Académique Documents
Professionnel Documents
Culture Documents
CARDIAC EXAM CHECKLIST
Transféré par
Nazia SalmanTitre original
Copyright
Formats disponibles
Partager ce document
Partager ou intégrer le document
Avez-vous trouvé ce document utile ?
Ce contenu est-il inapproprié ?
Signaler ce documentDroits d'auteur :
Formats disponibles
CARDIAC EXAM CHECKLIST
Transféré par
Nazia SalmanDroits d'auteur :
Formats disponibles
CARDIAC EXAMINATION CHECKLIST 2012 - 2013
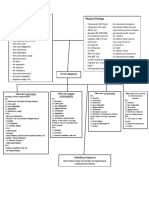
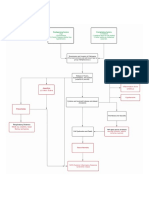
NOTE: Items with an asterisk * should be performed during the CCA exam. Please note you are responsible for the content knowledge of items without an asterisk that may be present on the written exam. Inspection (in sitting position) 1. Patient appearance (Comfortable, well appearing, anxious, short of breath, etc).* 2. Note any cyanosis, clubbing, pallor, cachexia, and tachypnea (see your physical diagnosis text for definition).* Vital signs, carotid pulses, jugular venous findings: 3. Check radial pulse for 15 seconds (Note pulse rate in beats per minute, also note if pulse is regular or irregular).* 4. Determine blood pressure in either arm. Patient should be in sitting position with YOU supporting his/her arm at heart level. Use appropriate sized cuff, and line up brachial artery with line on cuff. Pump cuff to 200 so you do not miss severe systolic hypertension. (Warn patient it may be a bit uncomfortable.)* 5. Ideally, blood pressure and pulse should be assessed in both the supine and sitting (or standing) positions in order to assess orthostatic changes. Be sure to allow the patient three to five minutes to equilibrate to the new position. 6. Position patient in supine position, with head elevated at 3045 degrees. Stand to the patients right.* 7. Inspect right carotid artery: Turn patients head to left, look for bounding pulses.* 8. Inspect right internal jugular vein while palpating right radial artery. Look for A waves and V waves (see text). State whether A wave is larger, smaller, or the same as the V wave. (This is NOT an easy task. Dont be frustrated if you cant see the waves).* 9. Sequentially palpate each carotid pulse. Are the pulses equal? Assess volume and upstroke (bounding, diminished, or delayed).*
Need to Practice
Feel Comfortable
CARDIAC EXAMINATION CHECKLIST 2012 - 2013 Need to Practice 10. Sequentially auscultate each carotid artery for bruits or transmitted murmurs.* 11. State the jugular venous pressure in centimeters of water (see text).* 12. Inspect precordium for abnormal pulsations.* Palpation 13. Palpate the apical impulse, and note its location (e.g. 5th intercostal space, midclavicular line). Note if the impulse is sharp or diffuse.* 14. Palpate the left parasternal borders for right ventricular heaves or thrills (a vibration representing a severe murmur).* 15. Palpate the 2nd left intercostal space for pulmonary artery pulsations.* 16. Palpate the suprasternal notch for aortic pulsations.* Auscultation (with head of bed up 30 45 degrees)* 17. Listen to the following areas of the precordium with both the bell and diaphragm: 2nd right intercostal space 2nd left intercostal space Left lower sternal border Apex 18. Listen for: S1 and S2 (Helpful hint: Palpate a carotid pulse while listening. S2 is after the carotid pulse).* Feel Comfortable
CARDIAC EXAMINATION CHECKLIST 2012 - 2013 Need to Practice 19. S3 and S4 (This can be tricky. S4 is before S1 and S2, and the three beats sound like Tennessee. S3 is after S1 and S2, and the sound is more like Kentucky.)* 20. Other sounds to listen for during systole and diastole: murmurs, rubs, clicks, opening snaps (see your physical diagnosis text for detailed descriptions).* 21. Ask patient to roll onto left side. Identify the apex by palpation (i.e., the point of maximal impulse or PMI). Using the bell, listen at the apex. This will bring out mitral valve abnormalities.* 22. Ask the patient to sit up and to inhale, exhale deeply, and then lean forward. Listen over the aortic and pulmonic areas for the diastolic murmur of aortic insufficiency and for pericardial rubs. (This maneuver is a particularly important one to master and remember.) Peripheral Vascular Exam 23. Inspect lower extremities for size, symmetry, color, temperature and venous patterns (e.g. venous stasis).* 24. Palpate lower extremities for signs of edema.* 25. Palpate lower extremity arterial pulses (i.e. dorsalis pedis and posterior tibial arteries).* Feel Comfortable
Vous aimerez peut-être aussi
- Cardiovascular Examination Checklist OSCEDocument1 pageCardiovascular Examination Checklist OSCESteve TanPas encore d'évaluation
- Farnsworth D15 Color Test KitDocument4 pagesFarnsworth D15 Color Test Kitdian eka saputraPas encore d'évaluation
- Lab 8 The Nervous SystemDocument15 pagesLab 8 The Nervous Systemcindy tranPas encore d'évaluation
- Cardiac Exam ChecklistDocument4 pagesCardiac Exam ChecklistZaidatul Atiqah MustafaPas encore d'évaluation
- H&P OutlineDocument5 pagesH&P Outlineginadaislu100% (1)
- General Exam What to See in a Comprehensive PhysicalDocument320 pagesGeneral Exam What to See in a Comprehensive Physicalmaybe100% (3)
- ECG Tutorial - Basic Principles of ECG Analysis - UpToDateDocument17 pagesECG Tutorial - Basic Principles of ECG Analysis - UpToDateImja94Pas encore d'évaluation
- Cardiovascular Examination:: General InspectionDocument6 pagesCardiovascular Examination:: General InspectionPhysician AssociatePas encore d'évaluation
- CVS Examination InstructionsDocument5 pagesCVS Examination Instructionsmagdy balahaPas encore d'évaluation
- Heart Assessment: Physical ExaminationDocument6 pagesHeart Assessment: Physical Examinationshannon c. lewisPas encore d'évaluation
- Cardiac Tamponade, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsD'EverandCardiac Tamponade, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsPas encore d'évaluation
- Valvular Heart Disease 2Document46 pagesValvular Heart Disease 2Topea BogdanPas encore d'évaluation
- Cardiovascular ExaminationDocument2 pagesCardiovascular ExaminationasimPas encore d'évaluation
- Valvular Heart DiseaseDocument10 pagesValvular Heart DiseaseEzyan SyaminPas encore d'évaluation
- Respiratory Assessment 2Document24 pagesRespiratory Assessment 2Kendal BartonPas encore d'évaluation
- Cardiovascular Examination GuideDocument2 pagesCardiovascular Examination Guiderhea100% (1)
- Thyroid Status Examination OSCE GuideDocument20 pagesThyroid Status Examination OSCE GuideemmaPas encore d'évaluation
- CARDIOVASCULAR DISEASES: SIGNS, SYMPTOMS AND TREATMENT OF HEART FAILUREDocument27 pagesCARDIOVASCULAR DISEASES: SIGNS, SYMPTOMS AND TREATMENT OF HEART FAILURESanthoshi Sadhanaa SankarPas encore d'évaluation
- Common Ecg Abnormalities PDFDocument2 pagesCommon Ecg Abnormalities PDFRonPas encore d'évaluation
- HW InotropesDocument3 pagesHW InotropesNatalie YeohPas encore d'évaluation
- Clinical MethodsDocument13 pagesClinical MethodsHashimIdreesPas encore d'évaluation
- Anatomy and Physiology of Blood VesselDocument3 pagesAnatomy and Physiology of Blood Vesselneleh grayPas encore d'évaluation
- Review of Systems and Physical Exam FindingsDocument6 pagesReview of Systems and Physical Exam FindingsJuliennePas encore d'évaluation
- Chest Pain: Sumit Bose, MD PGY-3Document55 pagesChest Pain: Sumit Bose, MD PGY-3Irfan100% (1)
- Medicine1 Grand PE ScriptDocument10 pagesMedicine1 Grand PE ScriptCarmeline Santi BeronillaPas encore d'évaluation
- Hemorrhagic Cerebro Vascular DiseaseDocument37 pagesHemorrhagic Cerebro Vascular Diseasejbvaldez100% (1)
- Body FluidsDocument6 pagesBody FluidsMemory MahwendaPas encore d'évaluation
- IM - Heart Failure Concept Map - PathophysDocument5 pagesIM - Heart Failure Concept Map - PathophysTrisPas encore d'évaluation
- Congestive Heart FailureDocument86 pagesCongestive Heart FailureNabeel ShahzadPas encore d'évaluation
- BBB EcgDocument33 pagesBBB EcgLokbre YoasPas encore d'évaluation
- Generic Name Therapeutic Classification Pharmacologic ClassificationDocument3 pagesGeneric Name Therapeutic Classification Pharmacologic ClassificationAnselle CasilPas encore d'évaluation
- Cardiovascular Exam Guide: Hands to NeckDocument13 pagesCardiovascular Exam Guide: Hands to NeckBitu JaaPas encore d'évaluation
- Almaghrabi Abdomen ExaminationDocument27 pagesAlmaghrabi Abdomen ExaminationSagit Nauman81100% (1)
- Breath Holding SpellDocument3 pagesBreath Holding SpellDimas Alphiano100% (1)
- 22 Ventricular Septal DefectDocument26 pages22 Ventricular Septal Defectdhiraj parmarPas encore d'évaluation
- Screening Head To Toe Physical ExaminationDocument16 pagesScreening Head To Toe Physical ExaminationJay Mar Mendoza BabatePas encore d'évaluation
- Terminology Causes of Cardiac Arrest C.P.R. For The Adult, Child & Baby Stroke & Stroke ManagementDocument28 pagesTerminology Causes of Cardiac Arrest C.P.R. For The Adult, Child & Baby Stroke & Stroke Managementbusiness911Pas encore d'évaluation
- Peripheral Vascular SystemDocument5 pagesPeripheral Vascular SystemBai-Rhema MarmayPas encore d'évaluation
- GIT OSCE (Week 9) : Mention You Would Observe General Appearance and Take VitalsDocument3 pagesGIT OSCE (Week 9) : Mention You Would Observe General Appearance and Take Vitalsrenae_vardPas encore d'évaluation
- Approach To Heart MurmursDocument57 pagesApproach To Heart MurmursRadley Jed PelagioPas encore d'évaluation
- CLINICAL EXAMINATION METHODSDocument18 pagesCLINICAL EXAMINATION METHODSPaolo BautistaPas encore d'évaluation
- Focused AssessmentDocument5 pagesFocused AssessmentPiyali SahaPas encore d'évaluation
- Nursing Management of Patient With Pericardial EffusionDocument2 pagesNursing Management of Patient With Pericardial EffusionAgung Alber0% (3)
- Management of diabetic ketoacidosis: principles of management in the first hourDocument13 pagesManagement of diabetic ketoacidosis: principles of management in the first hourAzim Abd Razak100% (1)
- Examination of The Respiratory SystemDocument2 pagesExamination of The Respiratory Systemkenners100% (17)
- Rheumatic Heart DiseaseDocument22 pagesRheumatic Heart DiseasemajdPas encore d'évaluation
- Congenital Heart DiseasesDocument6 pagesCongenital Heart Diseasestheglobalnursing100% (2)
- Percussion of The HeartDocument5 pagesPercussion of The HeartAbdul RahmanPas encore d'évaluation
- ECG Master Class-2Document138 pagesECG Master Class-2Shohag ID Center100% (1)
- Decreased Cardiac Output RM 7Document9 pagesDecreased Cardiac Output RM 7api-283470660Pas encore d'évaluation
- Cardiovascular History Taking and Physical ExaminationsDocument35 pagesCardiovascular History Taking and Physical ExaminationsEndalk AsfawPas encore d'évaluation
- Domingo, Precious Mae TDocument56 pagesDomingo, Precious Mae Tbevzie datuPas encore d'évaluation
- Introduction Definition: Types of PacemakersDocument8 pagesIntroduction Definition: Types of PacemakersPrasann RoyPas encore d'évaluation
- Congestive Heart Failure OverviewDocument12 pagesCongestive Heart Failure OverviewkazellePas encore d'évaluation
- Pulsus ParadoxusDocument2 pagesPulsus ParadoxusHassan.shehriPas encore d'évaluation
- HA - PA Findings Documentation (Head To Neck)Document9 pagesHA - PA Findings Documentation (Head To Neck)Bianca SandovalPas encore d'évaluation
- Basic Arrythmia AnalysisDocument60 pagesBasic Arrythmia AnalysisZakky KurniawanPas encore d'évaluation
- Abdominal Examination Check ListDocument9 pagesAbdominal Examination Check ListIbrahim Ahmed IbrahimPas encore d'évaluation
- Patient Education for Ileal Conduit CareDocument11 pagesPatient Education for Ileal Conduit CareICa MarlinaPas encore d'évaluation
- During The CCA Exam. Please Note You Are Responsible For The Content Knowledge of Items Without An Asterisk That May Be Present On The Written Exam.Document2 pagesDuring The CCA Exam. Please Note You Are Responsible For The Content Knowledge of Items Without An Asterisk That May Be Present On The Written Exam.helamahjoubmounirdmoPas encore d'évaluation
- Ventricular Septal Defect, A Simple Guide To The Condition, Treatment And Related ConditionsD'EverandVentricular Septal Defect, A Simple Guide To The Condition, Treatment And Related ConditionsPas encore d'évaluation
- A Simple Guide to Abdominal Aortic Aneurysm, Diagnosis, Treatment and Related ConditionsD'EverandA Simple Guide to Abdominal Aortic Aneurysm, Diagnosis, Treatment and Related ConditionsPas encore d'évaluation
- Please Answer The Following Questions:: QuestionnaireDocument2 pagesPlease Answer The Following Questions:: QuestionnaireNazia SalmanPas encore d'évaluation
- Please Answer The Following Questions:: QuestionnaireDocument2 pagesPlease Answer The Following Questions:: QuestionnaireNazia SalmanPas encore d'évaluation
- An16666 PDFDocument1 pageAn16666 PDFNazia SalmanPas encore d'évaluation
- HeidiDocument113 pagesHeidiTempenkePas encore d'évaluation
- Endometrial HyperplasiaDocument11 pagesEndometrial HyperplasiarinieeePas encore d'évaluation
- Anton Checkov's Swan Song DramaDocument18 pagesAnton Checkov's Swan Song DramaNazia SalmanPas encore d'évaluation
- Cricket and The Mathematical AgendaDocument17 pagesCricket and The Mathematical AgendaNazia SalmanPas encore d'évaluation
- Management of Gestational DiabetesDocument3 pagesManagement of Gestational DiabetesNazia SalmanPas encore d'évaluation
- The World of OzDocument87 pagesThe World of OzNazia SalmanPas encore d'évaluation
- Volume and Surface Area Formulas for ShapesDocument2 pagesVolume and Surface Area Formulas for ShapesNazia SalmanPas encore d'évaluation
- When To Use What Test PDFDocument8 pagesWhen To Use What Test PDFnetradeepPas encore d'évaluation
- BSC (Hons) Medical Biotechnology FlyerDocument4 pagesBSC (Hons) Medical Biotechnology FlyerNazia SalmanPas encore d'évaluation
- Tota - S For CAT 1Document2 pagesTota - S For CAT 1Nazia SalmanPas encore d'évaluation
- Adventures of Mr. ToadDocument37 pagesAdventures of Mr. ToadNazia SalmanPas encore d'évaluation
- 1 Month DietDocument5 pages1 Month DietNazia SalmanPas encore d'évaluation
- Chair: DR Ruqaiyyah Siddiqui Co-Chair: DR Naveed Khan Class of 2016'Document4 pagesChair: DR Ruqaiyyah Siddiqui Co-Chair: DR Naveed Khan Class of 2016'Nazia SalmanPas encore d'évaluation
- Guias Epoc Estabñe 2011.Document14 pagesGuias Epoc Estabñe 2011.Camilo Benavides BurbanoPas encore d'évaluation
- Median and Anterior Interosseous Nerve Entrapment Syndromes Versus Carpal Tunnel Syndrome: A Study of Two CasesDocument10 pagesMedian and Anterior Interosseous Nerve Entrapment Syndromes Versus Carpal Tunnel Syndrome: A Study of Two CasesNazia SalmanPas encore d'évaluation
- AtherenamDocument2 pagesAtherenamNazia SalmanPas encore d'évaluation
- .PHQ 9 Review Kroenke 63754Document7 pages.PHQ 9 Review Kroenke 63754Nazia SalmanPas encore d'évaluation
- Example To Exemplary EssaysDocument13 pagesExample To Exemplary EssaysNazia Salman100% (1)
- VR110531Document6 pagesVR110531Nazia SalmanPas encore d'évaluation
- 1 Month DietDocument5 pages1 Month DietNazia SalmanPas encore d'évaluation
- LaxativesDocument19 pagesLaxativesNazia SalmanPas encore d'évaluation
- Calculate Volume Using IntegrationDocument7 pagesCalculate Volume Using IntegrationMohammad Raimie RahimPas encore d'évaluation
- All About Vitamins & MineralsDocument42 pagesAll About Vitamins & MineralsHristo AtanasovPas encore d'évaluation
- Restoracion Del Organismo Humano 2 de 2Document56 pagesRestoracion Del Organismo Humano 2 de 2Eduardo UribePas encore d'évaluation
- FaciitisDocument17 pagesFaciitisdalaginding clophPas encore d'évaluation
- S4 Integumentary SystemDocument9 pagesS4 Integumentary Systemcam broquelPas encore d'évaluation
- Core Course - Allied Health SciencesDocument31 pagesCore Course - Allied Health SciencesMuhammad Sohail100% (1)
- Renal Function TestsDocument38 pagesRenal Function TestsSupriya NayakPas encore d'évaluation
- Cagayan Today 5-Minute News BroadcastDocument13 pagesCagayan Today 5-Minute News BroadcastNoren Dave Poli AsuncionPas encore d'évaluation
- Baby Vaccination ProgramDocument1 pageBaby Vaccination Programplainspeak100% (1)
- Diseases of Gall Bladder & Bile DuctsDocument24 pagesDiseases of Gall Bladder & Bile DuctsChampak PaulPas encore d'évaluation
- EmbryologyDocument26 pagesEmbryologyMeer BabanPas encore d'évaluation
- FACTORS AFFECTING THE PUBLIC SPEAKING FA - OdtDocument16 pagesFACTORS AFFECTING THE PUBLIC SPEAKING FA - OdtKenneth BitunPas encore d'évaluation
- 2004 2005 Magnetom Flash 2 2Document64 pages2004 2005 Magnetom Flash 2 2Herick SavionePas encore d'évaluation
- Antecedent Defined: Module 1 Section 2: HISTORICAL ANTECEDENTDocument4 pagesAntecedent Defined: Module 1 Section 2: HISTORICAL ANTECEDENTJudy CruzPas encore d'évaluation
- Haematology LastDocument65 pagesHaematology LastficocPas encore d'évaluation
- Preeclampsia and EclampsiaDocument24 pagesPreeclampsia and EclampsiaFawzia Haznah Nurul ImaniPas encore d'évaluation
- Tumour Markers PPT by DR VijayDocument31 pagesTumour Markers PPT by DR Vijaydr vijay60% (5)
- Nursing Student Documents Liver Disease CaseDocument2 pagesNursing Student Documents Liver Disease CaseQuinonez Anna MariePas encore d'évaluation
- Tissues Worksheet Class 9 Chapter 2Document3 pagesTissues Worksheet Class 9 Chapter 2My Fact worldPas encore d'évaluation
- 8 Shaped WalkDocument1 page8 Shaped WalkAmy MyzaraPas encore d'évaluation
- Correlation Does Not Imply CausationDocument9 pagesCorrelation Does Not Imply CausationeduliborioPas encore d'évaluation
- National Cancer Control Program OverviewDocument15 pagesNational Cancer Control Program OverviewAparna Kingini100% (1)
- National Mediclaim Policy: BrochureDocument3 pagesNational Mediclaim Policy: Brochureshukla8Pas encore d'évaluation
- Bangladesh Obesity AnalysisDocument16 pagesBangladesh Obesity AnalysisUnique OmarPas encore d'évaluation
- Beta - Lactam Antibiotics: Prof. R. K. Dixit Pharmacology and Therapeutics K. G. M. U. LucknowDocument29 pagesBeta - Lactam Antibiotics: Prof. R. K. Dixit Pharmacology and Therapeutics K. G. M. U. LucknowHely PatelPas encore d'évaluation
- Case Study About AlcoholismDocument6 pagesCase Study About AlcoholismElgin Renz Timbreza RociliPas encore d'évaluation
- Detect Sugars in Foods and DrinksDocument6 pagesDetect Sugars in Foods and DrinksWen LongPas encore d'évaluation
- CPE328 Lecture Notes 1Document5 pagesCPE328 Lecture Notes 1Study SmartPas encore d'évaluation