Académique Documents
Professionnel Documents
Culture Documents
C 0412010011
Transféré par
IOSR Journal of PharmacyTitre original
Copyright
Formats disponibles
Partager ce document
Partager ou intégrer le document
Avez-vous trouvé ce document utile ?
Ce contenu est-il inapproprié ?
Signaler ce documentDroits d'auteur :
Formats disponibles
C 0412010011
Transféré par
IOSR Journal of PharmacyDroits d'auteur :
Formats disponibles
IOSR Journal of Pharmacy (e)-ISSN: 2250-3013, (p)-ISSN: 2319-4219 www.iosrphr.
org Volume 4, Issue 1 (January 2014), Pp 10-11
Endoscopic removal of large Brunners gland adenoma
1,
S.J.Yaseen M.D, F.I.C.M.S, 2, F.I.C.M.S G&H, 3, A.A.Mitib C.A.B.M, 4, H.N.Mussa
Hussein Teaching Hospital, Department of Gastroenterology and Hepatology, Thi-Qar, Iraq. Dr.alaa jamel hasin general surgeon C.A.BS. MRCSI medical college, The-Qar University
1, 2, 3, 4,
Abstract: Brunners gland adenoma (also referred to as Brunners gland hamartoma or Brunerroma) is a rare
benign tumor of the duodenum. We report a 58-year-old man presenting with recurrent upper abdominal pain of variable intensity with occasional vomiting for three years. Duodenoscopy revealed a large pedunculated polyp with along stalk arising from the posterior wall of the duodenal bulb and extending into the second part of the duodenum. Endoscopic polypectomy was performed. Histological examination revealed a Brunners gland adenoma (hamartoma).
I.
INTRODUCTION:
Brunners glands were first described by the anatomist Brunner in 1688 and he thought that they are pancreas secondarium till Middeldorf (1684) correctly identified them as submucosal glands separate from duodenal glands, but structurally and functionally similar to glands of pylorus. (1) Brunners glands are mucussecreting acinotubular glands located in the deep mucosa and the sub mucosa of the duodenum, emptying into the crypts of Lieberkuhn. (2)A primary function of these glands is to secret alkaline mucus into the intestinal lumen in addition to other activities such as the secretion of insulin like growth factor and the lysozyme muramidase. There is also a possibility that these glands assist the function of intestinal crypts in transporting immunoglobulins into the gut lumen. In addition, they may contribute to the innate immunity in the intestinal tract. (3) The first to report a Brunners gland adenoma was Cruveilhier in 1835, describing a Brunners adenoma causing intussusceptions with patients death. (1, 4) We present a 58-year-old man with dyspeptic symptoms for three years. Endoscopy revealed a large pedunculated polyp in the duodenum, which was endoscopically resected and proven to be a Brunners gland adenoma on histology. The literature on Brunners gland adenoma (hamartoma) was reviewed. Case Report:
A 58-year-old man has upper abdominal pain and occasional bouts of vomiting for three years. He used to use over the counter medications and self prescriptions for his symptoms then he made medical consultation when his symptoms had intensified for the last one month. He reported no weight loss and his medical history is unremarkable apart from hypertension for five years controlled by tenormen 100 mg single dose daily. Physical examination revealed no abnormality. Complete blood count, blood sugar, liver enzymes and blood urea nitrogen all came normal. Abdominal ultrasound examination done to him and was reported as normal too. OGD disclosed a large duodenal polyp with smooth surface and a long stalk arising from the duodenal bulb and extending into the second part. A duodenoscope then used and a polypectomy was performed using coagulation current. The polyp was 3x2x1cm in size with lobulated surface. Histopathology reported a Brunners gland adenoma (hamartoma). Follow up endoscopy six months and two years later show no recurrence of the lesion and the patient was free of symptoms.
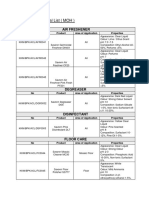
Fig. 1 and 2. Endoscopic view of big pedunculated Brunneroma arising from the duodenal bulb and falling into the second part.
10
Endoscopic removal of large Brunners gland adenoma
Fig. 3. Photomicrograph of Brunners gland hyperplasia shows proliferation of Brunners glands. (H and E, 10)
II.
DISCUSSION:
Benign tumors of the duodenum are rare. They are reported in 0.008% of the patients at autopsy; Brunner gland adenoma comprises 10.6% of these lesions. (4, 5) Brunners glands are mucin-secreting glands situated in the deep mucosa and the submucosa of the duodenum. (6) They extend from the pylorus distally to a variable distance usually up to the D2 segment, although in rare occasions it may reach up to the proximal jejunum, even the distal ileum, but they are most numerous in the proximal part of the duodenum immediately distal to the pylorus and diminished in size and number as they go distally. In infants they occupy 55% of the total duodenal area; by 50 years of age this drops to 35 %.( 7) Brunners gland adenomas have been reported in the proximal jejunum and in the proximal ileum. (4)
REFERENCES:
1. 2. 3. 4. 5. 6. 7. Chattopadhyay P, Kundu A K, Bhattacharyya S, et al.Diffuse nodular hyperplasia of Brunners gland present ing as upper gastrointestinal haemorrhage. Singapore Med J 2008; 49 (1) : 81. Janes SEJ, Zaitoun AM1, Catton JA, et al. Brunners gland hyperplasia at the ampulla of Vater.J Postgrad Med March 2006 Vol 52 Issue 1. Helio B. coutinho', Tania I. robalinho', Vera B. coutinho', et al. Immunocytochemical demonstration that human duodenal Brunner's glands may participate in intestinal defence. J. Anat. (1996) 189, pp. 193-197. J.M. Jansen, W.N.H.M. Stuifbergen, A.W.M. van Milligen de Wit. Endoscopic resection of a large Brunners gland adenoma. The Netherlands journal of medicine. JULY 2002, VOL. 60, NO. 6 253. Kovacevic I, Ljubicic N, Cupic H, et al. Helicobacter pylori infection in patients with Brunner's gland adenoma. Acta Med Croatica 2001; 55:157-60. Henken EM, Forouhar F. Hamartoma of Brunners gland causing partial obstruction of the ileum. J Can Assoc Radiol 1983; 34:73-4. Fuller JW, Maj MC Cruse CW, Williams JW. Hyperplasia of Brunner's glands of the duodenum. Am Surg 1997; 43:246-50.
11
Vous aimerez peut-être aussi
- Sulphasalazine Induced Toxic Epidermal Necrolysis A Case ReportDocument3 pagesSulphasalazine Induced Toxic Epidermal Necrolysis A Case ReportIOSR Journal of PharmacyPas encore d'évaluation
- A Case of Allergy and Food Sensitivity: The Nasunin, Natural Color of EggplantDocument5 pagesA Case of Allergy and Food Sensitivity: The Nasunin, Natural Color of EggplantIOSR Journal of PharmacyPas encore d'évaluation
- A Review On Step-by-Step Analytical Method ValidationDocument13 pagesA Review On Step-by-Step Analytical Method ValidationIOSR Journal of Pharmacy100% (1)
- A Review On Step-by-Step Analytical Method ValidationDocument13 pagesA Review On Step-by-Step Analytical Method ValidationIOSR Journal of Pharmacy100% (1)
- Treatment of Uthiravatha Suronitham (Rheumatoid Arthritis) With A Siddha Compound Formulation - A Case Study.Document3 pagesTreatment of Uthiravatha Suronitham (Rheumatoid Arthritis) With A Siddha Compound Formulation - A Case Study.IOSR Journal of Pharmacy100% (1)
- Phytochemical Screening and Antioxidant Activity of Clove Mistletoe Leaf Extracts (Dendrophthoe Pentandra (L.) Miq)Document6 pagesPhytochemical Screening and Antioxidant Activity of Clove Mistletoe Leaf Extracts (Dendrophthoe Pentandra (L.) Miq)IOSR Journal of PharmacyPas encore d'évaluation
- Shoe Dog: A Memoir by the Creator of NikeD'EverandShoe Dog: A Memoir by the Creator of NikeÉvaluation : 4.5 sur 5 étoiles4.5/5 (537)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeD'EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeÉvaluation : 4 sur 5 étoiles4/5 (5794)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceD'EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceÉvaluation : 4 sur 5 étoiles4/5 (895)
- The Yellow House: A Memoir (2019 National Book Award Winner)D'EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Évaluation : 4 sur 5 étoiles4/5 (98)
- Grit: The Power of Passion and PerseveranceD'EverandGrit: The Power of Passion and PerseveranceÉvaluation : 4 sur 5 étoiles4/5 (588)
- The Little Book of Hygge: Danish Secrets to Happy LivingD'EverandThe Little Book of Hygge: Danish Secrets to Happy LivingÉvaluation : 3.5 sur 5 étoiles3.5/5 (400)
- The Emperor of All Maladies: A Biography of CancerD'EverandThe Emperor of All Maladies: A Biography of CancerÉvaluation : 4.5 sur 5 étoiles4.5/5 (271)
- Never Split the Difference: Negotiating As If Your Life Depended On ItD'EverandNever Split the Difference: Negotiating As If Your Life Depended On ItÉvaluation : 4.5 sur 5 étoiles4.5/5 (838)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyD'EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyÉvaluation : 3.5 sur 5 étoiles3.5/5 (2259)
- On Fire: The (Burning) Case for a Green New DealD'EverandOn Fire: The (Burning) Case for a Green New DealÉvaluation : 4 sur 5 étoiles4/5 (74)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureD'EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureÉvaluation : 4.5 sur 5 étoiles4.5/5 (474)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryD'EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryÉvaluation : 3.5 sur 5 étoiles3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnD'EverandTeam of Rivals: The Political Genius of Abraham LincolnÉvaluation : 4.5 sur 5 étoiles4.5/5 (234)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaD'EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaÉvaluation : 4.5 sur 5 étoiles4.5/5 (266)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersD'EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersÉvaluation : 4.5 sur 5 étoiles4.5/5 (345)
- The Unwinding: An Inner History of the New AmericaD'EverandThe Unwinding: An Inner History of the New AmericaÉvaluation : 4 sur 5 étoiles4/5 (45)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreD'EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreÉvaluation : 4 sur 5 étoiles4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)D'EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Évaluation : 4.5 sur 5 étoiles4.5/5 (121)
- Her Body and Other Parties: StoriesD'EverandHer Body and Other Parties: StoriesÉvaluation : 4 sur 5 étoiles4/5 (821)
- Insomnii, Hipersomnii, ParasomniiDocument26 pagesInsomnii, Hipersomnii, ParasomniiSorina TatuPas encore d'évaluation
- Sodium Borate: What Is Boron?Document2 pagesSodium Borate: What Is Boron?Gary WhitePas encore d'évaluation
- Uptime Elements Passport: GineerDocument148 pagesUptime Elements Passport: GineerBrian Careel94% (16)
- Playwriting Pedagogy and The Myth of IntrinsicDocument17 pagesPlaywriting Pedagogy and The Myth of IntrinsicCaetano BarsoteliPas encore d'évaluation
- Approved Chemical ListDocument2 pagesApproved Chemical ListSyed Mansur Alyahya100% (1)
- 1E Star Trek Customizable Card Game - 6 First Contact Rule SupplementDocument11 pages1E Star Trek Customizable Card Game - 6 First Contact Rule Supplementmrtibbles100% (1)
- Snapshot Traveller January 2022Document11 pagesSnapshot Traveller January 2022api-320548675Pas encore d'évaluation
- Introduction To Instrumented IndentationDocument7 pagesIntroduction To Instrumented Indentationopvsj42Pas encore d'évaluation
- Exercise No.2Document4 pagesExercise No.2Jeane Mae BooPas encore d'évaluation
- AdverbsDocument10 pagesAdverbsKarina Ponce RiosPas encore d'évaluation
- A Terrifying ExperienceDocument1 pageA Terrifying ExperienceHamshavathini YohoratnamPas encore d'évaluation
- Old San Agustin NHS MSISAR Sept 2021Document2 pagesOld San Agustin NHS MSISAR Sept 2021ERICSON SABANGANPas encore d'évaluation
- Complete PDFDocument495 pagesComplete PDFMárcio MoscosoPas encore d'évaluation
- Exercise 1-3Document9 pagesExercise 1-3Patricia MedinaPas encore d'évaluation
- GearsDocument14 pagesGearsZulhilmi Chik TakPas encore d'évaluation
- Problem ManagementDocument33 pagesProblem Managementdhirajsatyam98982285Pas encore d'évaluation
- Writing - Hidden Curriculum v2 EditedDocument6 pagesWriting - Hidden Curriculum v2 EditedwhighfilPas encore d'évaluation
- Time Interest Earned RatioDocument40 pagesTime Interest Earned RatioFarihaFardeenPas encore d'évaluation
- ESU Mauritius Newsletter Dec 2014Document8 pagesESU Mauritius Newsletter Dec 2014Ashesh RamjeeawonPas encore d'évaluation
- Paediatrica Indonesiana: Sumadiono, Cahya Dewi Satria, Nurul Mardhiah, Grace Iva SusantiDocument6 pagesPaediatrica Indonesiana: Sumadiono, Cahya Dewi Satria, Nurul Mardhiah, Grace Iva SusantiharnizaPas encore d'évaluation
- Influencing Factors Behind The Criminal Attitude: A Study of Central Jail PeshawarDocument13 pagesInfluencing Factors Behind The Criminal Attitude: A Study of Central Jail PeshawarAmir Hamza KhanPas encore d'évaluation
- My ResumeDocument2 pagesMy ResumeWan NaqimPas encore d'évaluation
- Validator in JSFDocument5 pagesValidator in JSFvinh_kakaPas encore d'évaluation
- "What Is A Concept Map?" by (Novak & Cañas, 2008)Document4 pages"What Is A Concept Map?" by (Novak & Cañas, 2008)WaniePas encore d'évaluation
- FMEA 4th BOOK PDFDocument151 pagesFMEA 4th BOOK PDFLuis Cárdenas100% (2)
- Essay EnglishDocument4 pagesEssay Englishkiera.kassellPas encore d'évaluation
- Tamil and BrahminsDocument95 pagesTamil and BrahminsRavi Vararo100% (1)
- Forever Living Presentation PDFDocument34 pagesForever Living Presentation PDFCasey Rion100% (1)
- Hilti Product Technical GuideDocument16 pagesHilti Product Technical Guidegabox707Pas encore d'évaluation
- Book of Dynamic Assessment in Practice PDFDocument421 pagesBook of Dynamic Assessment in Practice PDFkamalazizi100% (1)