Académique Documents
Professionnel Documents
Culture Documents
Communication Case
Transféré par
fima_njCopyright
Formats disponibles
Partager ce document
Partager ou intégrer le document
Avez-vous trouvé ce document utile ?
Ce contenu est-il inapproprié ?
Signaler ce documentDroits d'auteur :
Formats disponibles
Communication Case
Transféré par
fima_njDroits d'auteur :
Formats disponibles
Nurse Practitioners and Medical Malpractice
CA SE STUDY WITH RIS K MA NA GEMENT S TRATEGIES
Presented by NSO and CNA
edical malpractice extends to every healthcare profession including nurse practitioners. As nurse practitioners assume an expanded role in the healthcare industry, related legal issues increase. As a result, nurse practitioners are more frequently being named in medical malpractice litigation. According to CNA HealthPros and NSOs 2009 nurse practitioner claims study encompassing ten years of nurse practitioner claim data, over $64.8 million was paid for medical malpractice claims on behalf of nurse practitioners.*
Case Study: Failure to Assess Resident and Failure to Inform the Physician of Residents Unstable Condition
Mediated Settlement Payment: $450,000 Legal Expenses: $181,225 to 8:00 a.m. to the nurse practitioner. The nurse practitioner was also expected to make resident visits as needed to assess patient status and well being. On day one of the case, the nursing home physician ordered that the resident be started on Bactrim for a bladder infection. The nursing home staff correctly questioned the order, since Bactrim has the potential to adversely react with the blood thinner Coumadin but the nursing home physician continued the order. The resident also took daily doses of ibuprofen for pain which may further increase the risk of bleeding. On day two, the residents laboratory test results showed no bladder infection, however, the Bactrim was not discontinued. On day six, the residents laboratory tests showed that her bleeding time had increased and that she was at risk of bleeding from the Coumadin. Documentation is unclear whether any of the three practitioners were notified of the residents increased bleeding time. On day eight, the resident began bleeding from her gastrointestinal tract. The nurse practitioner was notified and provided orders to stop the Coumadin for two days and to recheck the residents blood tests on day eleven. It was alleged on day 10 that the nurse practitioner was notified by the nursing home staff that the resident had blood clots in her stools, but the nurse practitioner has no recollection of being told this and maintained no documentation regarding the alleged notification. The nurse practitioner stated that it was her custom and practice after each call from the nursing home, to fax her oncall report for the nursing home physician to the nursing home fax number. Since the nurse practitioner responded to resident calls outside of normal business hours, it is reasonable to assume that the nursing home physician would not receive the fax until the next time he was physically present in the nursing home. The nurse practitioner stated that she did not keep copies of the reports or her notes made during calls from the nursing home. The nursing home physician denied receiving the defendants faxed on-call reports. continued... Note: There were multiple co-defendants in this claim who are not discussed in this scenario. While there may have been errors/negligent acts on the part of other defendants, the case, comments, and recommendations are limited to the actions of the defendant; the nurse practitioner. This case involves the treatment and subsequent death of a 78-year-old female resident of a nursing home. She had a number of medical conditions including hypertension, chronic anemia, chronic renal failure, congestive heart failure and morbid obesity. She was prescribed the anti-coagulant drug Coumadin because of atrial fibrillation and the related risk of blood clot formation. The nursing home physician (who was also the president and medical director of the nursing home) contracted with a physician-owned healthcare staffing agency where the physician owner was also the agencys medical director. The nurse practitioner defendant was employed by the physicianowned healthcare staffing agency and was assigned to the nursing home to provide telephonic on-call resident care services, emergency telephone resident services and on-site resident care services as needed. All three practitioners were involved in the case involving the decedent plaintiff. For purposes of this discussion, the nursing home physician/president/medical director will be referred to as the nursing home physician. The contracted staffing agency physician-owner and medical director will be referred to and the agency physician and the nurse practitioner defendant will be referred to as the nurse practitioner. The complex arrangement for the provision of resident services at the nursing home is a significant contributing factor in the events leading to the residents death. As noted above, the nurse practitioner was employed by the contracted staffing agency to provide on-call services to the nursing home and its residents. The nursing home physician delegated the responsibility to respond to all patient care calls from the nursing home staff on week day evenings from 5:00 p.m. to 10:00 p.m., on weekends from 8:00 a.m. to 10:00 p.m. and for emergent pager calls during the week from 10:00 p.m.
The resident continued to bleed through days nine, 10 and 11. The nurse practitioner and the nursing home physician were notified of the continued bleeding but neither modified the residents care plan. The nursing staff notes reflect that the resident was dizzy and nauseated but there is no evidence that the chain of command was utilized to involve nursing leadership in obtaining treatment for the resident. The morning of day 11, the resident was found to have expired in her bed. Subsequently, an autopsy was performed by the states Medical Investigators Office with the determination that the resident bled to death from a gastrointestinal hemorrhage. The daughter of the deceased sought damages and sued the nursing home, the nursing home physician, the contracted staffing agency, the agency physician and the nurse practitioner. The allegations against the nurse practitioner included: failure to evaluate, monitor and treat the resident's severe anemia and bleeding failure to timely contact the nursing home physician about the resident's bleeding exceeding her scope of practice by making medical decisions about the residents bleeding
According to the defense teams claim consultants, the nurse practitioner made a very credible witness. The defense team engaged numerous experts to defend her including a forensic pathologist, gastroenterologist, toxicologist, hepatologist, physician and two nurse practitioners. The defense argued that the nurse practitioner was within the standard of care when responding to a telephone triage call by ordering that the Coumadin be discontinued for two days and ordering a follow-up laboratory test of the residents bleeding time. The plaintiff experts argued that the nurse practitioner should have obtained vital signs, medications, current problem list, past medical history and laboratory studies. She should further have stopped the resident's Bactrim and ibuprofen, identified her anemia and ordered STAT laboratory tests. If the nurse practitioner felt she did not have a clear understanding of the resident's condition, she should have ordered that the resident be transferred to the hospital or she should have gone to the facility to personally examine her. Plaintiffs experts indicated that it was the nurse practitioners responsibility to order and obtain the information she needed to make an appropriate assessment of the residents condition rather than to wait for information to be provided to her.
Resolution
After two and one-half years, the claim against the nurse practitioner settled at mediation for $450,000, and an additional $181,225 in legal expenses were paid. The physicians, nursing home and the staffing agency also settled the actions against them at mediation. The amount of the additional settlements is not available.
Risk Management Comments
The daily responsibility for the clinical care of this resident was fragmented among multiple practitioners. Accountability and communication channels were unclear. It appears that the nursing home physician, agency physician and the nurse practitioner all contributed directly or indirectly to the residents care at some point with no one professional acting as the primary care provider with responsibility for the oversight of the residents unstable and rapidly failing condition. The nursing staff identified the potential for adverse interaction of the residents medications but their concerns were not heeded. There is no evidence that the nursing staff persisted through the nursing chain of command regarding their concerns and the resident continued to receive the Bactrim and ibuprofen even after the Coumadin was discontinued. The role of the dispensing pharmacist in this residents medication regime is unclear as the combination of medications had obvious contraindications and should have been reported to the nursing home physician (ordering physician) and clarified before being supplied to the nursing home by the pharmacist. The nurse practitioner never actually visited the resident during the period in question. She indicated that she had faxed information regarding clinical symptoms reported by nursing staff and laboratory findings for this resident to the nursing home physician. However, the nurse practitioner retained no copies of the faxed documents and made no entries into the residents health record. The nurse practitioner performed no follow-up actions to determine if the nursing home physician timely received the faxed information in order to adjust the residents care accordingly. The nurse practitioner maintained no notes related to her conversations with nursing home staff nor did she document her clinical decision-making process in any format. The nurse practitioner failed to physically assess the resident, failed to actively seek out the results of laboratory tests and when provided with clinical evidence of abnormal bleeding times and visible gastrointestinal bleeding, failed to order the residents immediate transfer to the hospital. Without knowing the results of the claim against the additional defendants in this case, it would appear that many disciplines failed to communicate effectively and that oversight for this residents care was not properly maintained by any individual practitioner. continued...
Risk Management Recommendations
The role and scope of clinical practice of a nurse practitioner in any clinical setting (whether employed or contracted) must be clearly defined and understood among all involved parties including: resident/patient/family nurse practitioner direct resident/patient care nursing staff nursing leadership attending, consulting and contracted physicians facility medical director dispensing pharmacist and consulting pharmacist administrative leadership The contract defining the responsibilities of nurse practitioners providing on-call coverage for resident/patient care should specify under what conditions the nurse practitioner is allowed/required to visit the resident/patient rather than stating visits are as needed. Communication between the nurse practitioner and any other party regarding the residents/patients care is to be documented in a pre-defined, consistent, confidential manner and retained where it is readily available to the members of the resident/patient care team. Verbal and telephone communication must be timely documented in the resident/patient health record. Each resident/patient must have an identified attending physician who is ultimately responsible for the overall clinical decision-making in determining the residents/patients care and treatment. On-call practitioners of all types should be required to physically assess a resident/patient in need if the attending physician is not available and the residents/patients condition is unstable or deteriorating. Practitioners of all types should be prohibited from faxing information without providing original documentation in the residents/patients health record within 24 hours. Practitioners of all types should refrain from providing orders and advice regarding complex or unstable residents/patients without obtaining full information regarding the residents diagnoses, medications, response to treatment and on-going clinical monitoring results. If such information is not readily available, the unstable resident/patient should be transported to a hospital for acute and immediate care.
Guide to Sample Risk Management Plan
Risk Management is an integral part of a healthcare professionals standard business practice. Risk management activities include identifying and evaluating risks, followed by implementing the most advantageous methods of reducing or eliminating these risks - A good Risk Management Plan will help you perform these steps quickly and easily! Visit www.nso.com/riskplan to access the Risk Management plan created by NSO and CNA. We encourage you to use this as a guide to develop your own risk management plan to meet the specific needs of your healthcare practice.
*Understanding Nurse Practitioner Liability: CNA HealthPro Nurse Practitioner Claims Analysis 1998-2008, Risk Management Strategies and Highlights of the 2009 NSO Survey, CNA Insurance Company, December 2009. To read the complete study visit www.nso.com/NPclaimstudy2009 This publication is for educational purposes. It is not legal, professional or medical advice. CNA makes no representations as to its correctness or completeness and accepts no liability for any injury or damage that may arise from its use. Specific legal or medical questions should be referred to a competent attorney or medical professional before applying this material in any particular factual situations. This material may address and discuss matters for which your policy does not provide coverage, and the material does not create or imply the existence of coverage. Please consult your insurance policy for the specific terms, coverages, amounts, conditions and exclusions of coverage. All products and services may not be available in all states and may not be available in all states and may be subject to change without notice. CNA policies are underwritten by the property/casualty companies of CNA, Chicago, IL. CNA is a registered trademark of CNA Financial Corporation. 2010 Continental Casualty Company. All rights reserved. This publication is intended to inform Affinity Insurance Services, Inc., customers of potential liability in their practice. It reflects general principles only. It is not intended to offer legal advice or to establish appropriate or acceptable standards of professional conduct. Readers should consult with a lawyer if they have specific concerns. Neither Affinity Insurance Services, Inc., NSO, nor CNA assumes any liability for how this information is applied in practice or for the accuracy of this information. This publication is published by Affinity Insurance Services, Inc., with headquarters at 159 East County Line Road, Hatboro, PA 19040-1218. Phone: (215) 773-4600. All world rights reserved. Reproduction without permission is prohibited. Nurses Service Organization is a registered trade name of Affinity Insurance Services, Inc.; in CA (License #0795465), MN and OK, AIS Affinity Insurance Agency, Inc.; and in NY, AIS Affinity Insurance Agency. 2010 Affinity Insurance Services, Inc. X-8610-710
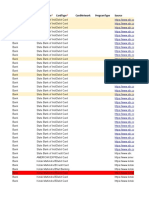
Vous aimerez peut-être aussi
- Let Her Go Lyrics ChordsDocument4 pagesLet Her Go Lyrics Chordsfima_njPas encore d'évaluation
- Epic of Gilgamesh Characters SLIDEDocument25 pagesEpic of Gilgamesh Characters SLIDEfima_nj100% (1)
- ACNEDocument1 pageACNEFimaJandzPas encore d'évaluation
- Nursing Process OUTPUTDocument5 pagesNursing Process OUTPUTfima_njPas encore d'évaluation
- The Worst Mistake You Can Make On Your ResumeDocument2 pagesThe Worst Mistake You Can Make On Your Resumefima_njPas encore d'évaluation
- Final Nursing ManagementDocument35 pagesFinal Nursing Managementfima_njPas encore d'évaluation
- NCM NotesDocument1 pageNCM Notesfima_njPas encore d'évaluation
- End Arte Rec To MyDocument3 pagesEnd Arte Rec To Myfima_njPas encore d'évaluation
- Cardiovascular, Lymphatic and Systemic DiseasesDocument69 pagesCardiovascular, Lymphatic and Systemic Diseasesfima_nj100% (1)
- Shoe Dog: A Memoir by the Creator of NikeD'EverandShoe Dog: A Memoir by the Creator of NikeÉvaluation : 4.5 sur 5 étoiles4.5/5 (537)
- Grit: The Power of Passion and PerseveranceD'EverandGrit: The Power of Passion and PerseveranceÉvaluation : 4 sur 5 étoiles4/5 (587)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceD'EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceÉvaluation : 4 sur 5 étoiles4/5 (890)
- The Yellow House: A Memoir (2019 National Book Award Winner)D'EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Évaluation : 4 sur 5 étoiles4/5 (98)
- The Little Book of Hygge: Danish Secrets to Happy LivingD'EverandThe Little Book of Hygge: Danish Secrets to Happy LivingÉvaluation : 3.5 sur 5 étoiles3.5/5 (399)
- On Fire: The (Burning) Case for a Green New DealD'EverandOn Fire: The (Burning) Case for a Green New DealÉvaluation : 4 sur 5 étoiles4/5 (73)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeD'EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeÉvaluation : 4 sur 5 étoiles4/5 (5794)
- Never Split the Difference: Negotiating As If Your Life Depended On ItD'EverandNever Split the Difference: Negotiating As If Your Life Depended On ItÉvaluation : 4.5 sur 5 étoiles4.5/5 (838)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureD'EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureÉvaluation : 4.5 sur 5 étoiles4.5/5 (474)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryD'EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryÉvaluation : 3.5 sur 5 étoiles3.5/5 (231)
- The Emperor of All Maladies: A Biography of CancerD'EverandThe Emperor of All Maladies: A Biography of CancerÉvaluation : 4.5 sur 5 étoiles4.5/5 (271)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreD'EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreÉvaluation : 4 sur 5 étoiles4/5 (1090)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyD'EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyÉvaluation : 3.5 sur 5 étoiles3.5/5 (2219)
- Team of Rivals: The Political Genius of Abraham LincolnD'EverandTeam of Rivals: The Political Genius of Abraham LincolnÉvaluation : 4.5 sur 5 étoiles4.5/5 (234)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersD'EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersÉvaluation : 4.5 sur 5 étoiles4.5/5 (344)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaD'EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaÉvaluation : 4.5 sur 5 étoiles4.5/5 (265)
- The Unwinding: An Inner History of the New AmericaD'EverandThe Unwinding: An Inner History of the New AmericaÉvaluation : 4 sur 5 étoiles4/5 (45)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)D'EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Évaluation : 4.5 sur 5 étoiles4.5/5 (119)
- Her Body and Other Parties: StoriesD'EverandHer Body and Other Parties: StoriesÉvaluation : 4 sur 5 étoiles4/5 (821)
- Service Operations V3.0AugmentedDocument882 pagesService Operations V3.0Augmentedrockmen2001Pas encore d'évaluation
- Kotak MahindraDocument43 pagesKotak MahindraUZARA KHANPas encore d'évaluation
- Accounting Equation Explained - Assets, Liabilities & Owner's EquityDocument43 pagesAccounting Equation Explained - Assets, Liabilities & Owner's Equitythella deva prasadPas encore d'évaluation
- Key Fact StatementDocument2 pagesKey Fact StatementBNREDDY PSPas encore d'évaluation
- Citf Chapter 3-Ts StudentDocument14 pagesCitf Chapter 3-Ts StudentAlin RaissaPas encore d'évaluation
- Nentr 6043Document4 pagesNentr 6043wadagrosPas encore d'évaluation
- JKTD47312900 Innsa 5F One R1Document2 pagesJKTD47312900 Innsa 5F One R1Riko ApriliantoPas encore d'évaluation
- AFAR 2305 Not-for-Profit OrganizationsDocument14 pagesAFAR 2305 Not-for-Profit OrganizationsDzulija TalipanPas encore d'évaluation
- Date/Time Patient PT Status Age Sex DOB LocationDocument56 pagesDate/Time Patient PT Status Age Sex DOB Locationzeerak khanPas encore d'évaluation
- 15 KRM Om10 Tif ch12Document35 pages15 KRM Om10 Tif ch12Dingyuan OngPas encore d'évaluation
- Hca-600-Week 4 Assignment - Health Care Policy IssuesDocument5 pagesHca-600-Week 4 Assignment - Health Care Policy Issuesapi-290742611Pas encore d'évaluation
- Car Insurance AssignmentDocument19 pagesCar Insurance AssignmentSidPas encore d'évaluation
- Ticket - Abibus PDFDocument2 pagesTicket - Abibus PDFTapan Chandratre60% (5)
- DR L. Ravindran, CFP, Ph. D, Founder Managing Director & CEO, Wealthmax Enterprises Management P LTD, BangaloreDocument14 pagesDR L. Ravindran, CFP, Ph. D, Founder Managing Director & CEO, Wealthmax Enterprises Management P LTD, Bangalorekeyur1975Pas encore d'évaluation
- Lecture Overview. UMTS Concept UTRA FDD TDDDocument39 pagesLecture Overview. UMTS Concept UTRA FDD TDDanhttp.nevigroupPas encore d'évaluation
- Luxus Hypermarket Service BlueprintDocument2 pagesLuxus Hypermarket Service BlueprintJITHA JOHNNY 22Pas encore d'évaluation
- Traffic Report from DPS to Europe 2016Document553 pagesTraffic Report from DPS to Europe 2016Ari cPas encore d'évaluation
- ISO/IEC 27001 Lead Implementer Training InvoiceDocument2 pagesISO/IEC 27001 Lead Implementer Training InvoiceWahid MATAPas encore d'évaluation
- ACCA F2 Sample Study NoteDocument21 pagesACCA F2 Sample Study Notebillyryan10% (1)
- BroadbandDocument8 pagesBroadbandmanish kumarPas encore d'évaluation
- Label - 1663795065759 - 1 2Document1 pageLabel - 1663795065759 - 1 2Tazkhan123Pas encore d'évaluation
- Module 1 NotesDocument36 pagesModule 1 NotesKunwar Partap SinghPas encore d'évaluation
- The Impact of Rising Car UseDocument2 pagesThe Impact of Rising Car UseIrene SanduPas encore d'évaluation
- Organizational Communication Group 18Document46 pagesOrganizational Communication Group 18pankajbhatt1993Pas encore d'évaluation
- Group học tập: Facebook:: Website: Giáo ViênDocument2 pagesGroup học tập: Facebook:: Website: Giáo Viênanh nguyen thi lanPas encore d'évaluation
- Amex Credit Card FeatureDocument5 pagesAmex Credit Card FeatureLight House School of Learning and DiversityPas encore d'évaluation
- Cisco UC5XX Default Conf 111Document12 pagesCisco UC5XX Default Conf 111LA-ZOUBE GAELPas encore d'évaluation
- HS 2019 Furniture GRDocument250 pagesHS 2019 Furniture GRKristina PeteuPas encore d'évaluation
- Heritage ISIDocument1 pageHeritage ISISebastian AguileraPas encore d'évaluation
- Audit Summary Cash Receipt and Sales Receipt FlowchartDocument8 pagesAudit Summary Cash Receipt and Sales Receipt Flowchartandi TenriPas encore d'évaluation