 - Olmos - Gestational Diabetes and Pre Pregnancy Overweight Possible Factors Involved inDocument7 pagesJ of Obstet and Gynaecol - 2011 - Olmos - Gestational Diabetes and Pre Pregnancy Overweight Possible Factors Involved iniriartenela14Pas encore d'évaluation
- Diagnosis of Gestational DiabetesDocument7 pagesDiagnosis of Gestational DiabetesAl Hasyr SarminPas encore d'évaluation
- Association Between Intrahepatic Cholestasis in Pregnancy and Gestational Diabetes Mellitus. A Retrospective AnalysisDocument6 pagesAssociation Between Intrahepatic Cholestasis in Pregnancy and Gestational Diabetes Mellitus. A Retrospective AnalysisDr.Karima EldarhobiPas encore d'évaluation
- Gestational Diabetes Screening The International.4 PDFDocument8 pagesGestational Diabetes Screening The International.4 PDFfakhriaiiPas encore d'évaluation
- Gestasional Diabetes Overview With Emphasis On Medical ManagementDocument12 pagesGestasional Diabetes Overview With Emphasis On Medical ManagementMuliana DatuPas encore d'évaluation
- Gestational Diabetes Mellitus DiagnosedDocument5 pagesGestational Diabetes Mellitus DiagnosedMutia AgustriaPas encore d'évaluation
- Gestational Diabetes Mellitus Screening and Outcomes: Original Investigation 25Document5 pagesGestational Diabetes Mellitus Screening and Outcomes: Original Investigation 25Eduardo SasintuñaPas encore d'évaluation
- 2010 Update On Gestational DiabetesDocument13 pages2010 Update On Gestational DiabetesAde Gustina SiahaanPas encore d'évaluation
- J Perinatol 2013 ShangDocument5 pagesJ Perinatol 2013 ShangAnonymous wXtDpPPas encore d'évaluation
- Diagnosis and Treatment of Gestational Diabetes: Scientific Impact Paper No. 23Document6 pagesDiagnosis and Treatment of Gestational Diabetes: Scientific Impact Paper No. 23Ane DamayantiPas encore d'évaluation
- Pattern of Glucose Intolerance Among Pregnant Women With Unexplained IUFDDocument5 pagesPattern of Glucose Intolerance Among Pregnant Women With Unexplained IUFDTri UtomoPas encore d'évaluation
- Cap. 11Document4 pagesCap. 11Familia CieletPas encore d'évaluation
- Exercise in Pregnant Women and Birth WeightDocument4 pagesExercise in Pregnant Women and Birth WeightJelita SihombingPas encore d'évaluation
- Gestational Weight GainDocument3 pagesGestational Weight GainainindyaPas encore d'évaluation
- Increase Fetal Adiposity1Document7 pagesIncrease Fetal Adiposity1Hervi LaksariPas encore d'évaluation
- Jog 12115Document7 pagesJog 12115niko4eyesPas encore d'évaluation
- Gestational Diabetes - On Broadening The DiagnosisDocument2 pagesGestational Diabetes - On Broadening The DiagnosisWillians ReyesPas encore d'évaluation
- Diagnosis and Treatment of Gestasional DiabetesDocument18 pagesDiagnosis and Treatment of Gestasional DiabetesDevi Christina Damanik (Papua medical School)Pas encore d'évaluation
- Influence of Maternal Weight Gain On Birth Weight: A Gestational Diabetes CohortDocument9 pagesInfluence of Maternal Weight Gain On Birth Weight: A Gestational Diabetes Cohortمالك مناصرةPas encore d'évaluation
- What Are The Existing Diagnostic Criteria?Document6 pagesWhat Are The Existing Diagnostic Criteria?Utkarsh AbhilashPas encore d'évaluation
- 190 - Gestational Diabetes Mellitus AgogDocument16 pages190 - Gestational Diabetes Mellitus Agogjorge vergara100% (2)
- Stir Rat 2014Document1 pageStir Rat 2014Dayana Cuyuche JuarezPas encore d'évaluation
- Artikel Aulia DyahDocument8 pagesArtikel Aulia DyahproluvieslacusPas encore d'évaluation
- Clinical and Epidemiological Profile of Diabetes Mellitus in Pregnancy, Isle of Youth, 2008Document6 pagesClinical and Epidemiological Profile of Diabetes Mellitus in Pregnancy, Isle of Youth, 2008nunki aprillitaPas encore d'évaluation
- Fetal Growth in Insulin Dependent DMDocument5 pagesFetal Growth in Insulin Dependent DMGeorge Tirta DihatmoPas encore d'évaluation
- GDM FOGSI Text Book FinalDocument29 pagesGDM FOGSI Text Book FinalKruthika Devaraja GowdaPas encore d'évaluation
- Umanand Prasad School of Medicine and Health ScienceDocument13 pagesUmanand Prasad School of Medicine and Health ScienceShakshi RainaPas encore d'évaluation
- Dean OfficeDocument73 pagesDean Officearief19Pas encore d'évaluation
- Acid Jurnal 4Document7 pagesAcid Jurnal 4awaloeiacidPas encore d'évaluation
- Point: Yes, It Is Necessary To Rely Entirely On Glycemic Values For The Insulin Treatment of All Gestational Diabetic WomenDocument2 pagesPoint: Yes, It Is Necessary To Rely Entirely On Glycemic Values For The Insulin Treatment of All Gestational Diabetic WomenGeorge Tirta DihatmoPas encore d'évaluation
- Medi 102 E33898Document7 pagesMedi 102 E33898ade lydia br.siregarPas encore d'évaluation
- DMG Diagnosis and ManagementDocument6 pagesDMG Diagnosis and ManagementCésar MonjarásPas encore d'évaluation
- Assignment On Course During CCGDM.Document6 pagesAssignment On Course During CCGDM.Biman MondalPas encore d'évaluation
- Early Gestational Diabetes Screening in Obese Women: A Randomized Controlled TrialDocument8 pagesEarly Gestational Diabetes Screening in Obese Women: A Randomized Controlled Trialunie cantiqPas encore d'évaluation
- 17 ShaofangDocument4 pages17 Shaofangiriartenela14Pas encore d'évaluation
- Case Write UpDocument5 pagesCase Write UpAisyah Hamdan100% (1)
- Effects of Low Glycemic Index Diets in Pregnancy On Maternal and Newborn Outcomes in Pregnant Women: A Meta Analysis of Randomized Controlled TrialsDocument11 pagesEffects of Low Glycemic Index Diets in Pregnancy On Maternal and Newborn Outcomes in Pregnant Women: A Meta Analysis of Randomized Controlled TrialssilvanaPas encore d'évaluation
- Pre-Existing Diabetes Mellitus and Adverse PDFDocument5 pagesPre-Existing Diabetes Mellitus and Adverse PDFMetebPas encore d'évaluation
- Obesidad y EmbarazoDocument5 pagesObesidad y EmbarazolandaburePas encore d'évaluation
- Gestational Diabetes and Intra Uterine Fetaldeath Complication in A Tertiary Health FacilityDocument5 pagesGestational Diabetes and Intra Uterine Fetaldeath Complication in A Tertiary Health Facilityade lydia br.siregarPas encore d'évaluation
- Embarazo DiabetesDocument10 pagesEmbarazo DiabetesMaria Gabriela AguilarPas encore d'évaluation
- Hypoglycemia and Associated Comorbidities Among Newborns of Mothers With Diabetes in An Academic Tertiary Care CenterDocument15 pagesHypoglycemia and Associated Comorbidities Among Newborns of Mothers With Diabetes in An Academic Tertiary Care CenterrimzeenafeeshaPas encore d'évaluation
- Poster Session II: ConclusionDocument1 pagePoster Session II: ConclusionSlr RandiPas encore d'évaluation
- Screening and DiagnosisDocument25 pagesScreening and DiagnosisM AbhiPas encore d'évaluation
- First Trimester Aneuploidy Screening Markers in Women With Pre-Gestational Diabetes MellitusDocument11 pagesFirst Trimester Aneuploidy Screening Markers in Women With Pre-Gestational Diabetes MellituslarazahabiPas encore d'évaluation
- Diabetes Acog 2017Document15 pagesDiabetes Acog 2017Holger Vicente Guerrero Guerrero100% (1)
- HiP Unit 1 Module 2 Lab TrainingDocument17 pagesHiP Unit 1 Module 2 Lab TrainingWajid MohammedPas encore d'évaluation
- Benefit and Risk of OHA Compared To Insulin in Women With GDMDocument13 pagesBenefit and Risk of OHA Compared To Insulin in Women With GDMNoraPas encore d'évaluation
- Tugas Ebm Anisa Fitri HandaniDocument23 pagesTugas Ebm Anisa Fitri HandanianisFitrihandani anisaPas encore d'évaluation
- Literature Review of Gestational Diabetes MellitusDocument7 pagesLiterature Review of Gestational Diabetes Mellitusc5rc7ppr100% (1)
- Correlations Between Parameters of Glycaemic Variability and Foetal Growth Neonatal Hypoglycaemia and Hyperbilirubinemia in Women With Gestational diabetesPLoS ONEDocument14 pagesCorrelations Between Parameters of Glycaemic Variability and Foetal Growth Neonatal Hypoglycaemia and Hyperbilirubinemia in Women With Gestational diabetesPLoS ONEVicente Fasce OlmosPas encore d'évaluation
- Physical Activity and Dietary Habits During Pregnancy: Effects On Glucose ToleranceDocument6 pagesPhysical Activity and Dietary Habits During Pregnancy: Effects On Glucose ToleranceJulia ChuPas encore d'évaluation
- Vidhya Finalised ThesisDocument84 pagesVidhya Finalised Thesisdr.vidhyaPas encore d'évaluation
- Caesarean ThesisDocument8 pagesCaesarean Thesisdr.vidhyaPas encore d'évaluation
- Medical Abortion: Frequently Asked Clinical QuestionsDocument41 pagesMedical Abortion: Frequently Asked Clinical Questionsdr.vidhyaPas encore d'évaluation
- CSOM3Document7 pagesCSOM3dr.vidhyaPas encore d'évaluation
- The Madras Medical Mission: Application FormDocument2 pagesThe Madras Medical Mission: Application Formdr.vidhyaPas encore d'évaluation
- Fetal Neurosonography by Fratelli Et Al PDFDocument12 pagesFetal Neurosonography by Fratelli Et Al PDFdr.vidhyaPas encore d'évaluation
- I, M S - PartiallyDocument9 pagesI, M S - Partiallydr.vidhyaPas encore d'évaluation
- Thesis Protocol Submission FormDocument5 pagesThesis Protocol Submission Formdr.vidhya0% (1)
- Fetal Neurosonography by Fratelli Et Al PDFDocument12 pagesFetal Neurosonography by Fratelli Et Al PDFdr.vidhyaPas encore d'évaluation
- AOICON - 2014, Mysore: Guidelines For E-Poster PresentationDocument2 pagesAOICON - 2014, Mysore: Guidelines For E-Poster Presentationdr.vidhyaPas encore d'évaluation
- Gestational Diabetes and Maternal ObesityDocument2 pagesGestational Diabetes and Maternal Obesitydr.vidhyaPas encore d'évaluation
- Blue Book - Guidelines For The Control of Infectious DiseaseDocument271 pagesBlue Book - Guidelines For The Control of Infectious DiseaseavarathunnyPas encore d'évaluation
- 2022 09 10NewScientistDocument60 pages2022 09 10NewScientistAyala AbishevaPas encore d'évaluation
- Circular To Dental CollegesDocument3 pagesCircular To Dental CollegesrajeshPas encore d'évaluation
- Intracardiac Epinephrine Injection During Open Thoracotomy and Circulatory Arrest 2155 6148.1000341Document2 pagesIntracardiac Epinephrine Injection During Open Thoracotomy and Circulatory Arrest 2155 6148.1000341samuelPas encore d'évaluation
- Yuan 2021Document34 pagesYuan 2021Sagar PatilPas encore d'évaluation
- Acta Pediatrica Enero 2021 - Topicos NeonatalesDocument113 pagesActa Pediatrica Enero 2021 - Topicos NeonatalesalbertoPas encore d'évaluation
- AIIMS 2015 Solved PaperDocument436 pagesAIIMS 2015 Solved PaperSurya TejaPas encore d'évaluation
- SP 32434 Warm Up and Cool Down - Indd PDFDocument1 pageSP 32434 Warm Up and Cool Down - Indd PDFMylene EntionPas encore d'évaluation
- AP Psych SyllabusDocument140 pagesAP Psych SyllabusAlex JinPas encore d'évaluation
- Project ENGLISH 2019 BacteriaDocument4 pagesProject ENGLISH 2019 BacteriaAna Maria MacoveiPas encore d'évaluation
- GE9 TheLifeAndWorksOfRizal CAMDocument4 pagesGE9 TheLifeAndWorksOfRizal CAMCriselPas encore d'évaluation
- Does WiFi Affect The BrainDocument6 pagesDoes WiFi Affect The BrainrustyPas encore d'évaluation
- Chapter 17 Unit IDocument23 pagesChapter 17 Unit IGlory MimiPas encore d'évaluation
- Research Project Sept. Milen GimenaDocument21 pagesResearch Project Sept. Milen GimenaKaitline LaxamanaPas encore d'évaluation
- Spinal StenosisDocument14 pagesSpinal StenosisHONGJYPas encore d'évaluation
- Epidemiology of Knee Injuries Among Boys and Girls in US High School AthleticsDocument7 pagesEpidemiology of Knee Injuries Among Boys and Girls in US High School AthleticsbomgorilaoPas encore d'évaluation
- Effect of Organic Manure On Growth and Yield of Strawberry: January 2014Document5 pagesEffect of Organic Manure On Growth and Yield of Strawberry: January 2014LekhonVlogsPas encore d'évaluation
- Envidea 2011 ASP Case StudyDocument17 pagesEnvidea 2011 ASP Case Studylefty298Pas encore d'évaluation
- Biology Notes (Bilingual)Document349 pagesBiology Notes (Bilingual)dipanjan biswasPas encore d'évaluation
- SAMPLE Outline PanicDocument3 pagesSAMPLE Outline PanicdexPas encore d'évaluation
- Clinical ChemistryDocument24 pagesClinical ChemistryQueency Dangilan100% (1)
- Lhea's Case StudyDocument14 pagesLhea's Case StudyMelody B. MiguelPas encore d'évaluation
- 9375 X PER3 Therapy Lamp ManualDocument26 pages9375 X PER3 Therapy Lamp ManualAmicus79Pas encore d'évaluation
- 1 s2.0 S2772594422001637 MainDocument5 pages1 s2.0 S2772594422001637 MainCatarina CourasPas encore d'évaluation
- Abreu, CarlosDocument1 pageAbreu, CarlosCarlos AbreuPas encore d'évaluation
- Screenshot 2021-06-23 at 11.36.48 AMDocument116 pagesScreenshot 2021-06-23 at 11.36.48 AMSmitha ShekarPas encore d'évaluation
- Failure of Endoscopic Spine SurgeryDocument6 pagesFailure of Endoscopic Spine SurgeryKaustubh KeskarPas encore d'évaluation
- Nursing Process of PneumoniaDocument5 pagesNursing Process of Pneumoniatin2x061275% (8)
- Ayurpharm8 PDFDocument8 pagesAyurpharm8 PDFRamling PatrakarPas encore d'évaluation
- DiphtheriaDocument10 pagesDiphtheriaAgustin IskandarPas encore d'évaluation
- Derma OSCEDocument3 pagesDerma OSCEUsama El BazPas encore d'évaluation