Académique Documents
Professionnel Documents
Culture Documents
2 Bab 1
Transféré par
Muhammad Rizki RamadanaCopyright
Formats disponibles
Partager ce document
Partager ou intégrer le document
Avez-vous trouvé ce document utile ?
Ce contenu est-il inapproprié ?
Signaler ce documentDroits d'auteur :
Formats disponibles
2 Bab 1
Transféré par
Muhammad Rizki RamadanaDroits d'auteur :
Formats disponibles
INTRODUCTION
Stevens-Johnson syndrome (SJS) and Toxic epidermal necrolysis (TEN) are mucocutaneous drug-induced or idiopathic reaction patterns characterized by skin tenderness and erythema o skin and mucosa! ollo"ed by extensive cutaneous and mucosal epidermal necrosis and sloughing# They are potentially li e-threatening due to multisystem involvement# $t a ecting approximately %or &'%!(((!((( annually! and are considered medical emergencies as they are potentially atal# They are characterized by mucocutaneous tenderness and typically hemorrhagic erosions! erythema and more or less severe epidermal detachment presenting as blisters and areas o denuded skin## %!& The $mmunological basis o Stevens-Johnson syndrome is )ypersensitivity Type $$$ * $+#, -enetic actors associated "ith drug hypersensitivity are a complex issue that has been studied in di erent populations and a variety o ethnic backgrounds# . uni/ue and strong association bet"een )uman 0eukocyte .ntigen ()0.)! drug hypersensitivity and ethnic background# # 1ost commonly implicated drugs are anti-convulsants! antibiotics (such as sul a! penicillin and cephalosporin) and anti-in lammatory medications# &!2 Table %# 3rugs .ssociated "ith Stevens-Johnson Syndrome and Toxic Epidermal Necrolysis Drugs Most Frequently Associated* Sul adoxine Sul adiazine Sul asalazine 4o-trimoxazole )ydantoins 4arbamazepine 7arbiturates 7enoxapro en 8henylbutazone Drugs Also Associated 4ephalosporins 5luoro/uinolones +ancomycin 6i ampin Ethambutol 5enbu en Tenoxicam Tiapro enic acid 3iclo enac
&
$soxicam 8iroxicam 4hlormezanone .llopurinol .mithiozone .minopenicillins
:
Sulindac $bupro en 9etopro en Naproxen Thiabendazole
Together these drugs account or approximately t"o-thirds o the cases attributed to
drugs in large series in 5rance! -ermany! and the ;nited States# % 8athogenesis o SJS-TEN is only partially understood# $t is vie"ed as a cytotoxic immune reaction aimed at the destruction o keratinocytes expressing oreign (drug-related) antigens# Epidermal in<ury is based on the induction o apoptosis# 3rug-speci ic activation o T cells has been sho"n in vitro on peripheral blood mononuclear cells o patients "ith drug eruptions# The nature o the antigens that drive the cytotoxic cellular immune reaction is not "ell understood# 3rugs or their metabolites act as haptens and render keratinocytes antigenic by binding to their sur aces# 4utaneous drug eruptions have been linked to a de ect o the detoxi ication systems o liver and skin! "hich results in direct toxicity or alteration o antigenic properties o keratinocytes# 4ytokines produced by activated mononuclear cells and keratinocytes probably contribute to local cell death! ever! and malaise# % Table# & 4linical 1ani estations o SJS * TEN 4linical 1ani estation 3istribution $nitial erythema on ace! extremities! becoming con luent over a e" hours or days# Epidermal sloughing may be generalized! resulting in large denuded areas# Scalp! palms! soles may be less severely involved or spared! and "idely distributed "ith prominent involvement o trunk and ace# =(> o patients have mucosal lesions! i#e#! erythema! pain ul erosions? lips! buccal mucosa! con<unctiva! genital and anal skin# @A> have con<unctival lesions? hyperemia! pseudo membrane ormationB synechiae bet"een eyelids and con<unctivaB keratitis! corneal erosions#
1ucous 1embranes Eyes
Table# , 0aboratory 5inding o SJS 0aboratory 5inding )ematology .nemia! lymphopeniaB eosino-philia uncommon# Neutropenia correlates "ith poor prognosis# Early? +acuolization'necrosis o basal keratinocytes and 3ermatopathology individual cell necrosis throughout the epidermis# 0ate? 5ull-thickness epidermal necrosis and detachment "ith ormation o subepidermal split above basement membrane# 0ittle or no in lammatory in iltrate in dermis# $mmuno luorescence studies unremarkable! ruling out other blistering disorders# Time rom irst drug exposure to onset o symptoms? % to , "eeks# Cccurs more rapidly "ith rechallenge# Cccurs a ter days o ingestion o the drugB ne"ly added drug is most suspect# 8rodromes? ever! in luenza-like symptoms % to , days prior to mucocutaneous lesions# 1ild to moderate skin tenderness! con<unctival burning or itching! then skin pain! burning sensation! tenderness! paresthesia# 1outh lesions are pain ul! tender# $mpaired alimentation! photophobia! pain ul micturition! anxiety# %!& .ll suspected cases o SJS should be con irmed by skin biopsy or histologic and immuno luorescence examinations# 0ater lesion sho"s ull-thickness epidermal necrosis and separation o epidermis rom dermis## A SJS-TEN is an acute! sel -limited disease! "ith high morbidity! that is potentially li e-threatening# Epidermal detachment may be extensive! to the entire skin sur ace# .s in severe burns! luid losses are massive! producing electrolyte imbalance# 1ucous membrane involvement (oropharynx! eyes! genitalia and anus) re/uire attentive nursing care# .ge! percentage o denuded skin! neutropenia! serum urea nitrogen level! and visceral involvement are prognostic actors# . ter healing! altered pigmentation and corneal lesions are the main long-term complications#D The diagnosis relies on the one hand on clinical symptoms and on the other hand on histological eatures# Typical clinical signs initially include areas o
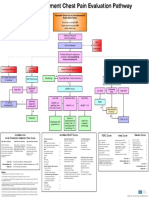
erythematous and livid macules on the skin! on "hich a positive Nikolsky sign can be induced by mechanical pressure on the skin! ollo"ed "ithin minutes to hours by the onset o epidermal detachment characterized by the development o blisters# & SJS and TEN are li e threatening conditions that need intensive care "ith experienced physicians and specialist nurses and multidisciplinary team "ork# The rame"ork o the management is depicted chart belo"# A
Vous aimerez peut-être aussi
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeD'EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeÉvaluation : 4 sur 5 étoiles4/5 (5794)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreD'EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreÉvaluation : 4 sur 5 étoiles4/5 (1090)
- Never Split the Difference: Negotiating As If Your Life Depended On ItD'EverandNever Split the Difference: Negotiating As If Your Life Depended On ItÉvaluation : 4.5 sur 5 étoiles4.5/5 (838)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceD'EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceÉvaluation : 4 sur 5 étoiles4/5 (895)
- Grit: The Power of Passion and PerseveranceD'EverandGrit: The Power of Passion and PerseveranceÉvaluation : 4 sur 5 étoiles4/5 (588)
- Shoe Dog: A Memoir by the Creator of NikeD'EverandShoe Dog: A Memoir by the Creator of NikeÉvaluation : 4.5 sur 5 étoiles4.5/5 (537)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersD'EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersÉvaluation : 4.5 sur 5 étoiles4.5/5 (345)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureD'EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureÉvaluation : 4.5 sur 5 étoiles4.5/5 (474)
- Her Body and Other Parties: StoriesD'EverandHer Body and Other Parties: StoriesÉvaluation : 4 sur 5 étoiles4/5 (821)
- The Emperor of All Maladies: A Biography of CancerD'EverandThe Emperor of All Maladies: A Biography of CancerÉvaluation : 4.5 sur 5 étoiles4.5/5 (271)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)D'EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Évaluation : 4.5 sur 5 étoiles4.5/5 (121)
- The Little Book of Hygge: Danish Secrets to Happy LivingD'EverandThe Little Book of Hygge: Danish Secrets to Happy LivingÉvaluation : 3.5 sur 5 étoiles3.5/5 (400)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyD'EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyÉvaluation : 3.5 sur 5 étoiles3.5/5 (2259)
- The Yellow House: A Memoir (2019 National Book Award Winner)D'EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Évaluation : 4 sur 5 étoiles4/5 (98)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaD'EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaÉvaluation : 4.5 sur 5 étoiles4.5/5 (266)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryD'EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryÉvaluation : 3.5 sur 5 étoiles3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnD'EverandTeam of Rivals: The Political Genius of Abraham LincolnÉvaluation : 4.5 sur 5 étoiles4.5/5 (234)
- On Fire: The (Burning) Case for a Green New DealD'EverandOn Fire: The (Burning) Case for a Green New DealÉvaluation : 4 sur 5 étoiles4/5 (74)
- The Unwinding: An Inner History of the New AmericaD'EverandThe Unwinding: An Inner History of the New AmericaÉvaluation : 4 sur 5 étoiles4/5 (45)
- Penyakit DegeneratifDocument29 pagesPenyakit DegeneratifMuhammad Rizki RamadanaPas encore d'évaluation
- Bksap Vacant 2018 eDocument65 pagesBksap Vacant 2018 eMuhammad Rizki RamadanaPas encore d'évaluation
- 3 BAB 2sDocument26 pages3 BAB 2sMuhammad Rizki RamadanaPas encore d'évaluation
- Stevens-Johnson Syndrome: Case ReportDocument1 pageStevens-Johnson Syndrome: Case ReportMuhammad Rizki RamadanaPas encore d'évaluation
- 19 01Document4 pages19 01Muhammad Rizki RamadanaPas encore d'évaluation
- Cerebral Palsy An Overview 2018Document11 pagesCerebral Palsy An Overview 2018Yhuliana AcostaPas encore d'évaluation
- Enzymes - What The Experts KnowDocument252 pagesEnzymes - What The Experts KnowRocio Uresti De Ramirez0% (1)
- Nash Leaders in TyphoidDocument25 pagesNash Leaders in TyphoidhompatPas encore d'évaluation
- Hepatitis BDocument61 pagesHepatitis BMichael AmandyPas encore d'évaluation
- Emergency Department Chest Pain Evaluation PathwayDocument2 pagesEmergency Department Chest Pain Evaluation Pathwaymuhammad sajidPas encore d'évaluation
- 21st Century DiseasesDocument8 pages21st Century DiseasesPapanaga ArinaPas encore d'évaluation
- Biliary Tract DiseaseDocument52 pagesBiliary Tract DiseaseAna Cotoman100% (1)
- Sexual HealthDocument11 pagesSexual Healthapi-236516264Pas encore d'évaluation
- Pathology MCQsDocument10 pagesPathology MCQsAnuradha Nanayakkara0% (2)
- Organic DiseasesDocument3 pagesOrganic DiseasesGlenn Cabance LelinaPas encore d'évaluation
- Modal & Phrasal VerbsDocument5 pagesModal & Phrasal VerbsPaf VenancioPas encore d'évaluation
- Algoritma CKD PDFDocument2 pagesAlgoritma CKD PDFDesla Citra100% (1)
- Typhoid FeverDocument11 pagesTyphoid FeverjhenvitoPas encore d'évaluation
- ExcerptDocument2 pagesExcerptcoloPas encore d'évaluation
- Biers BlockDocument4 pagesBiers Blockemkay1234Pas encore d'évaluation
- The Well Known Metal - Aurum Met PersonalityDocument81 pagesThe Well Known Metal - Aurum Met PersonalityDr. Deepthi BS100% (1)
- Sea RemediesDocument2 pagesSea Remedieskaravi schiniasPas encore d'évaluation
- Measles (Case Presentation)Document19 pagesMeasles (Case Presentation)Zam Pamate100% (3)
- Asthma or Copd Case StudyDocument10 pagesAsthma or Copd Case StudyMahendra ShrimaliPas encore d'évaluation
- Paragraph DevelopmentDocument7 pagesParagraph DevelopmentJacqueline Gregorio RamosPas encore d'évaluation
- Nutri Lec ReviewerDocument182 pagesNutri Lec ReviewerRaquel MonsalvePas encore d'évaluation
- Case PresentationDocument14 pagesCase PresentationFatema RavatPas encore d'évaluation
- Health FceDocument5 pagesHealth FceDoru AndreiPas encore d'évaluation
- Geriatric NursingDocument64 pagesGeriatric NursingMark Elben100% (2)
- Dengue, Chikungunya Yellow Fever: Dr. Saida SharminDocument48 pagesDengue, Chikungunya Yellow Fever: Dr. Saida SharminBishwajit BhattacharjeePas encore d'évaluation
- 02-09 2022 Pharm Pediatrics 2022 R4Document44 pages02-09 2022 Pharm Pediatrics 2022 R4Amira HelayelPas encore d'évaluation
- Awareness Knowledge and Attitude About Dengue AmonDocument5 pagesAwareness Knowledge and Attitude About Dengue AmonSachintha PasinduPas encore d'évaluation
- Neurological Disease in Lupus: Toward A Personalized Medicine ApproachDocument12 pagesNeurological Disease in Lupus: Toward A Personalized Medicine ApproachjerejerejerePas encore d'évaluation
- 4 Stool Culture PDFDocument35 pages4 Stool Culture PDFVenny PatriciaPas encore d'évaluation
- QuestionsDocument6 pagesQuestionsLorvic Andrew Juanson UmaliPas encore d'évaluation