Académique Documents
Professionnel Documents
Culture Documents
Johnsson Tossec Formula
Transféré par
Joshua Pattinson LegiCopyright
Formats disponibles
Partager ce document
Partager ou intégrer le document
Avez-vous trouvé ce document utile ?
Ce contenu est-il inapproprié ?
Signaler ce documentDroits d'auteur :
Formats disponibles
Johnsson Tossec Formula
Transféré par
Joshua Pattinson LegiDroits d'auteur :
Formats disponibles
AU J.T. 8(1): 15-20 (Jul.
2004)
A Study in Johnsons Formula: Fundal Height Measurement for Estimation of Birth Weight
Watchree Numprasert
Faculty of Nursing Science, Assumption University Bangkok, Thailand
Abstract
The purpose of this study was to determine the degree of positive estimation value of birth weights in Thai pregnancies by using Johnsons formula. There were 400 respondents who were attendants in the delivery room at Bhumibol Adulyadej Hospital between April and October 2002. The data for this study were obtained by interviews, fundal heights, and station level and baby weight measurements by midwives in the delivery room. The results of this study shown the majority of the respondents ages were between 21 to 30 years. The body mass index (BMI) of the sample showed nearly half had a BMI less than 19.8, and 55.5% had a BMI from 19.8 to 26.0. The estimating baby weight by using Johnsons formula had a higher percentage in positive estimation value than negative estimation value. The difference between the estimated weight using Johnsons formula was an average of 227 g higher than the actual baby weight. The standard error of weight difference between the estimated weight and actual weight was 9.01, with 95% confident interval of 209.51 to 244.83. The best cut-off level of an acceptable error was 310 g. It was concluded that there were 72% of the estimated weight predictions within the average 10% of the actual birth weight, while the estimated weight using Johnsons formula had a tendency towards an over estimation of baby weight in all groups of babies. Keywords: Fetal weight, positive estimation value, negative estimation value, body mass index, estimated weight, actual weight.
Introduction
The complexity of clinical intrapartum practice requires students to learn how to deliver nursing care to pregnant women based on theoretical knowledge and skills relevant to clinical practice situations. In planning and managing care for childbearing families, students frequently have a difficult task in integrating clinical situations and theoretical knowledge, although, there are several guidelines to assist students in their learning such as: McDonalds rule, Leopolds method, the Friedman Curve, and so on. In a predictable labor phase, a deliberate plan for contingencies for clinical experiences when the students have experiential learning, as traditionally, the proceeding three Ps: passage (pelvis),
15
passenger (fetus), and powers (contractions) were considered to be the major factors determining the outcome of labor and delivery. One essential element in which the student faces with the difficult of midwifery training is the estimation of fetal weight in P passenger (fetus). Because a clinical estimation of fetal size may be inaccurate, the diagnosis of macrosomia is often made until after fruitless attempts at delivery (Cunningham, et al. 1993). Nevertheless, competent clinical examinations should enable experienced examiners to arrive at fairly accurate estimates (in the absence of maternal obesity). Also ultrasounds can identify a group of fetuses with significantly increased risks of macrosomia (Cunningham, et al. 1993; Dickason and Schult 1998).
AU J.T. 8(1): 15-20 (Jul. 2004)
However, accurate identification of fetal size is an imperfect clinical skill. For example, Hirate, et al. (1990; cited in Cunningham, et al.; 1993) identified 141 fetuses estimated to weight nearly 4,000 g using Leopolds examinations, and then performed ultrasound examinations to test the accuracy of several reported sonar methods. The actual birth weights were ranged from 2,920 to 5,100 g and 22% of the fetuses weighed less than 4,000 g. They found that the best sonographic estimates of fetal macrosomia were obtained using abdominal circumference and femur length measurements, also ultrasound derived predictions of fetal macrosomia are prone to large inaccuracies. Unfortunately, the suspected macrosomic fetus and the very small or pre-viable fetus that ultrasonic fetal weight estimates are most inaccurate and difficult to obtain (OGrady and Gimovsky 1995). Fetal weight is indeed a very important factor based upon decision, must be made with concerns to labor and delivery. Assuming that in large fetuses, dystocia may arise because the head is not only larger, but also harder and less moldable with increasing weight. Cesarean delivery may be necessary if the fetus is too large to travel through the pelvis (fetopelvic disproportion) in an attempt to avoid birth trauma. A large fetus whose size is underestimated may experience trauma to the head as a result of strong contractions, which force the head against the bony structures of the pelvis. Cerebral edema, neurological damage, hypoxia and asphyxia may result. Moreover, shoulder dystocia and fractures of the clavicles and humerus are more common with large infants (Sherwen, et al. 1993). With small fetuses, fetal demise, birth asphyxia, meconium aspiration, and neonatal hypoglycemia and hypothermia are all increased because the fetal organs are not only becomes smaller in size, but also submature in function (Piper, et al. 1996). Therefore, these infants require special care from the health care team. However, extremely overweight infants have a relatively increased prenatal mortality rate. Perinatal mortality doubled from about 3.5 per 1,000 for
16
those overweight infants. Fundal height measurement can be used to estimate fetal weight using Johnsons formula. Johnsons formula requires the height of the fundus in cm, and station level to complete the calculation. Johnsons formula is a formula for the estimation of fetal weight in vertex presentations. The formula is as follows: Fetal weight (g) = [fundal height (cm) n] x 155 n = 12, if vertex is above the ischial spines n = 11, if vertex is below ischial spines. Considerable demographic variation, in our opinion, has less complexity than anticipated, based on skillful of abdominal exam or ultrasonography interpretations. Johnsons formula for estimation of fetal weight has been found to be accurate within 375 g in 75% of infants (Sherwen, et al. 1993). These results were collected using Whites pregnancies. Thailand has a smaller demographic ethnicity, so perhaps estimations of Thai fetal weight may not be accurate within normal limits. Therefore, Johnsons formula is required in applying estimations of fetal weight in Thai pregnancies. Given the importance of these expectations, one advantage enfolded into the curriculum of clinical intrapartum practice with the quality of educational problems and resulting outcomes scrutinized. Purpose of This Study The purposes of this study are to: (i) determine the degree of positive estimation value of Johnsons formula for the estimation of fetal weight in Thai pregnancies who were attended in the delivery room at Bhumibol Adulyadej Hospital. (ii) determine the degree of negative estimation value of Johnsons formula for the estimation of fetal weight in Thai pregnancies that were attended in the delivery room at Bhumibol Adulyadej Hospital. (iii) determine the degree of error for Thai fetal weight in grams, using Johnsons formula.
AU J.T. 8(1): 15-20 (Jul. 2004)
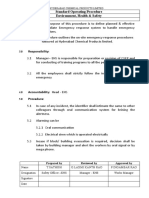
Research Methodology
Population Samples The samples used in this study were 400 Thai pregnancies, which met the eligibility criteria and were attended in the delivery room at Bhumibol Adulyadej Hospital between April and October 2002. Inclusion Criteria The following criteria were employed to include the samples: 1. Pregnancy, a singleton fetus 2. Presentation, preferably vertex 3. Station should not be located at 0 levels (level of the ischial spines) 4. Maternal height and pregnancy weight within 26.0 (BMI < 26.0) Exclusion Criteria The following criteria were employed to exclude the samples: 1. Pregnancy, complicated chronic disease. 2. Pregnancy, diagnosed oligohydramnios or polyhydramnios. 3. Death, fetus in uterine or abortion. 4. Pregnancy, uterine and/or abdominal mass. Instrumentation The survey instrument used for this study consisted of six components, subdivided into three parts namely: (i) demography, (ii) obstetrical history, abdominal examination, pelvic examination, and (iii) newborn record and fetal weight calculation by Johnsons formula which it was conceptualized by the researcher. The six components were developed from the concepts of labor assessment, AU Faculty of Nursing Science. The content validity for this instrument was further strengthened by three university professors, two administrative nurses and one executive obstetrician specializing in this area. Their opinions and suggestions were included for the improvement, clarity and utility of this instrument.
17
Research Procedure Data for this study were obtained in three ways: 1. Through the completion of survey instruments via interviews. 2. Through fundal height and station level examines by midwives. 2.1 Fundal height measurement: The bladder should be empty, then the fundal height is measured in cm using a tape measure. Placing the tip on the upper border of the maternal symphysis pubis, over the midline of the abdomen, to the top of the uterine fundus is an accurate method of measuring. 2.2 Station identification: A five level method is used for designating the station. When conducting a vaginal examination, the lowermost portion of the presenting fetal part is at the level of ischial spines. It is designated as being at zero (0) station. Levels above the spines are designated in centimeters by negative values, -1, -2, -3 stations. Levels below the spines are designated by positive value, +1, +2, +3 stations, down to the pelvic floor. 3. Through fetal outcome (weight) measurement: Weight is performed in the delivery room. The baby is placed unclothed in the center of a properly balanced scale. The weight is then recorded in grams.
Statistical Analyses
Part I To determine the personal data, frequencies, percentages and means (where appropriate) were computed. Part II and III Percentages, means and standard deviations were first computed. Then, positive estimation value, negative estimation value and degree of error were administered for Johnsons formula in calculation of Thai (baby) fetal weight.
AU J.T. 8(1): 15-20 (Jul. 2004)
Results
The results of this study were divided into three parts: (i) demography (ii) obstetric details, and (iii) differences between estimated weight and baby weight. Demography The majority of the respondents ages were in the range of 21 to 30 years old (55.25 %). One hundred and thirty-nine respondents had completed Grade 9 education. Many of the women were employees, nearly 60% earned incomes less than Baht 10,000 per month. The body mass index of the sample, nearly half had body mass index less than 19.8 and half had body mass index between 19.8-26.0. Obstetric Details There were 85.75% (n = 235) primigravida and 41.25% (n = 165) multigravida in the sample, with gestation age ranged from 34 to 42 weeks (mean = 39.14, SD = 1.668). The total pregnancy weight gain varied from 4 to 34
kg. (mean = 14.39, SD = 5.351). The height of fundus ranged from 27 to 44 cm (mean = 33.22, SD = 2.39), more than 85% had station minus (above ishial spines) and around 14% had station plus (below ishial spines). The Difference Between Estimated Weight and Baby Weight Of the 400 babies delivered, 209 were male (52.25%) and 191 female (42.75%), actual baby weight ranged from 1,900 g to 5,300 g (mean = 3,175.57; SD = 414.67). The estimated weight values obtained ranged from 2,325 g to 4,960 g, with a mean of 3,318.16 + 351.72 g. The difference between the estimated weight and actual baby weight ranged from -750 to +530 g, with a mean of 227.17 + 180.38 g (Table 1). The standard error was 9.010 g., with a 95% confidence interval (CI) of 209.51 to 244.83 g (Table 2). Positive estimation values of baby weight at critical cut-off points of 200 and 310 g, and 10% of actual baby weight, were 241 (60.25%), 287 (71.75%), and 286 (71.5%) of 400 cases, respectively (Table 3).
Table 1. Range, mean and standard deviation by height of fundus, baby weight (BW), estimated weight (EW), and difference between EW and BW Criteria Height of fundus (cm) Baby weight (g) Estimated weight (g) Difference between EW and BW (g) Range 27 44 1900 5300 2325 4960 (-750) 530 Mean 33.22 3175.57 3318.16 227.17 SD. 2.39 414.67 351.72 180.38
Table 2. Range, mean, standard deviation, standard error, confidence intervals (CI) and P value by estimation error Estimation error (g) (-750) 530 n 400 mean 227.71 SD 180.38 SE 9.01 95% confidence interval 209.51 to 244.83
Table 3. Frequency and percentage by positive estimation value (PEV) and negative estimation value (NEV) at the level of acceptable error Level of acceptable error (g) < 200 < 310 < 10% of birth weight Positive estimation value Number Percent 241 60.25 287 71.75 286 71.50
18
Negative estimation value Number Percent 159 39.75 113 28.25 114 28.5
AU J.T. 8(1): 15-20 (Jul. 2004)
From Table 4, positive estimation values of baby weight at critical cut-off points of 200 and 310 g, and 10% of actual baby weight by baby weight category of: (i) less than 2,500 g, were only 2 (15.38%), 3 (23.08%), and 2
(15.38%); (ii) 2,500-4,000 g were 232 (61.87%), 276 (73.02%), and 275 (72.75%); and (iii) greater than 4000 g were 6 (66.67%), 8 (88.89%), and 9(100%), respectively.
Table 4. Frequency and percentage by positive estimation value (PEV) and negative estimation value (NEV) in baby weight classification. Baby weight Acceptable of 200 g classification PEV NEV (g) n % n % < 2,500 2 15.38 11 84.62 2,500-4,000 232 61.87 145 38.67 > 4,000 6 66.67 3 33.33 Acceptable error of 10% birth weight PEV NEV PEV NEV n % n % n % n % 3 23.08 10 76.92 2 15.38 11 84.62 276 73.02 102 26.92 275 72.75 103 25.75 8 88.89 1 11.11 9 100 0 0 Acceptable of 310 g
Discussion
Estimation of fetal weight by symphysis fundal height (SFH) measurement has been reported by various authors including Edwards (2001), Bothner et al. (2000), Mongelli and Gardosi (1999), Promvijit et al. (2000) conducted a study to determine the measurement of fundal heights in labor as a means of estimating birth weight in singleton pregnancies. As a diagnostic test they reported fundal height useful on an individual basis and recommended that individual biometry or sonographic measurement more useful in assessing the growth of an at risk fetus. Probably a combination of SFH and biometry is an appropriate compromise of estimation of fetal weight. According to a recent study of 400 singleton pregnancies, results shown that estimating baby weight by Johnsons formula had a higher percentage of positive estimation value than negative estimation value. The best cut-off level of acceptable error was 310 g. Consequently, the statistical average baby weight should be concerned with determining baby weight at birth. The average estimated weight by using Johnsons formula was 227.17 g higher than the actual baby weight, whereas at 95% confidence interval was between 209.51 to 244.83 g. Similarly, Mhaskar, et al.
19
(2002) found the estimated weight by using Johnsons formula of an average 310 g higher than the actual weight. There were serious problems with calculating and reporting an estimated fetal weight. The main problems related to the calculation of estimated fetal weight using Johnsons formula was not sufficiently accurate in small gestation age babies (weight less than 2,500 g). Also, the results indicated that estimated fetal weight using Johnsons formula had a tendency toward over estimation of baby weight in all groups of babies, particularly in low birth weight cases. Therefore, sonographic estimation is essential to enhance accuracy. Low birth weight for gestation is a main cause of perinatal morbidity and mortality especially in developing countries. Thus, close monitoring during labor should be done for estimated low birth weight fetuses. Overall, 72% of the estimated weight predictions were within an average and 10% of the actual birth weight. In support of the idea of symphysis fundal height (SFH) measurement to determine baby weight, this researcher believes that SFH has adequate precision and accuracy for preparturition estimation of baby weight. The present study reveals that estimating fetal height intrapartally is crucial to enable the nurse-midwife and/or nursing student to:
AU J.T. 8(1): 15-20 (Jul. 2004)
(i) create a decision regarding the mode of delivery, (ii) anticipate problem during labor and hence close monitoring of labor could be obtained particularly for small gestation infants, (iii) anticipate possible shoulder dystocia and hence notify for availability of a senior competent nurse-midwife and/or obstetrician at the time of delivery, and (iv) predict individual birth weights and/or special resources requirement except a tailor measuring tape that its advantages are spread, economy and general applicability.
References
Bothner, B.K.; Gulmezoglu, A.M.; and Hofmeyr, G.J. 2000. Symphysis fundus height measurements during labour: A prospective, descriptive study. A J. Reprod. Health 4(1): 48-55. Cunningham, F.G.; McDonald, P.C.; Gant, N.F. 1993. Williams Obstetrics, 19th ed. Prentice-Hall Int., Norwalk, CT, USA. Dickason, E.J.; and Schult, M.O. 1998. Maternal-Infant Nursing Care. 1st ed. Mosby, St. Louis, MO, USA. Edwards, A. 2001. In the balance: the accuracy of sonographic estimation of fetal weight.
<http://www.asum.com.au.open/bullelin/v4 n1a.htm> Mhaskar, R.; Mhaskar, A. and Molly S.R. 2002. Symphysiofundal height (SFH) measurement for prediction of birth weight A new formula. J. Obstet.Gynecol . 51(4): 73-6. Mongelli, M.; and Gardosi, J. 1999. Symphysis - fundus height and pregnancy characteristics in ultrasound-dated pregnancies. Obstet Gyn.. 94: 591-4. OGrady, J.P.; and Gimovsky, M.L. 1995. Operative obstructs. William & Wilkins. Baltimore, MD, USA. Piper, J.M.; Xenakis, E.M.J.; McFarland, M.; Elliott, B.D.; Berkus, M.D. and Larger, O. 1996. Do growth-retarded premature infants have different rates of perinatal morbidity and mortality than appropriate grown premature infants? Obstet.Gyn. 87: 169-74. Promvijit, T.; Suntharasaj, T.; and Geater, A.A. 2000. Comparison of Leopolds Maneuver, McDonalds Measurement and Ultrasonic Estimation of Fetal Weight. <file//A Comparison of Leopolds maneuver, McDonalds> Sherwen, L.N.; Scoloveno, M.N.; and Weingarten, C.T. 1993. Nursing Care of the Childbearing Family. Appleton & Lange, New York, NY, USA.
20
Vous aimerez peut-être aussi
- Financial StatusDocument1 pageFinancial StatusJoshua Pattinson LegiPas encore d'évaluation
- Doctors For Kuwait: Atlas Consulting Is Currently Looking For Doctors To Recruit in Kuwait. We Urgently Look ForDocument3 pagesDoctors For Kuwait: Atlas Consulting Is Currently Looking For Doctors To Recruit in Kuwait. We Urgently Look ForJoshua Pattinson LegiPas encore d'évaluation
- ST BasilDocument1 pageST BasilJoshua Pattinson LegiPas encore d'évaluation
- Tiket PulaiDocument4 pagesTiket PulaiJoshua Pattinson LegiPas encore d'évaluation
- Gastroenteritis PPT Cha Dengan DiareDocument75 pagesGastroenteritis PPT Cha Dengan DiareJoshua Pattinson LegiPas encore d'évaluation
- Aum Serakup Indu ST BasilDocument1 pageAum Serakup Indu ST BasilJoshua Pattinson LegiPas encore d'évaluation
- Shoe Dog: A Memoir by the Creator of NikeD'EverandShoe Dog: A Memoir by the Creator of NikeÉvaluation : 4.5 sur 5 étoiles4.5/5 (537)
- The Yellow House: A Memoir (2019 National Book Award Winner)D'EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Évaluation : 4 sur 5 étoiles4/5 (98)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeD'EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeÉvaluation : 4 sur 5 étoiles4/5 (5794)
- The Little Book of Hygge: Danish Secrets to Happy LivingD'EverandThe Little Book of Hygge: Danish Secrets to Happy LivingÉvaluation : 3.5 sur 5 étoiles3.5/5 (400)
- Grit: The Power of Passion and PerseveranceD'EverandGrit: The Power of Passion and PerseveranceÉvaluation : 4 sur 5 étoiles4/5 (588)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureD'EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureÉvaluation : 4.5 sur 5 étoiles4.5/5 (474)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryD'EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryÉvaluation : 3.5 sur 5 étoiles3.5/5 (231)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceD'EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceÉvaluation : 4 sur 5 étoiles4/5 (895)
- Team of Rivals: The Political Genius of Abraham LincolnD'EverandTeam of Rivals: The Political Genius of Abraham LincolnÉvaluation : 4.5 sur 5 étoiles4.5/5 (234)
- Never Split the Difference: Negotiating As If Your Life Depended On ItD'EverandNever Split the Difference: Negotiating As If Your Life Depended On ItÉvaluation : 4.5 sur 5 étoiles4.5/5 (838)
- The Emperor of All Maladies: A Biography of CancerD'EverandThe Emperor of All Maladies: A Biography of CancerÉvaluation : 4.5 sur 5 étoiles4.5/5 (271)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaD'EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaÉvaluation : 4.5 sur 5 étoiles4.5/5 (266)
- On Fire: The (Burning) Case for a Green New DealD'EverandOn Fire: The (Burning) Case for a Green New DealÉvaluation : 4 sur 5 étoiles4/5 (74)
- The Unwinding: An Inner History of the New AmericaD'EverandThe Unwinding: An Inner History of the New AmericaÉvaluation : 4 sur 5 étoiles4/5 (45)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersD'EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersÉvaluation : 4.5 sur 5 étoiles4.5/5 (345)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyD'EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyÉvaluation : 3.5 sur 5 étoiles3.5/5 (2259)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreD'EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreÉvaluation : 4 sur 5 étoiles4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)D'EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Évaluation : 4.5 sur 5 étoiles4.5/5 (121)
- Her Body and Other Parties: StoriesD'EverandHer Body and Other Parties: StoriesÉvaluation : 4 sur 5 étoiles4/5 (821)
- Lawsuit Against DeWine, Ohio Over Coronavirus RestrictionsDocument56 pagesLawsuit Against DeWine, Ohio Over Coronavirus RestrictionsJo InglesPas encore d'évaluation
- Levetiracetam (Keppra®) in SarcinaDocument2 pagesLevetiracetam (Keppra®) in SarcinaI.m. DanielPas encore d'évaluation
- Relationship of Self-Regulation, Stress, and Life Satisfaction Among Middle School Students of Ekamai International School, Bangkok, ThailandDocument27 pagesRelationship of Self-Regulation, Stress, and Life Satisfaction Among Middle School Students of Ekamai International School, Bangkok, ThailandFrederick Edward FabellaPas encore d'évaluation
- BLSPPT 180126100212 PDFDocument58 pagesBLSPPT 180126100212 PDFKenneth PisofrintPas encore d'évaluation
- Vian Family Hospital - UgongDocument3 pagesVian Family Hospital - UgongKarenina VictoriaPas encore d'évaluation
- Internal Medicine NBME Form 3 ExplanationsDocument11 pagesInternal Medicine NBME Form 3 ExplanationssasghfdgPas encore d'évaluation
- MCN Oral Surgery Referral Guidelines For Gdps Jan 2019 v1Document23 pagesMCN Oral Surgery Referral Guidelines For Gdps Jan 2019 v1Smriti VermaPas encore d'évaluation
- Physical Therapy For Cardiopumonary DisordersDocument101 pagesPhysical Therapy For Cardiopumonary Disorderssunita_h100% (5)
- Pocket Guide For Asthma Management and PreventionDocument33 pagesPocket Guide For Asthma Management and PreventionRiaPas encore d'évaluation
- Term Requirement: Foundation of Special and Inclusive EducationDocument4 pagesTerm Requirement: Foundation of Special and Inclusive EducationMica Maureen Hipolito0% (1)
- Construction Style QuestionsDocument4 pagesConstruction Style QuestionsNikki DarlingPas encore d'évaluation
- Trigeminal NeuralgiaDocument18 pagesTrigeminal NeuralgiaKaran KohliPas encore d'évaluation
- Calypso Knee SystemDocument14 pagesCalypso Knee Systemapi-467445554Pas encore d'évaluation
- Title: Mock Drill: Hyderabad Chemical Products LimitedDocument4 pagesTitle: Mock Drill: Hyderabad Chemical Products Limitedakshay arya100% (1)
- Guide For Carers - Supporting and Caring For A Person With Depression Anxiety and or A Related DisorderDocument44 pagesGuide For Carers - Supporting and Caring For A Person With Depression Anxiety and or A Related DisorderPriya PuriPas encore d'évaluation
- Residents Self Assessment FormDocument5 pagesResidents Self Assessment Formapi-245673459Pas encore d'évaluation
- Bio Weapons TestsDocument10 pagesBio Weapons TestsRaptorman1973Pas encore d'évaluation
- Approach To Common Respiratory DiseaseDocument57 pagesApproach To Common Respiratory DiseaseRajhmuniran KandasamyPas encore d'évaluation
- Oxygen AdministrationDocument29 pagesOxygen Administrationjembut300100% (2)
- Part 2 Exam Sample Q 2015Document194 pagesPart 2 Exam Sample Q 2015Abdul QuyyumPas encore d'évaluation
- Circle DietDocument171 pagesCircle DietΧΤ90% (10)
- Psition Paper - Salupare - Ervin - DDocument2 pagesPsition Paper - Salupare - Ervin - DErvin SaluparePas encore d'évaluation
- NTMSPDocument84 pagesNTMSPAzry LuqmanPas encore d'évaluation
- RPH 2Document3 pagesRPH 2AYEN AROBINTOPas encore d'évaluation
- топик a visit to a dentistDocument2 pagesтопик a visit to a dentistEyeless DanteJackPas encore d'évaluation
- Full Download Test Bank For Priorities in Critical Care Nursing 6th Edition Urden PDF Full ChapterDocument36 pagesFull Download Test Bank For Priorities in Critical Care Nursing 6th Edition Urden PDF Full Chaptertenebraeaslakef0q6tz100% (23)
- Unit 2 - UHVDocument65 pagesUnit 2 - UHVSrihari PuttaPas encore d'évaluation
- Trauma Sequelae (Libro)Document537 pagesTrauma Sequelae (Libro)Andrea BautistaPas encore d'évaluation
- Aurobindo Pharma Receives USFDA Approval For Norethindrone Acetate Tablets (Company Update)Document1 pageAurobindo Pharma Receives USFDA Approval For Norethindrone Acetate Tablets (Company Update)Shyam SunderPas encore d'évaluation
- Chris Korhonian Korhonian 1Document6 pagesChris Korhonian Korhonian 1api-535175658Pas encore d'évaluation