Académique Documents
Professionnel Documents
Culture Documents
Keratoconus Jurnal
Transféré par
Azisah Soraya AzisDescription originale:
Copyright
Formats disponibles
Partager ce document
Partager ou intégrer le document
Avez-vous trouvé ce document utile ?
Ce contenu est-il inapproprié ?
Signaler ce documentDroits d'auteur :
Formats disponibles
Keratoconus Jurnal
Transféré par
Azisah Soraya AzisDroits d'auteur :
Formats disponibles
Graefes Arch Clin Exp Ophthalmol (2011) 249:8992 DOI 10.
1007/s00417-010-1423-9
CORNEA
Anterior stromal puncture for treatment of contact lens-intolerant keratoconus patients
Su Yeon Kang & Young Kee Park & Jong-Suk Song & Hyo Myung Kim
Received: 18 February 2010 / Revised: 9 May 2010 / Accepted: 14 May 2010 / Published online: 13 July 2010 # Springer-Verlag 2010
Abstract Purpose To report the results and effectiveness of anterior stromal puncture for contact lens-intolerant keratoconus patients with subepithelial fibrotic nodules. Methods Nine eyes of nine keratoconus patients who were rigid gas-permeable contact lenses (RGP)-intolerant due to subepithelial nodular scars were included in this study. The nine patients were enrolled in the study between March 2008 and December 2008. After confirming nodular elevation from slit-lamp biomicroscopy, the area where the epithelium of nodular scars had sloughed was punctured by anterior stromal puncture using a 26-gauge needle attached to a 1-ml syringe under slit-lamp biomicroscopy. The RGPs of all patients were refitted around 4 weeks after the puncture. Results Five of the nine patients were male, and the average patient age was 29.6 years (SD5.22 years). Mean follow-up time was 13.7 months (SD4.8 months), and the epithelial defect healed in 1.4 days on average. After the puncture, four of nine patients presented with a recurrent erosion of the nodule during follow-up and needed a second puncture. All the patients showed good contact lens
tolerance and satisfactory contact lens fit. No complications such as corneal perforation or keratitis developed. Conclusions Anterior stromal puncture using a 26-gauge needle can be a successful and effective method to induce corneal epithelium and Bowmans layer reattachment. It can be used as an outpatient procedure to improve RGP tolerance in patients with keratoconus with elevated subepithelial nodules. Keywords Anterior stromal puncture . Keratoconus . Keratoconus nodules . Contact lens intolerant
The authors have no proprietary, commercial, or financial interests in any of the products described in this study. S. Y. Kang : J.-S. Song : H. M. Kim (*) Department of Ophthalmology, Guro Hospital, Korea University College of Medicine, 80, Guro-dong, Guro-gu, Seoul 152-703, South Korea e-mail: hyomkim@korea.ac.kr S. Y. Kang e-mail: ligaya97@naver.com Y. K. Park Dr. Lee&Parks Eye Clinic, Seoul, South Korea
Keratoconus is a noninflammatory condition where the cornea assumes a conical shape because of thinning and protrusion of the corneal stroma [1]. The corneal thinning induces irregular astigmatism, myopia, and protrusion, leading to mild to marked impairment in the quality of vision. Symptoms are highly variable and, in part, depend on the stage of progression of the disorder [1]. Early in the disease, there may be no symptoms, but in advanced disease there is significant distortion of vision accompanied by profound visual loss [1]. The management of keratoconus varies depending on the stage of progression of the disease. In very early keratoconus cases, spectacles may provide adequate visual correction, but because spectacles do not conform to the unusual shape of the cornea and the resultant induced irregular astigmatism, contact lenses provide better correction, and are therefore the mainstay of therapy in keratoconus [1]. About 80% of all patients with keratoconus use spectacles, soft toric contact lenses, or rigid gas-permeable contact lenses (RGPs; the majority of patients) to successfully correct their vision [2]. However, contact lens intolerance in keratoconus sometimes occurs due to the formation of raised subepithelial nodular scars [3, 4]. These subepithelial nodular scars, which are also referred to as proud nebulae [3], are
90
Graefes Arch Clin Exp Ophthalmol (2011) 249:8992
typically at or near the apex of the cone [5]. These nodules can result in contact lens intolerance because of recurrent erosions and discomfort [6]. Although the erosions heal after a period without contact lens wear, the nodules remain elevated and may persist even after prolonged periods without lens wear [7]. Patients with these nodules often require more invasive procedures, including corneal transplantation, to correct their vision. Various treatment options have been used to treat these nodular scars successfully, including manual superficial keratectomy and excimer laser phototherapeutic keratectomy (PTK) [4, 6, 8, 9]. Although successful, these techniques require expensive equipment in an operative setting. In this study, we investigated the efficacy of anterior stromal puncture under slit-lamp biomicroscopy for treatment of recurrent corneal erosions, with the rationale that the puncture would enhance adherence of the epithelium to the basement membrane [10]. To the best of our knowledge, this is the first report of successful treatment of subepithelial nodules in keratoconus using anterior stromal puncture.
the sloughed epithelium of the elevated nodular scars, multiple anterior stromal punctures were made to the elevated nodular scar area under slit-lamp biomicroscopy while the patient was in a seated position. The number of punctures varied according to the size of the area. We used a bent 26-gauge (0.10.2 mm turned end) needle attached to a 1-ml disposable syringe. After the treatment, an antibiotic eyedrop (Cravit, levofloxacin 0.5%, Santen) was instilled, and an eye patch was worn until the day after the procedure. The patients were instructed to follow-up daily until the epithelium had healed, and to use antibiotic eyedrops every 6 hours for 1 week for prophylaxis. All the patients were refitted with RGPs approximately 4 to 6 weeks after the procedure, which is when we expected surgical healing to be complete and the scar to have formed.
Results We investigated nine eyes from five men and four women (Table 1). The mean age of the patients was 29.6 years 5.22 (SD) (range 22 to 36 years). The mean follow-up time was 13.7 months 4.8 (SD). Patients experienced no pain during the procedure, and reported minimal discomfort for up to 24 hours after the procedure, with no requests for analgesics. The epithelial defects healed in 1.4 days on average (range 12 days), and four of the nine eyes had an epithelial defect on the first post-procedure day. In all cases, successful anterior stromal punctures were performed; no complications such as corneal perforation or keratitis developed. Approximately 4 to 6 weeks after the procedure, all patients were refitted with RGPs and achieved corrected visual acuity. However, four of nine patients developed a recurrent erosion of subepithelial nodule after RGP refitting, and required a second puncture. The procedure was reported in all these patients as described above, and no further recurrences were observed during the follow-up period. No patients underwent penetrating keratoplasty during the follow-up period.
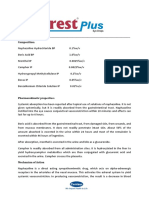
Materials and methods Patients were referred from the keratoconus clinic of Dr. Lee&Parks clinic to the the contact lens and cornea department of Ophthalmology, Korea University College of Medicine, Seoul. A total of nine eyes from nine referred keratoconus patients who were RGP-intolerant due to the presence of subepithelial nodules were treated using anterior stromal puncture between March 2008 and December 2008. In all patients, the subepithelial nodules were slightly down to the visual axis, and had failed to flatten either on refitting or discontinuing contact lens wear. Contact lenses were fitted according to the three-point touch technique with a light apical touch. All patients had previously worn RGP lenses and had achieved good visual acuity with these lenses. On slit-lamp examination, we confirmed the presence of an elevated subepithelial nodule with sloughed epithelium near the apex of the cone in all patients (Fig. 1a, b). Corneal topography (ORBScan, Orbttek Inc.) was performed for all cases. However, useful data was not obtained in some patients because of the irregularity of the tear film and epithelium. Informed consent was provided by all study participants, and the principles outlined in the Declaration of Helsinki were followed in this study. Procedure for anterior stromal puncture A topical anesthetic eyedrop (Alcaine, proparacaine hydrochloride 0.5%, Alcon) was instilled. After confirming
Discussion To remove keratoconus subepithelial nodules and to improve contact lens intolerance, several treatment options have been reported, including manual superficial keratectomy and excimer laser phototherapeutic keratectomy (PTK) [3, 69]. Excimer laser PTK is a successful treatment procedure for anterior corneal pathology, and has several advantages over surgical excision [3, 6]. Laser patients experience much less postoperative pain, and the resultant wound is much smaller and more regular than that made during surgical excision [3]. An early report by
Graefes Arch Clin Exp Ophthalmol (2011) 249:8992
91
Fig. 1 a. Slit-lamp photographs of a subepithelial nodule in a patient with keratoconus before anterior stromal puncture. Note the elevated nodule at the apex of cone (slit lamp; slit view, 16). b Fluorescein staining in the subepithelial scar area due to elevated epithelium of the nodule
Steinert and Puliafito [9] stated that PTK could be used to successfully remove keratoconus nodules. These authors reported that the patient was able to refit his/her contact lens 2 weeks after the procedure, with a visual acuity of 20/ 25; this visual acuity remained stable for the entire 6-week follow-up period. In another study by Moodaley et al. [3],. excimer laser PTK was used to remove keratoconus nodules in ten patients, and seven patients were able to resume regular contact lens wear within 1 month of completion of treatment. All patients achieved a postoperative visual acuity of 6/12 or better with a contact lens at the end of the 8-month follow-up period. Elsahn et al. [6]. recently reported on a larger series of 15 patients with a longer follow-up period of 23 months who underwent successful PTK for keratoconus nodules. However, several investigators have reported a variety of complications after PTK procedures. Lahners et al. [5]. reported a case of keratolysis following PTK for a subepithelial nodule in a patient with keratoconus; progressive keratolysis led to a central descemetocele. Infections such as bacterial keratitis [11] and herpes simplex keratitis [12] have also been reported, though the incidence of these is low. In some patients, a hyperopic shift induced by PTK has been observed [13, 14]. Other possible complications after the PTK procedure include delayed reepithelialization and recurrent erosions, scarring, and irregular astigmatism [15, 16].
Table 1 Preoperative patient data
In this study, we report the successful treatment of subepithelial nodules in the eyes of nine keratoconus patients, using anterior stromal puncture with a 26-gauge needle. Anterior stromal puncture is a treatment used for recurrent corneal erosions, as the punctures enhance epithelium adhesion to the basement membrane due to scar formation [10]. Anterior stromal puncture has some advantages over PTK for treating recurrent corneal erosion. It can be performed in an outpatient and office setting without the requirement for expensive equipment like an excimer laser; there is a very low risk of inducing visually significant corneal scarring and hyperopic shifts, and the epithelial healing time is much shorter [17]. In keratoconus patients, contact lens wear usually abrades the epithelium of the subepithelial nodule, and the patient may be unable to wear the contact lens because of discomfort [3]. In all cases in this study, we confirmed that sloughed epithelium from the subepithelial nodule made contact lens intolerable, and made anterior stromal punctures to ensure more secure bonding of the epithelium, similar to the treatment used for recurrent corneal erosion patients. In conclusion, anterior stromal puncture using a 26gauge needle is a successful and effective method for inducing corneal epithelium and Bowmans layer reattachment. This procedure can improve RGP tolerance in patients with keratoconus with elevated subepithelial nodules in an outpatient office setting.
Patient No 1 2 3 4 5 6 7 8 9
Age (years) 33 30 30 36 23 26 22 31 25
Sex M F F F M M M M F
Eye OS OD OS OD OS OD OS OS OS
K1 59.2 71.1 Notb 64.0 Not 51.7 Not 65.9 Not
Axis 140 5 4 109 106 -
K2 53.7 65.6 59.1 47.4 56.0 -
Axis 50 95 94 19 16 -
VAa (with RGP) 20/25 20/25 20/25 20/40 20/30 20/20 20/25 20/25 20/25
VA, visual acuity Not applicable due to irregular corneal surface
92
Graefes Arch Clin Exp Ophthalmol (2011) 249:8992 9. Steinert RF, Puliafito CA (1990) Excimer laser phototherapeutic keratectomy for a corneal nodule. Refract Corneal Surg 6:352 10. Malecha MA (2004) Anterior stromal puncture for recurrent corneal erosion after laser in situ keratomileusis. J Cataract Refract Surg 30:496498 11. Al-Rajhi AA, Wagoner MD, Badr IA, al-Saif A, Mahmood M (1996) Bacterial keratitis following phototherapeutic keratectomy. J Refract Surg 12:123127 12. Lu CK, Chen KH, Lee SM, Hsu WM, Lai JY, Li YS (2006) Herpes simplex keratitis following excimer laser application. J Refract Surg 22:509511 13. Doqru M, Katakami C, Yamanaka A (2001) Refractive changes after excimer laser phototherapeutic keratectomy. J Cataract Refract Surg 27:686692 14. Gartry D, Kerr Muir M, Marshall J (1991) Excimer laser treatment of corneal surface pathology: a laboratory and clinical study. Br J Ophthalmol 75:258269 15. Das S, Langenbucher A, Seitz B (2005) Delayed healing of corneal epithelium after phototherapeutic keratectomy for lattice dystrophy. Cornea 24:283287 16. Fagerholm P (2003) Phototherapeutic keratectomy: 12 years of experience. Acta Ophthalmol Scand 81:1932 17. Das S, Seitz B (2008) Recurrent corneal erosion syndrome. Surv Ophthalmol 53:315
References
1. Rabinowitz YS (1998) Keratoconus. Surv Ophthalmol 42:297319 2. Belin MW (1988) Optical and Surgical Correction of Keratoconus. Focal Points: Clinical Modules for Ophthalmologists, Vol 4. AAO, San Francisco 3. Moodaley L, Liu C, Woodward EG, OBrart D, Muir MK, Buckley R (1994) Excimer laser superficial keratectomy for proud nebulae in keratoconus. Br J Ophthalmol 78:454457 4. Dana MR, Putz JL, Viana MA, Sugar J, McMahon TT (1992) Contact lens failure in keratoconus management. Ophthalmology 99:11871192 5. Lahners WJ, Russell B, Grossniklaus HE, Stulting RD (2001) Keratolysis following excimer laser phototherapeutic keratectomy in a patient with keratoconus. J Refract Surg 17:555558 6. Elsahn AF, Rapuano CJ, Antunes VA, Abdalla YF, Cohen EJ (2009) Excimer laser phototherapeutic keratectomy for keratoconus nodules. Cornea 28:144147 7. Moodaley L, Buckley RJ, Woodward EG (1991) Surgery to improve contact lens wear in keratoconus. CLAO J 17:129131 8. Ward MA, Artunduaga G, Thompson KP, Wilson LA, Stulting RD (1995) Phototherapeutic keratectomy for treatment of nodular subepithelial corneal scar in patients with keratoconus who are contact lens intolerant. CLAO J 21:130132
Vous aimerez peut-être aussi
- Shoe Dog: A Memoir by the Creator of NikeD'EverandShoe Dog: A Memoir by the Creator of NikeÉvaluation : 4.5 sur 5 étoiles4.5/5 (537)
- Grit: The Power of Passion and PerseveranceD'EverandGrit: The Power of Passion and PerseveranceÉvaluation : 4 sur 5 étoiles4/5 (587)
- ATB and RSVDocument6 pagesATB and RSVAzisah Soraya AzisPas encore d'évaluation
- Cover Jurnal ReadingDocument1 pageCover Jurnal ReadingAzisah Soraya AzisPas encore d'évaluation
- ATB and RSVDocument6 pagesATB and RSVAzisah Soraya AzisPas encore d'évaluation
- Anatomi dan batas batas ginjalDocument4 pagesAnatomi dan batas batas ginjalAzisah Soraya AzisPas encore d'évaluation
- Anatomi dan batas batas ginjalDocument4 pagesAnatomi dan batas batas ginjalAzisah Soraya AzisPas encore d'évaluation
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceD'EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceÉvaluation : 4 sur 5 étoiles4/5 (890)
- The Yellow House: A Memoir (2019 National Book Award Winner)D'EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Évaluation : 4 sur 5 étoiles4/5 (98)
- The Little Book of Hygge: Danish Secrets to Happy LivingD'EverandThe Little Book of Hygge: Danish Secrets to Happy LivingÉvaluation : 3.5 sur 5 étoiles3.5/5 (399)
- On Fire: The (Burning) Case for a Green New DealD'EverandOn Fire: The (Burning) Case for a Green New DealÉvaluation : 4 sur 5 étoiles4/5 (73)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeD'EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeÉvaluation : 4 sur 5 étoiles4/5 (5794)
- Never Split the Difference: Negotiating As If Your Life Depended On ItD'EverandNever Split the Difference: Negotiating As If Your Life Depended On ItÉvaluation : 4.5 sur 5 étoiles4.5/5 (838)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureD'EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureÉvaluation : 4.5 sur 5 étoiles4.5/5 (474)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryD'EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryÉvaluation : 3.5 sur 5 étoiles3.5/5 (231)
- The Emperor of All Maladies: A Biography of CancerD'EverandThe Emperor of All Maladies: A Biography of CancerÉvaluation : 4.5 sur 5 étoiles4.5/5 (271)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreD'EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreÉvaluation : 4 sur 5 étoiles4/5 (1090)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyD'EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyÉvaluation : 3.5 sur 5 étoiles3.5/5 (2219)
- Team of Rivals: The Political Genius of Abraham LincolnD'EverandTeam of Rivals: The Political Genius of Abraham LincolnÉvaluation : 4.5 sur 5 étoiles4.5/5 (234)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersD'EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersÉvaluation : 4.5 sur 5 étoiles4.5/5 (344)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaD'EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaÉvaluation : 4.5 sur 5 étoiles4.5/5 (265)
- The Unwinding: An Inner History of the New AmericaD'EverandThe Unwinding: An Inner History of the New AmericaÉvaluation : 4 sur 5 étoiles4/5 (45)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)D'EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Évaluation : 4.5 sur 5 étoiles4.5/5 (119)
- Her Body and Other Parties: StoriesD'EverandHer Body and Other Parties: StoriesÉvaluation : 4 sur 5 étoiles4/5 (821)
- Iqvia Institute General Use of Medicines 2024 For WebDocument60 pagesIqvia Institute General Use of Medicines 2024 For Webaguiar.jessicapPas encore d'évaluation
- INNOVATIVE CARE LINEDocument4 pagesINNOVATIVE CARE LINEJose Luis Paez NeiraPas encore d'évaluation
- Mini Question Bank - Vety Sci - For Students PDFDocument106 pagesMini Question Bank - Vety Sci - For Students PDFRakesh Prajapati100% (3)
- Replacing ESR with Plasma ViscosityDocument6 pagesReplacing ESR with Plasma ViscosityRyan ChenPas encore d'évaluation
- Hospital Job DescriptionsDocument48 pagesHospital Job DescriptionsLoresita Amoranto Rebong RNPas encore d'évaluation
- Reading Sub-Test: Answer Key - Part ADocument23 pagesReading Sub-Test: Answer Key - Part AAlwin BrightPas encore d'évaluation
- Pink Panther - Diabetes Management - Chapter 9Document16 pagesPink Panther - Diabetes Management - Chapter 9jennmoyerPas encore d'évaluation
- Overdentures Improve Chewing Efficiency and Bone SupportDocument8 pagesOverdentures Improve Chewing Efficiency and Bone SupportMezo SalahPas encore d'évaluation
- Bell's PalsyDocument12 pagesBell's PalsyMercy nafulaPas encore d'évaluation
- Boys Centile ChartDocument1 pageBoys Centile ChartElma AprilliaPas encore d'évaluation
- Nervous SystemDocument8 pagesNervous Systemfadedphotograph12340Pas encore d'évaluation
- Treatment Head LiceDocument26 pagesTreatment Head LiceCherry Amor Betita MadronaPas encore d'évaluation
- Guava Soap Cures AcneDocument10 pagesGuava Soap Cures AcneAubrey VaflorPas encore d'évaluation
- Medical Council of Inida Declaration Form 2010-2011for FacultyDocument9 pagesMedical Council of Inida Declaration Form 2010-2011for FacultydrtpkPas encore d'évaluation
- Ocurest Plus2018Document4 pagesOcurest Plus2018rotastrainPas encore d'évaluation
- 5-Week Candida Weight Loss ProgramDocument174 pages5-Week Candida Weight Loss ProgramAnd100% (1)
- MHGap Intervention Guide PDFDocument107 pagesMHGap Intervention Guide PDFfundj22100% (1)
- Inamsc Literature Review Dg1fQQFe Guideline INAMSC 2018Document20 pagesInamsc Literature Review Dg1fQQFe Guideline INAMSC 2018DevinPas encore d'évaluation
- Semen AnalysisDocument2 pagesSemen AnalysisSabir KamalPas encore d'évaluation
- CLONE - Chinoike Clan - The HomebreweryDocument7 pagesCLONE - Chinoike Clan - The Homebreweryrashid jones100% (1)
- Advances in Psychological and Social Support After DisastersDocument149 pagesAdvances in Psychological and Social Support After DisastersjprewittdiazPas encore d'évaluation
- Types of Casts and Their IndicationsDocument3 pagesTypes of Casts and Their IndicationsPhylum ChordataPas encore d'évaluation
- MCI - SyllabusDocument11 pagesMCI - Syllabusintaa khabPas encore d'évaluation
- Hands Only CPRDocument7 pagesHands Only CPRJulisa FernandezPas encore d'évaluation
- DPD ResumeDocument3 pagesDPD Resumeapi-272384986Pas encore d'évaluation
- The Medication Order Unit 11Document10 pagesThe Medication Order Unit 11novie100% (2)
- Narcotic Drugs: Opium Herion Codeine Tramadol MorphineDocument9 pagesNarcotic Drugs: Opium Herion Codeine Tramadol MorphineSyed renobaPas encore d'évaluation
- Manila Standard Today - Friday (September 14, 2012) IssueDocument22 pagesManila Standard Today - Friday (September 14, 2012) IssueManila Standard TodayPas encore d'évaluation
- Akf Stok 13Document67 pagesAkf Stok 13Grace Riani Pongsipulung TariganPas encore d'évaluation
- Thulium e Alopecia AndrogenéticaDocument9 pagesThulium e Alopecia AndrogenéticacristiannePas encore d'évaluation