Académique Documents
Professionnel Documents
Culture Documents
Irritant Contact Dermatitis
Transféré par
syavirapsDescription originale:
Copyright
Formats disponibles
Partager ce document
Partager ou intégrer le document
Avez-vous trouvé ce document utile ?
Ce contenu est-il inapproprié ?
Signaler ce documentDroits d'auteur :
Formats disponibles
Irritant Contact Dermatitis
Transféré par
syavirapsDroits d'auteur :
Formats disponibles
Irritant Contact Dermatitis
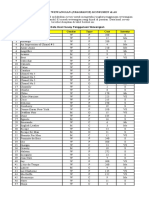
ICD is caused by exposure of the skin to chemical or other physical agents that are capable of irritating the skin, acutely or chronically. Severe irritants can cause toxic reactions even after a short exposure. Most cases, however, are caused by chronic cumulative exposure to one or more irritants. he hands are the most commonly affected area. In addition to dermatitis, irritant contact responses of the skin include! sub"ective irritancy, transient irritant reactions, persistent irritant reactions, toxic #caustic$ burn. Irritant contact responses of skin appendages and pigmentary system include! follicular and acneform eruptions, miliaria, pigmentary changes #hypo% and hyperpigmentation$, granulomatous reactions, and alopecia. &pidemiology ICD is the most common form of occupational skin disease, accounting for up to '() of all occupational skin disorders. *owever, ICD need not be occupational and can occur in anyone being exposed to a substance irritant or toxic to the skin. +ccupational &xposure Individuals engaged in the following occupations,activities are at risk for ICD! housekeepinghairdressing- medical, dental, and veterinary services- cleaning- floral arranging- agriculturehorticulture- forestry- food preparation and catering- printing- painting- metal work- mechanical engineering- car maintenance- construction- fishing. &tiology &tiologic .gents # able /%0$ .brasives, cleaning agents, oxidi1ing agents #e.g., sodium hypochlorite$- reducing agents #e.g., phenols, hydra1ine, aldehydes, thiophosphates$, plants #e.g., spurge, 2oracinaceae, 3anunculaceae$, animal en1ymes, secretions- dessicant powders, dust, soils- excessive exposure to water. able /%0 Most Common Irritant, oxic .gents
Soaps, detergents, waterless hand cleaners .cids and alkalis4! hydrofluoric acid, cement, chromic acid, phosphorus, ethylene oxide, phenol, metal salts. Industrial solvents! coal tar solvents, petroleum, chlorinated hydrocarbons, alcohol solvents, ethylene glycol ether, turpentine, ethyl ether, acetone, carbon dioxide, DMS+, dioxane, styrene. 5lants! &uphorbiaceae #spurges, crotons, poinsettias, machneel tree$. 3acunculaceae #buttercup$, Cruciferae #black mustard$, 6rticaceae #nettles$, Solanaceae #pepper, capsaicin$, +puntia #prickly pear$. +thers! fiberglass, wool, rough synthetic clothing, fire%retardant fabrics, 78C37 paper. 4 9ead to chemical burns and necrosis, if concentrated.
5redisposing :actors
.topics with a history of atopic dermatitis are at highest risk for ICD- the ma"ority of workers with significant occupational ICD are atopics. +thers! white skin, temperature #low$, climate #low humidity$, occlusion, mechanical irritation. Cement ICD tends to flare in summer in hot humid climates. 5athogenesis 2oth chemical and physical agents can be irritants, causing cell damage if applied for sufficient time and in ade;uate concentration. ICD occurs when defense or repair capacity of the skin is unable to maintain normal skin integrity and function or when penetration of chemical#s$ induces an inflammatory response. 9esser irritants cause reaction only after prolonged exposure. he initial reaction is usually limited to the site of contact with the irritant- the concentration of irritant diffusing outside the area of contact almost always falls below the critical threshold necessary to provoke a reaction. Mechanisms involved in acute and chronic phases of ICD are fundamentally different. .cute reactions involve direct cytotoxic damage to keratinocytes. Chronic ICD results from repeated exposures to solvents and surfactants that cause slow damage to cell membranes, disrupting the skin barrier and leading to protein denaturation and cellular toxicity. .cute Irritant Contact Dermatitis Symptoms In some individuals, sub"ective symptoms #burning, stinging, smarting$ may be the only manifestations. 5ainful sensations can occur within seconds after exposure #immediate%type stinging$, e.g., to acids, chloroform, and methanol. Delayed%type stinging occurs within 0 to / min, peaking at < to 0( min, fading by =( min, and is caused by agents such as aluminum chloride, phenol, propylene glycol, and others. In acute delayed ICD, ob"ective skin symptoms do not start until ' to /> after exposure #e.g., anthralin, ethylene oxide, ben1alconium chloride$ and are accompanied by burning rather then itching. 5hysical &xamination Skin :indings May occur minutes after exposure or may be delayed up to /> h. he spectrum of changes ranges from erythema to vesiculation and caustic burn with necrosis. .cute ICD represents sharply demarcated erythema and superficial edema, corresponding to the application site of the toxic substance. 9esions do not spread beyond the site of contact. In more severe reactions vesicles and blisters arise within the erythematous lesions, followed by erosions and,or even frank necrosis, as with acids or alkline solutions. 8o papules. Configuration often bi1arre or linear #7outside "ob7 or dripping effect$. &volution of 9esions &rythema with a dull, nonglistening surface vesiculation #or blister formation$ erosion crusting shedding of crusts and scaling or #in chemical burn$ erythema necrosisshedding of necrotic tissue ulceration healing.
Distribution Isolated, locali1ed to one region or generali1ed #plant dermatitis$, depending on contact with toxic agent. Duration
Days, weeks depending on tissue damage. Constitutional Symptoms 6sually none, but in widespread acute ICD 7acute illness7 syndrome, including fever. Chronic Irritant Contact Dermatitis ypes Cumulative ICD Most common- develops slowly after repeated additive exposure to mild irritants #water, soap, detergents etc.$, usually on hands. 3epeated exposures to toxic or subtoxic concentrations of offending agents usually associated with a chronic disturbance of the barrier function that allows even subtoxic concentrations of offending agents to penetrate into the skin and elicit a chronic inflammatory response- e.g., after repeated exposure to alkaline detergents and organic solvents, which, if applied only once to normal skin, do not elicit a reaction. In"ury #e.g., repeated rubbing of the skin$, prolonged soaking in water, or chronic contact after repeated, cumulative physical trauma ? friction, pressure, abrasions in individuals engaged in manual work #traumatic ICD$. Irritant 3eaction ICD &arly, subclinical dermatitis on hands of individuals exposed to wet work. 6sually during first months of training of hair dressers or of metal workers. Symptoms Stinging and itching, pain as fissures develop. 5hysical &xamination Skin :indings Dryness chapping erythema hyperkeratosis and scaling fissures and crusting. Sharp margination gives way to ill%defined borders, lichenification. In irritant reaction ICD also vesicles, pustules, and erosions. 6sually on hands #:ig. /%=$. In cumulative ICD usually starting at finger web spaces, spreading to sides and dorsal surface of hands and then to palms. In housewives often starting on finger tips #pulpitis$. 3arely in other locations exposed to irritants and,or trauma, e.g., in violinists on mandible or neck, or on exposed sites as in airborne ICD #see below$.
Duration Chronic, months to years. Constitutional Symptoms 8one, except when infection occurs. Chronic ICD #e.g., hand dermatitis- see below$ can become a severe occupational and emotional problem. 9aboratory &xamination
*istopathology In acute ICD, epidermal cell necrosis, neutrophils, vesiculation, and necrosis. In chronic ICD, acanthosis, hyperkeratosis, lymphocytic infiltrate. 5atch ests hese are negative in ICD unless allergic contact dermatitis is also present #see below$. Diagnosis and Differential Diagnosis Diagnosis is by history and clinical examination #lesions, pattern, site$. Most important differential diagnosis is .CD #see able /%=$. +n palms and soles! palmoplantar psoriasis- in exposed sites! photoallergic contact dermatitis. able /%= Differences 2etween Irritant and .llergic Contact Dermatitis4
Irritant CD Symptoms 9esions .cute .cute Stinging, smarting itching Chronic Itching,pain
.llergic CD Itching pain Itching,pain
&rythema vesicle erosion &rythema papules vesicles crust scaling erosions crust scaling fissures, 5apules, pla;ues, scaling, crusts
Chronic 5apules, pla;ues, scaling, crusts Margination and site .cute
Sharp, strictly confined to site of Sharp, confined to site of exposure but exposure spreading in the periphery- usually tiny papules- may become generali1ed Ill%defined, spreads hours after 8ot so rapid #0/ to @/ h after exposure$ 3apid #few exposure$
Chronic Ill%defined &volution .cute
Chronic Months to years of repeated Months or longer- exacerbation after exposure every reexposure Causative agents Dependent on concentration of agent and state of skin barrieroccurs only above threshold level May occur everyone in 3elatively independent of amount applied, usually very low concentrations sufficient but depends on degree of sensiti1ation
Incidence
practically +ccurs only in the sensiti1ed
4 Differences are printed in bold. Course and 5rognosis *ealing usually occurs within / weeks of removal of noxious stimuli- in more chronic cases, A weeks or longer may be re;uired. In the setting of occupational ICD, only one%third of individuals have complete remission and may re;uire allocation to another "ob- atopic individuals have a worse prognosis. In cases of chronic subcritical levels or irritant, some workers develop tolerance or 7hardening.7 Management
5revention .void irritant or caustic chemical#s$ by wearing protective clothing #i.e., goggles, shields, gloves$. If contact does occur, wash with water or weak neutrali1ing solution. 2arrier creams. In occupational ICD that persists in spite of adherence to the above measures, change of "ob may be necessary. reatment .cute Identify and remove the etiologic agent. Bet dressings with gau1e soaked in 2urowCs solution, changed every / to = h. 9arger vesicles may be drained, but tops should not be removed. opical class I glucocorticoid preparations. In severe cases, systemic glucocorticoids may be indicated. 5rednisone! /%week course, A( mg initially, tapering by steps of 0( mg. Subacute and Chronic Identify and remove etiologic,pathogenic agent. &mploy a potent topical glucocorticoid preparation, betamethasone dipropionate or clobetasol propionate, and provide ade;uate lubrication. .s healing occurs, continue with lubricating,protective creams or ointments. In chronic ICD of hands a 7hardening effect7 can be achieved in most cases with topical #soak or bath$%56D. therapy #see 5alms and Soles$. he newer topical anti%inflammatory agents #pimecrolimus and tacrolimus$ are being evaluated. .llergic Contact Dermatitis +ne of the most fre;uent, vexing, and costly skin problems. .n ec1ematous #papules, vesicles, pruritic$ dermatitis due to reexposure to a substance to which the individual is sensiti1ed. &pidemiology :re;uent. .ccounts for @) of occupationally related illnesses in the 6nited States. *owever, there are data suggesting that the actual indicence rate is 0( to <( times greater than reported in the 6.S. 2ureau of 9abor Statistics data. In addition, nonoccupational .CD is estimated to be three times greater than occupational .CD.
.ge of +nset 8o influence on capacity for sensiti1ation- however, allergic contact dermatitis is uncommon in young children and in individuals older than @( years. +ccupation +ne of the most important causes of disability in industry. 5athogenesis .CD is a classic, delayed, cell%mediated hypersensitivity reaction. &xposure to a strong sensiti1er such as poison ivy resin results in sensiti1ation in a week or so, while exposure to a weak allergen may take months to years for sensiti1ation. he antigen is taken up by 9angerhans cells in the epidermis, which process the antigen and migrate from the epidermis to the draining lymph nodes,
where they present the processed antigen in association with M*C class II molecules to cells that then proliferate. Sensiti1ed cells leave the lymph node, enter the blood circulation, home to the skin, and, after being presented by 9angerhans cells with the same specific antigen, produce and mediate the release by other cells of a variety of cytokines. hus, all the skin becomes hypersensitive to the contact allergen and will react wherever the specific allergen is represented. .llergens Contact allergens are diverse and range from metal salts to antibiotics, dyes to plant products. hus, allergens are found in "ewelry, personal care products, topical medications, plants, house remedies, and chemicals the individual may come in contact with at work. he most common allergens in the 6nited States are listed in able /%/. able /%/ op en Contact .llergens #8orth .merican Contact Dermatitis Eroup$ and +ther Common Contact .llergens
.llergen 8ickel sulfate 8eomycin sulfate 2alsam of 5eru :ragrance mix himerosal Sodium gold thiosulfate :ormaldehyde Fuaternium%0< Cobalt chloride 2acitracin Methyldibromoglutaronitrile, phenoxylethanol Carba mix &thyleneurea melamine%formaldehyde resin hiuram p%5henylene diamine 5arahydroxyben1oic acid ester 5ropylene glycol 5rocaine, ben1ocaine Sulfonamides urpentine Mercury salts Chromates Cinnamic aldehyde
5rincipal Sources of Contact Metals, metals in clothing, "ewelry, cataly1ing agents 6sually contained in creams, ointments opical medications :ragrances, cosmetics .ntiseptics Medication Disinfectant, curing agents, plastics Disinfectant Cement, galvani1ation, industrial oils, cooling agents, eyeshades +intments, powder 5reservatives, cosmetics 3ubber, latex extile additives 3ubber 2lack or dark dyes of textiles, printerCs ink Conserving agent in foodstuffs 5reservatives, cosmetics 9ocal anesthetics Medication Solvents, shoe polish, printerCs ink Disinfectant, impregnation Cement, antioxidants, industrial oils, matches, leather :ragrance, perfume
*istory he eruption starts in a sensiti1ed individual >' h or days after contact with the allergen- repeated exposures lead to a crescendo reaction, i.e., the eruption worsens. Site of the eruption is confined to site of exposure. Symptoms Sub"ective symptoms are intense pruritus- in severe reactions also stinging and pain. Constitutional Symptoms 7.cute illness7 syndrome, including fever, but only in severe allergic contact dermatitis #e.g., poison ivy$. 5hysical &xamination Skin 9esions he appearance of .CD depends on severity, location, and duration. ype .cute Bell%demarcated erythema and edema on which are superimposed closely spaced, nonumbilicated vesicles, and,or papules #:igs. /%> and /%<$- in severe reactions, bullae, confluent erosions exuding serum, and crusts #:ig. /%A$. Subacute 5la;ues of mild erythema showing small, dry scales, sometimes associated with small, red, pointed or rounded, firm papules. Chronic 5la;ues of lichenification #thickening of the epidermis with deepening of the skin lines in parallel or rhomboidal pattern$, scaling with satellite, small, firm, rounded or flat%topped papules, excoriations, erythema, and pigmentation. .rrangement Initially, confined to area of contact with allergen Ge.g., earlobe #earrings$, dorsum of foot #shoes$, wrist #watch or watch%band$, collar%like #necklace$, lips #lipstick$H. +ften linear, with artificial patterns, an 7outside "ob.7 5lant contact often results in linear lesions #e.g., 3hus dermatitis$. Initially confined to site of contact, later spreading beyond. Distribution &xtent Isolated, locali1ed to one region #e.g., shoe dermatitis$, or generali1ed #e.g., plant dermatitis$.
5attern 3andom or on exposed areas #as in airborne .CD$. Course &volution of .CD he duration of .CD varies among individuals, resolving in some in 0 to / weeks. .CD continues to get worse as long as allergen continues to come into contact with the skin. .cute &rythema papules vesicles erosions crusts scaling.
8ote! In the acute forms of contact dermatitis, papules occur only in .CD, not in ICD. Chronic 5apules scaling lichenification excoriations. Chronic inflammation with thickening,
fissuring, scaling, and crusting results. 8ote! Contact dermatitis is always confined to the site of exposure to the allergen. Margination is originally sharp in .CD- however, it spreads in the periphery beyond the actual site of exposure. If strong sensiti1ation has occurred, spreading to other parts of the body and generali1ation occur. he main differences between toxic irritant and allergic contact dermatitis are summari1ed in able /%=. 9aboratory &xaminations Dermatopathology .cute 5rototype of spongiotic dermatitis. Inflammation with intraepidermal intercellular edema #spongiosis$, lymphocytes and eosinophils in the epidermis, and monocyte and histiocyte infiltration in the dermis. Chronic In chronic .CD there are also spongiosis plus acanthosis, elongation of rete ridges, and elongation and broadening of papillae- hyperkeratosis- and a lymphocytic infiltrate. 5atch ests In .CD sensiti1ation is present on every part of the skin- therefore, application of the allergen to any area of normal skin provokes an ec1ematous reaction. . positive patch test shows erythema and papules, as well as possibly vesicles confined to the test site. 5atch tests should be delayed until the dermatitis has subsided for at least / weeks and should be performed on a previously uninvolved site. #See Clinical ests.$ Diagnosis and Differential Diagnosis
2y history and clinical findings including evaluation of site and distribution. *istopathology may be helpful- verification of offending agent #allergen$ by patch test. &xclude ICD # able /%=$, atopic dermatitis, seborrheic dermatitis #face$, psoriasis #palms and soles$, epidermal dermatophytosis #I+*$, fixed drug eruption, erysipelas phytophotodermatitis. 5hysical &xamination Skin 9esions Initially, well%demarcated patches of erythema, characteristic linear lesions #:ig. /%@$- rapidly evolve into papules and edematous pla;ues- may be severe especially on face and,or genitals, resembling cellulitis #:ig. /%'$. Microvesiculation may evolve to vesicles and,or bullae. &rosions, crusts. Bith resolution, erythematous pla;ues Jscale, Jerosion, Jcrusting. 5ostinflammatory hyperpigmentation common in darker skinned individuals. Distribution Most commonly on exposed extremities, where contact with the plant occurs- blotting can transfer to any exposed site- palms,soles are usually spared- however, lateral fingers can be involved. Clothing%5rotected Sites +leoresin can penetrate damp clothing onto covered skin. 8onexposed Sites 7Id7%like reaction or some systemic absorption can be associated with disseminated urticarial, erythema multiforme%like, or scarlatiniform lesions away from sites of exposure in some individuals with well%established .5D. 9aboratory &xaminations Dermatopathology See .CD, above. 5atch ests with 5entadecylcatechols Contraindicated. Can sensiti1e the individual to hapten. Diagnosis 2y history and clinical findings. Differential Diagnosis .CD to other allergens, phytophotodermatitis, soft%tissue infection #cellulitis, erysipelas$, atopic dermatitis, inflammatory dermatophytosis, early herpes 1oster, fixed drug eruption. Management of .CD ermination of &xposure Identify and remove the etiologic agent.
opical herapy opical glucocorticoid ointments,gels #classes I to III$ are effective for early nonbullous lesions. 9arger vesicles may be drained, but tops should not be removed. Bet dressings with cloths soaked in 2urowCs solution changed every / to = h. Since treatment with glucocorticoids is usually short%term in .CD, there is usually no danger of glucocorticoid side effects. .n exception is airborne .CD, which may re;uire systemic treatment. he newer immunomodulating topicals pimecrolimus and tacrolimus are effective in .CD but are still being evaluated. Systemic herapy Elucocorticoids are indicated if severe #i.e., if patient cannot perform usual daily functions, cannot sleep$ for exudative lesions. 5rednisone beginning at @( mg #adults$, tapering by < to 0( mg,d over a 0% to /%week period. In airborne .CD where complete avoidance of allergen may be impossible, immunosuppression with oral cyclosporine may become necessary. .topic Dermatitis .topic dermatitis #.D$ is an acute, subacute, or chronic relapsing skin disorder that usually begins in infancy and is characteri1ed principally by dry skin and pruritus- conse;uent rubbing and scratching lead to lichenification and hence to further itching and scratching #itch%scratch cycle$. he diagnosis is based on clinical findings, although the serum Ig& level is usually #'<)$ elevated. .D is often associated with a personal or family history of .D, allergic rhinitis, and asthma- =<) of infants with .D develop asthma later in life. Synonyms! Ig& dermatitis, 7ec1ema,7 atopic ec1ema. See more images in the Eallery. &pidemiology .ge of +nset :irst / months of life and by the first years in A() of patients. =() are seen for the first time by age <, and only 0() develop .D between A and /( years of age. 3arely .D has an adult onset. Eender Slightly more common in males than females. 5revalence 2etween @ and 0<) reported in population studies in Scandinavia and Eermany. Eenetic .spects he inheritance pattern has not been ascertained. *owever, in one series, A() of adults with .D had children with .D. he prevalence in children was higher #'0)$ when both parents had .D. &liciting :actors Inhalants Specific aeroallergens, especially dust mites and pollens, have been shown to cause exacerbations of
.D. Microbial .gents &xotoxins of Staphylococcus aureus may act as superantigens and stimulate activation of macrophages. .utoallergens Sera of patients with .D contain Ig& antibodies directed at human proteins. he release of these autoallergens from damaged tissue could trigger Ig& or cell responses, suggesting maintenance of allergic inflammation by endogenous antigens. :oods Subset of infants and children have flares of .D with eggs, milk, peanuts, soybeans, fish, and wheat. +ther &xacerbating :actors Skin 2arrier Disruption! decrease of barrier function associated with reduced ceramide levels and increased transepidermal water loss by fre;uent bathing and hand washing- dehydration is an important exacerbating factor. Infections! S. aureus is almost always present in severe cases- group . streptococcus- rarely fungus #dermatophytosis, candidiasis$. Season! in temperate climates, .D usually improves in summer, flares in winter. Clothing! pruritus flares after taking off clothing. Bool is an important trigger- wool clothing or blankets directly in contact with skin #also wool clothing of parents, fur of pets, carpets$. &motional Stress! results from the disease or is itself an exacerbating factor in flares of the disease. 5athogenesis Complex interaction of skin barrier, genetic, environmental, pharmacologic, and immunologic factors. ype I #Ig&%mediated$ hypersensitivity reaction occurring as a result of the release of vasoactive substances from both mast cells and basophils that have been sensiti1ed by the interaction of the antigen with Ig& #reaginic or skin%sensiti1ing antibody$. he role of Ig& in .D is still not fully clarified, but epidermal 9angerhans cells possess high%affinity Ig& receptors through which an ec1ema%like reaction can be mediated. */ and *0 both contribute to skin inflammation in .D. .ctute cell infiltration in .D is associated with a predominance of interleukin #I9$ > and I9%0= expression, and chronic inflammation in .D with increased I9%<, granulocyte%macrophage colony%stimulating factor cells and
#EM%CS:$, I9%0/, and interferon #I:8$ of cell activation.
. hus, skin inflammation in .D shows a biphasic pattern
*istory Skin Symptoms 5atients have dry skin. 5ruritus is the sine ;ua non of atopic dermatitis?7ec1ema is the itch that rashes.7 he constant scratching leads to a vicious cycle of itch scratch rash itch.
+ther Symptoms of .topy .llergic rhinitis, characteri1ed by snee1ing, rhinorrhea, obstruction of nasal passages, con"uctival and pharyngeal itching, and lacrimation- may be seasonal when associated with pollen. 5hysical &xamination Skin 9esions .cute 5oorly defined erythematous patches, papules, and pla;ues with or without scale. &dema with widespread involvement- skin appears 7puffy7 and edematous #:ig. /%0($. &rosions! moist, crusted. 9inear or punctate, resulting from scratching. Secondarily infected sites! S. aureus. +o1ing erosions #:igs. /%00 and /%0/$ and,or pustules #usually follicular$. Crusts. Chronic 9ichenification #thickening of the skin with accentuation of skin markings$! results from repeated rubbing or scratching #:ig. /%0=$- follicular lichenification #especially in brown and black persons$ #:ig. /%0>$. :issures! painful, especially in flexures #:ig. /%0<$, on palms, fingers, and soles. .lopecia! lateral one%third of the eyebrows as a result of rubbing. 5eriorbital pigmentation! also as a result of compulsively rubbing. Characteristic infraorbital fold in the eyelids #Dennie%Morgan sign$. Distribution 5redilection for the flexures, front and sides of the neck, eyelids, forehead, face, wrists, and dorsa of the feet and hands #Image /%0$. Eenerali1ed in severe disease. Special :eatures 3elated to &thnicity In blacks, so%called follicular ec1ema is common and is characteri1ed by discrete follicular papules #:ig. /%0>$ involving all hair follicles of the involved site. Special :eatures 3elated to .ge Infantile .D he lesions present as red skin, tiny vesicles on 7puffy7 surface. Scaling, exudation with wet crusts and cracks #fissures$ #:igs. /%0(, /%00, and /%0/$. Skin lesions seem to be a reaction to itching and
rubbing. Childhood% ype .D he lesions are papular, lichenified pla;ues, erosions, crusts, especially on the antecubital and popliteal fossae #:igs. /%0=, /%0>, /%0<, and /%0A$, the neck and face. .dult% ype .D here is a similar distribution, with lichenification and exoriations being the most conspicuous symptoms #:ig. /%0@$. .ssociated :indings 7Bhite7 dermatographism is a special and uni;ue feature of involved skin! stroking will not lead to redness as in normal skin but to blanching- delayed blanch to cholinergic agents. Ichthyosis vulgaris and keratosis pilaris occur in 0() of patients. Dernal con"uctivitis with papillary hypertrophy or cobblestoning of upper eyelid con"uctiva. .topic keratocon"unctivitis is disabling, may result in corneal scarring. Ieratoconus rare. Cataracts in a small percentage. Diagnosis *istory in infancy, clinical findings #typical distribution sites, morphology of lesions, white dermatographism$. Differential Diagnosis Seborrheic dermatitis, ICD, .CD, psoriasis, nummular ec1ema, dermatophytosis, early stages of mycosis fungoides. 3arely, acrodermatitis enteropathica, glucagonoma syndrome, histidinemia, phenylketonuria- also, some immunologic disorders including Biskott%.ldrich syndrome, K%linked agammaglobulinemia, hyper%Ig& syndrome, 9etterer%Siwe disease, and selective Ig. deficiency. 9aboratory &xaminations 2acterial Culture Coloni1ation with S. aureus is very common in the nares and in the involved skin- almost L() of patients with severe .D are secondarily coloni1ed,infected. 9ook out for M3S.. Diral Culture 3ule out herpes simplex virus #*SD$ infection in crusted lesions #ec1ema herpeticum- see Section /<$. 2lood Studies Increased Ig& in serum, eosinophilia. Dermatopathology Darious degrees of acanthosis with rare intraepidermal intercellular edema #spongiosis$. he dermal infiltrate is composed of lymphocytes, monocytes, and mast cells with few or no eosinophils.
Special :orms of .D *and Dermatitis .ggravated by wetting and washing with detergents, harsh soaps, and disinfectants- leads to ICD in the atopic. Clinically indistinguishable from 7normal ICD7 #see Special :orms of ICD$. &xfoliative Dermatitis #See Section '$ &rythroderma in patients with extensive skin involvement. Eenerali1ed redness, scaling, weeping, crusting, lymphadenopathy, fever, and systemic toxicity. Course and 5rognosis 6ntreated involved sites persist for months or years. Spontaneous, more or less complete remission during childhood occurs in M>() with occasional, more severe recurrences during adolescence. In many patients, the disease persists for 0< to /( years, but is less severe. :rom =( to <() of patients develop asthma and,or hay fever. .dult%onset .D often runs a severe course. S. aureus infection leads to extensive erosions and crusting, and herpes simplex infection to ec1ema herpeticum, which may be life%threatening #see Section /<$. Management &ducation of the patient to avoid rubbing and scratching is most important. opical antipruritic #menthol,camphor$ lotions are helpful in controlling the pruritus but are useless if emollients are not used and the patient continues to scratch and rub the pla;ues. .n allergic workup is rarely helpful in uncovering an allergen- however, in patients who are hypersensitive to house dust, mites, various pollens, and animal hair proteins, exposure to the appropriate allergen may cause flares. .topic dermatitis is considered by many to be related, at least in part, to emotional stress. 5atients should be warned of their special problems with herpes simplex and the fre;uency of superimposed staphylococcal infection, for which oral antibiotics are indicated. .ntiviral drugs for herpes simplex are indicated if *SD infection is suspected. .cute 0. Bet dressings and topical glucocorticoids- topical antibiotics #mupirocin ointment$ when indicated. /. *ydroxy1ine, 0( to 0(( mg ;id for pruritus. =. +ral antibiotics #dicloxacillin, erythromycin$ to eliminate S. aureus and treat M3S. according to sensitivity as shown by culture. Subacute and Chronic 0. *ydration #oilated baths or baths with oatmeal powder$ followed by application of unscented emollients #e.g., hydrated petrolatum$ form the basic daily treatment needed to prevent xerosis. Soap showers are permissible to wash the body folds, but soap should seldom be used on the other parts of the skin surface. 0/) ammonium lactate or 0() % hydroxy acid lotion is very effective for the xerosis seen in .D. /. opical anti%inflammatory agents such as glucocorticoids, hydroxy;uinoline preparations, and tar are the mainstays of treatment. +f these, glucocorticoids are the most effective. *owever, topical glucocorticoids may lead to skin atrophy if used for prolonged periods of
time and if used excessively will lead to suppression of the pituitary%adrenal axis, osteoporosis, growth retardation. .nother problem is 7glucocorticoidophobia.7 5atients or their parents are increasingly aware of glucocorticoid side effects and refuse their use, no matter how beneficial they may be. =. 8ew nonsteroidal anti%inflammatory agents are now available and will probably replace glucocorticoids for most patients in the future. hese are topical tacrolimus and pimecrolimus. hey potently suppress itching and inflammation and do not lead to skin atrophy. he only problem with tacrolimus is that some patients cannot tolerate the immediate #but transient$ burning on application. 2urning is less of a problem with pimecrolimus. >. +ral *0 antihistamines are useful in reducing itching. <. Systemic glucocorticoids should be avoided, except in rare instances in adults for only short courses #rescue treatment$. hey are widely overused. +steopenia and cataracts are complications. :or severe intractable disease, prednisone, A( to '( mg daily for / days, then halving the dose each / days for the next A days. 5atients with .D tend to become dependent on oral glucocorticoids. +ften, small doses #< to 0( mg$ make the difference in control and can be reduced gradually to even /.< mg,d, as is often used for the control of asthma. Intramuscular glucocorticoids are risky and should be avoided. A. 6D.%6D2 phototherapy #combination of 6D. plus 6D2 and increasing the radiation dose each treatment, with a fre;uency of two to three times weekly$. 8arrow band 6D #=00 nm$, 56D. photochemotherapy also effective. @. In severe cases of adult .D and in normotensive healthy persons without renal disease cyclosporin treatment #starting dose < mg,kg per day$ is indicated when all other treatments fail, but should be monitored closely. reatment is limited to = to A months because of potential side effects, including hypertension and reduced renal function. 2lood pressure should be checked weekly and chemistry panels biweekly. 8ifedipine can be used for moderate increases in blood pressure. '. 5atients should learn and use stress management techni;ues. L. . suggested algorithm of .D management is as follows! 2aseline therapy of dryness with emollients Suppression of mild to moderate .D by prolonged topical pimecrolimus or tacrolimus and continued emollients Supression of severe flares with topical glucocorticoids followed by pimecrolimus or tacrolimus and emollients +ral and topical antibiotics to eliminate S. aureus *ydroxy1ine to suppress pruritus
Vous aimerez peut-être aussi
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeD'EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeÉvaluation : 4 sur 5 étoiles4/5 (5794)
- Charlotte Bronte - Jane Eyre PDFDocument499 pagesCharlotte Bronte - Jane Eyre PDFAayushi JindalPas encore d'évaluation
- The Yellow House: A Memoir (2019 National Book Award Winner)D'EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Évaluation : 4 sur 5 étoiles4/5 (98)
- Festivals (1st District of Albay)Document3 pagesFestivals (1st District of Albay)Nor Antonette Bongao BamianoPas encore d'évaluation
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryD'EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryÉvaluation : 3.5 sur 5 étoiles3.5/5 (231)
- Kobelco SK 200 10 ManualDocument1 312 pagesKobelco SK 200 10 Manualivan skyler anjaya96% (80)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceD'EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceÉvaluation : 4 sur 5 étoiles4/5 (895)
- Ssi Cai Company Profile 2015Document30 pagesSsi Cai Company Profile 2015Kim Lee CoPas encore d'évaluation
- The Little Book of Hygge: Danish Secrets to Happy LivingD'EverandThe Little Book of Hygge: Danish Secrets to Happy LivingÉvaluation : 3.5 sur 5 étoiles3.5/5 (400)
- Neverwas Excerpt by Kelly Moore, Tucker Reed & Larkin ReedDocument7 pagesNeverwas Excerpt by Kelly Moore, Tucker Reed & Larkin Reedevenstar818Pas encore d'évaluation
- Shoe Dog: A Memoir by the Creator of NikeD'EverandShoe Dog: A Memoir by the Creator of NikeÉvaluation : 4.5 sur 5 étoiles4.5/5 (537)
- 08-18-11 - Moneysaver - Lewis-Clark EditionDocument20 pages08-18-11 - Moneysaver - Lewis-Clark EditionDavid ArndtPas encore d'évaluation
- Never Split the Difference: Negotiating As If Your Life Depended On ItD'EverandNever Split the Difference: Negotiating As If Your Life Depended On ItÉvaluation : 4.5 sur 5 étoiles4.5/5 (838)
- Flange Management Procedure IFUDocument32 pagesFlange Management Procedure IFUMarvan Audy Buriko100% (1)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureD'EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureÉvaluation : 4.5 sur 5 étoiles4.5/5 (474)
- NoitcelesDocument69 pagesNoitcelesAngela CudiaPas encore d'évaluation
- Grit: The Power of Passion and PerseveranceD'EverandGrit: The Power of Passion and PerseveranceÉvaluation : 4 sur 5 étoiles4/5 (588)
- Josee, The Tiger and The Fish DarkDocument193 pagesJosee, The Tiger and The Fish Darklacaron.kurtalexanderPas encore d'évaluation
- DLP-TLE (Masonry 9)Document6 pagesDLP-TLE (Masonry 9)colleenPas encore d'évaluation
- The Emperor of All Maladies: A Biography of CancerD'EverandThe Emperor of All Maladies: A Biography of CancerÉvaluation : 4.5 sur 5 étoiles4.5/5 (271)
- 06 Raise Organic Small RuminantsDocument44 pages06 Raise Organic Small RuminantsAlma Chavez Cubilla88% (8)
- On Fire: The (Burning) Case for a Green New DealD'EverandOn Fire: The (Burning) Case for a Green New DealÉvaluation : 4 sur 5 étoiles4/5 (74)
- Medieval ChairDocument21 pagesMedieval ChairRamona Gheorghe100% (1)
- Team of Rivals: The Political Genius of Abraham LincolnD'EverandTeam of Rivals: The Political Genius of Abraham LincolnÉvaluation : 4.5 sur 5 étoiles4.5/5 (234)
- The Red Death (Edgar Allan Poe)Document4 pagesThe Red Death (Edgar Allan Poe)Mariana OteroPas encore d'évaluation
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaD'EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaÉvaluation : 4.5 sur 5 étoiles4.5/5 (266)
- My Dear Henry: A Jekyll & Hyde Remix by Kalynn BayronDocument16 pagesMy Dear Henry: A Jekyll & Hyde Remix by Kalynn BayronMacmillan KidsPas encore d'évaluation
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersD'EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersÉvaluation : 4.5 sur 5 étoiles4.5/5 (344)
- Analisa FragranceDocument4 pagesAnalisa Fragrancezulfardi asharPas encore d'évaluation
- YUE Issue0112Document138 pagesYUE Issue0112Sydney F. SarachanPas encore d'évaluation
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyD'EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyÉvaluation : 3.5 sur 5 étoiles3.5/5 (2259)
- Endangered by Eliot Schrefer ExcerptDocument30 pagesEndangered by Eliot Schrefer ExcerptI Read YA50% (6)
- Clothing IndustryDocument5 pagesClothing IndustrySyed Aashir Raza BilgramiPas encore d'évaluation
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreD'EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreÉvaluation : 4 sur 5 étoiles4/5 (1090)
- H & M Chemical Restrictions - 2009-12-14Document52 pagesH & M Chemical Restrictions - 2009-12-14xtrayangPas encore d'évaluation
- Revenge Is All The SweeterDocument228 pagesRevenge Is All The Sweetererica babad100% (1)
- Rocket Age - Signature CharactersDocument27 pagesRocket Age - Signature Charactersalegurthatain100% (1)
- The Unwinding: An Inner History of the New AmericaD'EverandThe Unwinding: An Inner History of the New AmericaÉvaluation : 4 sur 5 étoiles4/5 (45)
- MoraHernandez Gonzalo MO7S1AI1 WORDDocument3 pagesMoraHernandez Gonzalo MO7S1AI1 WORDJesus Antonio Lopez LoyaPas encore d'évaluation
- Bohemian EarringsDocument5 pagesBohemian Earringsmahira_tippu100% (1)
- Wim Hof InterviewDocument7 pagesWim Hof InterviewMacak50% (2)
- Proof of Work CSM - Mansi Goswami 2Document26 pagesProof of Work CSM - Mansi Goswami 2Sandeep SharmaPas encore d'évaluation
- Inside Crochet 57Document100 pagesInside Crochet 57Екатерина Матушинец100% (2)
- ConsumptionDocument20 pagesConsumptionProttoy DiptoPas encore d'évaluation
- Lead CostaDocument10 pagesLead Costavisha183240100% (1)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)D'EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Évaluation : 4.5 sur 5 étoiles4.5/5 (121)
- Fresh Reliance MartDocument62 pagesFresh Reliance MartHarsh VijayPas encore d'évaluation
- Beatriz Colomina - Sex Lies DecorationDocument12 pagesBeatriz Colomina - Sex Lies DecorationSue ChoiPas encore d'évaluation
- Her Body and Other Parties: StoriesD'EverandHer Body and Other Parties: StoriesÉvaluation : 4 sur 5 étoiles4/5 (821)