Académique Documents
Professionnel Documents
Culture Documents
Incentive Spirometry
Transféré par
Nursidar Pascual MukattilCopyright
Formats disponibles
Partager ce document
Partager ou intégrer le document
Avez-vous trouvé ce document utile ?
Ce contenu est-il inapproprié ?
Signaler ce documentDroits d'auteur :
Formats disponibles
Incentive Spirometry
Transféré par
Nursidar Pascual MukattilDroits d'auteur :
Formats disponibles
IS 1.0 PROCEDURE: Incentive spirometry, also referred to as sustained maximal inspiration (SMI), is a component of bronchial hygiene therapy.(1-3) IS 2.
0 DESCRIPTION/DEFINITION: 2.1 Incentive spirometry is designed to mimic natural sighing or yawning by encouraging the patient to take long, slow, deep breaths.(1,2,4,5) This is accomplished by using a device that provides patients with visual or other positive feedback when they inhale at a predetermined flowrate or volume and sustain the inflation for a minimum of 3 seconds.(2,3,5-7) The objectives of this procedure are to increase transpulmonary pressure and inspiratory volumes, improve inspiratory muscle perfor-mance,8 and re-establish or simulate the normal pattern of pulmonary hyperinflation.3 When the procedure is repeated on a regular basis, airway patency may be maintained and lung atelectasis prevented and reversed.(1-3,5,6,9,10) 2.2 Incentive spirometry should be contrasted with expiratory maneuvers (such as the use of blow bottles) that do not mimic the sigh and have been associated with the production of reduced lung volumes.(5,6) IS 3.0 SETTINGS: 3.1 Critical care 3.2 Acute care inpatient 3.3 Extended care and skilled nursing facility 3.4 Home care(8) IS 4.0 INDICATIONS: 4.1 Presence of conditions predisposing to the development of pulmonary atelectasis 4.1.1 upper-abdominal surgery(2,4,9-14) 4.1.2 thoracic surgery(9,10,13-15) 4.1.3 surgery in patients with chronic obstructive pulmonary disease (COPD)(7,13-15) 4.2 Presence of pulmonary atelectasis(16) 4.3 Presence of a restrictive lung defect associated with quadraplegia and/or dysfunctional diaphragm.(6,8,14,17,18) IS 5.0 CONTRAINDICATIONS: 5.1 Patient cannot be instructed or supervised to assure appropriate use of the device. 5.2 Patient cooperation is absent(2,16) or patient is unable to understand or demonstrate proper use of the device.(16) 5.3 IS is contraindicated in patients unable to deep breathe effectively (eg, with vital capacity [VC] less than about 10 mL/kg or inspiratory capacity [IC] less than about one third of predicted). 5.4 The presence of an open tracheal stoma is not a contraindication but requires adaptation of the spirometer.
IS 6.0 HAZARDS AND COMPLICATIONS: 6.1 Ineffective unless closely supervised or performed as ordered(6) 6.2 Inappropriate as sole treatment for major lung collapse or consolidation 6.3 Hyperventilation 6.4 Barotrauma (emphysematous lungs)(19) 6.5 Discomfort secondary to inadequate pain control(15,18) 6.6 Hypoxia secondary to interruption of prescribed oxygen therapy if face mask or shield is being used 6.7 Exacerbation of bronchospasm 6.8 Fatigue(20,21) IS 7.0 LIMITATIONS OF METHOD: Evidence suggests that deep breathing alone without mechanical aides can be as beneficial as incentive spirometry in preventing or reversing pulmonary complications,(1-5) and controversy exists concerning overuse of the procedure.(1,4,6) IS 8.0 ASSESSMENT OF NEED: 8.1 Surgical procedure involving upper abdomen or thorax(4,5) 8.2 Conditions predisposing to development of atelectasis including immobility, poor pain control, and abdominal binders 8.3 Presence of neuromuscular disease involving respiratory musculature(8) IS 9.0 ASSESSMENT OF OUTCOME: 9.1 Absence of or improvement in signs of atelectasis 9.1.1 decreased respiratory rate(16,17) 9.1.2 resolution of fever(2,18) 9.1.3 normal pulse rate(14) 9.1.4 absent crackles (rales)(20) or presence of or improvement in previously absent or diminished breath sounds 9.1.5 normal chest x-ray(2) 9.1.6 improved arterial oxygen tension (PaO2) and decreased alveolar-arterial oxygen tension gradient, or P(Aa)O2(1,3,4,9,10) 9.1.7 increased VC and peak expiratory flows(4,16,17) 9.1.8 return of functional residual capacity (FRC) or VC to preoperative values4,(15-17) in absence of lung resection 9.2 Improved inspiratory muscle perfor-mance 9.2.1 attainment of preoperative flow and volume levels1(1) 9.2.2 increased forced vital capacity (FVC) IS 10.0 RESOURCES:
10.1Equipment 10.1.1 incentive spirometer 10.1.2 conclusive evidence to support the use of one type or brand of device over others is lacking(20,22) 10.2 Personnel 10.2.1 Level I personnel should possess 10.2.1.1 mastery of techniques for proper operation and clinical application of device(6) and understanding of the importance of effective postopera-tive pain relief(15,16,18) and the absence of other impediments to patient cooperation (such as residual anesthetic or sensory impairment(12,17)) 10.2.1.2 ability to instruct patient in proper technique(2,6) and an under-standing of the importance of preoperative instruction and supervised practice 10.2.1.3 ability to respond appropriately to adverse effects 10.2.1.4 knowledge of and ability to implement Universal Precautions 10.2.2 Level II personnel, in addition to possessing knowledge and abilities described in 10.2.1.1-10.2.1.4, should have demonstrated ability to assess patient need for and response to therapy and recommend modifications and discontinu-ance as appropriate. IS 11.0 MONITORING: Direct supervision of every patient performance is not necessary once the patient has demonstrated mastery of technique;(6,16,23) however, preoperative instruction, volume goals, and feedback are essential to optimal performance. 11.1 Observation of patient performance and utilization 11.1.1 frequency of sessions(16) 11.1.2 number of breaths/session(16) 11.1.3 inspiratory volume or flow goals achieved(16) and 3- to 5-second breath-hold maintained 11.1.4 effort/motivation(16) 11.2 Periodic observation of patient compliance with technique,(6,16,23) with additional in-struction as necessary 11.3 Device within reach of patient(5) and patient encouraged to perform independently 11.4 New and increasing inspiratory volumes established each day 11.5 Vital signs IS 12.0 FREQUENCY: A number of authors suggest using the device 5-10 breaths per session, at a minimum, every hour while awake (ie, 100 times a day).(2,7,19) Caregiver does not need to be present with each performance, and patient should be encouraged to perform independently. IS 13.0 INFECTION CONTROL: 13.1 Universal Precautions(24) 13.2 Proper labeling and appropriate storage of devices between uses and appropriate cleaning of devices between patients(25)
Vous aimerez peut-être aussi
- Incentive SpirometryDocument6 pagesIncentive SpirometryRiza Angela BarazanPas encore d'évaluation
- Hirschsprung’s Disease, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsD'EverandHirschsprung’s Disease, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsPas encore d'évaluation
- Module 2 - Incentive Spirometry (Student)Document4 pagesModule 2 - Incentive Spirometry (Student)febie pacheco0% (1)
- Checklist On Incentive Siprometry Procedure 1 2 3 4 5 Remarks Preparatory PhaseDocument1 pageChecklist On Incentive Siprometry Procedure 1 2 3 4 5 Remarks Preparatory PhaseShermayne Mallapre HernandezPas encore d'évaluation
- Teaching Module Hypertension PregnancyDocument17 pagesTeaching Module Hypertension PregnancyQueenie BlasurcaPas encore d'évaluation
- Urine Specimen CollectionDocument3 pagesUrine Specimen Collectionyota_ahlyPas encore d'évaluation
- SuctioningDocument27 pagesSuctioningMoni Mbumba MelekePas encore d'évaluation
- Pregnancy Induced HypertensionDocument4 pagesPregnancy Induced HypertensionMjhay SalvadorPas encore d'évaluation
- Oxygen InhalationDocument26 pagesOxygen InhalationdaisyPas encore d'évaluation
- DialysisDocument3 pagesDialysisSarah BenjaminPas encore d'évaluation
- 07.04.05 Venturi Face MaskDocument2 pages07.04.05 Venturi Face MaskRosintchi MirsalPas encore d'évaluation
- NGT GavageDocument29 pagesNGT GavageMaan LapitanPas encore d'évaluation
- Performing Chest PhysiotherapyDocument14 pagesPerforming Chest PhysiotherapyDivya Chauhan100% (1)
- Assignment ON MyelographyDocument12 pagesAssignment ON MyelographyDiana CharaPas encore d'évaluation
- Endotracheal IntubationDocument5 pagesEndotracheal Intubationpriyanka bhavsarPas encore d'évaluation
- Atrial Septal DefectDocument5 pagesAtrial Septal DefectalmorsPas encore d'évaluation
- CP On AGEDocument31 pagesCP On AGELeah CaressaPas encore d'évaluation
- Levine Theory ApplicationDocument38 pagesLevine Theory ApplicationSimon JosanPas encore d'évaluation
- Glasgow Coma ScaleDocument13 pagesGlasgow Coma ScaleDanna Christine Gumboc PaguntalanPas encore d'évaluation
- Femur Fracture Health EducationDocument1 pageFemur Fracture Health EducationMadx VPas encore d'évaluation
- WeaningDocument7 pagesWeaningKiran KhasaPas encore d'évaluation
- Cpms College of Nursing Assignment ON Oral Medication: DATED: 18 MAY, 2021 Subject: Child Health NursingDocument4 pagesCpms College of Nursing Assignment ON Oral Medication: DATED: 18 MAY, 2021 Subject: Child Health NursingAmy LalringhluaniPas encore d'évaluation
- Chest PhysiotherapyDocument22 pagesChest Physiotherapyغيداء الذويبي100% (1)
- Endotracheal Tube SuctioningDocument5 pagesEndotracheal Tube SuctioningArlene DalisayPas encore d'évaluation
- HypothermiaDocument5 pagesHypothermiaMRS CHAKRAPANIPas encore d'évaluation
- Incentive SpirometersDocument3 pagesIncentive SpirometersmlbonthelinePas encore d'évaluation
- DiabetesDocument59 pagesDiabetesshiv gautamPas encore d'évaluation
- Initiating A Blood TransfusionDocument5 pagesInitiating A Blood TransfusionJoyce Kathreen Ebio LopezPas encore d'évaluation
- Care of Unconscious PatientDocument7 pagesCare of Unconscious PatientSalliePas encore d'évaluation
- Hemodynamic MonitoringDocument28 pagesHemodynamic MonitoringKimberlie Dela Merced Tomas100% (1)
- Nursing Care Plans For Diabetes MellitusDocument12 pagesNursing Care Plans For Diabetes MellitusPuteri AzmanPas encore d'évaluation
- Nursing Skill Iv InsertionDocument8 pagesNursing Skill Iv InsertionSabrina TolentinoPas encore d'évaluation
- Chest Physiotherapy - Postural DrainageDocument2 pagesChest Physiotherapy - Postural DrainageMicah MagallanoPas encore d'évaluation
- Care of HemophiliaDocument7 pagesCare of HemophiliaBasant karn100% (4)
- Nursing Care of The NBDocument37 pagesNursing Care of The NBJan Oliver YaresPas encore d'évaluation
- Bag Mask VentilationDocument35 pagesBag Mask VentilationedrinsnePas encore d'évaluation
- Oxygen Therapy Administration For Paediatric PatientsDocument7 pagesOxygen Therapy Administration For Paediatric PatientsYwagar YwagarPas encore d'évaluation
- Orogastric Tube InsertionDocument5 pagesOrogastric Tube InsertionUday KumarPas encore d'évaluation
- Acute Respiratory Distress Syndrome, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsD'EverandAcute Respiratory Distress Syndrome, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsPas encore d'évaluation
- Pediatric Ist SeminarDocument21 pagesPediatric Ist SeminarAsha jiluPas encore d'évaluation
- Tracheostomy CareDocument10 pagesTracheostomy CareSharifa Al AmerPas encore d'évaluation
- Dr. Rosi - CPAPDocument65 pagesDr. Rosi - CPAPtom24Pas encore d'évaluation
- Glasgow Coma ScaleDocument2 pagesGlasgow Coma Scalejean theresePas encore d'évaluation
- ANP - Family and Home NursingDocument11 pagesANP - Family and Home NursingRinal Barad100% (1)
- RestraintsDocument48 pagesRestraintsLeena Pravil100% (1)
- Chest PhysiotherapyDocument29 pagesChest PhysiotherapyHari25885Pas encore d'évaluation
- Guidelines For Performing Suctioning in ChildrenDocument4 pagesGuidelines For Performing Suctioning in Childrensusheewa100% (3)
- Nasogastric Tube InsertionDocument11 pagesNasogastric Tube InsertionDiane Kate Tobias Magno100% (1)
- Urine CollectionDocument6 pagesUrine CollectionfaithnsocPas encore d'évaluation
- Neonatal ResuscitationDocument5 pagesNeonatal Resuscitationabdirahiim ahmedPas encore d'évaluation
- Esophageal AtresiaDocument18 pagesEsophageal AtresiaNeha RathorePas encore d'évaluation
- Bipap Ventilation Basic and MonitoringDocument33 pagesBipap Ventilation Basic and MonitoringPradip ChougalePas encore d'évaluation
- The Newborn Care: Fcnlxa - St. Luke's College of NursingDocument10 pagesThe Newborn Care: Fcnlxa - St. Luke's College of NursingFrancine LaxaPas encore d'évaluation
- Reteplase (MIRel)Document23 pagesReteplase (MIRel)Jhoann JamanilaPas encore d'évaluation
- Procedure On Lumber PunctureDocument8 pagesProcedure On Lumber PunctureDimpal ChoudharyPas encore d'évaluation
- Oesophageal Atresia by GabriellaDocument7 pagesOesophageal Atresia by GabriellaGabriellePas encore d'évaluation
- Epidimiological ApprochDocument14 pagesEpidimiological ApprochBabita DhruwPas encore d'évaluation
- NCM 106 Skills - Handout - Heimlich ManeuverDocument6 pagesNCM 106 Skills - Handout - Heimlich ManeuverStudentnurseMjPas encore d'évaluation
- Angina PectorisDocument33 pagesAngina PectorisRosse Del MundoPas encore d'évaluation
- Incentive Spirometry1Document4 pagesIncentive Spirometry1Reisha FungoPas encore d'évaluation
- Pathophysilogy of CvaDocument3 pagesPathophysilogy of CvaNursidar Pascual MukattilPas encore d'évaluation
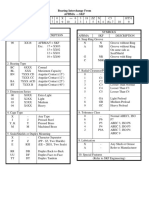
- Stats HandoutDocument1 pageStats HandoutNursidar Pascual MukattilPas encore d'évaluation
- Application of Nursing TheoriesDocument3 pagesApplication of Nursing TheoriesNursidar Pascual Mukattil100% (1)
- Data AnalysisDocument1 pageData AnalysisNursidar Pascual MukattilPas encore d'évaluation
- Two Types of Diabetes MellitusDocument1 pageTwo Types of Diabetes MellitusNursidar Pascual MukattilPas encore d'évaluation
- Data AnalysisDocument1 pageData AnalysisNursidar Pascual MukattilPas encore d'évaluation
- Computers and NursingDocument5 pagesComputers and NursingNursidar Pascual MukattilPas encore d'évaluation
- Diabetes Mellitus: Nhamier M. Jikiri, RN, MD, FPCP Internal MedicineDocument27 pagesDiabetes Mellitus: Nhamier M. Jikiri, RN, MD, FPCP Internal MedicineNursidar Pascual MukattilPas encore d'évaluation
- LET Reviewer MathDocument8 pagesLET Reviewer MathNursidar Pascual MukattilPas encore d'évaluation
- Endocrine Disease Review NotesDocument6 pagesEndocrine Disease Review NotesNursidar Pascual Mukattil100% (2)
- StatisticsDocument3 pagesStatisticsNursidar Pascual MukattilPas encore d'évaluation
- Easy Way To Learn ABGsDocument13 pagesEasy Way To Learn ABGsMunaim TahirPas encore d'évaluation
- Renal FailureDocument17 pagesRenal FailureNursidar Pascual MukattilPas encore d'évaluation
- November 2015 NLE Performance of SchoolsDocument17 pagesNovember 2015 NLE Performance of SchoolsPRC Board100% (1)
- OBE Presentation Department of NursingDocument2 pagesOBE Presentation Department of NursingNursidar Pascual MukattilPas encore d'évaluation
- OBE Presentation Department of NursingDocument2 pagesOBE Presentation Department of NursingNursidar Pascual MukattilPas encore d'évaluation
- Nursing InformaticsDocument13 pagesNursing InformaticsNursidar Pascual MukattilPas encore d'évaluation
- Nursing InformaticsDocument5 pagesNursing InformaticsNursidar Pascual MukattilPas encore d'évaluation
- Computer 101Document4 pagesComputer 101Nursidar Pascual MukattilPas encore d'évaluation
- Overview of Computers and Nursing Nursing InformaticsDocument2 pagesOverview of Computers and Nursing Nursing InformaticsNursidar Pascual MukattilPas encore d'évaluation
- Classroom Rules and RegulationsDocument8 pagesClassroom Rules and RegulationsNursidar Pascual MukattilPas encore d'évaluation
- Basic ISO Setting For DSLRDocument1 pageBasic ISO Setting For DSLRNursidar Pascual MukattilPas encore d'évaluation
- CHED Handbook On Typology, OBE and ISADocument90 pagesCHED Handbook On Typology, OBE and ISAAlfonse Sarmiento100% (2)
- Personal Data SheetDocument4 pagesPersonal Data SheetLeonil Estaño100% (7)
- News Broadcasting ScriptDocument8 pagesNews Broadcasting ScriptNursidar Pascual MukattilPas encore d'évaluation
- Blood Type Compatibility A, B, AB, ODocument2 pagesBlood Type Compatibility A, B, AB, ONursidar Pascual MukattilPas encore d'évaluation
- Snellen Eye ExamDocument5 pagesSnellen Eye ExamNursidar Pascual MukattilPas encore d'évaluation
- Phenomenological Studies: Qualitative ResearchDocument21 pagesPhenomenological Studies: Qualitative Researchshaer_nahyarPas encore d'évaluation
- Medical AbbreviationsDocument2 pagesMedical AbbreviationsNursidar Pascual MukattilPas encore d'évaluation
- ABG Analysis in Simple WayDocument1 pageABG Analysis in Simple WayNursidar Pascual MukattilPas encore d'évaluation
- Sap Ewm OverviewDocument11 pagesSap Ewm OverviewsachinPas encore d'évaluation
- BIF-V Medium With Preload: DN Value 130000Document2 pagesBIF-V Medium With Preload: DN Value 130000Robi FirdausPas encore d'évaluation
- Reynold A. Nicholson - The Mystics of IslamDocument65 pagesReynold A. Nicholson - The Mystics of IslamLuminon SamanPas encore d'évaluation
- Arts Class: Lesson 01Document24 pagesArts Class: Lesson 01Lianne BryPas encore d'évaluation
- Nomenclatura SKFDocument1 pageNomenclatura SKFJuan José MeroPas encore d'évaluation
- Medical GeneticsDocument4 pagesMedical GeneticsCpopPas encore d'évaluation
- Azure Machine Learning StudioDocument17 pagesAzure Machine Learning StudioNurain IsmailPas encore d'évaluation
- CS402 Mcqs MidTerm by Vu Topper RMDocument50 pagesCS402 Mcqs MidTerm by Vu Topper RMM. KhizarPas encore d'évaluation
- Indoor Air Quality Standard Procedures - 2014 RevDocument12 pagesIndoor Air Quality Standard Procedures - 2014 RevFioriAmeliaHathawayPas encore d'évaluation
- Esterification Oil of WintergreenDocument8 pagesEsterification Oil of WintergreenMaria MahusayPas encore d'évaluation
- 331-10 331 Operators Manual enDocument12 pages331-10 331 Operators Manual enYahir VidalPas encore d'évaluation
- Multi Organ Dysfunction SyndromeDocument40 pagesMulti Organ Dysfunction SyndromeDr. Jayesh PatidarPas encore d'évaluation
- Resume: Satyam KumarDocument3 pagesResume: Satyam KumarEr Satyam Kumar KrantiPas encore d'évaluation
- The Spirit Controlled Life Ebook PDF 1Document184 pagesThe Spirit Controlled Life Ebook PDF 1Okesola AbayomiPas encore d'évaluation
- Chillers VoltasDocument4 pagesChillers Voltasanil shuklaPas encore d'évaluation
- Adriano Costa Sampaio: Electrical EngineerDocument3 pagesAdriano Costa Sampaio: Electrical EngineeradrianorexPas encore d'évaluation
- Pusheen With Donut: Light Grey, Dark Grey, Brown, RoséDocument13 pagesPusheen With Donut: Light Grey, Dark Grey, Brown, RosémafaldasPas encore d'évaluation
- Veronte Autopilot Kit DatasheetDocument2 pagesVeronte Autopilot Kit DatasheetEkmedzicPas encore d'évaluation
- Region 1 - Concreting Works Materials Prices - PHILCON PRICESDocument9 pagesRegion 1 - Concreting Works Materials Prices - PHILCON PRICESMark Gregory RimandoPas encore d'évaluation
- Data SiEMEx School SafetyPreparedness 25 26 NOVDocument81 pagesData SiEMEx School SafetyPreparedness 25 26 NOVSuraj RajuPas encore d'évaluation
- Yoga SadhguruDocument6 pagesYoga Sadhgurucosti.sorescuPas encore d'évaluation
- Harmonic Analysis of Separately Excited DC Motor Drives Fed by Single Phase Controlled Rectifier and PWM RectifierDocument112 pagesHarmonic Analysis of Separately Excited DC Motor Drives Fed by Single Phase Controlled Rectifier and PWM RectifierGautam Umapathy0% (1)
- Case 445Document4 pagesCase 445ForomaquinasPas encore d'évaluation
- Aquaculture Scoop May IssueDocument20 pagesAquaculture Scoop May IssueAquaculture ScoopPas encore d'évaluation
- Bulk Material/Part Ppap Process Checklist / Approval: Required?Document32 pagesBulk Material/Part Ppap Process Checklist / Approval: Required?krds chidPas encore d'évaluation
- Tabla de Avances de AcesoriosDocument3 pagesTabla de Avances de AcesoriosPedro Diaz UzcateguiPas encore d'évaluation
- Lima Indiana Oil FieldDocument32 pagesLima Indiana Oil FieldCHARLES PATULAYPas encore d'évaluation
- Ict 2120 Animation NC Ii Week 11 20 by Francis Isaac 1Document14 pagesIct 2120 Animation NC Ii Week 11 20 by Francis Isaac 1Chiropractic Marketing NowPas encore d'évaluation
- Bagpipe LV 1-5Document228 pagesBagpipe LV 1-5Sathia Kdms100% (2)
- CCNA Training New CCNA - RSTPDocument7 pagesCCNA Training New CCNA - RSTPokotete evidencePas encore d'évaluation