Académique Documents
Professionnel Documents
Culture Documents
Ekg Dan Syncope
Transféré par
DIdit FAjar NUgrohoCopyright
Formats disponibles
Partager ce document
Partager ou intégrer le document
Avez-vous trouvé ce document utile ?
Ce contenu est-il inapproprié ?
Signaler ce documentDroits d'auteur :
Formats disponibles
Ekg Dan Syncope
Transféré par
DIdit FAjar NUgrohoDroits d'auteur :
Formats disponibles
Electrocardiogram Findings in Emergency Department Patients with Syncope
James Quinn, MD, MS, and Daniel McDermott, MD
Abstract
Objectives: To determine the sensitivity and specicity of the San Francisco Syncope Rule (SFSR) electrocardiogram (ECG) criteria for determining cardiac outcomes and to dene the specic ECG ndings that are the most important in patients with syncope. Methods: A consecutive cohort of emergency department (ED) patients with syncope or near syncope was considered. The treating emergency physicians assessed 50 predictor variables, including an ECG and rhythm assessment. For the ECG assessment, the physicians were asked to categorize the ECG as normal or abnormal based on any changes that were old or new. They also did a separate rhythm assessment and could use any of the ECGs or available monitoring strips, including prehospital strips, when making this assessment. All patients were followed up to determine a broad composite study outcome. The nal ECG criterion for the SFSR was any nonsinus rhythm or new ECG changes. In this specic study, the initial assessments in the database were used to determine only cardiac-related outcomes (arrhythmia, myocardial infarction, structural, sudden death) based on set criteria, and the authors determined the sensitivity and specicity of the ECG criteria for cardiac outcomes only. All ECGs classied as abnormal by the study criteria were compared to the ofcial cardiology reading to determine specic ndings on the ECG. Univariate and multivariate analysis were used to determine important specic ECG and rhythm ndings. Results: A total of 684 consecutive patients were considered, with 218 having positive ECG criteria and 42 (6%) having important cardiac outcomes. ECG criteria predicted 36 of 42 patients with cardiac outcomes, with a sensitivity of 86% (95% condence interval [CI] = 71% to 94%), a specicity of 70% (95% CI = 66% to 74%), and a negative predictive value of 99% (95% CI = 97% to 99%). Regarding specic ECG ndings, any nonsinus rhythm from any source and any left bundle conduction problem (i.e., any left bundle branch block, left anterior fascicular block, left posterior fascicular block, or QRS widening) were 2.5 and 3.5 times more likely associated with signicant cardiac outcomes. Conclusions: The ECG criteria from the SFSR are relatively simple, and if used correctly can help predict which patients are at risk of cardiac outcomes. Furthermore, any left bundle branch block conduction problems or any nonsinus rhythms found during the ED stay should be especially concerning for physicians caring for patients presenting with syncope. ACADEMIC EMERGENCY MEDICINE 2011; 18:714718 2011 by the Society for Academic Emergency Medicine
yncope is dened as a transient loss of consciousness resulting in loss of postural tone, followed by spontaneous recovery with return to baseline neurologic function. It is a common clinical problem,
From the Division of Emergency Medicine Stanford University (JQ), Palo Alto, CA; and the Department of Emergency Medicine, University of California San Francisco (DM), San Francisco, CA. Received October 13, 2010; revision received January 6, 2011; accepted February 2, 2011. The authors have no relevant nancial information or potential conicts of interest to disclose. Supervising Editor: Eddy Lang, MD. Address for correspondence and reprints: James Quinn, MD, MS; e-mail: quinnj@stanford.edu.
accounting for 1.2% of emergency department (ED) visits and up to 6% of acute hospitalizations.1,2 The assessment of patients with syncope is challenging because of the heterogeneity of the underlying cause. Many causes of syncope are benign, with neurocardiogenic (vagal) presentations being the most common. However, many patients present to EDs with unclear causes, with 5% to 10% of these patients suffering signicant morbidity or mortality. Cardiac arrhythmia and sudden death are the most serious causes of syncope in this group.3,4 As a result, a large number of patients with benign syncope are admitted for inpatient evaluation, at an estimated cost in the United States of over $2 billion dollars a year.5 There is a large variation in the number of patients admitted, with the rate in the United States reported to be 50% to 85%, while in
714
ISSN 1069-6563 PII ISSN 1069-6563583
2011 by the Society for Academic Emergency Medicine doi: 10.1111/j.1553-2712.2011.01120.x
ACADEMIC EMERGENCY MEDICINE July 2011, Vol. 18, No. 7
www.aemj.org
715
Canada and Australia the admission rate is between 15% and 30%.1,2,68 There is great potential to improve the efciency of the admission decision, and numerous studies have attempted to derive predictors or risk factors for those at high risk for serious outcomes. Regardless of the study, cardiac risk and the presenting electrocardiogram (ECG) ndings are consistently the most important factors in risk-stratication of syncope patients.914 However, studies vary on what constitutes an abnormal ECG. Furthermore, failure to apply simple ECG criteria has led to a variety of results when externally validating prediction rules for syncope.7,15,16 The largest series of prospective consecutive ED patients with syncope examined emergency physician interpretation of ECGs.2,11 In the derivation of the San Francisco Syncope Rule (SFSR), the denition of an abnormal ECG included any nonsinus rhythm on the 12-lead ECG, during routine cardiac monitoring, and or any new changes in the ECG compared to a previous ECG. However, the SFSR study considered all serious outcomes and did not distinguish cardiac outcomes from noncardiac serious outcomes. Furthermore, it did not specify which ECG ndings were abnormal. In this study, we determined the sensitivity for the ECG criteria of the SFSR for cardiac outcomes and reviewed all the abnormal ECGs in the SFSR study to determine the specic abnormalities and their importance when evaluating patients with syncope. METHODS Study Design This was an analysis of a database of prospectively collected data from consecutive patients with syncope. The original data set was collected under the approval of the University of California San Francisco committee on human research. The Stanford University institutional review board approved the reanalysis of data for this study. Study Setting and Population The initial prospective cohort study was conducted at a large university teaching hospital from July 1, 2000, until February 28, 2002, and included patients presenting with acute syncope or near syncope as a reason for their ED visit. Research assistants prospectively screened patients with complaints of syncope, loss of consciousness, fall, collapse, seizure, light-headedness, tachycardia, bradycardia, shortness of breath, and chest pain. Exclusion criteria were persistent altered mental status, alcohol or illicit drug related loss of consciousness, a denite seizure, or transient loss of consciousness caused by head trauma. Study Protocol Original Study. A research nurse reviewed daily patient logs and ensured enrollment of all possible patients. Prospective patients were identied and brought to the attention of the attending physician, who made the nal decision to enroll the patient. After assessing the patients, physicians completed a structured data form. The physicians assessed 50 predictor variables, including an ECG and rhythm assessment.
For the ECG assessment, the physicians were asked to categorize the ECG as normal (completely normal or old changes) or abnormal (any new changes). Specically, physicians were instructed that they should consider any new change as an abnormal ECG if there was no old ECG for comparison, but were encouraged to use old ECGs from previous visits or serial ECGs in their assessments. Physicians also did a separate rhythm assessment, which was considered as a separate variable. While monitoring was not mandated, they could use any of the ECGs or available monitoring strips, including prehospital strips, when making this assessment. Physicians marked the rhythm as sinus rhythm, supraventricular tachycardia (SVT), bradyarrhythmia, ventricular ectopy, or other. Where possible, two physicians independently evaluated patients to measure agreement on these two variables. In the derivation study both variables had good agreement and were combined to form the ECG criteria for the SFSR, the ECG criteria for the rule being positive if there were any new ECG changes or any nonsinus rhythm.2 Each patient was followed by a study coordinator to determine whether he or she had suffered a serious outcome by day 7. Serious outcomes for the study were death, myocardial infarction (MI), arrhythmia thought to cause the event, pulmonary embolism, stroke, subarachnoid hemorrhage, signicant hemorrhage, or any condition causing or likely to cause a return ED visit and hospitalization or therapeutic procedure for a related event. Current Study. In this reanalysis, we blinded ourselves to the initial assessments in the database and determined only cardiac-related outcomes based on set criteria. This included sudden death, MI (dened as any elevation of troponin or ECG change with an accompanying diagnosis of MI on the discharge diagnosis), any arrhythmia captured on monitoring and thought to have had a temporal relationship to the syncopal event, and any structural heart disease (primarily valvular) thought to have caused the event. We also considered any acute cardiac intervention such as pacemaker insertion and cardiac catheterization as important cardiac outcomes. All ECGs classied as abnormal by the study criteria were collected. We used the ofcial cardiology reading to determine the following specic ndings on the ECG: rhythm abnormalities on the ECG (ventricular tachycardia, heart block, paced, SVT), presence of right branch bundle block (RBBB), left branch bundle block (LBBB), ST-segment changes, nonspecic ST-T wave changes, interval variants (PR, QT), presence of ectopy, and presence of Q-waves. We also reanalyzed the specic rhythm ndings obtained during the separate rhythm assessment. Data Analysis We completed univariate chi-square analysis on the specic rhythm and ECG ndings to determine important relationships for determining cardiac outcomes. Where appropriate we also combined related variables to determine signicance and considered them for entry into a direct multivariate logistic regression
716
Quinn and Mc Dermott
ECG FINDINGS IN ED PATIENTS WITH SYNCOPE
model based on statistical signicance of p < 0.2. When variables were combined or clinically related (for example isolated LBBB vs. any LBBB or nonsinus on ECG vs. nonsinus from any source) we used the most signicant variable for entry. Forty outcomes would allow sufcient power to consider up to four variables in our multivariate model.17 The Hosmer-Lemeshow goodness-of-t test was used to determine the model t. Data were entered into an Access database (Microsoft Corp., Redmond, WA) and analyzed using SPSS version 18 (SPSS Inc., Chicago, IL) RESULTS A total of 684 consecutive patients were considered during the study period and represented 1.4% of the ED volume. Of the 684 patients, 634 had an ECG and rhythm analysis completed by an attending physician, and 10 had no ECG but a rhythm analysis documented. It was determined that 42 patients (6%) suffered cardiac outcomes, each of whom had both an ECG and a rhythm assessment. Of the 644 patients with ECG criteria, 218 were classied as having positive criteria, with 216 ECGs available for further analysis. Characteristics of all patients, those with abnormal ECGs and those with cardiac outcomes are outlined in Table 1. The abnormal ECG criteria predicted 36 of the 42 patients with cardiac outcomes, giving a sensitivity of 86%, a specicity of 70%, and a negative predictive value of 99% (see Table 2 for condence intervals [CIs]). Of the six patients not predicted by the criteria, three were diagnosed with non-Q-wave MI, one of whom died during cardiac catheterization. All were felt to have ECGs that were unchanged from previous readings. One had an exacerbation of CHF resulting in eventual death during hospitalization with an unchanged ECG on ED evaluation, and two were felt to have completely normal ECGs but were subsequently diagnosed with SVT. Considering specic ECG ndings, isolated LBBB, or any LBBB partial or complete, were associated with serious cardiac outcomes. The presence of Q-waves, RBBB, ST-segment changes, and sinus rhythm were not.
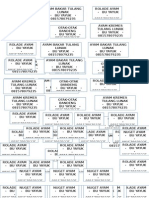
Table 2 Sensitivity and Specicity of SFSR ECG Criteria for Detecting Cardiac Outcomes Criteria Positive Cardiac outcome No cardiac outcome Total 36 180 216 Criteria Negative 6 422 428
Sensitivity = 86% (95% CI = 71% to 94%); specicity = 70% (95% CI = 66% to 74%); negative predictive value = 99% (95% CI = 97% to 99%); LR positive = 2.9 (95% CI = 2.4 to 3.4); LR negative = 0.2 (95% CI = 0.1 to 0.4). ECG = electrocardiogram; LR = likelihood ratio; SFSR = San Francisco Syncope Rule.
On separate rhythm assessment (using all ED information including monitoring), a signicantly greater number of patients were found to have nonsinus rhythms compared to the rhythm assessment using only the ECG reading (72% vs. 34%, p = 0.001), and this rhythm variable was signicant on univariate analysis (Table 3). On the multivariate logistic regression analysis, the Hosmer-Lemeshow goodness-of-t statistic was not signicant (p = 0.86), indicating that the model prediction did not signicantly differ from the observed. Only two variables met criteria for entry: any nonsinus rhythm from any source and any left bundle conduction problem (any LBBB, left anterior fascicular block, left posterior fascicular block, or QRS widening), which were 2.8 and 3.2 times more likely, respectively, associated with signicant cardiac outcomes (see Table 4 for CIs). DISCUSSION An ECG is currently recommended in almost all patients with syncope, as it is consistently the most
Table 3 Univariate Analysis of Specic ECG and Rhythm Findings Cardiac Outcome (n = 36) 5 15 4 7 4 23 4 7 1 9 2 17 29 (14) (42) (11) (19) (11) (64) (11) (19) (3) (25) (6) (47) (81) No Cardiac Outcome (n = 180) 7 49 16 36 16 133 11 67 1 45 5 61 113 (4) (27) (9) (20) (9) (74) (6) (37) (0.1) (25) (3) (34) (63)
Finding Table 1 Clinical and Demographic Characteristics Abnormal ECG Criteria (n = 216) 72.5 201 165 2.2 (17) (48.6) (76) (3) Cardiac Outcomes (n = 42) 78.6 17 41 4.9 (9.5) (40.1) (98) (4.2) ECG Isolated complete LBBB Any LBBB RBBB Q-waves Ventricular ectopy Sinus on ECG only ST segment changes Rhythm Sinus SVT Bradyarrhythmia PVC Other Any nonsinus
p-value 0.03 0.01 0.68 0.94 0.67 0.19 0.23 0.04 0.20 1.0 0.58 0.13 0.04
All (N = 684) Mean age (yr) Female Admitted Mean admission length (days) 7-day serious outcomes Cardiac outcomes Arrhythmia Ischemic Structural 62.1 402 376 1.6 (23) (58.9) (54.9) (2.4)
79 (11.5) 42 30 9 3 (6.1) (4.4) (1.3) (0.4)
49 (23) 36 28 6 1 (17) (13) (2.8) (0.1)
Values are given as n (%) or mean (SD).
Values are reported as n (%) ECG = electrocardiogram; LBBB = left branch bundle block; PVC = premature ventricular contraction; RBBB = right branch bundle block; SVT = supraventricular tachycardia.
ACADEMIC EMERGENCY MEDICINE July 2011, Vol. 18, No. 7
www.aemj.org
717
Table 4 Multivariate Analysis of Important ECG and Rhythm Findings Adjusted OR Any LBBB Any nonsinus rhythm 3.2 2.8 95% CI 1.46.9 1.16.8
ECG = electrocardiogram; LBBB = left branch bundle block.
important risk stratication tool as recommended by most society guidelines.18,19 In this study we determined the sensitivity and specicity of the SFSR ECG criteria when considering cardiac outcomes in patients with syncope and determined that the likelihood of a signicant cardiac outcome in a patient with normal SFSR ECG criteria was very low. We further dened specic ECG ndings for patients with abnormal ECGs and found nonsinus rhythms any time during an ED evaluation and left bundle branch conduction problems on ECG to be important specic ECG ndings. Almost every study attempting to risk stratify patients with syncope has found the ECG to be an important predictor for adverse events.2,9,12,13,20 However, there has been no agreement on what an abnormal ECG is in the setting of syncope. Denitions for signicant ECG ndings are generally long descriptions often dened by consensus specialty groups. Furthermore, there is no evidence regarding whether these ndings can be determined and applied by physicians evaluating these patients at the bedside.18 In one of the initial risk stratication studies by Martin et al.,12 their denition was broad. They acknowledged that ventricular arrhythmias, bradycardia associated with symptoms, atrial ventricular (AV) blocks (Mobitz II and complete heart block), and pacemaker malfunction were considered signicant. However, ectopic beats, brief SVT, and atrial dysrhythmias were not considered abnormal, unless the patient was symptomatic. They excluded any nonspecic ST-T wave abnormalities as being signicant. This denition was signicantly different from that used by Colivicchi et al.20 in their risk stratication. Their denition included any rhythm abnormalities, signicant AV blocks, signicant bundle branch blocks, right or left ventricular hypertrophy, left axis deviation, old MI, or any ST segment or ST-T wave abnormalities possibly consistent with myocardial ischemia. In the EGSYS trial, the denition of an abnormal ECG was comprehensive but nonspecic, including evaluation of the 12-lead ECG, as well as cardiac monitoring, electrophysiology studies, and ECG stress testing.14 When determining variables for the SFSR we kept a simple, broad, nonspecic denition that was subjective but tested for physician agreement for both the ECG ndings and the rhythm assessment. The subsequent combining of the rhythm nding into the ECG criteria has seemed to confuse people. Many have failed to understand the origin of the rhythm assessment and in simplifying the rule have assumed the rhythm criteria applies only to one ECG and not all sources, as it was derived.16 This had led to difculty applying the criteria and validating our ndings.7,15 In the rst external validation of the SFSR, Sun et al.15 note in their
limitations that they did not follow the ECG denition used in the SFSR, instead using a separate non-validated criteria any rhythm other than sinus, any bundle branch block, left-axis deviation, mono- or biventricular hypertrophy, any abnormal conduction interval except for rst degree atrioventricular block, any Q ST T change consistent with ischemia (acute or chronic), or isolated, nonspecic ST T abnormalities. In a separate validation study by Birnbaum et al.,7 the cardiology overread of ECGs was used when applying the criteria and appeared to ignore any monitoring abnormalities when applying the rhythm criteria. In a recently published study, a group from the University of Ottawa looked at the sensitivity of the SFSR with and without the use of monitoring ndings when dening rhythm abnormalities.8 When using the same ECG criteria as the initial SFSR studies, they were able to externally validate the results with the same sensitivity.8 In this study, we showed that over half of abnormal rhythms will be missed if only one ECG during the ED visit is used as the only source for rhythm determination. LIMITATIONS This was an observational cohort study that did not mandate care or specic standardized testing including monitoring in the ED. There were a signicant number of cases where the ECG showed sinus rhythm, but in those same 216 patients, the number with a sinus rhythm decreased substantially when all sources were used to determine the rhythm (Table 3). So while we cannot make recommendations on who should be monitored or for how long, it is clear that when monitoring occurs, the ndings should not be ignored. Another limitation in this and the original derivation study for the SFSR was that some of the predictor variables could have been dened as outcomes. For example, if a patient had an arrhythmia thought to cause the event (one of the outcome denitions), it could have been the same arrhythmia that was seen on the initial ECG. We also only reviewed specic changes in those ECGs that were considered abnormal, and it is possible that some of the ECGs meeting normal criteria had some old changes that may have been important. However, that would have pertained to only four such ECGs, and including all other normal ECGs without outcomes in our analysis would have yielded little information but added background noise to our analysis. Finally, we may not have considered all specic ndings that could have been important, such as right or left ventricular hypertrophy. CONCLUSIONS There are many factors that go into evaluating the patient with syncope. ECG and rhythm ndings from all sources (multiple ECGs and rhythm strips) are important. The ECG criteria from the San Francisco Syncope Rules are relatively simple and if used correctly can predict which patients are at risk of cardiac outcomes. Furthermore, any left branch bundle block conduction problems or any nonsinus rhythms found during the ED evaluation of patients with syncope should be particularly concerning.
718
Quinn and Mc Dermott
ECG FINDINGS IN ED PATIENTS WITH SYNCOPE
References 1. Blanc JJ, LHer C, Touiza A, Garo B, LHer E, Mansourati J. Prospective evaluation and outcome of patients admitted for syncope over a 1 year period. Eur Heart J. 2002; 23:81520. 2. Quinn JV, Stiell IG, McDermott DA, Sellers KL, Kohn MA, Wells GA. Derivation of the San Francisco Syncope Rule to predict patients with shortterm serious outcomes. Ann Emerg Med. 2004; 43:22432. 3. Kapoor WN. Syncope. NEJM. 2000; 343:185662. 4. Soteriades ES, Evans JC, Larson MG, et al. Incidence and prognosis of syncope. N Engl J Med. 2002; 347:87885. 5. Sun BC, Emond JA, Camargo CA Jr. Direct medical costs of syncope-related hospitalizations in the United States. Am J Cardiol. 2005; 95:66871. 6. Cosgriff T. External Validation of the San Francisco Syncope Rule in the Australian context. CJEM. 2007; 9:15761. 7. Birnbaum A, Esses D, Bijur P, Wollowitz A, Gallagher EJ. Failure to validate the San Francisco Syncope Rule in an independent emergency department population. Ann Emerg Med. 2008; 52:1519. 8. Thiruganasambandamoorthy V, Hess EP, Alreesi A, Perry JJ, Wells GA, Stiell IG. External validation of the San Francisco Syncope Rule in the Canadian setting. Ann Emerg Med. 2010; 55:46472. 9. Costantino G, Perego F, Dipaola F, et al. Short- and long-term prognosis of syncope, risk factors, and role of hospital admission: results from the STePS (Short-Term Prognosis of Syncope) study. J Am Coll Cardiol. 2008; 51:27683. 10. Reed MJ, Newby DE, Coull AJ, Prescott RJ, Jacques KG, Gray AJ. The ROSE (risk stratication of syncope in the emergency department) study. J Am Coll Cardiol. 2010; 55:71321.
11. Quinn J, McDermott D, Stiell I, Kohn M, Wells G. Prospective validation of the San Francisco Syncope Rule to predict patients with serious outcomes. Ann Emerg Med. 2006; 47:44854. 12. Martin TP, Hanusa BH, Kapoor WN. Risk stratication of patients with syncope. Ann Emerg Med. 1997; 29:45966. 13. Sarasin FP, Hanusa BH, Perneger T, Louis-Simonet M, Rajeswaran A, Kapoor WN. A risk score to predict arrhythmias in patients with unexplained syncope. Acad Emerg Med. 2003; 10:13127. 14. Del Rosso A, Ungar A, Maggi R, et al. Clinical predictors of cardiac syncope at initial evaluation in patients referred urgently to a general hospital: the EGSYS score. Heart. 2008; 94:16206. 15. Sun BC, Mangione CM, Merchant G, et al. External validation of the San Francisco Syncope Rule. Ann Emerg Med. 2007; 49:4207. 16. McDermott D, Quinn J. Response to failure to validate the San Francisco Syncope Rule in an independent emergency department population [letter]. Ann Emerg Med. 2009; 53:693. 17. Hsieh FY, Bloch DA, Larsen MD. A simple method of sample size calculation for linear and logistic regression. Stat Med. 1998; 17:162334. 18. Brignole M, Alboni P, Benditt DG, et al. Guidelines on management (diagnosis and treatment) of syncope-update 2004. Executive Summary. Eur Heart J. 2004; 25:205472. 19. Huff JS, Decker WW, Quinn JV, et al. Clinical policy: critical issues in the evaluation and management of adult patients presenting to the emergency department with syncope. Ann Emerg Med. 2007; 49:43144. 20. Colivicchi F, Ammirati F, Melina D, Guido V, Imperoli G, Santini M. Development and prospective validation of a risk stratication system for patients with syncope in the emergency department: the OESIL risk score. Eur Heart J. 2003; 24:8119.
Copyright of Academic Emergency Medicine is the property of Wiley-Blackwell and its content may not be copied or emailed to multiple sites or posted to a listserv without the copyright holder's express written permission. However, users may print, download, or email articles for individual use.
Vous aimerez peut-être aussi
- Detection of Silent Myocardial Ischemia in Asymptomatic Diabetic SubjectsDocument8 pagesDetection of Silent Myocardial Ischemia in Asymptomatic Diabetic SubjectsDiah Kris AyuPas encore d'évaluation
- Missed Ischemic Stroke Diagnosis in The Emergency Department by Emergency Medicine and Neurology ServicesDocument7 pagesMissed Ischemic Stroke Diagnosis in The Emergency Department by Emergency Medicine and Neurology ServicesReyhansyah RachmadhyanPas encore d'évaluation
- Early Prediction of Severity StrokeDocument11 pagesEarly Prediction of Severity StrokeainihanifiahPas encore d'évaluation
- Diagnosis of Left Ventricular Systolic Dysfunction (LVSD) : Development and Validation of A Clinical Prediction Rule in Primary CareDocument8 pagesDiagnosis of Left Ventricular Systolic Dysfunction (LVSD) : Development and Validation of A Clinical Prediction Rule in Primary CareVashish RamrechaPas encore d'évaluation
- McotrothmaDocument7 pagesMcotrothmaDayuKurnia DewantiPas encore d'évaluation
- Stroke PreventionDocument8 pagesStroke PreventionjaanhoneyPas encore d'évaluation
- Diabetes and Glycemic Control Linked to Heart Failure Risk in CAD PatientsDocument10 pagesDiabetes and Glycemic Control Linked to Heart Failure Risk in CAD PatientsEmy VishudPas encore d'évaluation
- 10.1007@s10554 020 01913 6Document10 pages10.1007@s10554 020 01913 6Bosman AriestaPas encore d'évaluation
- Electrical Injury Guidelines (Feb-05-09)Document9 pagesElectrical Injury Guidelines (Feb-05-09)Dwi WirastomoPas encore d'évaluation
- Increased Heart Rate During Walk Test Predicts Chronic-Phase Worsening of Renal Function in Patients With Acute Myocardial Infarction and Normal Kidney FunctionDocument10 pagesIncreased Heart Rate During Walk Test Predicts Chronic-Phase Worsening of Renal Function in Patients With Acute Myocardial Infarction and Normal Kidney Functionvn0328897777Pas encore d'évaluation
- Historical Criteria That Distinguish Syncope From SeizuresDocument7 pagesHistorical Criteria That Distinguish Syncope From SeizuresAlexPas encore d'évaluation
- Diabetes, Glycemic Control, and New-Onset Heart Failure in Patients With Stable Coronary Artery DiseaseDocument6 pagesDiabetes, Glycemic Control, and New-Onset Heart Failure in Patients With Stable Coronary Artery DiseaseAMADA122Pas encore d'évaluation
- Eur J Echocardiogr 2007 Scardovi 30 6Document7 pagesEur J Echocardiogr 2007 Scardovi 30 6Eman SadikPas encore d'évaluation
- F QRSDocument9 pagesF QRSaisyah hamzakirPas encore d'évaluation
- Clinical Cases in Heart FailureD'EverandClinical Cases in Heart FailureRavi V. ShahPas encore d'évaluation
- Admission Inferior Vena Cava Measurements Are Associated With Mortality After Hospitalization For Acute Decompensated Heart FailureDocument18 pagesAdmission Inferior Vena Cava Measurements Are Associated With Mortality After Hospitalization For Acute Decompensated Heart FailurePuja Nastia LubisPas encore d'évaluation
- 2001 - Value of ECG in AMI - JAMADocument8 pages2001 - Value of ECG in AMI - JAMAMichail PapafaklisPas encore d'évaluation
- Cardiac ArrhythmiasDocument5 pagesCardiac Arrhythmiastere glezPas encore d'évaluation
- Causes of Syncope in Patients With AlzheDocument8 pagesCauses of Syncope in Patients With AlzheMichael VavosaPas encore d'évaluation
- Effect of Right Ventricular Function and Pulmonary Pressures On Heart Failure PrognosisDocument7 pagesEffect of Right Ventricular Function and Pulmonary Pressures On Heart Failure PrognosisMatthew MckenziePas encore d'évaluation
- Calcium Channel Blocker Use and Mortality Among Patients With End-Stage Renal DiseaseDocument8 pagesCalcium Channel Blocker Use and Mortality Among Patients With End-Stage Renal DiseasekarenafiafiPas encore d'évaluation
- Theemergency Department Approachtosyncope: Evidence-Based Guidelinesand PredictionrulesDocument14 pagesTheemergency Department Approachtosyncope: Evidence-Based Guidelinesand PredictionrulesBruno J. DoppelgangerPas encore d'évaluation
- Cardio EstudantesDocument5 pagesCardio EstudantesNestor Torres MarinaPas encore d'évaluation
- MINOCA STEMI Manuscript 0Document19 pagesMINOCA STEMI Manuscript 0wellaPas encore d'évaluation
- Go 2006Document12 pagesGo 2006my accountPas encore d'évaluation
- Association of Low-Grade Albuminuria With Adverse Cardiac MechanicsDocument14 pagesAssociation of Low-Grade Albuminuria With Adverse Cardiac MechanicsM. Ryan RamadhanPas encore d'évaluation
- Gala TrialDocument11 pagesGala TrialRichard ZhuPas encore d'évaluation
- Clinical and Imaging Outcomes After Stroke With Normal AngiogramsDocument4 pagesClinical and Imaging Outcomes After Stroke With Normal AngiogramsAgustina 'tina' HartutiPas encore d'évaluation
- Heart Rate Variability and Myocardial Infarction Systematic Literature Review and Meta AnalysisDocument7 pagesHeart Rate Variability and Myocardial Infarction Systematic Literature Review and Meta Analysisea68afjePas encore d'évaluation
- Admission Serum Potassium in Patients With Acute Myocardial InfarctionDocument10 pagesAdmission Serum Potassium in Patients With Acute Myocardial InfarctionSurya UlhaqPas encore d'évaluation
- Komplikasi Stroke PDFDocument7 pagesKomplikasi Stroke PDFJose Hady PuteraPas encore d'évaluation
- Severe Hyperkalemia Can The Electrocardiogram Risk Stratify For Short-Term Adverse EventsDocument9 pagesSevere Hyperkalemia Can The Electrocardiogram Risk Stratify For Short-Term Adverse EventsCavalerul Mesei CromaticePas encore d'évaluation
- 1 s2.0 0735109795004548 MainDocument7 pages1 s2.0 0735109795004548 MainLuisa OsorioPas encore d'évaluation
- Age +estimated+glomerular+filtration+rate+and+ejection+fraction+score+predicts+contrast-Induced+acute+kidney+injury+in+patients+with+diabetes+and+chronic+kidney+disease +insight+from+the+TRACK-D+studyDocument5 pagesAge +estimated+glomerular+filtration+rate+and+ejection+fraction+score+predicts+contrast-Induced+acute+kidney+injury+in+patients+with+diabetes+and+chronic+kidney+disease +insight+from+the+TRACK-D+studyangga_darmawan26Pas encore d'évaluation
- ESCAPE Study - JAMA 2005Document9 pagesESCAPE Study - JAMA 2005MICHAEL AMARILLO CORREAPas encore d'évaluation
- Low Systemic Vascular ResistanceDocument7 pagesLow Systemic Vascular ResistanceMuhammad BadrushshalihPas encore d'évaluation
- Jurnal Gagal JantungDocument10 pagesJurnal Gagal Jantungindah ayuPas encore d'évaluation
- Nurses Application FormDocument7 pagesNurses Application FormVillanueva Ameera MaePas encore d'évaluation
- Dissert. AnisimovDocument7 pagesDissert. AnisimovcamiloPas encore d'évaluation
- Screening For Heart Disease in Diabetic SubjectsDocument4 pagesScreening For Heart Disease in Diabetic SubjectsHendro Adi KuncoroPas encore d'évaluation
- Review Articles: Medical ProgressDocument10 pagesReview Articles: Medical ProgressMiko AkmarozaPas encore d'évaluation
- Assessment of Palpitation Complaints Benign Paroxysmal Positional VertigoDocument6 pagesAssessment of Palpitation Complaints Benign Paroxysmal Positional VertigoHappy PramandaPas encore d'évaluation
- 1405 9940 Acm 92 2 203Document6 pages1405 9940 Acm 92 2 203abdul alvarez poncePas encore d'évaluation
- FCVM 05 00075Document7 pagesFCVM 05 00075Calon DokterPas encore d'évaluation
- In-Hospital Arrhythmia Development and Outcomes in Pediatric Patients With Acute MyocarditisDocument15 pagesIn-Hospital Arrhythmia Development and Outcomes in Pediatric Patients With Acute MyocarditisAnonymous OU6w8lX9Pas encore d'évaluation
- Evaluation Study of Congestive Heart Failure and Pulmonary Artery Catheterization EffectivenessDocument9 pagesEvaluation Study of Congestive Heart Failure and Pulmonary Artery Catheterization EffectivenessMelisa AnaPas encore d'évaluation
- SLMF - ResumenDocument5 pagesSLMF - ResumenMaría F SLPas encore d'évaluation
- Notes AKI - Evidence For Supporting Market NeedDocument2 pagesNotes AKI - Evidence For Supporting Market NeedSofia CunhaPas encore d'évaluation
- Prognostic Significance of PVCS and Resting Heart RateDocument9 pagesPrognostic Significance of PVCS and Resting Heart RateLivianty HukubunPas encore d'évaluation
- The Role of Tilt-Table Test in Differential Diagnosis of Unexplained SyncopeDocument7 pagesThe Role of Tilt-Table Test in Differential Diagnosis of Unexplained SyncopeYusrina Njoes SaragihPas encore d'évaluation
- Accuracy and Clinical Effect of Out of Hospital ElDocument10 pagesAccuracy and Clinical Effect of Out of Hospital ElAGGREY DUDUPas encore d'évaluation
- Blood Pressure and Clinical Outcomes in The International Stroke TrialDocument7 pagesBlood Pressure and Clinical Outcomes in The International Stroke TrialMif Al-HudaPas encore d'évaluation
- Cardiac ResuscitationDocument24 pagesCardiac ResuscitationPaulinaPas encore d'évaluation
- Comparison of Clinical Diagnosis With Computed Tomography in Ascertaining Type of StrokeDocument3 pagesComparison of Clinical Diagnosis With Computed Tomography in Ascertaining Type of StrokeDyah Wulan RamadhaniPas encore d'évaluation
- PE and CHFDocument9 pagesPE and CHFKu Li ChengPas encore d'évaluation
- HFN 031Document8 pagesHFN 031Isti RismaPas encore d'évaluation
- Randomized Trial of Stents Versus Bypass Surgery For Left Main Coronary Artery DiseaseDocument9 pagesRandomized Trial of Stents Versus Bypass Surgery For Left Main Coronary Artery DiseaseTommy WidjayaPas encore d'évaluation
- Rendina 2016Document9 pagesRendina 2016Sarital BoronPas encore d'évaluation
- RoladeDocument1 pageRoladeDIdit FAjar NUgrohoPas encore d'évaluation
- Dermatitis AtopikDocument8 pagesDermatitis Atopikpauling26Pas encore d'évaluation
- Diagnostic Row CTDocument13 pagesDiagnostic Row CTDIdit FAjar NUgrohoPas encore d'évaluation
- Reading Medical Article Treatment RCTDocument9 pagesReading Medical Article Treatment RCTDIdit FAjar NUgrohoPas encore d'évaluation
- Prognosis Heart FailureDocument9 pagesPrognosis Heart FailureDIdit FAjar NUgrohoPas encore d'évaluation
- Neuropathy PainDocument26 pagesNeuropathy PainDIdit FAjar NUgrohoPas encore d'évaluation
- Highlights: Signs of StrokeDocument16 pagesHighlights: Signs of StrokeDIdit FAjar NUgrohoPas encore d'évaluation
- Energy BalanceDocument10 pagesEnergy BalanceDIdit FAjar NUgrohoPas encore d'évaluation
- Post-Op Complications of Ventriculoperitoneal Shunt in Pediatric Hydrocephalus PatientsDocument18 pagesPost-Op Complications of Ventriculoperitoneal Shunt in Pediatric Hydrocephalus PatientsDIdit FAjar NUgrohoPas encore d'évaluation
- Aktivitas Antioksidan Psidium Guajava PDFDocument5 pagesAktivitas Antioksidan Psidium Guajava PDFDIdit FAjar NUgrohoPas encore d'évaluation
- Highlights: Signs of StrokeDocument16 pagesHighlights: Signs of StrokeDIdit FAjar NUgrohoPas encore d'évaluation
- Pedia TriDocument4 pagesPedia TriDIdit FAjar NUgrohoPas encore d'évaluation
- Scoring System of Syncope PDFDocument7 pagesScoring System of Syncope PDFDIdit FAjar NUgrohoPas encore d'évaluation
- Blok AV Dan SyncopeDocument4 pagesBlok AV Dan SyncopeDIdit FAjar NUgrohoPas encore d'évaluation
- Joc25028 1414 1419Document6 pagesJoc25028 1414 1419DIdit FAjar NUgrohoPas encore d'évaluation
- EKGDocument137 pagesEKGGbariel100% (3)
- AHA The ECG Examination PDFDocument41 pagesAHA The ECG Examination PDFSaeful AnwarudinPas encore d'évaluation
- ECG Basics: An Overview of ElectrocardiographyDocument51 pagesECG Basics: An Overview of ElectrocardiographyJamuna PatelPas encore d'évaluation
- MCQDocument64 pagesMCQade winataPas encore d'évaluation
- CASE PRESENTATION: UPPER GASTROINTESTINAL BLEEDING DUE TO DUODENAL ULCERDocument90 pagesCASE PRESENTATION: UPPER GASTROINTESTINAL BLEEDING DUE TO DUODENAL ULCERMaria Charis Anne IndananPas encore d'évaluation
- 001Document38 pages001Menly SusadaPas encore d'évaluation
- Hardware Implementation of ECG System On FPGADocument13 pagesHardware Implementation of ECG System On FPGAmadhuPas encore d'évaluation
- Presentasi Ska PIT IDIDocument63 pagesPresentasi Ska PIT IDIAyu WahyuniPas encore d'évaluation
- Aed NT-180Document63 pagesAed NT-180Nattawut ZuesatPas encore d'évaluation
- Case Study With ECG Reading OcañaDocument3 pagesCase Study With ECG Reading OcañaNicole Chloe OcanaPas encore d'évaluation
- Practice Essentials: Essential Updates: Distinguishing Between Left-And Right-Sided Atrial TachycardiaDocument28 pagesPractice Essentials: Essential Updates: Distinguishing Between Left-And Right-Sided Atrial TachycardiaRully SyahrizalPas encore d'évaluation
- Basic ECG Interpretation MWDocument211 pagesBasic ECG Interpretation MWLorelie AsisPas encore d'évaluation
- Blue Eyes Technology: - Monitoring Human-Operator SystemDocument16 pagesBlue Eyes Technology: - Monitoring Human-Operator SystemMohamed AbubackerPas encore d'évaluation
- Fba Imp Bits and KeyDocument7 pagesFba Imp Bits and Keybathula hariniPas encore d'évaluation
- Inventarisasi Rs Type DDocument63 pagesInventarisasi Rs Type DAnonymous 5wBxtyIPas encore d'évaluation
- Rapid Interpretation of EKG Sixth E Dition by by Dale Dubin: Direct DownloadDocument4 pagesRapid Interpretation of EKG Sixth E Dition by by Dale Dubin: Direct DownloadAlex HirschPas encore d'évaluation
- EKG ExamplesDocument9 pagesEKG ExamplesMayer Rosenberg99% (235)
- Electrical Conduction Pathway: Course Lesson Student Email Atika - Salsabila91@ui - Ac.idDocument12 pagesElectrical Conduction Pathway: Course Lesson Student Email Atika - Salsabila91@ui - Ac.idlemon kyuteaPas encore d'évaluation
- Ecg TeachingDocument44 pagesEcg TeachingarvindkanagaratnamPas encore d'évaluation
- Ecaps12c BSM Ug-ADocument128 pagesEcaps12c BSM Ug-Amogahid jojoPas encore d'évaluation
- Module 4 MedicineDocument50 pagesModule 4 Medicinepjanu86Pas encore d'évaluation
- 2013 - 04 - BeneView T8T5 Operation Manual (English) - v26.0Document438 pages2013 - 04 - BeneView T8T5 Operation Manual (English) - v26.0manualslibPas encore d'évaluation
- NUR3111 Post-Lecture QuizDocument28 pagesNUR3111 Post-Lecture QuizliPas encore d'évaluation
- Sample Transes 2Document11 pagesSample Transes 2Sophia SalamatPas encore d'évaluation
- GA Holter Part 3 Software V5 0 en 001Document70 pagesGA Holter Part 3 Software V5 0 en 001Richard RodríguezPas encore d'évaluation
- 9.2 Contingency TableDocument5 pages9.2 Contingency Tablebay nguyenPas encore d'évaluation
- Amsa232 PDFDocument4 pagesAmsa232 PDFSunny KumarPas encore d'évaluation
- LEPU MEDICAL Pocket ECG PCECG-500 CatalogDocument4 pagesLEPU MEDICAL Pocket ECG PCECG-500 CatalogAlbert KayPas encore d'évaluation
- Real-Time 3D Vectorcardiography: An Application For Didactic UseDocument8 pagesReal-Time 3D Vectorcardiography: An Application For Didactic Usealejandroescobar264Pas encore d'évaluation
- Manual of M8000 Veterinary MonitorDocument151 pagesManual of M8000 Veterinary MonitorCIBMEDICS SASPas encore d'évaluation