Académique Documents
Professionnel Documents
Culture Documents
Blood Groups
Transféré par
Malik IrfanDescription originale:
Copyright
Formats disponibles
Partager ce document
Partager ou intégrer le document
Avez-vous trouvé ce document utile ?
Ce contenu est-il inapproprié ?
Signaler ce documentDroits d'auteur :
Formats disponibles
Blood Groups
Transféré par
Malik IrfanDroits d'auteur :
Formats disponibles
Blood group or blood type and Rh factor Blood group or blood type
Our blood is composed of blood cells and an aqueous fluid known as plasma. Human blood type is determined by the presence or absence of certain identifiers on the surface of red blood cells. These identifiers also called antigens, help the body's immune system to recognize its own red blood cell type. A total of 32 human blood group systems are now recognized by the International Society of Blood Transfusion (ISBT). The two most important ones are ABO and the RhD antigen. They determine four main ABO blood type groupings: A, B, AB, and O. These blood groups are determined by the antigen on the blood cell surface and the antibodies (Immunoglobulin M antibodies)present in the blood plasma. ABO antigens are glycolipid in nature, meaning they are oligosaccharides attached directly to lipids on red cell membrane Many pregnant women carry a fetus with a blood type different from their own, and the mother can form antibodies against fetal RBCs. Sometimes these maternal antibodies are IgG, a small immunoglobulin, which can cross the placenta and cause hemolysis of fetal RBCs, which in turn can lead to hemolytic disease of the newborn called erythroblastosis fetalis, an illness of low fetal blood counts that ranges from mild to severe. Sometimes this is lethal for the fetus; in these cases it is called hydrops fetalis.
The discovery of blood groups
Experiments with blood transfusions, the transfer of blood or blood components into a person's blood stream, have been carried out for hundreds of years. Many patients have died and it was not until 1901, when the Austrian Karl Landsteiner discovered human blood groups, that blood transfusions became safer. Mixing blood from two individuals can lead to blood clumping or agglutination. The clumped red cells can crack and cause toxic reactions. This can have fatal consequences. Karl Landsteiner discovered that blood clumping was an immunological reaction which occurs when the receiver of a blood transfusion has antibodies against the donor blood cells.
Karl Landsteiner's work made it possible to determine blood groups and thus paved the way for
blood transfusions to be carried out safely. For this discovery he was awarded the Nobel Prize in Physiology or Medicine in 1930.
ABO blood grouping system
According to the ABO blood group system there are four different kinds of blood groups: 1. 2. 3. 4. Blood Group Blood Group Blood Group Blood Group A B AB O (null).
1. Blood group A If you belong to the blood group A, you have A antigens on the surface of your red blood cells and B antibodies in your blood plasma. 2. Blood group B If you belong to the blood group B, you have B antigens on the surface of your red blood cells and A antibodies in your blood plasma. 3. Blood group AB If you belong to the blood group AB, you have both A and B antigens on the surface of your red blood cells and no A or B antibodies at all in your blood plasma. 4. Blood group O If you belong to the blood group 0 (null), you have neither A or B antigens on the surface of your red blood cells but you have both A and B antibodies in your blood plasma.
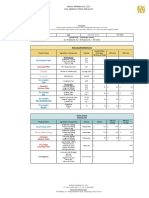
Type A+ O+ B+ AB+ AOBAB-
You Can Give Blood To A+ AB+ O+ A+ B+ AB+ B+ AB+ AB+ A+ A- AB+ ABEveryone B+ B- AB+ ABAB+ AB-
You Can Receive Blood From A+ A- O+ OO+ OB+ B- O+ OEveryone A- OOB- OAB- A- B- O-
According to above blood types, you can belong to either of following eight blood groups: A Rh+ A RhB Rh+ B RhAB Rh+ AB RhO Rh+ O Rh-
Rh+ blood can never be given to someone with Rh - blood, but the other way around works. For example, O Rh+ blood can not be given to someone with the blood type AB Rh -.
Blood Donors-since it can be life threatening to give the wrong ABO group to the patient.
Transfusion recipients-since we need to know the donor blood is ABO compatible. Transplant Candidates and Donors-ABO antigens are found in other tissues as well. Therefore the transplant candidates and donors must be compatible.
Prenatal Patients-To determine whether the mothers may have babies who are suffering from ABO-HDN. It is also beneficial to know the ABO group should she start hemorrhaging.
Newborns (sometimes) If the baby is demonstrating symptoms of Hemolytic Disease of the Newborn, the ABO group needs to be determined along with Rh and others.
Paternity testing Since the inheritance of the ABO Blood Group System is very specific, this serves as one of the first methods to determine the likelihood that the accused father is the father or not.
Rh blood system
Introduction The Rh (Rhesus) blood group system (including the Rh factor) is one of thirty-two current human blood group systems. it is the most important blood group system after ABO. At present, the Rh blood group system consists of 50 defined blood-group antigens, among which the five antigens D, C, c, E, and e are the most important.
This is the Rhesus (Rh) blood group system, which determines whether a blood type is negative or positive. The presence of the Rhesus D antigen decides whether you have positive or negative blood. The commonly used terms Rh factor, Rh positive and Rh negative refer to the D antigen only. Besides its role in blood transfusion, the Rh blood group system specifically, the D antigen is used to determine the risk of hemolytic disease of the newborn (or erythroblastosis fetalis) as prevention is key. Karl Landsteiner, an Austrian later American physician discovered ABO blood groups in 1900. . For this discovery he was awarded the Nobel Prize in Physiology or Medicine in 1930. In 1940,
10 years after receiving the Nobel Prize, he made still another famous discovery. This was a blood group called the Rh factor, named after rhesus monkeys, in which it was first found. Unlike the ABO system, antibodies to Rh antigens don't develop naturally. They develop only as an immune response after a transfusion or during pregnancy. The proteins which carry the Rh antigens are transmembrane proteins
Rh Antigens -Rh-Positive and Rh-Negative People.
There are six common types of Rh antigens, each of which is called an Rh factor. These types are designated C,D, E, c, d, and e. The type D antigen is widely prevalent in the population and considerably more antigenic than the other Rh antigens. Anyone who has this type of antigen is said to be Rh positive, whereas a person who does not have type D antigen is said to be Rh negative. However, it must be noted that even in Rhnegative people, some of the other Rh antigens can still cause transfusion reactions, although the reactions are usually much milder. About 85 per cent of all white people are Rh positive and 15 per cent, Rh negative. In American blacks, the percentage of Rh-positives is about 95, whereas in African blacks, it is virtually 100 per cent. Rh Immune Response Formation of Anti-Rh Agglutinins When red blood cells containing Rh factor are injected into a person whose blood does not contain the Rh factor that is, into an Rh-negative person anti Rh agglutinins develop slowly, reaching maximum concentration of agglutinins about 2 to 4 months later. This immune response occurs to a much greater extent in some people than in others. With multiple exposures to the Rh factor, an Rh-negative person eventually becomes strongly sensitized to Rh factor.
Vous aimerez peut-être aussi
- ABO Grouping & RH FactorDocument3 pagesABO Grouping & RH FactorMadhurima PurkaitPas encore d'évaluation
- Blood Groups: HAP Unit 5thDocument31 pagesBlood Groups: HAP Unit 5thC RonaldoPas encore d'évaluation
- Blood Groups: HAP Unit 5thDocument31 pagesBlood Groups: HAP Unit 5thSNEHASIS POLLEYPas encore d'évaluation
- The Blood Group Systems: Inheritance and GeneticsDocument34 pagesThe Blood Group Systems: Inheritance and GeneticsP Vinod Kumar100% (1)
- Blood GroupingDocument3 pagesBlood GroupingShanmuga Priya Shanmuga PriyaPas encore d'évaluation
- Blood TypesDocument17 pagesBlood TypesJenetaiswariyaPas encore d'évaluation
- Blood Groups: Blood Is A Specialized Bodily Fluid That Delivers Necessary Substances To The Body'sDocument11 pagesBlood Groups: Blood Is A Specialized Bodily Fluid That Delivers Necessary Substances To The Body'sayyappan6031Pas encore d'évaluation
- Blood Groups, Blood Typing and Blood TransfusionsDocument27 pagesBlood Groups, Blood Typing and Blood TransfusionsvishalkumarmorwalPas encore d'évaluation
- 1.blood GroupDocument38 pages1.blood GroupteraraPas encore d'évaluation
- Facts Statistics Awareness Video Clip Related Topics Citation Discussion PrintDocument6 pagesFacts Statistics Awareness Video Clip Related Topics Citation Discussion PrintprasadPas encore d'évaluation
- Blood Group System - EssayDocument9 pagesBlood Group System - EssayMarleth100% (1)
- Blood GroupingDocument3 pagesBlood GroupingJalajarani AridassPas encore d'évaluation
- Blood Type Test ExperimentDocument8 pagesBlood Type Test ExperimentUpz PhaPas encore d'évaluation
- ABO Blood GroupDocument12 pagesABO Blood GroupGhost AnkanPas encore d'évaluation
- Bio ProjectDocument10 pagesBio Projectshwetanshu2109Pas encore d'évaluation
- Blood TypingDocument6 pagesBlood TypingmaniiiiiiiiPas encore d'évaluation
- Blood GroupsDocument3 pagesBlood GroupsMian Talha KamalPas encore d'évaluation
- Abo Blood RH GroupingDocument27 pagesAbo Blood RH GroupingJames Carbonell Dela PeñaPas encore d'évaluation
- Bloog GroupDocument3 pagesBloog GroupChennai IbrahimPas encore d'évaluation
- Index: S.No Content Page NoDocument11 pagesIndex: S.No Content Page NoAufin SmartPas encore d'évaluation
- Blood Types A B O Ab: Reynaldo Cus 2CDocument6 pagesBlood Types A B O Ab: Reynaldo Cus 2CVirgilio CusPas encore d'évaluation
- Biology Project: C XIBDocument18 pagesBiology Project: C XIBPranjal SharmaPas encore d'évaluation
- BLood GroupsDocument6 pagesBLood GroupsAhsanFarooqPas encore d'évaluation
- Blood TypingDocument34 pagesBlood Typingaurezea100% (1)
- Blood GroupsDocument38 pagesBlood GroupsVirendra JoshiPas encore d'évaluation
- Abo Group.Document33 pagesAbo Group.R.KABILANPas encore d'évaluation
- Blood Group NotesDocument1 pageBlood Group NotesSabsPas encore d'évaluation
- ABO Blood Group System PDFDocument3 pagesABO Blood Group System PDFPerry Sin100% (1)
- Biology Investigatory Blood GroupDocument13 pagesBiology Investigatory Blood Groupanonymous user 345Pas encore d'évaluation
- Blood Group ND Transfusion - 231202 - 151259Document54 pagesBlood Group ND Transfusion - 231202 - 151259Archisman Mukherjee FAPSIANPas encore d'évaluation
- Lab 5Document22 pagesLab 5Aveen MustafaPas encore d'évaluation
- Blood Group MLDDocument5 pagesBlood Group MLDHarsheen KaurPas encore d'évaluation
- Blood GroupDocument1 pageBlood GroupĐỗ Ngọc ÁnhPas encore d'évaluation
- Abo Blood RH GroupingDocument22 pagesAbo Blood RH GroupingĐỗ Ngọc ÁnhPas encore d'évaluation
- Genotype and Blood Group CompatibilityDocument5 pagesGenotype and Blood Group CompatibilityajayranjithPas encore d'évaluation
- Blood Grouping and Cross MatchingDocument8 pagesBlood Grouping and Cross MatchingJeevitha Vanitha100% (1)
- Blood Grouping Presentation 4Document13 pagesBlood Grouping Presentation 4Aisha ShahfiqueePas encore d'évaluation
- Anatomy Module 17Document23 pagesAnatomy Module 17JayR MendonesPas encore d'évaluation
- Blood Type - Wikipedia 08-26-2021Document14 pagesBlood Type - Wikipedia 08-26-2021michael_sr_44Pas encore d'évaluation
- ABO Blood Grouping Cbsebiology4uDocument14 pagesABO Blood Grouping Cbsebiology4uRahit BiswasPas encore d'évaluation
- Blood GroupsDocument14 pagesBlood GroupsIsaac MapulangaPas encore d'évaluation
- Blood GroupsDocument2 pagesBlood GroupsAnuola OyindamolaPas encore d'évaluation
- Blood Groups and Blood Transfusion BioDocument23 pagesBlood Groups and Blood Transfusion BiowhyyoucarePas encore d'évaluation
- Blood Transfusion Is Generally The Process of Receiving Blood Products IntoDocument3 pagesBlood Transfusion Is Generally The Process of Receiving Blood Products IntoMaverick RodriguezPas encore d'évaluation
- Biology ProjectDocument21 pagesBiology ProjectBad Time?85% (13)
- Information About BloodDocument4 pagesInformation About BloodCalvin ChinPas encore d'évaluation
- Blood Case 6Document12 pagesBlood Case 6إنعام الحفيانPas encore d'évaluation
- 2 4 6 Neuro 1 Sistem Penggolongan Darah 3 Maret 2013Document91 pages2 4 6 Neuro 1 Sistem Penggolongan Darah 3 Maret 2013sari antiPas encore d'évaluation
- The Circulatory System - Blood Elements, Clotting, and The ABO and RH Blood Groups - EditedDocument6 pagesThe Circulatory System - Blood Elements, Clotting, and The ABO and RH Blood Groups - EditedJuliusPas encore d'évaluation
- LECTURE Blood GroupingDocument31 pagesLECTURE Blood Groupingjaveria choudharyPas encore d'évaluation
- Serologi ForensikDocument65 pagesSerologi ForensikbayuPas encore d'évaluation
- ABO Blood Group System CAIDocument34 pagesABO Blood Group System CAIrupertgrint2000Pas encore d'évaluation
- Blood BasicsDocument30 pagesBlood Basicskholoud220Pas encore d'évaluation
- Blood TypeDocument1 pageBlood TypeSohail ShareePas encore d'évaluation
- Blood Group PresentationDocument13 pagesBlood Group PresentationAli Hanzala YaseenPas encore d'évaluation
- ABO Blood Grouping Cbsebiology4uDocument15 pagesABO Blood Grouping Cbsebiology4uanandbhanwalkar111Pas encore d'évaluation
- Blood Groups, Blood Transfusion & Rhesus FactorDocument38 pagesBlood Groups, Blood Transfusion & Rhesus FactorUzma KhanPas encore d'évaluation
- ABO Blood Grouping Cbsebiology4uDocument10 pagesABO Blood Grouping Cbsebiology4usorojsahu85Pas encore d'évaluation
- The Connection Between Blood Type and Diseases: Health, #15D'EverandThe Connection Between Blood Type and Diseases: Health, #15Pas encore d'évaluation
- Subject: Field Observation Report: Pphi SindhDocument2 pagesSubject: Field Observation Report: Pphi Sindhrafique512Pas encore d'évaluation
- Read and Choose The Correct Answer From The Box Below.: Boys GirlsDocument1 pageRead and Choose The Correct Answer From The Box Below.: Boys GirlsjekjekPas encore d'évaluation
- Sound TherapyDocument1 pageSound TherapyibedaflyPas encore d'évaluation
- PAS HAndbookDocument375 pagesPAS HAndbookJheanell JamesPas encore d'évaluation
- Nephrolithiasis PDFDocument21 pagesNephrolithiasis PDFAulia AlmaPas encore d'évaluation
- Drug Addiction Treatment and Rehabilitation-Imran Ahmad SajidDocument108 pagesDrug Addiction Treatment and Rehabilitation-Imran Ahmad Sajidimranahmadsajid0% (1)
- Jurnal DysmenorrheaDocument10 pagesJurnal Dysmenorrheaanisah tri agustiniPas encore d'évaluation
- Clinic: Klinikos Is Sloping or Reclining and Latin Is ClinicusDocument3 pagesClinic: Klinikos Is Sloping or Reclining and Latin Is Clinicusfl004Pas encore d'évaluation
- Order of Payment: Food and Drug AdministrationDocument2 pagesOrder of Payment: Food and Drug AdministrationTheGood GuyPas encore d'évaluation
- MassageDocument13 pagesMassageAjay IyerPas encore d'évaluation
- Adrian Jess Galindo: DefinitionDocument2 pagesAdrian Jess Galindo: DefinitionAdrian MangahasPas encore d'évaluation
- Buffer Systems in The Body: Protein Buffers in Blood Plasma and CellsDocument11 pagesBuffer Systems in The Body: Protein Buffers in Blood Plasma and CellsK Jayakumar KandasamyPas encore d'évaluation
- Silver Is The New BlackDocument30 pagesSilver Is The New BlackSeptriyani KaswindiartiPas encore d'évaluation
- 2021 Nexus Pharma Injection Price List FinalDocument5 pages2021 Nexus Pharma Injection Price List FinalRyu SanurPas encore d'évaluation
- 1999 CQfirstphaseallotments PDFDocument73 pages1999 CQfirstphaseallotments PDFISMAIL KHANPas encore d'évaluation
- Life-Changed Self-Healing Series Ayurvedic Oil PullingDocument19 pagesLife-Changed Self-Healing Series Ayurvedic Oil PullingReverend Michael Zarchian Amjoy100% (2)
- Uv DoseDocument6 pagesUv DoseRajesh DeshmukhPas encore d'évaluation
- Cicatrización ImplanteDocument18 pagesCicatrización Implantejorge sepulvedaPas encore d'évaluation
- PIL 18047 LatestDocument2 pagesPIL 18047 LatestWendy EscalantePas encore d'évaluation
- 2 Articles From Oui Magazine (Feat. Robert Anton Wilson)Document16 pages2 Articles From Oui Magazine (Feat. Robert Anton Wilson)Jakob AndradePas encore d'évaluation
- DAFTAR PUSTAKA Rachel ParasianDocument3 pagesDAFTAR PUSTAKA Rachel ParasianAnto TomodachiRent SusiloPas encore d'évaluation
- Writing Knee OsteoarthritisDocument58 pagesWriting Knee OsteoarthritisHanani KamaludinPas encore d'évaluation
- Psychological Intervention Di Unit HemodialisaDocument19 pagesPsychological Intervention Di Unit HemodialisaAnjeli FiranikaPas encore d'évaluation
- Social and Psychological Manipulation PDFDocument287 pagesSocial and Psychological Manipulation PDFNicolae BeianPas encore d'évaluation
- Management of Infective EndocarditisDocument14 pagesManagement of Infective Endocarditismhafzam2020Pas encore d'évaluation
- The Supine PositionDocument29 pagesThe Supine PositionKlaue Neiv CallaPas encore d'évaluation
- Gestational Trophoblastic Neoplasia: NCCN Clinical Practice Guidelines in Oncology (NCCN Guidelines)Document45 pagesGestational Trophoblastic Neoplasia: NCCN Clinical Practice Guidelines in Oncology (NCCN Guidelines)Roshni SethiaPas encore d'évaluation
- PackagingDocument29 pagesPackagingSagar TummaPas encore d'évaluation
- Porco EspinhoDocument9 pagesPorco EspinhoLeticia LimaPas encore d'évaluation
- Nabh Entry LevelDocument64 pagesNabh Entry LevelRenuka MuruganPas encore d'évaluation