Académique Documents
Professionnel Documents
Culture Documents
Ethics Curriculum Emergency Medicine
Transféré par
Angkat Prasetya Abdi NegaraDescription originale:
Copyright
Formats disponibles
Partager ce document
Partager ou intégrer le document
Avez-vous trouvé ce document utile ?
Ce contenu est-il inapproprié ?
Signaler ce documentDroits d'auteur :
Formats disponibles
Ethics Curriculum Emergency Medicine
Transféré par
Angkat Prasetya Abdi NegaraDroits d'auteur :
Formats disponibles
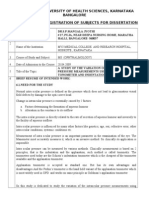
Ethics Curriculum for Emergency Medicine Residencies
1994
SAEM Ethics Committee James G Adams Terri A Schmidt (Chair Arthur R !erse Glenn C "reas #e$is R Goldfran% &enneth ' (serson )orm ! &al*fleisch Samuel M &eim Ro*ert & &no++ Gregory # #ar%in Marc # ,ollac% !a-id , S%lar
Table of Contents (. ((. (((. (ntroduction/ 0asic Ethical "oundations of Clinical Medicine A++lying Ethics to Emergency Medicine (ssues Related to ,atient Autonomy A. (nformed Consent and Refusal 0. ,atient !ecision Ma%ing Ca+acity C. Treatment of Minors !. Ad-ance !irecti-es ('. End of #ife !ecisions A. #imiting Resuscitation 0. "utility '. The ,hysician1,atient Relationshi+ A. Confidentiality 0. Truth Telling and Communication C. Com+assion and Em+athy '(. (ssues Related to Justice A. 2ealth Care Rationing 0. !uty C. Moral (ssues in !isaster Medicine !. Research '((. Teaching '(((. ,hysician Relationshi+s $ith the 0iomedical (ndustry
The +ur+ose of this manual is to +ro-ide a teaching guide to residency directors and others res+onsi*le for teaching ethics to emergency medicine residents. The goal is to +ro-ide residents $ith the information necessary to *e a*le to ma%e a reasoned analysis of ethical conflicts and to allo$ them to de-elo+ the s%ill to resol-e ethical dilemmas in an a++ro+riate manner. After an introductory section3 the manual is di-ided into teaching modules. Each module includes o*4ecti-es3 an illustrati-e case3 a discussion3 study 5uestions3 and a *rief *i*liogra+hy. The o*4ecti-es define *asic material a resident $ould *e e6+ected to master after each session. The study 5uestions can *e used to focus discussion3 +ro-ide *road understanding of the su*4ect3 and stimulate thought. Most of the 5uestions may not ha-e one correct ans$er. #i%e all of medicine3 *iomedical ethics is continually e6+anding. )o effort is made to co-er all as+ects of each su*4ect3 *ut rather3 an attem+t $as made to offer a short3 +ertinent analysis for *oth the instructor and the resident. This is not intended to *e a com+lete te6t on ethics in emergency medicine3 *ut a curriculum guide. This guide includes modules $hich can *e taught to emergency medicine residents throughout their training. 0efore s+ecific ethical issues are discussed3 the relationshi+ *et$een ethics and the la$ must *e clarified. ,hysicians must loo% to the la$ for guidance3 *ut the la$ does not +ro-ide the ans$er to many ethical +ro*lems. (n addition3 statutes may -ary su*stantially *et$een states. Ethical theory should guide +hysicians to$ard a uni-ersally a++lica*le standard. The la$ may *e am*iguous3 so no clear guidance is offered3 or it might *e -ery s+ecific3 a++lying only to cases $ith su*stantially similar circumstances. The la$ also neither addresses the *readth of ethical im+erati-es $hich o*ligate emergency +hysicians nor does it necessarily reflect ethical *eha-ior. 7hile the la$ is limited in its a*ility to +ro-ide uni-ersal
guidance and direction3 ethical analysis should +ro-ide a frame$or% for determining moral duty3 o*ligation and conduct. Similarly3 ethical analysis does not su*stitute for a++ro+riate legal guidance. 7hen dealing $ith dilemmas3 $hen initiating +olicy and +rotocols3 or $hen u+dating e6isting +rocedures3 informed legal ad-ice is encouraged. An attorney familiar $ith emergency medicine and $ell1-ersed in rele-ant statutory and case la$ $ill hel+ to define legally acce+ta*le actions. Bibliography Ales  Charlson ME3 7illiams1Russo ,3 Allengrante J,/ 8sing faculty consensus to de-elo+ and im+lement a medical ethics course. Academic Medicine 1999:;</4=;1 4=>. Crimmins TJ/ Ethics3 la$3 and emergency medicine. Minnesota Medicine 19>>:<1/<=>1<1=. Mos%o+ JC3 Mitchell JM3 Ray 'G/ An ethics curriculum for teaching emergency medicine residents. Ann Emerg Med 199=: 19/1><1199. Strong C3 Commelly JE3 "orro$ #/ Teachers? +erce+tions of difficulties in teaching ethics in residencies. Academic Medicine 1999:;</@9>14=9. 7inden$erder 7/ Ethical dilemmas for housestaff +hysicians. JAMA 19>A:9A4/@4A41 @4A<.
I. Basic Ethical Foundation of Clinical Medicine Objectives 1. !iscuss the moral +rinci+les that underlie the +ractice of medicine. 9. !efine ethics. @. !efine res+ect for autonomy. 4. !efine +aternalism. A. !efine *eneficence. ;. !efine non1maleficence. <. !efine 4ustice.
Ethics studies -alues and moral reasoning. )on1normati-e ethics descri*es and analyBes moral *eliefs $ithout ma%ing a -alue 4udgement a*out right and $rong. )ormati-e ethics attem+ts to define actions that are right and $rong. (n medicine3 the ethical challenge may include deciding *et$een the lesser of t$o e-ils or the greater of t$o goods. ,u*lic +olicy3 formal codes3 guidelines3 regulations and clinical decision ma%ing should *e *ased on an ethical foundation. "our +rinci+les are commonly thought to define $estern health care ethics/ res+ect for autonomy3 *eneficence3 nonmaleficence and 4ustice. The +riority each is gi-en is determined *y the situation. )o +rinci+le al$ays ta%es +recedence o-er another. 0eneficence and nonmaleficence are ancient tenants of health care ethics em*odied in the #atin Primium non nocere3 Ca*o-e all do no harmC. 7hile some moral +hiloso+hers ma%e no distinction *et$een *eneficence and nonmaleficence3 others feel that a distinction should *e made. 0eneficence can *e -ie$ed as a +ositi-e action and nonmaleficence as an a-oidance of a negati-e action. Thus3 at a minimum3 +hysicians must not act in a $ay $hich is detrimental to +atients.
0eneficence re5uires +hysicians to act in the *est interests of their +atients. ,hysicians must *alance goods and +otential harms and act in the *est interests of the +atient. 0eneficence is em*odied in the 2i++ocratic +hysician?s +ledge to act for the good of the +atient. There is a s+ecific o*ligation of *eneficence *ased on the health +ro-ider1+atient relationshi+. This is a contractual3 fiduciary o*ligation3 yet the +rofessional?s o*ligation to *enefit a +atient is not *ased on the +rofessional?s e6+ectation of recei-ing *enefits from the +atient. The o*ligation to act in the *est interest of the +atient is a fundamental +art of the role of the +hysician. ,resent day ethics codes strongly em*ody the guiding +rinci+le of *eneficence. The !eclaration of Gene-a3 s$orn *y many medical students at graduation3 states3 Cthe health of my +atient $ill *e my first considerationC (7orld Medical Association3 19>@ . Autonomy is deri-ed from t$o Gree% root $ords3 autos and nomos meaning3 self rule. Res+ect for autonomy in health care ethics has only *ecome +rominent in the last half of the t$entieth century. Changes in our society $hich ha-e encouraged the rise of res+ect for autonomy include the e6+ansion of +olitical democracy3 im+ro-ement in the education of American citiBens3 and an increase in di-ersity of -alues $hich encourages indi-iduals to +rotect their o$n +ersonal -alues. The need to res+ect autonomy $as highlighted *y the a*uses of medical research committed *y )aBi Germany on concentration cam+ -ictims3 the 8S1 Tus%eegee sy+hilis study3 $hich continued into the 19<=s3 and the 8S go-ernment1 s+onsored radiation studies. Res+ect for autonomy is su++orted *y la$. )e$ Dor% State Su+reme Court Justice CardoBa said in 1914 that Cany indi-idual of sound mind has the right to determine $hat shall *e done to his *ody...C 2o$e-er3 informed consent does not a++ear as +art of American case la$ until 19A<. Since then3 the conce+t of +atient autonomy has +ro-en to *e enduring3 and is no$ fundamental.
The final +rinci+le of health care ethics is 4ustice. Justice is the +rinci+le $e consider $hen attem+ting to ma%e decisions a*out com+eting interests3 or allocation of resources. Justice is often e5uated $ith fairness. Aristotle defined it as treating e5uals e5ually3 and une5uals une5ually. Theories of 4ustice ha-e *een descri*ed as deontological and utilitarian. 8tilitarian theories are *ased on the assum+tion that the right action is the action that creates the greatest +ossi*le *alance of good o-er harm. 8tilitarianism has often *een descri*ed as Cthe end 4ustifies the means. !eontological theories are *ased on the *elief that some actions are right or $rong *ased on a higher rule or rules3 not 4ust *ased on the conse5uence of the action. Bibliography 0eaucham+ T# and Childress J"/ ,rinci+les of 0iomedical Ethics @rd ed E6ford 8ni-ersity ,ress3 )e$ Dor%3 19>9. Edelstein3 # (194@ The 2i++ocratic Eath/ Te6t3 Translational (nter+retation 0ulletin of the 2istory of Medicine3 Su++lement 1 0altimore/ The Johns 2o+%ins ,ress3 +. @. (serson &'3 Sanders A03 Mathieu !R3 0uchanan AE (eds / Ethics in Emergency Medicine. 0altimore3 7illiams and 7il%ins3 19>;. Jonsen AR3 Siegler M3 7inslade 7J (eds / Clinical Ethics3 @nd ed. McGra$12ill3 (nc3 )e$ Dor%3 1999. #uce JM/ Ethical +rinci+les in critical care. JAMA 199=:9;@/;9;1<==.
II. Applying Ethics to E Objectives
ergency Medicine
1. #ist s+ecial +ro*lems associated $ith ethical decision1ma%ing in emergency medicine. 9. !escri*e t$o models for ethical decision1ma%ing in emergency medicine. @. #ist ad-antages and disad-antages of the t$o models in emergency medicine. A 99 year old man in acute res+iratory distress is *rought into the emergency de+artment from a nursing home. 2e had *een at the nursing home for ; months and is descri*ed as normally alert and oriented3 *ut *edridden due to his end stage congesti-e heart failure. 2e has no family in the area. 2e a++ears frail and de*ilitated3 and cannot ans$er any 5uestions. 2is *lood +ressure is 9= systolic3 heart rate is 19= and res+iratory rate is 4=. 2e has rales in all lung fields. Records from the nursing home do not +ro-ide any information a*out +atient +references regarding resuscitation or Ccode status.C Shortly after arri-al3 his daughter from out of state calls and states her father $ould not $ant Caggressi-e treatmentC. The E! is not only a com+le6 medical en-ironment3 *ut +resents com+le6 ethical challenges as $ell. Eur unfamiliarity $ith our +atients and their $ishes3 the minimal time to esta*lish a relationshi+3 and the com+le6 situations3 all contri*ute to ethical conflict. (n addition3 decisions must often *e made 5uic%ly3 sometimes *efore sufficient information is a-aila*le. (t is useful to ha-e a model for ma%ing ethical decisions3 4ust as $e use models to ma%e other clinical decisions. Ene such model $as de-elo+ed *y Jonsen3 Siegler and 7inslade. They +ro+ose that any ethical decision can *e made *y considering four factors/ medical indications3 +atient +references3 5uality of life and conte6tual features. The conce+t of medical indications includes the diagnosis and treatment of the +atient?s condition and a consideration of $hat is needed to e-aluate and treat the +ro*lem. The conce+t of +atient +references is *ased on the *elief that health care +ro-iders should res+ect the $ishes of +atients3 and $hene-er +ossi*le +ro-ide treatment $hich meets the +atient?s goals. Fuality of life considerations assume the goal of medical inter-ention is to im+ro-e the 5uality
of the +atient?s life. (t is im+ortant to remem*er that 5uality of life must *e defined from the +atient?s +oint of -ie$3 not the health care +ro-ider?s. "inally3 conte6tual features include all the other factors $hich may *e in-ol-ed in a s+ecific situation such as the $ishes of the family3 the rules of la$3 the effect a decision $ill ha-e on others3 including the health care $or%ers3 and socioeconomic considerations. This model assists in the organiBation of the health care +ro-ider?s thought3 and hel+s a-oid o-erloo%ing any +ertinent as+ect of the situation. Ethical decisions are then made *ased on the +rinci+les of res+ect for autonomy3 *eneficence3 nonmaleficence and 4ustice. This model3 $hile thorough3 may sometimes *e too time consuming to *e hel+ful in emergency settings. (serson has de-elo+ed another model s+ecifically designed to *e hel+ful in the emergency setting. The first ste+ is to as% the 5uestion3 C(s this a ty+e of ethics +ro*lem for $hich you ha-e already $or%ed out a rule or is this at least similar enough so that a rule could reasona*ly *e e6tended to co-er itGC. (f so3 then follo$ the rule. The second ste+ is to as% the 5uestion3 C(s there an o+tion $hich $ill *uy time for deli*eration $ithout e6cessi-e ris% to the +atientGC. (f yes3 *uy time. "inally3 if the first t$o ste+s do not yield a solution3 then there are three rules to a++ly to any ethical decision. The three rules are/ 1. (m+artiality11 the decision ma%er +laces in the +osition of the +atient *y saying3 C7ould you *e $illing to ha-e this action +erformed if you $ere in the +atient?s +laceGC. 9. 8ni-ersaliBa*ility117ould you *e $illing to use the same solution in all similar casesG @. (nter+ersonal 4ustifia*ility11Consider $hether you $ould *e $illing to defend the decision to others3 to share the decision in +u*lic. Emergency +hysicians are *ound *y the same o*ligations and are su*4ect to the same +itfalls as any other +hysician. Just as residents must de-elo+ e6+ertise
and sensiti-ity for clinical decision ma%ing3 e6+ertise must *e concurrently de-elo+ed to address ethical 5uestions. !tudy "uestions 1. (n the a*o-e case3 $hat do you %no$ a*out medical indications3 5uality of life3 +atient +references and conte6tual featuresG 9. 2o$ does that %no$ledge hel+ you to ma%e a decisionG @. 8se the (serson model to hel+ formulate a decision in this situation. Bibliography Adams JG3 Arnold R3 Siminoff #3 7olfson A0/ Ethical conflicts in the +rehos+ital setting. Ann Emerg Med 1999:91/19A9119;A. Jonsen AR3 Siegler M3 7inslade 7J (eds / Clinical Ethics3 9nd ed. )e$ Dor%3 MacMillan3 1999. (serson &'3 Sanders A03 Mathieu !R3 0uchanan AE (eds / Ethics in Emergency Medicine. 0altimore3 7illiams and 7il%ins3 19>;. (serson &'/ Emergency medicine and *ioethics/ a +lan for an e6+anded -ie$. J Emerg Med 1991:9/;A1;;. Schmidt TA/ (nto6icated airline +ilots/ A case *ased ethics model Academic Emergency Medicine 1994: 1/AA1A9.
III. Issues #elated to $atient Autono A. Infor ed Consent Objectives
1. E6+lain $hy informed consent is o*tained for treatment. 9. #ist the critical elements in the consent +rocess. @. !efine the emergency rule. 4. !efine e6+ress consent. A. !efine im+lied consent. ;. !escri*e the circumstances under $hich a +hysician may treat a +atient against his or her $ill. A @9 year old +atient +resents $ith a se-ere headache. The +atient has a history of headaches3 *ut this e+isode is $orse than usual. There is no fe-er3 and the +atient has a non1focal neurological e6amination: the +atient?s sensorium is clear. 2ead CT scan is normal. The +hysician feels that a lum*ar +uncture is indicated.
Res+ect for autonomy re5uires us to recogniBe a +erson?s right to ma%e inde+endent choices3 and ta%e actions *ased on +ersonal -alues and *eliefs. A +erson cannot ma%e inde+endent choices $ithout the necessary information to ma%e those decisions. Thus3 informed consent in-ol-es t$o duties/ the duty to disclose information to +atients3 and the duty to o*tain +atients? consent. 8nderstanding the *asis u+on $hich the +atient grants +ermission for medical treatment is fundamental to effecti-e3 rational and medicolegally acce+ta*le care. (n the emergency care setting issues of consent fre5uently arise in the form of informed consent for +rocedures3 informed refusal of care3 treatment of minors3 and consent for research +rotocols. (nformed consent is intended to +romote +atient self1determination and $ell *eing. Although +atient self1determination im+lies a unilateral decision3 the
+rocess of decision ma%ing is *y necessity a shared one/ the +hysician offers information and e6+ert ad-ice for the +atient to consider. (t is the health care +ro-ider?s res+onsi*ility to assure that the +atient can meaningfully +artici+ate in the decisions. Shared decision ma%ing re5uires that the +atient +ossess correct and com+lete information3 and that the decision +romote the +atient?s goals and life -alues. (n the consent +rocess the three elements that must *e met are information3 com+rehension and -oluntariness. %egal support for infor ed consent
7hile informed consent is fundamentally an ethical im+erati-e3 8nited States la$ re5uires that a +atient +ro-ide informed consent for medical treatment3 e6ce+t under unusual circumstances. This legal +rinci+le $as recogniBed in 1914 $hen the )e$ Dor% State Su+reme Court held that E-ery +erson of adult years and sound mind has the right to determine $hat shall *e done $ith his o$n *ody and a surgeon $ho +erforms an o+eration $ithout his +atient?s consent commits an assault for $hich he is lia*le in damages.
This landmar% case cites the fundamental +remise u+on $hich our understanding is *ased. Any time a health care +ro-ider touches a +atient3 such action must *e authoriBed *y the +atient. (n the a*sence of such authoriBation3 the inter-ention could *e actiona*le in tort as a *attery. The imminent threat of such a -iolation constitutes assault. This +rinci+le gi-es the +atient $ith decision ma%ing ca+acity the legal right to refuse medical care. (n addition3 lac% of informed consent may result in an action for negligence against the health care +ro-ider. A failure to disclose +otential com+lications or alternati-e treatments may constitute negligence if such information $ould influence the +atient to alter his or her decision. This distinction $as made clear in 19<93 $hen the court affirmed that +erforming an unauthoriBed +rocedure is
*attery3 *ut +erforming an authoriBed +rocedure $ithout a++ro+riately disclosing the ris%s constitutes negligence.
The E
ergency #ule The court stated that an emergency e6ce+tion to informed consent e6ists
$hen the +atient is unconscious or other$ise inca+a*le of consenting3 and harm from a failure to treat is imminent and out$eighs any threatened harm *y the +ro+osed treatment. 7hen time does not +ermit informed consent3 emergency ser-ices o+erate under the moral im+erati-e of *eneficence3 acting in the *est interests of the +atient. Courts also ha-e held that in time of life threatening crisis3 it is the +hysician?s duty to do that $hich the occasion demands3 e-en $ithout the consent of the +atient. 2o$e-er3 it is im+erati-e that the condition of the +atient *e so se-ere that definiti-e care could not *e delayed until consent is o*tained. The emergency rule de+ends u+on the +atient?s ina*ility to offer consent as $ell as urgent circumstances. 2o$ urgent a situation is de+ends +rimarily u+on the conse5uences to the +atient of a delay in rendering treatment3 or indeed u+on the conse5uences of a failure to render any treatment at all.
!ubstituted Consent 7hen the +atient is una*le to consent due to +hysical or +sychological distress3 the nearest relati-e or designated surrogate is turned to for consent (see +atient decision1ma%ing ca+acity . (t is then assumed that surrogate decision ma%ers $ill ma%e decisions *ased either on the +atient?s *est interests or the +atient?s +re-iously e6+ressed $ishes.
plied Consent C(m+lied consentC is defined as a logical inference from the conduct of the
+atient. The indi-idual +atient?s actions $ould indicate to the health care +ro-ider that the treatment $as re5uested. This is descri*ed in the case of E?0rien -. Cunard Steamshi+ Co.. A +assenger sued the steamshi+ com+any for administering an immuniBation $ithout his consent. The court held that *y the +laintiff?s act of standing in the line $here in4ections $ere *eing administered3 rolling u+ his slee-e and su*mitting to the in4ection3 he +ro-ided a consent im+lied *y his actions. The ty+ical +rehos+ital or E! encounter may +arallel this situation. The +atient or a designee re5uests hel+3 and care is administered. The +atient im+lies consent as he or she +artici+ates in the care3 and acti-ely su*mits to treatment. E6+ress consent must *e sought for any inter-ention $ith more than remote ris%s. (nformation must *e freely shared $ith +atients. (m+lied consent might e6tend to that necessary to relie-e suffering and +reser-e and +romote the care of the +atient. All such treatment rendered must *e $ell $ithin the sco+e of acce+ted thera+y. (f the +atient is unconscious or $ithout decision ma%ing ca+acity3 the emergency rule su+ersedes. #efusal of Care As e6+lained in other sections3 informed consent re5uires decision ma%ing ca+acity. (t follo$s that +atients $ith decision ma%ing ca+acity ha-e a right not to consent to care. The elements of a -alid3 informed refusal are the same as consent/ the +atient must ha-e decision ma%ing ca+acity3 information including significant ris%s and magnitude of harm must *e +ro-ided3 the +atient must com+rehend the information and the refusal must *e -oluntary $ithout coercion or duress. 0ecause refusal of care may conflict $ith the 4udgement and recommendation of the +hysician3 it is +rudent for the +hysician to em+hasiBe the ris%s +resented *y refusing care and outline s+ecific conse5uences to *e e6+ected. The +hysician
must *e careful *ecause *oth consent and refusal must *e made $ithout coercion or duress. ,hysicians should +ro-ide treatment des+ite a -er*al refusal in +atients $ho do not ha-e decision ma%ing ca+acity3 or $hen the life threat is so acute that the +hysician does not ha-e time to assess their refusal. 7hen +atients do not ha-e decision ma%ing ca+acity3 the e6+ected *enefit of the inter-ention must out$eigh the +otential ris% of harm to the +atient.
!tudy "uestions 1. (n this case3 $hat must *e discussed $ith the +atient in order to o*tain her consentG 9. !o you need to o*tain $ritten consent from this +atientG @. 7hy does a +hysician o*tain informed consent for treatmentG 4. 2o$ do the +rinci+les of *eneficence and autonomy relate to consent issuesG
Bibliography A++lelaum ,S3 #idB C73 Meisel J!/ (nformed Consent/ #egal Theory and Clinical ,ractice E6ford 8ni-ersity ,ress3 )e$ Dor%3 19><. 0oisau*in E'3 !resser R/ (nformed consent in emergency care/ (llusion and reform. Ann Emerg Med 19><: 1;/;91;<. 0roc% !7/ (nformed +artici+ation and decisions in (serson &'3 Sanders A03 Mathieu !R3 0uchanan AE (eds / Ethics in Emergency Medicine. 0altimore3 7illiams and 7il%ins3 19>;. S+rung C#3 7inic% 0J/ (nformed consent in theory and +ractice/ legal and medical +ers+ecti-es on the informed consent doctrine and a +ro+osed reconce+tualiBation Crit Care Med 19>9: 1</1@4;11@A4.
III. Issues #elated to $atient Autono B. $atient &ecision Ma'ing Capacity Objectives 1. 9. !efine decision ma%ing ca+acity
Contrast medical inter+retations of decision ma%ing ca+acity $ith the legal definition of com+etence.
@. 4.
!efine surrogate decision ma%er and health care +ro6y #ist the $ays decisions can *e made $hen a +atient lac%s decision1 ma%ing ca+acity.
A AA year old male +atient came to an E! com+laining of nausea and chest +ain o-er the +ast t$o hours. An E&G immediately u+on arri-al re-ealed significant (@ mm ST de+ression in an anterio1se+tal distri*ution (' 914 . The +atient?s chest +ain $as relie-ed after a third su*lingual nitroglycerin ta*let $as administered. Su*se5uent E&G re-ealed 119mm ST de+ression. 2e has not seen a +hysician in the +ast A years. 2e ta%es no medications and smo%es 1 +ac% of cigarettes a day. 2e refuses to *e admitted to the hos+ital and demands that he immediately *e released. !es+ite all efforts *y the +hysician to con-ince him to stay3 he demands that he *e allo$ed to go home. 7hen a +atient arri-es in an emergency de+artment and an e-aluation *y a +hysician is *egun3 a +hysician1+atient relationshi+ is esta*lished. This relationshi+ carries certain legal and ethical o*ligations for *oth +arties. The +hysician assesses the +atient and +ro+oses a +lan of e-aluation or a course of care. ,atients ha-e the ultimate authority to acce+t or refuse this +ro+osal. The +atient?s authority is founded on 1 the ethical +rinci+le of res+ect for autonomy3 9 the legal right of self1determination3 and is *ased on the +i-otal assum+tion that the +atient is acting in his or her o$n *est interests. The o*ligation of +hysicians to +rotect +atients from harm can conflict $ith the o*ligation to res+ect +atient autonomy $hen the +atient ma%es decisions that seem un$ise or harmful. 7hen this conflict occurs3 +hysicians must assess the
+atient?s a*ility to ma%e a reasoned decision. Com+etence and decision1ma%ing ca+acity are t$o descri+tors commonly utiliBed to characteriBe this a*ility. The former is a legal term3 the latter a +hrase recently coined that a++lies the conce+t of com+etence to a medical setting.
The Medical Concept of &ecision Ma'ing Capacity
All adult +atients are assumed to ha-e a++ro+riate decision ma%ing ca+acity to acce+t or refuse a +lan of e-aluation or course of thera+y unless there is e-idence o*tained *y history3 *eha-ior3 or +hysical e6amination that $ould lead the +hysician to *elie-e that the +atient?s decision1ma%ing ca+acity has *een significantly com+romised. The determination of decision ma%ing ca+acity re5uires that/ 1. The +atient a++reciates he or she has the +o$er to ma%e decisions on his or her *ehalf 9. The +atient understands the medical situation and +rognosis3 the nature of the recommended e-aluation or care3 the alternati-es3 the ris%s and *enefits of each3 and the li%ely conse5uences @. The +atient?s decision is sta*le o-er time3 and is consistent $ith his or her life -alues or goals. The degree or le-el of decision1ma%ing ca+acity a +atient must sho$ -aries $ith the degree and +ro*a*ility of ris%3 the degree and +ro*a*ility of *enefit3 and the +atient?s decision to consent or refuse. The greater the ris% +osed *y the +atient?s decision3 the more e6acting the standard of decision ma%ing ca+acity needs to *e. Thus3 a +atient might need only a lo$ le-el of decision ma%ing ca+acity to consent to a +rocedure $ith su*stantial3 highly +ro*a*le *enefits and
minimal3 lo$ +ro*a*le ris%s3 *ut a high le-el of decision ma%ing ca+acity to refuse the same treatment.
The Concept of %egal Co
petence
(n the la$3 com+etence re5uires mental ca+acities sufficient to a++reciate the nature and conse5uences of such legal rights or res+onsi*ilities as ma%ing a $ill or contract3 standing trial3 or rearing a child. The degree of understanding re5uired *y the la$ $ill -ary in relation to the tas% to *e +erformed. The la$ assumes that adults are com+etent until +ro-en other$ise in a formal legal decree. Ence the +erson is formally 4udged incom+etent3 a guardian or conser-ator is a++ointed *y the court to ma%e decisions. !e+ending on the degree of incom+etence3 a +erson may *e 4udged incom+etent relati-e to *usiness or financial affairs3 yet com+etent to consent to or refuse medical e-aluation or treatment. (f a conser-ator is a++ointed to ma%e medical decisions on *ehalf of the +atient3 then the conser-ator is the indi-idual $ho must gi-e consent3 not the +atient or mem*ers of his or her family. Each state may ha-e slightly different criteria for the determination of com+etence. 2o$e-er3 it *ears re+eating that a +erson is determined to *e incom+etent only after a formal legal +roceeding.
(hen a $atient %ac's &ecision)Ma'ing Capacity (f the +hysician %no$s that a +atient does not ha-e medical decision1ma%ing ca+acity to gi-e an informed consent3 ho$ should medical decisions *e madeG The ans$er to this 5uestion de+ends on the s+eed $ith $hich the decision must *e made3 and $hat information a*out +atient +references is a-aila*le. (f a decision needs to *e made immediately to sa-e a +erson?s life or lim*3 then legally and ethically3 the emergency +hysician is o*ligated to +ro-ide a++ro+riate care $ithout the need for consent (See Emergency Rule . (f time
+ermits and there is a legal decree that the +atient is incom+etent3 then the emergency +hysician should contact the conser-ator of the +atient $ho $ould ha-e legal res+onsi*ility for medical decision ma%ing. (n addition3 +atients may ha-e a dura*le +o$er of attorney for health care3 li-ing $ill or +re-iously e6+ressed $ishes to family or others $hich should *e honored (see section on ad-ance directi-es . 7hen +atients +re-iously e6+ressed $ishes are %no$n3 *ased on the +rinci+le of res+ect for autonomy3 those $ishes should generally *e honored. 2istorically3 there $as su*stantial ethical and legal consensus su++orting the conce+t of surrogate decision ma%ing *y family mem*ers. 2o$e-er3 recent legal cases suggest that courts may *e less reliant on family mem*ers to act as surrogate decision ma%ers. Still3 each state has la$s that descri*e the hierarchy of authority for family surrogate decision ma%ing. Surrogate decision1ma%ers may *e acce+ta*le in the emergency setting3 *ut the time re5uired to confirm surrogate identity3 e6+lain the medical circumstances and +rognosis3 and assure sound reasoning3 may *e +rohi*iti-e $hen there is a medical im+erati-e to inter-ene. 7hen dou*t e6ists3 a conser-ati-e course (resuscitationHsta*iliBation is $arranted. !tudy "uestions 1. (n the case +resented3 $hat must *e discussed $ith the +atient $hile counselling him regarding his refusalG 9. @. 7hat must you %no$ so that you can ade5uately counsel himG 2o$ $ould you assess $hether the +atient +ossessed ade5uate decision1 ma%ing ca+acityG Bibliography A++le*aum ,S3 Grisso T/ Assessing +atients? ca+acities to consent to treatment. ) Engl J Med 19>>: @19/1;@A11;@>. 0roc%3 ! and 7artman3 SA 7hen com+etent +atients ma%e irrational choices. ) Eng J Med @99/1A9A11A99.
Emanuel3 EJ and Emanuel3 ## ,ro6y decision ma%ing for incom+etent +atients/ An ethical and em+irical analysis. JAMA 1999: 9;</9=;<19=<1. Jonsen AR3 Siegler M3 7inslade 7J (eds / Clinical Ethics3 @nd ed. McGra$12ill3 (nc3 )e$ Dor%3 1999. #o3 0 Assessing decision ma%ing ca+acity. #a$3 Medicine3 and 2ealth Care 199= 1>/@("all 19@19=1. #o 03 Rouse "3 !orn*rand #/ "amily decision ma%ing on trial/ 7ho decides for incom+etent +atientsG ) Engl J Med 199=:@99/199>119@9.
III. Issues #elated to $atient Autono C. Treat ent of inors Objectives* 1. 9. @.
E6+lain ho$ consent for minors is o*tained. E6+lain ho$ the Cemergency ruleC a++lies to minors. E6+lain ho$ state la$s regarding minors and +regnancy3 se6ually transmitted diseases3 su*stance a*use3 and child a*use relate to consent and confidentiality.
4. A.
E6+lain the conce+ts of emanci+ated minors and mature minors. !escri*e situations $hen a minor can refuse care.
A si6teen year old is *rought to the emergency de+artment *y his +arents $ho insist on a drug screen to confirm their sus+icions that the teenager is using mari4uana. The +atient refuses to su*mit to any e6am or +roduce a urine sam+le.
Res+ect for autonomy +resumes that a +erson $ith decision ma%ing ca+acity has a right to ma%e choices a*out health care. 2o$e-er3 minors are generally +resumed not to ha-e decision ma%ing ca+acity. (n general3 consent for treatment of minors is o*tained from the +arent or legal guardian. 7e assume that +arents $ill ma%e decisions *ased on the *est interests of their child. Thus3 $ith minors $e are more li%ely to *ase our actions on the +rinci+le of *eneficence than on the +rinci+le of res+ect for autonomy. 2o$e-er3 as children *ecome old enough to e6+ress their $ishes and reason for themsel-es3 they are entitled to res+ect for their +references. The ethical tas% is to $eigh the +references of +arents and children and sol-e the conflicts $hich may arise.
(n addition3 ethical issues surrounding the care of minors in the E! are intert$ined $ith state la$s that address consent su*stance a*use3 +regnancy3 a*ortion3 and child a*use and neglect. ,hysicians must %no$ the re5uirements of the la$ in the state in $hich they +ractice. Although ethics and the la$3 generally +resume that a minor lac%s decision ma%ing ca+acity3 there are many im+ortant e6ce+tions to this rule. The emergency rule (see section on informed consent +resumes consent for anyone3 including minors3 $ith a true emergency. Emergency has *een construed *y courts to go *eyond 4ust life threatening or disa*ling disease or in4ury to include treatment to alle-iate +ain or suffering from serious *ut nonemergent conditions. Many states ha-e la$s $hich allo$ minors to consent $hen they see% care for +regnancy3 se6ually transmitted diseases3 su*stance a*use3 or child a*use. (n addition3 many states *y statute or common la$ allo$ emanci+ated minors or mature minors to consent for their o$n medical care. Emanci+ated minors are usually defined as minors $ho li-e inde+endently of their +arents and are self1su++orting3 minors $ho are married3 ha-e *een +regnant3 or $ho are in the armed forces. The mature minor is a young +erson (usually 1A or older $ho the +hysician *elie-es +ossesses the re5uisite decision ma%ing ca+acity and demonstrates understanding of the nature of treatment. 8nder most circumstances the mature minor can consent to or refuse treatment $hich is of lo$ ris% and to the minor?s *enefit. #i%e adult +atients3 minors ha-e a right to +ri-acy and res+ect for confidentiality. Ethical dilemmas may arise $hen a minor is accom+anied *y a +arent $ho demands to %no$ the nature of the condition or treatment $hich in-ol-es one of the e6ce+tions for $hich a minor can gi-e consent
(+regnancy3 child a*use3 etc. and the minor refuses to +ro-ide that information to the +arent. The +hysician may feel conflicted $hen she or he *elie-es that in-ol-ing the +arent is in the child?s *est interests. 2o$e-er3 in general3 the $ishes of the minor +atient should *e res+ected $hen the minor is allo$ed *y la$ or ethics to consent. (n addition3 older minors ha-e a right to +ri-acy and sensiti-e information should generally not *e shared $ith +arents or others $ithout first discussing disclosure $ith the minor.
!tudy "uestions* 1. 2o$ should you resol-e the a*o-e caseG Can you treat this teenager against his $illG 9. !escri*e treatments for $hich a mature minor may gi-e consent3 and treatments for $hich the mature minor may not gi-e consent. @. Can an emanci+ated minor refuse a life sa-ing *lood transfusion on religious groundsG Bibliography 2older AR/ ,arents3 courts and refusal of treatment J ,ediatr 19>@: 1=@/A1A1 A91. Jonsen AR3 Siegler M3 7inslade 7J (eds / Clinical Ethics3 @nd ed. McGra$12ill3 (nc3 )e$ Dor%3 1999. #egal Corres+ondent/ Teenage confidence and consent. 0rit Med J 19>A:99=/144114A. Morrissey J3 2offman A3 Thor+e J/ Consent and Confidentiality in the 2ealth Care of Children and Adolescents/ #egal Guide Macmillan/ The "ree ,ress3 )e$ Dor%3 19>;. RoBofs%y "/ Consent to Treatment/ A ,ractical Guide 9nd ed3 #ittle 0ro$n3 0oston3 199=. Tsai A&3 Schafermeyer R73 &alifon !3 et al/ E-aluation and treatment of minors/ Reference on consent. Ann Emerg Med 199@:99/19111191<.
III. Issues #elated to $atient Autono &. Advance &irectives Objectives
1. !efine ad-ance directi-es/ dura*le +o$er of attorney for health care and li-ing $ills 9. State the +ur+ose of an ad-ance directi-e and descri*e the re5uirements for a -alid ad-ance directi-e. @. E6+lain your state la$s regarding ad-ance directi-es. 4. E6+lain the conditions $hich ma%e an ad-ance directi-e a++lica*le. A 4A year old male is *rought into the emergency de+artment $ith altered le-el of consciousness. According to his com+anion3 he has A(!S3 *ut until yesterday $as alert and interacti-e3 although confused at times. 2e has *een diagnosed $ith A(!S dementia. 2is com+anion *rings along the +atient?s dura*le +o$er of attorney for health care that names the com+anion as the surrogate decision ma%er.
An ad-ance directi-e is a $ritten document $hich e6+resses the future $ishes of a +atient. (t is designed to gi-e +atients control o-er the treatment decisions $hich $ill *e made $hen they are una*le to +artici+ate directly. The t$o main ty+es of ad-ance directi-e are li-ing $ills and dura*le +o$ers of attorney for health care. (t is li%ely that the use of ad-ance directi-es $ill increase $ith im+lementation of the +atient self determination act3 $hich *ecame effecti-e !ecem*er 13 1991. This federal act re5uires that all hos+itals $hich acce+t Medicare and Medicaid funds +ro-ide information a*out ad-ance directi-es and de-elo+ +olicies for im+lementation of ad-ance directi-es. (nformation a*out ad-ance directi-es has also *een mailed to all social security reci+ients.
#i-ing $ills e6+ress the $ishes of +atients regarding life1sustaining +rocedures in the e-ent of terminal illness. They are legally recogniBed *y o-er 4A states. #i-ing $ills ha-e s+ecific restrictions $hich state that the +erson $ould not $ant resuscitation if he or she is terminally ill3 death is imminent and resuscitation $ould only +rolong the dying +rocess. 0ecause of these restricti-e +hrases3 li-ing $ills are often of little -alue in the emergency and +rehos+ital setting. Clarification may *e +ro-ided *y the +atient?s +hysician or +ro6y decision ma%er. 7hen the a++lica*ility and circumstances are clear3 ho$e-er3 the emergency +hysician has an o*ligation to res+ect the li-ing $ill. (f the +hysician cannot in good conscious do so3 he or she should +ro-ide for another +hysician to care for the +atient. "inally3 the +atient can re-o%e a li-ing $ill at any time3 e-en during a time of crisis in the emergency de+artment. All states ha-e statutes go-erning dura*le +o$ers of attorney. (n some states3 additional statutes e6+licitly identify that dura*le +o$ers of attorney may a++ly to health care decisions. A dura*le +o$er of attorney gi-es to another +erson the authority to ma%e decisions for a +atient if he or she *ecomes inca+acitated. The +erson then *ecomes a legally recogniBed +ro6y decision ma%er for the +atient. 7hen a dura*le +o$er of attorney e6ists3 the emergency +hysician should allo$ the designated +erson to +artici+ate in decisions regarding the +atient?s medical care. The +ro6y decision ma%er should not *ase re5uests to initiate or $ithhold resuscitation on his or her o$n -alues3 *ut must ma%e decisions according to the %no$n $ishes of the +atient. (mmunity is generally granted to the +hysician $ho carries out the +ro6y?s decision in good faith. ,hysicians should *e a$are of state la$3 federal guidelines and ethical res+onsi*ilities $hich outline +olicies
regarding health care +ro6ies and li-ing $ills. Emergency de+artments should ha-e guidelines regarding ad-ance directi-es.
!tudy +uestions 1. 7hat are your state la$s as they relate to ad-ance directi-esG 7hich forms of ad-ance directi-es are allo$edG 9. (n this case3 $ho has decision ma%ing +o$er for this +ersonG @. 7ho $ould you consult for decisions if the +arents also came to the emergency de+artment and re5uested to ma%e decisions for their sonG Bibliography Annas GJ/ The health care +ro6y and the li-ing $ill. ) Engl J Med 1991:@94/191=1191@. Emanuel EJ3 Emanuel ##/ ,ro6y decision ma%ing for incom+etent +atients. JAMA 1999:9;</9=;<19=<1. (serson &'/ "ederal ad-ance directi-es legislation/ +otential effects on emergency medicine. J Emerg Med 1991:9/;<1<=. Miles S2/ Ad-anced directi-es to limit treatment/ the need for +orta*ility. J Amer Ger Soc 19><:@A/<41<;. Erentlicher !/ Ad-ance medical directi-es. JAMA 199=:9;@/9@;A19@;<. Siner !A/ Ad-ance directi-es in emergency medicine/ Medical3legal and ethical im+lications. Ann Emerg Med 19>9:1>/1@;411@;9.
I,. End of %ife &ecisions A. %i iting #esuscitation Objectives
1. 9.
!efine C!o )ot Resuscitate ErderC (!)R order . E6+lain the conditions $hich must *e +resent to $ithhold resuscitation in the emergency de+artment and in the out of hos+ital en-ironment.
@.
E6+lain the role of family and significant others in decisions a*out
resuscitation. An >@ year old $oman $as found asystolic. The family +resented the +aramedics $ith a +a+er3 signed *y a +hysician3 noting that the +atient $as not to *e resuscitated in the e-ent of cardiac arrest. State EMS +olicy3 ho$e-er3 does not recogniBe +rehos+ital do not resuscitate orders. (n this +atient3 no resuscitation $as underta%en. The +olice $ere notified that the +atient $as Cdead on arri-alC.
(t is legally and ethically acce+ta*le to $ithhold resuscitation attem+ts on +atients $ho ha-e e6+ressed clear $ishes not to undergo resuscitation. The challenge arises in the communication of such desires. The means of communication must *e legally3 ethically3 and medically sound. The emergency setting +resents difficulties since the +atient?s $ishes3 medical condition3 and +rognosis are usually un%no$n. Effecti-e means of communication must *e +resent to relay the +atient?s desire that resuscitation *e $ithheld. This can *e through standardiBed mechanisms that many regions ha-e de-elo+ed. Some states utiliBe a form $ith +atient and +hysician signature and a +atient arm1*and. (f there is dou*t regarding the +atient?s $ishes or the -alidity of a document3 resuscitati-e efforts should *e initiated. The decision to
resuscitate must *e an immediate yes or no decision. CSlo$ codes3C su*o+timal effort3 or delayed inter-ention are ne-er medically or ethically acce+ta*le. There is a clear need for emergency medical ser-ices to honor Cdo not resuscitateC orders. RecogniBa*le3 standard !)R orders should identify those +atients $ho $ish to ha-e no resuscitation attem+ts. #i-ing $ills should not *e used to limit +rehos+ital resuscitation since the a++lica*ility of the document may not *e clear. 7hile it is ethically a++ro+riate to honor !)R orders in the +rehos+ital setting3 a num*er of o+erational3 legal3 medical and ethical challenges must *e o-ercome. The emergency medical ser-ice must rely on the +ersonal +hysician to +ro-ide a++ro+riate3 $ritten !)R orders $hich are consistent $ith +atient +references and medical indications. The form used for !)R orders must *e acce+ta*le to the emergency medical ser-ice and the legal 4urisdiction. (t must *e clear regarding those inter-entions $hich are to *e im+lemented and those $hich are to *e $ithheld. Mechanisms must *e in +lace to ensure that the document reflects the current status of the +atient. This can *e accom+lished *y re5uiring +eriodic rene$al of the order. ,rehos+ital !)R orders should *e +orta*le3 so the directi-e can *e honored e5ually in the hos+ital3 nursing home3 +ri-ate home or +u*lic setting. An ideal system $ould +ossess !)R orders $ith standard communication and authoriBation +rocedures $hich are easily recogniBa*le and do not demand inter+retation or cause confusion. The document should *e familiar to the emergency medical ser-ice3 the family3 the emergency de+artment3 the +ri-ate +hysician3 and nursing homes.
!tudy "uestions
1. Should the +aramedics ha-e follo$ed state +olicy and attem+ted resuscitationG 9. @. 7hat e-idence of +atient $ishes does a +hysician need $ithhold resuscitation attem+tsG (s a relati-e?s -er*al re5uest enoughG !oes the age3 a++earance3 or +hysical condition of the +atient matterG
Bibliography Adams JG3 !erse AR3 Gotthold 7E3 Mitchell JM3 Mos%o+ JC3 Sanders A0/ Ethical As+ects of Resuscitation Ann Emerg Med 1999:91/19<@119<;. Ayres RJ/ Current contro-ersies in +rehos+ital resuscitation of the terminally ill +atient. ,rehos+ital and !isaster Medicine 199=:A/491A<. American College of Emergency ,hysicians/ Guidelines for Cdo not resuscitate ordersC in the +rehos+ital setting. Ann Emerg Med 19>>:1</11=;111=>. Miles S23 Crimmins TJ/ Erders to limit emergency treatment for an am*ulance ser-ice in a large metro+olitan area. JAMA 19>A:9A4/A9A1A9<. Ramos T3 Reagan JE/ ?)o? $hen the family says ?go?/ resisting families? re5uests for futile C,R. 19>9:1>/>9>1>99.
I,. End of %ife &ecisions B. Futility Objectives 1. !efine futility 9. !escri*e situations in $hich futility may *e used to $ithhold treatment in the emergency de+artment and out of hos+ital setting. A 9A year old male is *rought to the emergency de+artment *y +aramedics after sustaining a gunshot $ound to his head. 2e arri-es $ith agonal res+irations3 and a *lood +ressure of ;= systolic. The *ullet entered at the left tem+le and there is a large e6it $ould $ith e6truding *rain from the right tem+le. 2e has a GCS of @.
Although not e6+licitly stated3 $e generally assume that health care +ro-iders are not e6+ected to offer treatments to their +atients $hich are not medically indicated. "or many clinical conditions3 the medical indications and +rognosis for resuscitati-e measures still need to *e defined. ,hysicians and ethicists continue to discuss ho$ to +roceed $hen it is *elie-ed that attem+ts at resuscitation $ould *e futile. (f a medical inter-ention is of no *enefit3 then it should not *e a++lied. Det relying on +oorly defined notions of futility may diminish +atient autonomy. The American 2eart Association suggests the follo$ing criteria for medical futility in AC#S/ 1. A++ro+riate 0#S and A#S ha-e already *een attem+ted $ithout restoration of circulation. 9. )o +hysiologic *enefit can *e e6+ected from A#S and 0#S *ecause the +atient?s +hysiologic functions are deteriorating des+ite ma6imum thera+y (e6am+les3 o-er$helming se+sis3 cardiogenic shoc% . )o sur-i-ors ha-e *een re+orted under the gi-en circumstances in $ell1designed studies.
@.
Another definition states that if in the last 1== cases a medical treatment has *een useless3 that treatment is futile. This +ro*a*ility analysis allo$s for the +ossi*ility that @ successes $ould occur in the ne6t 1== similar cases. This definition is a++ealing *ecause of its +recision3 and use of +ro*a*ility3 *ut lea-es in dou*t the inter+retation of useless. A distinction is made *et$een an effect on one +art of the *ody and a *enefit3 $hich im+ro-es the +erson as a $hole. Ethers ha-e +ointed out the im+ortance of determining the goals $hen defining futility. A common e6am+le is the +atient for $hich li-ing for a fe$ days $ould *e a *enefit *ecause it $ould allo$ her to say good*ye to family3 or for out1of1to$n relati-es to arri-e. Thus3 $hile some authors ha-e argued that +atients and families need not *e consulted in determining futility3 it ma%es more sense to communicate $ith +atients and families in order to understand their goals for treatment. 7hile the decision not to +ro-ide a futile thera+y may rest $ith the +hysician3 only through dialogue can the +hysician understand the goals of treatment. This a++roach allo$s for e6+loration of the desired outcome3 acce+ta*ility of *urdens3 and the +atient?s or family?s $illingness to gam*le $ith the outcome. There is a +resum+tion in fa-or of resuscitation in dou*tful cases. Thus3 the sco+e of medical futility in resuscitation decisions is narro$: it does not include estimates of future 5uality of life. Engoing research into outcomes of resuscitation should hel+ determine more +recisely the e6+ected outcome of inter-ention and there*y more clearly indicate $hen inter-ention is futile.
!tudy "uestions
1.
!iscuss situations in $hich you might use futility to sto+ treatment in the emergency de+artment.
9.
!iscuss the difference *et$een strict medical futility as no +ossi*ility of long term sur-i-al3 and futility as lac% of *enefit.
@.
!oes this case fit the definition of medical futilityG 7hat efforts to$ard resuscitation should *e attem+tedG
Bibliography Jec%er )S3 Schneiderman #J/ Ceasing futile resuscitation in the field/ ethical considerations. Arch (nt Med 1999:9@9919@9<. #oe$y E23 Carlson RA/ "utility and (ts 7ider (m+lications Arch (ntern Med 199@: 1A@/49914@1. #antos J!3 Singer ,A3 7al%er RM et al/ The (llusion of "utility in Clinical ,ractice Am J Med 19>9: ></>11>4. Schneiderman #J3 Jec%er )S3 Jonsen AR/ Medical "utility/ (ts Meaning and Ethical (m+lications Ann (ntern Med 199=: 119/94919A4. Schneiderman #J and Jec%er )/ "utility in ,ractice Arch (ntern Med 199@: 1A@/4@<1441. Tomlinson T and 0rody 2/ "utility and the Ethics of Resuscitation JAMA 199=: 9;4/19<;119>=. Truog R!3 "rader J/ The +ro*lem $ith futility. ) Eng J Med 1999:@9;/1A;=1 1A;4.
,. The $hysician)$atient #elationship A. Confidentiality Objectives 1. !efine confidentiality. 9. !iscuss your duty of confidentiality to E! +atients @. !escri*e threats to +atient confidentiality in the E! including hos+ital em+loyees3 +er+etrators and -ictims of -iolent crime3 minors and cele*rities. 4. !iscuss the duty to *reach confidentiality including duty to $arn3 +u*lic health and contagious diseases and legal re+orting re5uirements. A @9 year1old +aramedic comes to the emergency de+artment in a +ost1ictal state. 2e $as $itnessed to ha-e a grand mal seiBure. After a*out an hour3 he *ecomes more res+onsi-e and relates that he had a similar e+isode in the +ast. 2e *egs you not to tell the !e+artment of Motor 'ehicles (!M' *ecause if he does not ha-e a dri-er?s license he cannot $or% as a +aramedic. Dour state la$ re5uires you to re+ort e+isodes of loss of consciousness.
Confidentiality and confide are deri-ed from the #atin confidere, to trust. ,atients confide in their +hysicians $ith the understanding that $hat they re+ort $ill not *e disclosed $ithout e6+licit +ermission. Since res+ecting confidentiality has long *een ac%no$ledged as a *asic res+onsi*ility of +hysicians3 it is understood as an im+licit +romise to +atients. Confidentiality +romotes full disclosure of detailed and accurate +atient information $hich is essential to +ro+er diagnosis and treatment. Confidentiality +romotes societal trust3 +ersonal autonomy3 and thera+eutic candor. 'arious codes of 7estern medical ethics echo the sentiment that confidentiality is an im+ortant +rinci+le in the healing arts. "or e6am+le3 the 2i++ocratic oath states/
7hatsoe-er in my +ractice or not in my +ractice ( shall see or hear amid the li-es of men3 $hich ought not to *e noised a*road3 as to this ( $ill %ee+ silence3 holding such things unfitting to *e s+o%en.
More recently3 the AMA Council on Ethical and Judicial Affairs acce+ted the statement/ The +atient has a right to confidentiality. The +hysician should not re-eal confidential information $ithout the consent of the +atient3 unless +ro-ided *y la$ or *y the need to +rotect the $elfare of the indi-idual or the +u*lic interest. Thus3 *oth ancient and modern +hysicians ha-e recogniBed the im+ortance of confidentiality and ha-e included it in -arious oaths3 +rinci+les3 and rules of +rofessional conduct. American common la$ has found +hysicians lia*le for *reach of confidentiality on grounds of defamation3 in-asion of +ri-acy3 and *reach of an im+lied contract. En the other hand3 +hysicians ha-e *een indicted for failing to *rea% confidentiality $hen it $as deemed o*ligatory for them to do so in order to $arn or +rotect others. "or e6am+le3 the courts ha-e found against +hysicians for failing to $arn a third +arty a*out a +atient?s seiBures3 failing to $arn a third +arty of the danger of infection from a +atient?s $ound3 failing to $arn neigh*ors and others li-ing in +ro6imity to +atients $ith contagious diseases3 and failing to $arn a $oman that a +atient $as contem+lating her murder. (n s+ite of its -ital im+ortance3 the duty to maintain confidentiality is *est -ie$ed as a prima facie (not a*solute o*ligation that may *e o-erridden $hen it conflicts $ith stronger moral duties. "or e6am+le3 $hen a +atient threatens to harm others3 emergency +hysicians may need to *reach confidentiality in order to +rotect the needs of identifia*le -ictims. The
+ro*a*ility and the magnitude of harm must *e *alanced against the +rotection of confidentiality. 0eaucham+ and Childress (19>> +rioritiBe four +ossi*le com*inations of +ro*a*ility and magnitude of harm *y assigning the follo$ing hierarchy/ 1 ma4or harm ris%1high +ro*a*ility3 9 minor harm1high +ro*a*ility: @ ma4or harm ris%1lo$ +ro*a*ility: and 4 minor harm1lo$ +ro*a*ility. According to this scale a lo$er num*er +ro-ides strong 4ustification to *reach confidentiality. (ndeed3 some ethicists hold that $hen confronted $ith a situation of ma4or harm and high +ro*a*ility the +ro-ider is not merely ethically 4ustified in *reaching confidentiality3 *ut is ethically re5uired to do so. Moral grounds for honoring confidentiality3 ho$e-er con-incing3 may sometimes yield to stronger moral grounds for disclosure. The follo$ing situations 4ustify disclosure/ 1. Re+orting related to +u*lic health la$s $hich may include 'ital statistics (*irth and death certificates Contagious diseases Child and elder a*use Criminally inflicted in4uries ,oisoning #oss of consciousness 9. #egal +roceedings @. Fuality assurance re-ie$ 4. ,rotection of a third +arty from mortal harm. (n general3 +hysicians may disclose confidential information $hen +atients agree to disclose or $hen disclosure is re5uired in order to fulfill a stronger moral duty to +re-ent harm or to o*ey 4ust la$s. !isclosure to +rofessionals directly in-ol-ed in the care of the +atient3 in most instances3 can *e understood as ha-ing the +atient?s im+lied consent. The +hysician?s
decision to re-eal information to +re-ent harm should *e *ased on the certainty3 duration and magnitude of the harm and the +ossi*ility of alternati-e methods for a-oiding harm $hich do not re5uire infringement of confidentiality. !tudy "uestions 1. Should you re+ort the +atient in this case to the !M'G 7hat are the conflicting ethical +rinci+lesG (f the +atient $as a highly -isi*le +u*lic figure $hat3 if anything3 $ould you re+ort to either the media or !M'G (f the +atient -oluntarily agreed not to dri-e $ould this affect your decision to re+ortG
9.
@.
Bibliography American Medical Association/ Council on Ethical and Judicial Affairs/ Current o+inions of the Council on Ethical and Judicial Affairs3 Chicago3 19>;3 IA.=9. Annas GJ/The rights of +atients/ The *asic AC#8 guide to +atients rights 9nd ed3 #i*rary of Congress cataloging1in1,u*lication !ata3 19>93 ++.1<A119A. 0eaucham+ T#3 Childress J" (eds / ,rinci+les of 0iomedical Ethics @rd ed3 )e$ Dor%3 E6ford 8ni-ersity ,ress3 19>9. Mc!onald 0A/ Ethical +ro*lems for +hysicians raised *y A(!S and 2(' infection/ Conflicting legal o*ligations of confidentiality and disclosure S+ecialty #a$ !igest 2ealth Care 199=: 1@4/<149. Siegel !M/ Confidentiality in Emergency Ris% Management ACE,3 !allas3 ++. 1>111>4. Siegler M/ Confidentiality in medicine1A decre+it conce+t. ) Engl J Med 19>9:@=</1A1>11A91.
,. The $hysician)$atient #elationship B. Truth telling and Co unication Objectives 1. E6+lain $hy truth telling is im+ortant. 9. !iscuss circumstances $hen one might not tell a +atient the truth. @. E6+lain the ethical foundations mandating honest +atient1+hysician communication. 4. !iscuss *arriers to effecti-e communication in the E!. A A; year1old man $ith a ;= +ac% year history of smo%ing comes to the emergency de+artment $ith shortness of *reath. 2is chest 61ray sho$s a large mass. (n +re+aring to admit the +atient3 he as%s $hat his 61ray sho$s. 7hen told of the mass3 $hich you thin% is +ro*a*ly cancer3 the +atient as%s3 C(t?s not li%ely to *e cancer3 is it3 doctorCG Dou say3 C7e can?t *e sure at this timeC. The +atient +ersists in %no$ing $hat you thin% it is. 7hat do you tell himG
Telling the truth may seem to *e a straight for$ard and ancient ethical +rinci+le in health care. Certainly3 religious and moral codes ha-e +roscri*ed lying3 from the Ten Commandments of Mosaic la$ to the $ritings of St. Augustine. 2o$e-er3 the duty of truth1 telling in medicine has actually only recently *ecome an ethical issue and in certain cultures such as Ja+an and (taly3 truth1telling is not the current norm. The 2i++ocratic oath does not ma%e any mention of truth telling to +atients3 nor is telling the truth +art of the 2i++ocratic tradition. The +re-ailing ethic su++orted *y Thomas ,erci-al in his 1>=@ ,rinci+les of Ethics $as one of *ene-olent dece+tion: he recommended that *ad ne$s *e %e+t from +atients to a-oid se-ere reactions. The AMA?s first Code of Ethics in 1>4< +er+etuated this attitude. This *ene-olent dece+tion $as 4ustified *y the +rinci+le of nonmaleficence and continued into this century. (n 19;13 9=J of +hysicians still $ould not
tell a +atient of a diagnosis of cancer. (t $as not until 19<< that 9<J of +hysicians fa-ored telling +atients? their diagnosis. A num*er of factors ser-ed to change +hysicians? attitudes. The first $as the de-elo+ment in the common la$ of the doctrine of informed consent (see section on informed consent . Another factor $as the rise in em+hasis on ci-il rights and +atient autonomy. "inally3 the scandals in-ol-ing rights of +atients in-ol-ed in e6+erimentation led to the national commission for the +rotection of human su*4ects of *iomedical and *eha-ioral research. This commission issued a re+ort summariBing *asic ethical +rinci+les3 and setting out re5uirements of informed consent3 assessment of ris%s and *enefits to the su*4ects of research3 and fair +rocedures in the selection of human su*4ects. !es+ite this ne$ em+hasis on truth telling3 the thera+eutic +ri-ilege is still acce+ted as morally licit $hen there is su*stantial e-idence that offering the +atient the truth has a significant +ro*a*ility of causing harm. 2o$e-er3 +hysicians must *e -ery cautious in using this +aternalistic argument for not sharing *ad ne$s $ith the +atient. Studies sho$ that +atients generally do $ant to %no$ their diagnoses $hen +hysicians assume they do not3 and that harms from disclosure are less than +hysicians thin%3 and the *enefits are greater. "urther3 telling the truth may *e more difficult for the +hysician than the +atient3 es+ecially $hen the emergency +hysician must *ear stressful ne$s such as the death of a lo-ed one to the family. "inally3 the em+hasis on truth telling in medical ethics is culturally *ased. (n some cultures +atients may still e6+ect that *ad ne$s $ill *e con-eyed only to the family. 7e are only one generation remo-ed from a centuries? old medical norm that +racticed *ene-olent dece+tion. The *etter +ractice is to
com+assionately inform the +atient of *ad ne$s so that she or he is a*le to control the medical decision ma%ing +rocess. This route may *e uncomforta*le for the +atient and the +hysicians3 *ut the *enefits are greater for +atients $hen +hysician and +atient engage in $hat has *een a++ro+riately called braving the truth. !tudy "uestions 1. 7hat ans$er should *e gi-en to the +atient in this situationG 9. Dou diagnose a +atient $ith gonorrhea and *elie-e his $ife needs treatment. 2e as%s you to treat her3 *ut not tell her no$ she ac5uired the infection. 7hat should you say to the man?s $ifeG A +atient comes to the emergency de+artment re5uesting o+iate +ain medication for his *ac% +ain. 2e is %no$n to ha-e a history of drug a*use. Dou +rescri*e an in4ecta*le anti1inflammatory medication. The +atient as%s $hat he is getting. (s it ethically 4ustified to lie or Cstretch the truthCG !oes it ma%e a difference if the +atient has engaged in dece+tionG
@.
Bibliography )o-ac% !23 !etering 0J3 Arnold R et al/ ,hysicians attitudes to$ard using dece+tion to resol-e difficult ethical +ro*lems JAMA 19>9: 9;1/99>=199>A. ,ellegrino E!/ (s truth telling to the +atient a cultural artifactG JAMA 1999: 9;>/1<@411<@A. Schmidt TA3 )orton R#3 Tolle S7/ Sudden death in the E!/ Educating residents to com+assionately inform families J Emerg Med 1999: 1=/;4@1;4<.
,. The $hysician)$atient #elationship C. Co passion and E pathy Objectives
1. 9.
!escri*e the im+ortance of com+assion and em+athy in the E!. !escri*e ho$ com+assion and em+athy im+ro-e +atient care3 +hysician satisfaction3 and +atient satisfaction.
A +atient $ith metastatic terminal +rostate cancer comes to the E! for a C+ain shotC. 2e is on !ilaudid3 *ut lately the *one +ain is se-ere. 2e is una*le to ta%e oral medications *ecause of se-ere nausea and -omiting. 2e is an6ious and frightened a*out dying. The de+artment is *usy3 *ut he $ants to tal% to you a*out his fears. 7hat ethical +rinci+les a++ly to this situationG Although em+athy is a desira*le attri*ute of health care +ro-iders3 it is not contained $ithin the ethical +rinci+les3 *ut rather +ro-ides de+th and human feeling to them. Em+athy is a central tenant of all as+ects of medical ethics3 $ithout $hich the +rinci+les are *arren3 lifeless and lac%ing in color. (t is this a*ility to trade +laces emotionally $ith the sic% +erson that allo$s health care +ro-iders to feel the anguish of illness and struggle to treat the anguish e-en if the illness cannot *e cured. Em+athy is the feeling C( am youC or C( could *e youC3 $hile sym+athy creates the message3 C( $ant to hel+ youC. Throughout history +hysicians did little *ut +ro-ide a caring3 em+athetic ear to +atients for $hom they had no treatment. (t is easy to *e nice to +atients $hom $e li%e and $ho ha-e illnesses $hich im+ress us. Com+assion and em+athy are harder to feel $hen the +atients are distasteful and non1com+liant. Ma4or tragedy may rarely mo-e us3 $e may scoff at the CminorC com+laints $hich generate so much concern. (f $e neither understand nor connect $ith the grief3 fear and concern of our +atients3 ho$e-er3 $e cannot address the feelings. (gnoring the emotional com+onent of +atients and families lea-es them unsatisfied and lea-es the
+hysician3 at *est3 ignorant of the +atient?s +ers+ecti-e. Com+assion and em+athy im+ro-e +atient and +hysician satisfaction *y +romoting communication3 minimiBing conflict3 and ma6imiBes +atient confidence in the diagnosis and treatment +lan. !tudy +uestions 1. 2o$ should the +hysician res+ond in the a*o-e caseG 9. Can em+athy *e taughtG @. 2o$ do $e encourage em+athy in +hysicians and traineesG
Bibliography 0ellet ,3 Maloney M/ The im+ortance of em+athy as an inter-ie$ing s%ill. JAMA 1991:9;;/1>@111>@9. Grumet G/ ,andemonium in the modern hos+ital. ) Engl J Med 199@:@9>/4@@1 4@<. &atB J/ The Silent 7orld of !octor and ,atient The "ree ,ress3 )e$ Dor%3 19>4. )o-ac% !23 !u*e C3 Goldstein MG/ Teaching medical inter-ie$ing Arch (ntern Med 1999: 1A9/1>1411>9=. )elson AR/ 2umanism and the art of medicine. JAMA 19>9:9;9/199>119@=. S+iro 23 McCrea Curnen MG3 ,eschel E3 St. James ! (ed Em+athy and the ,ractice of Medicine Dale 8ni-ersity ,ress3 )e$ 2a-en3 199@.
,I. Issues #elated to -ustice A. .ealth Care #ationing Objectives 1. 9. @. !efine rationing. !efine allocation. E6+lain ho$ rationing and allocation im+act emergency care.
A 4A year old man cuts his finger and then goes to the emergency de+artment for treatment. (n the E! he is noted to ha-e hy+ertension. The +atient states that he $as on medication for hy+ertension. 2o$e-er3 *ecause he lost his health care co-erage he has not seen a +hysician and no longer ta%es his medication. 2e is gi-en a +rescri+tion for a once a day ACE inhi*itor3 and the +hone num*ers of se-eral +hysicians. 7hen he goes to the +harmacy3 he learns that the medication is -ery e6+ensi-e. 2e contacts each of the +hysicians to $hom he $as referred and none of them $ill acce+t ne$ uninsured +atients. 2e is referred to a local clinic3 $hich has a @ month $aiting list. 0ecause he $as +rescri*ed only enough medications for t$o $ee%s3 he returns to the E! for follo$1u+. !istri*uti-e 4ustice3 a *asic +rinci+le of medical ethics3 demands that $e see% a morally correct distri*ution of *enefits and *urdens in society. !istri*uti-e 4ustice re5uires an e5uita*le3 *ut not necessarily3 an e5ual allocation of health care resources. )orman !aniels has descri*ed e5uita*le distri*ution as re5uiring that there *e no information *arriers3 financial *arriers or su++ly anomalies $hich +re-ent access to a Cdecent *asic minimumC of health care. !istri*uti-e 4ustice affects allocation of health care resources at three se+arate le-els. "irst3 health care is *ut one of many societal interests. 7hen society allocates its resources3 health care com+etes $ith other interests including housing3 education3 defense and the en-ironment. Currently health care accounts for 14J of the gross national +roduct (G), 3 and has *een gro$ing more ra+idly than any other go-ernment +rogram.
7ithout health care reform3 it is estimated that health care $ill account for 9=J of the G), *y the year 9===. Gi-en our limited resources and gro$ing *udget deficit3 continued increases in health care e6+enditures $ill result in reductions in other +rograms. At a second le-el3 distri*uti-e 4ustice affects allocation decisions in-ol-ing health care resources. 2ealth care is rationed (rationing is defined as the distri*ution of a limited amount of goods and ser-ices in all societies: the ma4or difference is the criteria used for rationing. These criteria should *e de-elo+ed at the societal le-el3 not the *edside. Such decisions should *e *ased on medical need3 cost effecti-eness3 and +ro+er distri*ution of *enefits and *urdens in society. Eur society must decide the a++ro+riate allocation of limited resources to -arious medical inter-entions such as +u*lic health and +re-enti-e medicine3 child and maternal health3 ne$ technologies3 +rehos+ital and emergency care3 comfort and +alliation. 7e must also consider the im+act of +oor nutrition3 lac% of ade5uate housing3 inade5uate education3 +ollution and -iolence on an indi-idual?s health. The effect of these +ro*lems on health demonstrates the com+le6ity of the relationshi+ *et$een social issues and health care. At a third le-el3 distri*uti-e 4ustice affects allocation at the institutional le-el and *edside. (n emergency medicine3 allocation of scarce resources is the ethical +rinci+le under+inning triage decisions. ,hysicians also consider distri*uti-e 4ustice $hen ma%ing decisions a*out costs and resource allocation. Although some +hysicians *elie-e it is unethical to allo$ costs to influence clinical decisions3 a +hysician $ho ignores all cost considerations ignores the ad-erse conse5uences such decisions $ill ha-e on their +atient as $ell as others.
,hysicians ha-e enormous influence on health care e6+enditures *ecause $e decide $hich resources are needed to diagnose and treat +atients. Ene of the *asic tenets of our +rofession is the duty to $or% for the *est interests of our +atients. This im+lies that +hysicians should use resources $hich *enefit the +atient3 $ithout creating undue *urden. 8nfortunately3 $e fre5uently lac% the outcome data to determine $hether a s+ecific treatment +roduces *enefit3 marginal *enefit3 no *enefit or harm. (n these cases $e must use our *est 4udgement a*out the +otential *enefit to our +atients. Cost can and should *e a +art of that consideration. !es+ite the con-entional -ie$ that +hysicians and +atients ma%e decisions at the *edside *ased solely on the *est interests of the +atient3 many e6ternal factors including a*ility to +ay3 health insurance co-erage3 insurance mandates for a second o+inion and scarcity of resources may influence the decision ma%ing +rocess. As emergency +hysicians3 $e see the conse5uences of allo$ing distri*ution of health care to *e *ased on the a*ility to +ay. ,atients $ith no health insurance see% medical care for nonemergent +ro*lems in the emergency de+artment. A++ro+riate care often re5uires follo$1u+ *y a +rimary care +hysician $ho may not *e a-aila*le to these +atients. The im+ortance of health insurance $as highlighted *y a recent study that re+orted an association *et$een lac% of insurance and increased mortality. !ecisions a*out health care allocation must *e made *oth at the le-el of society (macroallocation and at the le-el of the indi-idual +atient (microallocation . Although *eneficence must *e the guiding +rinci+le for microallocation decisions3 distri*uti-e 4ustice guides macroallocation decisions and also +lays a role in microallocation decisions in our current system.
!tudy "uestions 1. 7hat is distri*uti-e 4ustice and ho$ does it a++ly to health careG 9. 2o$ does this case illustrate +ro*lems in our current deli-ery of health careG @. 2o$ do $e currently ration health careG 4. (n your o+inion3 ho$ should $e ration health careG Bibliography American College of ,hysicians Ethics Manual Ann (ntern Med 1999: 11</94<1 9;=. 0eaucham+ T#3 Childress J" (eds / ,rinci+les of 0iomedical Ethics @rd ed3 )e$ Dor%3 E6ford 8ni-ersity ,ress3 19>9. Callahan !/ Rationing medical +rogress/ the $ay to afforda*le health care. ) Engl J Med 199=:@99/1>1=11>1@. !aniels )/ Just 2ealth Care Cam*ridge 8ni-ersity ,ress3 Cam*ridge3 19>A. Eddy !M/ Rationing *y +atient choice. JAMA 1991:9;A/1=A11=>. (serson &'/ Assessing -alues/ Rationing emergency de+artment care. Am J Emerg Med 1999:1=/9;@19;4. Society for Academic Emergency Medicine Ethics Committee/ An ethical foundation for health care/ An emergency medicine +ers+ecti-e Ann of Emerg Med 1999: 91/1@>111@><.
,I. Issues #elated to -ustice B. &uty Objectives 1. !efine the CGood SamaritanC statute in your state.
9. E6+lain the a++lica*ility of the CGood SamaritanC statute to emergency +hysicians in the +rehos+ital setting and in the Emergency !e+artment. @. !efine your ethical and legal duty to +atients $ho +resent to the E!. A +atient +resents to the emergency de+artment $ith nausea3 -omiting3 and mild diarrhea. The +atient *elongs to an 2ME $hich re5uires +re1a++ro-al for emergency care. The 2ME denies a++ro-al for the +atient to *e seen in the E!3 since the +atient has no fe-er3 no significant a*dominal +ain3 and is not dehydrated.
Emergency +hysicians ha-e *oth an ethical and legal duty to e-aluate and treat any +atient $ho re5uests treatment. These +atients must at least *e screened to ensure that no illness e6ists that $ill cause harm to the +atient if untreated. This duty is *ased on the +rinci+les of *eneficence and nonmaleficence as $ell as 4ustice. This o*ligation also has *een codified into federal la$ *y the CE0RA legislation. Reim*ursement issues do not affect this duty: all +atients must *e e-aluated regardless of a*ility to +ay. (f +otentially significant illness or in4ury is +resent3 the +atient must *e sta*iliBed or treated. 2ealth care reform and managed care are going to add ne$ strains to emergency +hysicians? traditional role of +ro-iding uni-ersal access. (n an effort to control costs3 more third +arty +ayors are going to e6+ect Cgate%ee+ersC to limit access to s+ecialists and other ser-ices. )onetheless3 emergency de+artments must maintain their a-aila*ility to all +atients $ho
see% ser-ices3 and at a minimum screen +atients to determine the e6tent of their urgent medical need. 2o$e-er3 other circumstances do e6ist $hich may limit the o*ligation to treat +atients. Although all health care +ro-iders assume some +ersonal ris% in choosing to treat +atients3 emergency +hysicians do not ha-e to +lace themsel-es in e6cessi-e +hysical danger. ,atients $ho are threatening +hysical harm to staff or other +atients do not ha-e a right to treatment. 7ea+ons may also *e remo-ed from +atients as a condition of treatment. 7e do ha-e an ethical o*ligation to treat +atients des+ite the ris% of e6+osure to contagious diseases. (n addition to defining res+onsi*ility of health care $or%ers on the 4o*3 society has an interest in +romoting the $illingness of +eo+le $ith health care e6+ertise to assist others in need e-en $hen the +erson $ith e6+ertise is not on the 4o*. CGood SamaritanC statutes ha-e *een instituted to ser-e this end. These la$s generally state that a +erson $ho has no duty to another and e6+ects no +ayment for ser-ices is +rotected *y la$ as long as no gross and $illful negligence is committed. The CGood SamaritanC rule does not generally a++ly to +hysicians in the emergency de+artment since a duty is generally recogniBed to all +atients +resent3 *ut $ould a++ly to an emergency +hysician $ho comes u+on an automo*ile accident or $itnesses a cardiac arrest. !tudy "uestions 1. 7hat is the duty of the emergency +hysician to the +atient in this caseG 9. 8nder $hat circumstances might you refuse treatment to a +atientG @. (s it acce+ta*le for the emergency +hysician to loo% at the +atient3 *riefly e6amine the a*domen3 and +ro-ide detailed3 $ritten instructions of signs and sym+toms that signify an emergencyG
Bibliography American College of Emergency ,hysicians/ Emergency care/ res+onsi*ilities and +rinci+les. +olicy statement3 June 1991. American College of Emergency ,hysicians/ Guidelines concerning $or% sto++ages and slo$do$ns. Ann Emerg Med 19>A:14/<<. Curran 7J/ Economic and legal considerations in emergency care. ) Engl J Med 19>A:@19/@<41@<A. !erlet R73 )ishio !A/ Refusing care to +atients $ho +resent to an emergency de+artment/ Ann Emerg Med 199=/19/9;919;<. (serson &'/ Refusal of care/ the ethical dilemma. (letter Ann Emerg Med 199=:19/119<. Miles S2/ 7hat are $e teaching a*out indigent +atientsG JAMA 1999:9;>/9A;119A;9. Sha$ &)3 Sel*st SM3 Gill "M/ (ndigent children $ho are denied care in the emergency de+artment. Ann Emerg Med 199=:19/A91;9. Kuger A/ +rofessional res+onsi*ilities in the A(!S generation. 2astings Cent Re+ June 19><:1</1;19=.
,I. Issues #elated to -ustice C. Moral Issues in &isaster Medicine Objectives 1. !iscuss the sco+e and limits of medical effecti-eness in disaster situations. 9. @. (dentify the moral +rinci+les underlying triage. !iscuss criteria for ma%ing triage decisions and their ethical 4ustification.
A +lane crashes3 resulting in in4ury to many +atients. The -ictims range in age from 1 year old to 9@ years old. Ene of the -ictims is a 8S senator.
Some of the +atients ha-e se-ere *urns3 others *lunt head3 a*dominal or chest trauma. There are > +atients in cardio+ulmonary arrest. Ene +atient has agonal res+irations3 and another has almost 1==J *ody *urns. A $oman is in la*or and at least A +atients a++ear to *e in shoc%. At least 1A +atients ha-e minor in4uries. Dou are the sole +hysician +resent. (n disasters3 $hen resources are scarce3 the +rimary ethical +rinci+le *ecomes 4ustice. The goal is to treat +eo+le e5uita*ly and fairly. This has led to the conce+t of triage. Triage is *ased on the utilitarian ethical +rinci+le of +ro-iding the greatest *enefit to the greatest num*er. 2o$e-er3 there $ill al$ays *e some uncertainty as to $hat *enefit a +articular +atient $ill deri-e from any action. 0ased on this +rinci+le3 +riority should *e
gi-en to firefighters3 +u*lic safety3 and medical +ersonnel $ho might *e a*le to return to the rescue effort. (n addition3 those in4uries most amena*le to treatment3 such as air$ay o*struction and *leeding3 and those acti-ities most useful in alle-iating suffering3 such as administration of +ain medication3 should *e em+hasiBed.
Should there *e any differentiation *ased on age or social $orthG The most famous case of triage *y social $orth is the Seattle committee that made decisions a*out $ho $ould recei-e %idney dialysis. ,hysicians de-elo+ed a list of +eo+le $ho could +otentially *enefit from this ne$ medical inter-ention. Then3 a committee of non1+hysicians chose the indi-iduals $ho $ould recei-e this then scarce resource. ,riority $as gi-en to indi-iduals $ith +roducti-e 4o*s3 or a family to su++ort. The result $as that most of the early reci+ients of dialysis $ere middle class3 $hite males. Although the committee $as certainly $ell meaning3 many later felt that their system of social $orth led to *iases against the +oor3 $omen and minorities. Thus3 although it is tem+ting to consider the -alue of the -arious -ictims3 the general consensus of most ethicists is that social $orth is an unfair criteria for the distri*ution of resources. Rather3 treatment is *ased on medical need and the li%elihood of *enefit.
!tudy +uestions 1. 2o$ should you +roceed to care for +atients in this caseG 9. 7ould you gi-e some +riority attention to the 8S SenatorG @. Could any +atient distract you and cause you to +ay e6tra attention or +ro-ide longer3 more attenti-e careG Bibliography 0ell )&/ Triage in medical +ractices/ An unacce+ta*le modelG Soc Sci Med 19>1:1A"/1A111A;. Jonsen AR3 Siegler M3 7inslade 7J/ Clinical Ethics @rd ed3 McGra$12ill (nc3 )e$ Dor%3 19993 + 1@9. ,ledger 2G/ Triage of casualties after nuclear attac%. #ancet 19>;:;<>1;<9.
Triage in Reich 7 (ed Encyclo+edia of 0ioethics 9nd ed The "ree ,ress3 )e$ Dor%3 1999. 7inslo$ GR/ ,rinci+les for triage3 in Triage and Justice3 0er%eley3 8ni-ersity of California ,ress3 19>93 ++ ;=11=9.
,I. Issues #elated to -ustice &. #esearch Objectives 1. 9. !efine the moral +rinci+les for research on human su*4ects. !escri*e the uni5ue moral challenges $hich face research in an
emergency setting. @. !escri*e ho$ to o*tain informed consent for research.
A @9 year old man too% @= mg of loraBe+am. 2e $as somnolent *ut arousa*le and his -ital signs $ere sta*le. 2e and his family $ere informed that he $ould *e trans+orted to the medical center across to$n Csince they ha-e a medicine to treat this o-erdose.C (The center $as conducting trials $ith a *enBodiaBe+ine antagonist .
As a result of the atrocities of medical e6+eriments carried out *y the )aBis in 7orld 7ar ((3 the infamous Tus%egee Sy+hilis Study and other unethical research3 go-ernments and +rofessional organiBations made a concerted effort to de-elo+ ethical +rinci+les for *iomedical research. The )urem*erg Code3 the 2elsin%i !eclaration and the 0elmont Re+ort ser-e as a foundation for de-elo+ing ethical +rinci+les for research. These +rinci+les include res+ect for +eo+le as autonomous agents3 truth telling3 *eneficence in ma6imiBing the *enefits and minimiBing the *urdens for research su*4ects3 and 4ustice in e5uita*ly distri*uting the *enefits and *urdens of research. !uring the +ast decade3 $e ha-e $itnessed a dramatic increase in re+orts of unethical conduct in *iomedical research. 7hether this re+resents an increased incidence of unethical conduct or rather a com*ination of increased recognition and re+orting of such occurrences is unclear. )e-ertheless3 the result has *een an outcry from the +u*lic3 go-ernment
officials3 and medical +rofessionals to esta*lish guidelines that $ill ensure the integrity of *iomedical research. 0ecause +hysicians de+end on research to im+ro-e +atient care3 $e should *e con-ersant $ith the ethical issues in research. Among the most im+ortant issues are scientific misconduct (fraud3 +lagiarism3 fa*rication of data 3 unethical treatment of human and nonhuman su*4ects3 conflict of interest3 and res+onsi*ilities to colleagues3 student and other trainees. A +articularly difficult area for emergency medicine is informed consent for resuscitation and other research $hen time is critical and the +atient does not ha-e decision ma%ing ca+acity. (n the +ast3 guidelines ha-e allo$ed the use of deferred consent3 in $hich consent $as o*tained after the study inter-ention. !eferred consent is criticiBed as an illogical conce+t3 and recent de-elo+ments suggest that $ai-ed consent ma%es more sense. The current criteria for $ai-ed consent are 1 minimal ris% to su*4ects3 9 the $ai-er $ill not ad-ersely affect the rights and $elfare of the su*4ects3 @ the research could not *e carried out $ithout the $ai-er3 and 4 su*4ects $ill *e +ro-ided information follo$ing +artici+ation. (n recent years3 the federal go-ernment3 +rofessional organiBations and institutions ha-e de-elo+ed +olicies and +rocedures to address some other ethical concerns. Ene e6am+le of this is the C8niform Re5uirements for Manuscri+ts Su*mitted to 0iomedical JournalsC. This $as de-elo+ed *y the (nternational Committee of Medical Journal Editors. (n addition to descri*ing the format for su*missions3 the Committee addressed the issues of authorshi+ as $ell as +rior and du+licate +u*lication.
!tudy "uestions
1.
(s it a++ro+riate for +atients to *e trans+orted to a +articular hos+ital in order to enroll them in a research +rotocolG
9. @.
2o$ should consent *e o*tained for resuscitation researchG (s it +ossi*le to o*tain informed consent for emergency researchG
Bibliography 0inder #/ (nformed consent in emergency medicine research SAEM )e$sletter Se+tem*er3 199@. (nternational Committee of Medical Journal Editors/ 8niform re5uirements for manuscri+ts su*mitted to *iomedical 4ournals Ann (ntern Med 19>>: 1=>/9A>1 9;A. Sie*er JE/ Ethical considerations in +lanning and conducting research on human su*4ects Academic Medicine 199@: ;> (su++ /s91s1@. S+i-ey 723 A*ramson )S3 (serson &'3 Mac&ay CR3 Cohen M,/ (nformed consent for *iomedical research in acute care medicine. Ann Emerg Med 1991:9=/19A1119;A. 8S Go-ernment/ The 0elmont Re+ort/ Ethical ,rinci+les and Guidelines for the ,rotection of 2uman Su*4ects of Research 8S Go-ernment ,rinting Effice3 7ashington !.C.3 19>>.
,II. Teaching Objectives 1. !escri*e the ethical issues surrounding the use of animals for teaching and research. 9. !escri*e the ethical issues surrounding the use of the ne$ly dead for education. Emergency medicine +hysicians attem+ted cardiac resuscitation of an >> year old +atient. Efforts $ere discontinued after @A minutes. Ene of the residents as%ed if anyone $ould mind if he e6tu*ated and re1intu*ated the +atient to +ractice. Clinical Teaching
A ma4or o*ligation of academic +hysicians is to ensure that future generations of +hysicians +ossess the re5uisite s%ills to effecti-ely and e6+ertly +ro-ide medical care. Emergency medicine +hysicians and allied +rofessionals3 themsel-es3 share an o*ligation to *e s%illed and com+etent $hen they hold themsel-es out as medical +rofessionals. The uns%illed +rofessional1in1training must ac5uire the +rofessional attri*utes +rior to assuming full res+onsi*ility for +atient care. These +rofessional attri*utes include the re5uisite %no$ledge3 a++ro+riate *eha-ior3 and technical a*ilities. Educational +rograms must struggle $ith the *alance *et$een the resident?s need for graded res+onsi*ility3 and the +atient?s right to *e treated *y a fully 5ualified +hysician. (n the +ast3 an im+licit assum+tion $as made that indigent +atients +aid for their health care *y allo$ing learners to treat them. 7ith health care reform and uni-ersal insurance this assum+tion may need to change. "aculty +hysicians $ill *e e6+ected to *e more directly in-ol-ed in the care of all +atients treated in the emergency de+artment. At
the same time our students and residents $ill continue to need access to +atients and learning o++ortunities. Ac5uiring technical s%ills such as endotracheal intu*ation3 central line +lacement3 and chest tu*e thoracostomy re5uires that the trainee ha-e a++ro+riate +ractice +rior to +erforming it in time of crisis. ,ractice is a++ro+riately ac5uired on +lastic manne5uins3 *ut the manne5uin remains an im+erfect model. (n addition3 these s%ills can *e learned in more controlled settings such as o+erating room intu*ation3 central line +lacement in sta*le (C8 +atients and chest tu*es in the sta*le +atient $ith a s+ontaneous +neumothora6. 2o$e-er3 these forms of training may not al$ays *e ade5uate. The /se of Models for Teaching Contro-ersy e6ists a*out the use of animals3 as $ell as the use of recently deceased human *eings. Grou+s concerned a*out the use of animals in teaching and e6+erimentation e6+ress t$o ethical concerns a*out the use of animals. Those $ho su++ort animal rights e6+ress the *elie-e that animals3 li%e humans3 ha-e certain *asic rights as sentient *eings. Animals are inca+a*le of gi-ing informed consent and should3 therefore3 not *e used for teaching or e6+erimentation. Ethers3 $hile not e6+ressing concern a*out the rights of animals are concerned a*out animal $elfare. These +eo+le are concerned a*out inhumane treatment and unnecessary harm. (nstitutions ha-e de-elo+ed committees $hich address issues surrounding the use of animals in the same $ay that institutional re-ie$ *oards address research on human su*4ects. Any use of animals re5uires treatment and care that is as humane and discomfort1free as +ossi*le. Contro-ersy also e6ists a*out +erforming +rocedures on the ne$ly dead. Those $ho o++ose +racticing +rocedures on the ne$ly dead raise
concerns a*out res+ect for autonomy. The +atient is una*le to gi-e consent3 and generally em+athy and com+assion +reclude us from as%ing the *erea-ed family for consent. 2o$e-er3 it may *e argued that res+ect for autonomy is *ased on +rinci+les of freedom and li*erty $hich do not a++ly to the dead. (n addition3 *ased on utility3 little or no harm is done to the deceased and much might *e gained *y resident education. Some also ma%e a distinction *et$een non1disfiguring +rocedures such as intu*ation3 and more in-asi-e +rocedure such as chest tu*es.
!tudy "uestions 1. !oes your institution allo$ or encourage +ractice of in-asi-e s%ills on recently deceased +atientsG 9. @. Should consent *e o*tained from the familyG Should an attending +hysician see e-ery +atient $ho comes to the emergency de+artment of a teaching hos+italG 4. 7hat guidelines does your institution ha-e on the use of animals for teachingG Are these guidelines ethically 4ustifiedG A. 7hat do you *elie-e a*out the use of animal model in teachingG The use of the ne$ly deadG Bibliography (serson &'/ The su+er-ision of +hysicians in training/ an educational and ethical dilemma. Medical Teacher 19>>: 1=/19A19=1. (serson &'/ Re5uiring consent to +ractice and teach using the recently dead. J Emerg Med 1991: 9/A=91A1=. (serson &'/ ,ostmortem +rocedures in the emergency de+artment/ using the recently dead to +ractice and teach. J Med Eth June 199@.
'arner GE/ The +ros+ects for consensus and con-ergence in the animal rights de*ate 2astings Center Re+ort 1994: 94 (1 /9419>. 7in%en$erder 7/ Ethical dilemmas for house staff +hysicians. JAMA 19>A: 9A4/@4A41@4A<.
,III. #elationships 0ith the Bio Objectives 1. 9. @.
edical Industry
!iscuss +romotional offerings that are clearly not to *e acce+ted *y +hysicians. E6+lain circumstances $hen gifts of nominal -alue can *e acce+ted. E6+lain $hy the relationshi+ $ith industry must remain ethically a++ro+riate.
A drug com+any re+resentati-e in the emergency de+artment as%s to s+ea% $ith the senior resident for a moment. The senior resident sits $ith the re+resentati-e in the charting area3 and they discuss the -alue of his com+any?s ne$ anti*iotic for an emergency de+artment use3 -ersus other +roducts on the mar%et. The re+resentati-e distri*utes +romotional material on the anti*iotic to the resident and other residents in the area. The re+resentati-e then reaches into his shoulder *ag and +asses out com+any +ens3 note +ads3 and +enlights to the residents3 and +resents a Cte6t*oo%C on infectious diseases for the resident?s E! li*rary. The resident than%s the re+resentati-e for his gratuities. The re+resentati-e +asses out his card and offers to *ring food to one of the future resident conferences3 or +ay for a noted emergency medicine s+ea%er to come and +resent a grand rounds on infectious diseases in the emergency de+artment.
The interaction *et$een emergency medicine residents and the *iomedical industry has recently *ecome a matter of concern *y organiBations $ithin emergency medicine. As the *iomedical industry must com+ete in a free enter+rise mar%et system3 they must ad-ertise +roducts to +hysician consumers. )e-ertheless3 +hysicians must *ase their +harmacothera+y on the scientific literature. ,romotional materials de-elo+ed *y the *iomedical industry may not *e designed to gi-e +hysicians o*4ecti-e scientific data regarding a +roduct. ,hysicians may not *e
a$are of ho$ undue influence3 +romotional materials and gift gi-ing im+acts their clinical decisions. Additionally3 *iomedical industry re+resentati-es are
fundamentally moti-ated to +romote only their +roduct3 and therefore3 a +resentation from them is inherently *iased. S+ea%ers $ho recei-e e6cessi-e com+ensation may also ha-e a conflict of interest. (n-itations to s+ea% at residency or CME conferences should come from the residency organiBation itself and not from the *iomedical com+any. (t is the residency +rogram?s res+onsi*ility to ensure that a *alanced3 un*iased -ie$ of the scientific data is +resented. Academic +rograms should set u+ guidelines to regulate the interaction of residents $ith the *iomedical industry. A gift acce+ted *y a resident +hysician should +ro-ide an education to the +hysician3 or a direct *enefit to the +hysician?s +atients. Residents of a +rogram may acce+t te6t*oo%s of reasona*le -alue3 +ro-ided they are +u*lications not s+ecifically +roduced *y the *iomedical com+any. (t is common for +hysicians to acce+t gifts of nominal -alue such as +ens3 +enlights3 note +ads. Gifts of significant -alue such as tic%ets to s+orting functions3 e6+ensi-e dinners3 or hos+itality suite +arties should *e a-oided. Ene standard to 4udge $hether the gift is a++ro+riate is to as% the 5uestion3 C7ould ( *e $illing to defend this gift to my +atientsGC )o gift should *e acce+ted if it is gi-en to re$ard a s+ecific +rescri*ing +attern or other +hysician *eha-ior. A healthy ethical relationshi+ $ith the *iomedical industry can e6ist. Scholarshi+s3 residency +rogram su++ort3 monies to stimulate resident research or education could *e directed to the residency organiBation itself3 *y+assing indi-idual +hysician influence. 0oth the ethics committee and the research committee of the Society for Academic Emergency Medicine ha-e de-elo+ed guidelines for interaction $ith *iomedical com+anies. These +a+ers descri*e +otential ethical conflicts in the relationshi+ *et$een
+hysicians and the *iomedical industry and suggest ethical guidelines for +hysicians and researchers. Emergency medicine residents and faculty should *e con-ersant $ith these guidelines. !tudy "uestions 1. 9. 7hy do *iomedical +romotional acti-ities3 such as gift gi-ing3 +resent +otential ethical conflicts to the emergency +hysicianG 7hat as+ects of +romotional materials and +resentations *y com+any1 s+onsored s+ea%ers could su*-ert a *alanced3 un*iased medical educationG 2o$ can +hysicians and residency +rograms interact to +romote ethical relationshi+s $ith the *iomedical industryG
@.
Bibliography 1. American Medical Association/ Gifts To ,hysicians "rom (ndustry. JAMA3 1991: 9;A/A=1. 9. &essler !A3 ,ines 7#/ The "ederal Regulation of ,rescri+tion !rug Ad-ertising and ,romotion. JAMA3 199=: 9;4/94=91941A. @. Chren MM3 #andefeld S3 Murray T2/ !octors3 !rug Com+anies3 and Gifts. JAMA 19>9:9;9/@44>1@4A1. 4. Sanders A03 &eim SM3 S%lar !3 Adams J/ Emergency ,hysicians and the 0iomedical (ndustry. Ann Emerg Med 1999:91/AA;1AA>. A. A-orn J3 Chen M3 2artley R/ Scientific -ersus Commercial Sources of (nfluence En the ,rescri*ing 0eha-ior of ,hysicians. AM J ME! 19>9:<@/41>.
Vous aimerez peut-être aussi
- Judika-Sampai AkhirDocument1 pageJudika-Sampai AkhirAngkat Prasetya Abdi NegaraPas encore d'évaluation
- Book 1Document13 pagesBook 1Semba Anggen RachmaniPas encore d'évaluation
- KLP1 Jurnal IlmiahDocument8 pagesKLP1 Jurnal IlmiahArya KusumaPas encore d'évaluation
- Cyclosporine Reduces Reperfusion InjuryDocument3 pagesCyclosporine Reduces Reperfusion InjuryAngkat Prasetya Abdi NegaraPas encore d'évaluation
- Nilai RemediDocument21 pagesNilai RemediAngkat Prasetya Abdi NegaraPas encore d'évaluation
- Nilai Normal Laboratorium Pada AnakDocument6 pagesNilai Normal Laboratorium Pada AnakMaharani Primastuti ArganistPas encore d'évaluation
- Critical Appraisal of Epidemiological Study PDFDocument11 pagesCritical Appraisal of Epidemiological Study PDFYessy Dwi OktaviaPas encore d'évaluation
- 2965 CONSORT+2010+ChecklistDocument2 pages2965 CONSORT+2010+ChecklistsongsiriPas encore d'évaluation
- Rajiv Gandhi University of Health Sciences, Karnataka Bangalore Proforma For Registration of Subjects For DissertationDocument5 pagesRajiv Gandhi University of Health Sciences, Karnataka Bangalore Proforma For Registration of Subjects For DissertationAngkat Prasetya Abdi NegaraPas encore d'évaluation
- Review Article: Today and Future of Age-Related Macular DegenerationDocument9 pagesReview Article: Today and Future of Age-Related Macular DegenerationAngkat Prasetya Abdi NegaraPas encore d'évaluation
- Nilai Normal Vital PediatriDocument4 pagesNilai Normal Vital PediatriEkaPutri AzizPas encore d'évaluation
- Pengendalian Emosi Pasien Hipertensi Dengan Terpai MusikDocument5 pagesPengendalian Emosi Pasien Hipertensi Dengan Terpai MusikAngkat Prasetya Abdi NegaraPas encore d'évaluation
- Correlation Between Body Mass Index and Intraocular Pressure in Normotensive SubjectsDocument1 pageCorrelation Between Body Mass Index and Intraocular Pressure in Normotensive SubjectsAngkat Prasetya Abdi NegaraPas encore d'évaluation
- B82 FDD 01Document24 pagesB82 FDD 01Angkat Prasetya Abdi NegaraPas encore d'évaluation
- Correlation Between Body Mass Index and Intraocular Pressure in Normotensive SubjectsDocument1 pageCorrelation Between Body Mass Index and Intraocular Pressure in Normotensive SubjectsAngkat Prasetya Abdi NegaraPas encore d'évaluation
- B82 FDD 01Document24 pagesB82 FDD 01Angkat Prasetya Abdi NegaraPas encore d'évaluation
- Eeb05036 767 772Document6 pagesEeb05036 767 772Angkat Prasetya Abdi NegaraPas encore d'évaluation
- D4 AF0 D 01Document11 pagesD4 AF0 D 01Angkat Prasetya Abdi NegaraPas encore d'évaluation
- Intraocular Pressure in An American Community: The Deover Dom Eye StudyDocument5 pagesIntraocular Pressure in An American Community: The Deover Dom Eye StudyAngkat Prasetya Abdi NegaraPas encore d'évaluation
- BMC Genetics: Intraocular Pressure in Genetically Distinct Mice: An Update and Strain SurveyDocument15 pagesBMC Genetics: Intraocular Pressure in Genetically Distinct Mice: An Update and Strain SurveyAngkat Prasetya Abdi NegaraPas encore d'évaluation
- Association of Life-Style With Intraocular Pressure in Middle-Aged and Older Japanese ResidentsDocument8 pagesAssociation of Life-Style With Intraocular Pressure in Middle-Aged and Older Japanese ResidentsAngkat Prasetya Abdi NegaraPas encore d'évaluation
- Original ArticleDocument5 pagesOriginal ArticleAngkat Prasetya Abdi NegaraPas encore d'évaluation
- Height and Its Relationship To Refraction and Biometry Parameters in Singapore Chinese ChildrenDocument6 pagesHeight and Its Relationship To Refraction and Biometry Parameters in Singapore Chinese ChildrenAngkat Prasetya Abdi NegaraPas encore d'évaluation
- 6187 DD 01Document4 pages6187 DD 01Angkat Prasetya Abdi NegaraPas encore d'évaluation
- 257 EEd 01Document4 pages257 EEd 01Angkat Prasetya Abdi NegaraPas encore d'évaluation
- D 01Document10 pagesD 01Angkat Prasetya Abdi NegaraPas encore d'évaluation
- 265 901 2 PBDocument5 pages265 901 2 PBAngkat Prasetya Abdi NegaraPas encore d'évaluation
- 2011 02 Obese Women GlaucomaDocument1 page2011 02 Obese Women GlaucomaAngkat Prasetya Abdi NegaraPas encore d'évaluation
- International Journal of Biomedical and Advance ResearchDocument4 pagesInternational Journal of Biomedical and Advance ResearchAngkat Prasetya Abdi NegaraPas encore d'évaluation
- Intraocular Pressure: Harry Murgatroyd BSC MB CHB (Hons) Jane Bembridge MB CHB (Hons) FrcaDocument4 pagesIntraocular Pressure: Harry Murgatroyd BSC MB CHB (Hons) Jane Bembridge MB CHB (Hons) FrcaAngkat Prasetya Abdi NegaraPas encore d'évaluation
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeD'EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeÉvaluation : 4 sur 5 étoiles4/5 (5794)
- The Little Book of Hygge: Danish Secrets to Happy LivingD'EverandThe Little Book of Hygge: Danish Secrets to Happy LivingÉvaluation : 3.5 sur 5 étoiles3.5/5 (400)
- Shoe Dog: A Memoir by the Creator of NikeD'EverandShoe Dog: A Memoir by the Creator of NikeÉvaluation : 4.5 sur 5 étoiles4.5/5 (537)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceD'EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceÉvaluation : 4 sur 5 étoiles4/5 (895)
- The Yellow House: A Memoir (2019 National Book Award Winner)D'EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Évaluation : 4 sur 5 étoiles4/5 (98)
- The Emperor of All Maladies: A Biography of CancerD'EverandThe Emperor of All Maladies: A Biography of CancerÉvaluation : 4.5 sur 5 étoiles4.5/5 (271)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryD'EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryÉvaluation : 3.5 sur 5 étoiles3.5/5 (231)
- Never Split the Difference: Negotiating As If Your Life Depended On ItD'EverandNever Split the Difference: Negotiating As If Your Life Depended On ItÉvaluation : 4.5 sur 5 étoiles4.5/5 (838)
- Grit: The Power of Passion and PerseveranceD'EverandGrit: The Power of Passion and PerseveranceÉvaluation : 4 sur 5 étoiles4/5 (588)
- On Fire: The (Burning) Case for a Green New DealD'EverandOn Fire: The (Burning) Case for a Green New DealÉvaluation : 4 sur 5 étoiles4/5 (73)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureD'EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureÉvaluation : 4.5 sur 5 étoiles4.5/5 (474)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaD'EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaÉvaluation : 4.5 sur 5 étoiles4.5/5 (266)
- The Unwinding: An Inner History of the New AmericaD'EverandThe Unwinding: An Inner History of the New AmericaÉvaluation : 4 sur 5 étoiles4/5 (45)
- Team of Rivals: The Political Genius of Abraham LincolnD'EverandTeam of Rivals: The Political Genius of Abraham LincolnÉvaluation : 4.5 sur 5 étoiles4.5/5 (234)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyD'EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyÉvaluation : 3.5 sur 5 étoiles3.5/5 (2259)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreD'EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreÉvaluation : 4 sur 5 étoiles4/5 (1090)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersD'EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersÉvaluation : 4.5 sur 5 étoiles4.5/5 (344)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)D'EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Évaluation : 4.5 sur 5 étoiles4.5/5 (121)
- Her Body and Other Parties: StoriesD'EverandHer Body and Other Parties: StoriesÉvaluation : 4 sur 5 étoiles4/5 (821)
- CHAPTER 12 Partnerships Basic Considerations and FormationsDocument9 pagesCHAPTER 12 Partnerships Basic Considerations and FormationsGabrielle Joshebed AbaricoPas encore d'évaluation
- ParlPro PDFDocument24 pagesParlPro PDFMark Joseph SantiagoPas encore d'évaluation
- EDUC 303 Essay ActivityDocument3 pagesEDUC 303 Essay ActivityImee MandasocPas encore d'évaluation
- Welcome To HDFC Bank NetBankingDocument1 pageWelcome To HDFC Bank NetBankingsadhubaba100Pas encore d'évaluation
- ReservationsDocument30 pagesReservationsplasmadragPas encore d'évaluation
- Chapter 1Document25 pagesChapter 1Annie Basing-at AngiwotPas encore d'évaluation
- Eada Newsletter-May-2015 (Proof3)Document2 pagesEada Newsletter-May-2015 (Proof3)api-254556282Pas encore d'évaluation
- 12-Chemical Hazard CommunicationDocument9 pages12-Chemical Hazard CommunicationHalime HalimePas encore d'évaluation
- Online Auction: 377 Brookview Drive, Riverdale, Georgia 30274Document2 pagesOnline Auction: 377 Brookview Drive, Riverdale, Georgia 30274AnandPas encore d'évaluation
- 005 SPARK v. Quezon City G.R. No. 225442Document28 pages005 SPARK v. Quezon City G.R. No. 225442Kenneth EsquilloPas encore d'évaluation
- Additional Material For TX-ZWE 2021 FinalDocument26 pagesAdditional Material For TX-ZWE 2021 Finalfarai murumbiPas encore d'évaluation
- Η Πολιτική Νομιμοποίηση της απόθεσης των παιδιώνDocument25 pagesΗ Πολιτική Νομιμοποίηση της απόθεσης των παιδιώνKonstantinos MantasPas encore d'évaluation
- LabRel MT Long QuizDocument4 pagesLabRel MT Long QuizDerek EgallaPas encore d'évaluation
- 01 Manual's WorksheetsDocument39 pages01 Manual's WorksheetsMaria KhanPas encore d'évaluation
- Ultra 3000 Drive (2098-In003 - En-P)Document180 pagesUltra 3000 Drive (2098-In003 - En-P)Robert BarnettePas encore d'évaluation
- Reform in Justice System of PakistanDocument5 pagesReform in Justice System of PakistanInstitute of Policy Studies100% (1)
- FW 8 BenDocument1 pageFW 8 BenMario Vargas HerreraPas encore d'évaluation
- Philippine Laws On WomenDocument56 pagesPhilippine Laws On WomenElle BanigoosPas encore d'évaluation
- Explanatory Note To The Revision of FIATA Model Rules For Freight Forwarding ServicesDocument16 pagesExplanatory Note To The Revision of FIATA Model Rules For Freight Forwarding ServicesFTU.CS2 Tô Hải YếnPas encore d'évaluation
- AQA GCSE Citizenship Revision Guide - FINALDocument19 pagesAQA GCSE Citizenship Revision Guide - FINALJohn SmithPas encore d'évaluation
- A - A - Benjamin Zephaniah PoemsDocument6 pagesA - A - Benjamin Zephaniah PoemsJakub KonopkaPas encore d'évaluation
- ASME B31.5-1994 Addend Refrigeration PipingDocument166 pagesASME B31.5-1994 Addend Refrigeration PipingFRANCISCO TORRES100% (1)
- Book Building: IPO Price Discovery MechanismDocument35 pagesBook Building: IPO Price Discovery MechanismDevyansh GuptaPas encore d'évaluation
- Payroll in Tally Erp 9Document13 pagesPayroll in Tally Erp 9Deepak SolankiPas encore d'évaluation
- Solved Acme Realty A Real Estate Development Company Is A Limited PDFDocument1 pageSolved Acme Realty A Real Estate Development Company Is A Limited PDFAnbu jaromiaPas encore d'évaluation
- Julius Caesar - Gallic War Bilingual - 10 First PagesDocument12 pagesJulius Caesar - Gallic War Bilingual - 10 First PagesTyrex: Psychedelics & Self-improvementPas encore d'évaluation
- Research - Procedure - Law of The Case DoctrineDocument11 pagesResearch - Procedure - Law of The Case DoctrineJunnieson BonielPas encore d'évaluation
- SAP Project System - A Ready Reference (Part 1) - SAP BlogsDocument17 pagesSAP Project System - A Ready Reference (Part 1) - SAP BlogsSUNIL palPas encore d'évaluation
- Sia vs. PeopleDocument26 pagesSia vs. PeopleolivePas encore d'évaluation
- Affidavit of UndertakingDocument3 pagesAffidavit of UndertakingPingotMagangaPas encore d'évaluation