Académique Documents
Professionnel Documents
Culture Documents
Diagnostic Tests
Transféré par
Cristina L. JaysonDescription originale:
Copyright
Formats disponibles
Partager ce document
Partager ou intégrer le document
Avez-vous trouvé ce document utile ?
Ce contenu est-il inapproprié ?
Signaler ce documentDroits d'auteur :
Formats disponibles
Diagnostic Tests
Transféré par
Cristina L. JaysonDroits d'auteur :
Formats disponibles
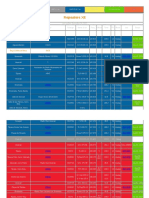
DIAGNOSTIC TESTS Hospital: Adventist Medical Center Iligan January 31, 2014 (on admission) CBC with platelet
et Blood Component Normal Values RBC 4-6 10 12/L Hematocrit 0.37-0.47 110-180 g/L 5-10 10 9/L 0.50-0.65 0.25-0.35 0.05-0.10 0.03-0.07 0.01-0.03 0.01 140-450 10 9/L
Result 4.30 0.34
Interpretation Normal Decreased
Significance May suggests anemia, hemodilution due to fluid retention
Hemoglobin WBC Segmenters
125.0 8.22 0.81
Normal Normal Increased
Viral and some bacterial infections, hepatitis. Decrease count occur in aplastic anemia, AIDS and bone marrow suppression Infection
Lymphocytes
0.15
Decreased
Stabs Monocytes Eosinophils Basophils Platelet Creatinine Normal Value (53-100 umol/L)
0 0.02 0.02 0 248
Normal Decreased Normal Normal Normal
Result 120.16
Interpretation Increased
Significance Impaired renal function or may suggest damage to the kidneys
February 2, 2014 HBSAG (for screening purposes) Normal Value Result nonreactive nonreactive Potassium Normal Value 3.5-5.3 mmol/L
Interpretation normal
Significance
Result 2.86
Interpretation Decreased
Significance Hypokalemia may results to vomiting or edema or ascites
February 3, 2014 Prothrombin time Result Patient: 12.3s Control: 13.1s Activity: 100% INR: 1.00
Interpretation normal
Significance
Bilirubin Normal Values Bilirubin (1.7-20.5 umol/L) B1 or indirect (1.7-17.1 umol/L) B2 or direct (0-5.1 umol/L)
Results 7.37 4.92 2.45
Interpretation Normal Normal Normal
Significance
Albumin Normal Values 35-54 g/L
Results 23.56
Interpretation Decreased
Significance Hypoalbuminemia may indicate acute liver failure
Liver Enzymes Normal Values Alanine aminotransferase or SGOT (8-40 Iu/L) Aspartate aminotransferase or SGPT (5-35 u/L)
Results 23.92 11.77
Interpretation Normal Normal
Significance
Whole Abdomen Ultrasound Normal Result Results A normal scan Impression: o Minimal hepatic reveals no parenchymal fatty change abnormalities in the o Cholelithiasis with chronic size, shape, or cholecystitis density of the organs scanned. o Normal sized kidneys with minimal parenchymal changes (no urolithiasis nor signs of ureteral obstruction) o Sonologically normal biliary ducts, pancreas, spleen, urinary bladder, uterus and adnexae o Minimal bilateral pleural effusion (165cc on the right and 187cc on the left) o Minimal ascites
Interpretation Abnormal result
Significance Chronic Cholecystitis Ascites (minimal) Pleural Effusion (Bilateral)
February 5, 2014 Creatinine Normal Value 53-100 umol/L
Result 107.10
Interpretation Increased
Significance Impaired renal function or may suggest damage to the kidneys
February 6, 2014 2D echo Normal Result A normal echocardiogram shows a normal heart structure and the normal flow of blood through the heart chambers and heart valves. Albumin Normal Values 35-54 g/L
Result Normal sized left ventricle with good wall motion and contractility, preserved overall systolic function.
Interpretation normal
Significance
Results 28.89
Interpretation Decreased
Significance Hypoalbuminemia may indicate acute liver failure
Thyroid-stimulating Hormone Normal Values Results (FT4) Free T4 (9-20pmol/L) 15.16 TSH (0.47-5.01 ulU/ml) 3.24
Interpretation Normal Normal
Significance
February 7, 2014 Upper Abdomen Ultrasound Normal Result Result A normal scan reveals o Follow-up Sonographic Evaluation no abnormalities in the showed the normal sized liver with size, shape, or density minimal fatty infiltration. of the organs scanned. o No focal parenchymal mass lesion seen. The gland outline is smooth. o The portal vein, intrahepatic and common bile duct are dilated. CBD = 4mm, normal caliber. o The gallbladder was partially contracted with minimal thickened wall. o The 3cm cholelithiasis was again noted. o The pancreas and the spleen are normal in size and configuration. o The abdominal aorta is normal in caliber with no abnormal focal dilatation. o Normal sized kidneys with minimal parenchymal changes. o Persistent minimal ascites with no significant interval change. o Persistent bilateral pleural effusion (219cc on the right and 195cc on the left). No significant interval regression.
Significance Cholecystitis Minimal Ascites Bilateral Pleural Effusion
Alkaline Phosphatase Normal Values Results 53-141 U/L 67.91 February 8, 2014
Interpretation Normal
Significance
Upper Gastrointestinal Endoscopy Normal Result Result The endoscopy o Esophagus: Unremarkable should reveal normal o Stomach: Some amount of food debris seen. function and Patchy areas of hyperemia and edematous appearance of the mucosa noted. No definite mass nor ulcer area being examined. seen in the visualized mucosa. Biopsy taken for rapid urease test. o Duodenum: 1st and 2nd portion: Unremarkable o H.pylori: Positive
Significance Gastritis with H.Pylori infection
Hemoglucotest (HGT) Monitoring Date Jan 31, 2014 Feb 1, 2014 Time 11PM 5AM 11AM 5PM 65 193 HGT Result 119
Normal Value: 60 110mg/dL Intervention
11PM Feb 2, 2014 5AM 11AM 5PM 11PM Feb 3, 2014 5AM 11AM 5PM Feb 4, 2014 5AM 11AM 5PM 11PM Feb 5, 2014 5AM 11AM 11PM Feb 6, 2014 5AM 11AM 5PM 11PM Feb 7, 2014 5AM 5PM 11PM Feb 8, 2014 5AM 11AM 8PM 11PM Feb 9, 2014 5AM 11PM
113 120 82 123 64 118 169 173 71 144 162 94 79 171 155 153 87 90 106 107 253 212 148 196 174 187 174 133 Humulin 70/30 10units pre-supper D50 W Humulin 70/30 20units prebreakfast
Hospital: Dr. Uy Hospital January 28, 2014 admission CBC with platelet Blood Component RBC Hematocrit Normal Values 4-4.5 10 12/L 0.37-0.45 120-140 g/L 5-10 10 9/L 0.55-0.70 0.25-0.40 0.01-0.08 140-440 10 9/L Result 3.5 0.31 Interpretation Decreased Decreased Significance May suggest anemia May suggests anemia, hemodilution due to fluid retention May indicate anemia or hemodilution due to fluid retention
Hemoglobin
104
Decreased
WBC Segmenters Lymphocytes Monocytes Platelet Creatinine Normal Values 0.50-1.20mg/dL or 53100 umol/L
8.9 0.66 0.29 0.05 240
Normal Normal Normal Normal Normal
Results 1.7 or 150.20 mmol/L
Interpretation Increased
Significance Impaired renal function or may suggest damage to the kidneys
Sodium Normal Values 135-148.0 mmol/L Potassium Normal Values 3.5-5.3 mmol/L
Results 143.0
Interpretation Normal
Significance
Results 2.97
Interpretation Decreased
Significance Hypokalemia may results to vomiting or edema or ascites
Chest X-ray PA view Normal Result Results A normal chest x Impression: o Minimal ray will show Cardiomegaly normal structures for the age and medical history of the patient.
Interpretation Abnormal result
Significance Cardiomegaly (minimal)
Whole Abdomen Ultrasound: Normal Result Results A normal scan Impression: reveals no o Minimal Hepatic Parenchymal Fatty Change o 3cm Cholelithiasis. No evidence of biliary abnormalities in the size, shape, or obstruction. density of the o Normal Sonographic Evaluation of the biliary organs scanned. ducts, pancreas, spleen, both kidneys, urinary bladder and uterus
Significance Cholelithiasis
January 29, 2014 Urine Analysis: Normal Values
Specific gravity Ph Protein Glucose Ketone Bilirubin Blood Nitrite Leukocyte Urobilinogen Micro RBCs WBCs RBC casts 1.002-1.030 5-7 negativetrace negative negative negative negative negative negative 0.2-1.0 Ehr U/dL 0-2/HPF 0-2/HPF 0/HPF
o o o o o o o o o
Results Color: Yellow pH: 7.0 Specific Gravity: 1.010 Sugar: +4 Albumin: +3 RBC: 7-10/HPF Epithelial Cells: Abundant Amorphous subs. : Few Bacteria: Moderate
Interpretation Presence of sugar, albumin with moderate bacteria
Significance Albuminuria, Glycosuria, possible UTI
January 30, 2014 Albumin Normal Values 38-51 g/L
Results 23.3
Interpretation Decreased
Significance Hypoalbuminemia may indicate acute liver failure
Potassium Normal Values 3.5-5.3 mmol/L
Results 2.81
Interpretation Decreased
Significance Hypokalemia may results to vomiting or edema or ascites
Hemoglucotest (HGT) Monitoring Date January 28, 2014 Time On admission 5PM January 29, 2014 5AM 5PM January 30, 2014 5AM 5PM January 31, 2014 5AM
Normal Value: 60 110mg/dL HGT Result 164.0 153.0 85 217.0 164.0 148.0 95 Intervention
Procedures and Nursing Interventions LABORATORY TESTS Albumin, Alkaline Phosphatase, Complete Blood Count (with Platelet Count), Creatinine, Hemoglucotest, Prothrombin Time, Serum Sodium and Potassium, SGOT, SGPT, TSH (TSH AND FREE T4).
PRETEST: Positively identify the patient using at least two unique identifiers before providing care, treatment, or services. Obtain a history of the patients complaints, including a list of known allergens, especially allergies or sensitivities to latex. Obtain a history of the patients gastrointestinal, genitourinary, and hepatobiliary systems, symptoms, and results of previously performed laboratory tests and diagnostic and surgical procedures. Obtain a list of the patients current medications including herbs, nutritional supplements, and nutraceuticals. Explain the procedure. Inform the patient that specimen collection takes approximately 5 to 10 min. Address concerns about pain and explain that there may be some discomfort during the venipuncture. Sensitivity to social and cultural issues, as well as concern for modesty, is important in providing psychological support before, during, and after the procedure. There are no food, fluid, or medication restrictions unless by medical direction.
INTRATEST: If the patient has a history of allergic reaction to latex, avoid the use of equipment containing latex. Instruct the patient to cooperate fully and to follow directions. Direct the patient to breathe normally and to avoid unnecessary movement. Observe standard precautions. Positively identify the patient, and label the appropriate tubes with the corresponding patient demographics, date, and time of collection. Perform a venipuncture. Remove the needle and apply direct pressure with dry gauze to stop bleeding. Observe venipuncture site for bleeding or hematoma formation and secure gauze with adhesive bandage. Promptly transport the specimen to the laboratory for processing and analysis.
POST-TEST: A written report of the results will be sent to the requesting health care provider (HCP), who will discuss the results with the patient. Instruct patient to resume any medications stopped before the test
SPECIAL CONSIDERATION: Creatinine Instruct patient to restrict activities 8 hours prior to the test Alkaline Phosphatase Instruct the patient to fast for at least 8 hours before the test because fat intake stimulates intestinal alkaline phosphatase (ALP) secretion Thyroid-stimulating Hormone venipuncture should be performed between 6 a.m. and 8 a.m.
URINANALYSIS
PRETEST: Explain that this analysis helps to diagnose renal or urinary tract disease and to evaluate overall body function. Inform the patient that there is no food or fluid restriction Notify the laboratory and physician of drugs the patient is taking that may affect laboratory results
INTRATEST: Collect a random urine specimen (a midstream-catch) of at least 15ml. obtain a firstvoided morning specimen if possible Label the specimen (name, date, time, physician) and submit to the laboratory within 30mins
POST-TEST: Inform the patient that she may resume her usual diet and medication
CHEST XRAY PRETEST: Positively identify the patient using at least two unique identifiers before providing care, treatment, or services. Inform the patient that the procedure assesses cardiopulmonary status. Explain that the patient will be asked to take a deep breath and hold it momentarily during the XRAY Explain that the test takes less than 5minutes Any metals should be remove from the patients body during the test
INTRATEST: The patient is instructed to stand or sit in front of a stationary radiography machine
POST-TEST: Assist the patients needs (e.g. changing of clothes) Instruct to resume activities and diet
UPPER AND WHOLE ABDOMEN ULTRASONOGRAPHY PRETEST: Make sure the patient or responsible party has signed a consent form Note and report all allergies Provide a fat-free meal in the evening before the procedure Tell the patient that he must fast for 8-12hours before the procedure Instruct the patient to remain still as possible during the procedure and to hold her breath when requested
INTRATEST: Assist the patient into a supine position
Coat the target area with a water-soluble jelly. The transducer is used to scan the area, projecting the images on the oscilloscope screen. The image on the screen is photographed for subsequent examination
POST-TEST: Remove the lubricating jelly from the patients skin Have the patient resume her normal diet
UPPER G.I. ENDOSCOPY PRETEST: Positively identify the patient using at least two unique identifiers before providing care, treatment, or services. Inform the patient that the procedure assesses the esophagus and upper GI tract. Obtain a history of the patients complaints, including a list of known allergens, especially allergies or sensitivities to latex, iodine, seafood, anesthetics, or contrast mediums. Obtain a history of the patients GI system, symptoms and results of previously performed laboratory tests and diagnostic and surgical procedures. Note any recent barium or other radiological contrast procedures ordered. Ensure that barium studies are performed after this study. Record the date of the last menstrual period and determine the possibility of pregnancy in perimenopausal women. Obtain a list of the patients current medications including anticoagulants, aspirin and other salicylates, herbs, nutritional supplements, and nutraceuticals. Note the last time and dose of medication taken. Review the procedure with the patient. Address concerns about pain related to the procedure and explain that some pain may be experienced during the test, and there may be moments of discomfort, but that the throat will be anesthetized with a spray or swab. Inform the patient that he or she will not be able to speak during the procedure, but that breathing will not be affected. Inform the patient that the procedure is performed in a GI lab or radiology department, usually by a health care provider (HCP) and support staff, and takes approximately 30 to 60 min. Sensitivity to social and cultural issues, as well as concern for modesty, is important in providing psychological support before, during, and after the procedure. Explain that an IV line may be started to allow for the infusion of a sedative or IV fluids. Inform the patient that a laxative and cleansing enema may be needed the day before the procedure, with cleansing enemas on the morning of the procedure, depending on the institutions policy. Inform the patient that dentures and eyewear will be removed before the test. Instruct the patient to remove jewelry and other metallic objects from the area to be examined. Instruct the patient to fast and restrict fluids for 8 hours prior to the procedure. Protocols may vary from facility to facility. Make sure a written and informed consent has been signed prior to the procedure and before administering any medications.
INTRATEST: Ensure the patient has complied with dietary and medication restrictions and pretesting preparations for at least 8 hr prior to the procedure. Ensure the patient has removed all external metallic objects from the area to be examined prior to the procedure.
Assess for completion of bowel preparation according to the institutions procedure. Have emergency equipment readily available. Instruct the patient to void prior to the procedure and to change into the gown, robe, and foot coverings provided. Instruct the patient to cooperate fully and to follow directions. Instruct the patient to remain still throughout the procedure because movement produces unreliable results. Observe standard precautions. Positively identify the patient, and label the appropriate collection container with the corresponding patient demographics, date, and time of collection. Obtain and record baseline vital signs. Start an IV line and administer ordered sedation. Spray or swab the oropharynx with a topical local anesthetic. Provide an emesis basin for the increased saliva and encourage the patient to spit out the saliva because the gag reflex may be impaired. Place the patient on an examination table in the left lateral decubitus position with the neck slightly flexed forward. The endoscope is passed through the mouth with a dental suction device in place to drain secretions. A side- viewing flexible, fiberoptic endoscope is advanced, and visualization of the GI tract is started. Air is insufflated to distend the upper GI tract, as needed. Biopsy specimens are obtained and/or endoscopic surgery is performed. Promptly transport the specimens to the laboratory for processing and analysis. At the end of the procedure, excess air and secretions are aspirated through the scope and the endoscope is removed. Remove the needle or catheter and apply a pressure dressing over the puncture site.
POST-TEST: A report of the examination will be sent to the requesting HCP, who will discuss the results with the patient. Observe the patient for indications of esophageal perforation (i.e., painful swallowing with neck movement, substernal pain with respiration, shoulder pain or dyspnea, abdominal or back pain, cyanosis, or fever). Do not allow the patient to eat or drink until the gag reflex returns; then allow the patient to eat lightly for 12 to 24 hr. Monitor vital signs and neurological status every 15 min for 1 hr, then every 2 hr for 4 hr, and as ordered by the HCP. Take temperature every 4 hr for 24 hr. Compare with baseline values. Notify the HCP if temperature is elevated. Protocols may vary from facility to facility. Instruct the patient to resume usual activity and diet in 24 hr or as tolerated after the examination, as directed by the HCP. Inform the patient that he or she may experience some throat soreness and hoarseness. Instruct patient to treat throat discomfort with lozenges and warm gargles when the gag reflex returns. Inform the patient that any belching, bloating, or flatulence is the result of air insufflation and is temporary. Instruct the patient that any severe pain, fever, difficulty breathing, or expectoration of blood must be immediately reported to the HCP. Recognize anxiety related to test results, and offer support. Discuss the implications of abnormal test results on the patients lifestyle. Provide teaching and information regarding the clinical implications of the test results, as appropriate.
2D ECHO PRETEST: Tell the patient that she may be asked to breathe in and out slowly, to hold her breath or to inhale a gas with a slightly sweet odor (amyl nitrite) while changes in heart function are recorded Warn about the possible adverse effects of amyl nitrite (dizziness, flushing, and tachycardia), but reassure that such effects quickly subsides Stress the need to remain still during the test because movement may distort results Explain that the test takes 15 to 30 minutes
INTRATEST: The patient is placed into the supine position and conductive gel is applied to the third or fourth intercostal space to the left of the sternum. The transducer is placed directly over it. The transducer is systematically angled to direct ultrasonic waves at specific parts of the patients heart. During the test, the oscilloscope screen is observed; significant findings are recorded on a strip chart recorder or on a videotape recorder For left lateral view, patient is placed on her left side Doppler echocardiography may also be used: color flow simulates RBC flow through the heart valves. The sound of blood flow may also be used to assess heart sounds and murmurs as they relate to cardiac hemodynamics
POST-TEST: Remove the conductive gel from the patients skin
Vous aimerez peut-être aussi
- Individual Therapy Key PointsDocument9 pagesIndividual Therapy Key PointsCristina L. JaysonPas encore d'évaluation
- Mindanao Sanitarium Nursing ClinicalsDocument1 pageMindanao Sanitarium Nursing ClinicalsCristina L. JaysonPas encore d'évaluation
- HelloDocument1 pageHelloCristina L. JaysonPas encore d'évaluation
- New Bon-NleDocument3 pagesNew Bon-NleCristina L. JaysonPas encore d'évaluation
- OooDocument1 pageOooCristina L. JaysonPas encore d'évaluation
- 3 RDDocument1 page3 RDCristina L. JaysonPas encore d'évaluation
- 1 STPRCDocument1 page1 STPRCCristina L. JaysonPas encore d'évaluation
- Medical Sources BibliographyDocument1 pageMedical Sources BibliographyCristina L. JaysonPas encore d'évaluation
- References For Drug Study and Diagnostic TestsDocument2 pagesReferences For Drug Study and Diagnostic TestsCristina L. JaysonPas encore d'évaluation
- May 2014 NLE Rooms CDODocument71 pagesMay 2014 NLE Rooms CDOCoolbuster.NetPas encore d'évaluation
- FBDocument1 pageFBCristina L. JaysonPas encore d'évaluation
- Nursing HistoryDocument1 pageNursing HistoryCristina L. JaysonPas encore d'évaluation
- CorrectionsDocument4 pagesCorrectionsCristina L. JaysonPas encore d'évaluation
- HAAD ReviewerDocument35 pagesHAAD ReviewerSydRey92% (24)
- PRC TinaDocument4 pagesPRC TinaCristina L. JaysonPas encore d'évaluation
- GordonsDocument3 pagesGordonsCristina L. JaysonPas encore d'évaluation
- Normal Anatomy and PhysiologyDocument8 pagesNormal Anatomy and PhysiologyCristina L. JaysonPas encore d'évaluation
- Diagnostic TestsDocument11 pagesDiagnostic TestsCristina L. JaysonPas encore d'évaluation
- Phytoplankton Data DipsinDocument125 pagesPhytoplankton Data DipsinCristina L. JaysonPas encore d'évaluation
- NCPDocument10 pagesNCPCristina L. JaysonPas encore d'évaluation
- 1st Phase ReportDocument42 pages1st Phase ReportCristina L. JaysonPas encore d'évaluation
- 3vital Information: Year) - BSED BioDocument3 pages3vital Information: Year) - BSED BioCristina L. JaysonPas encore d'évaluation
- Grand Case Presentation InformationDocument7 pagesGrand Case Presentation InformationCristina L. JaysonPas encore d'évaluation
- 634379489751247500Document32 pages634379489751247500Cristina L. JaysonPas encore d'évaluation
- IrisDocument4 pagesIrisYazmin Vasquez BarreraPas encore d'évaluation
- PerosDocument5 pagesPerosCristina L. JaysonPas encore d'évaluation
- Final DefenseDocument16 pagesFinal DefenseCristina L. JaysonPas encore d'évaluation
- Project Contract For Phyto Ra-2Document1 pageProject Contract For Phyto Ra-2Cristina L. JaysonPas encore d'évaluation
- Project Contract For Phyto Ra-2Document1 pageProject Contract For Phyto Ra-2Cristina L. JaysonPas encore d'évaluation
- Shoe Dog: A Memoir by the Creator of NikeD'EverandShoe Dog: A Memoir by the Creator of NikeÉvaluation : 4.5 sur 5 étoiles4.5/5 (537)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeD'EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeÉvaluation : 4 sur 5 étoiles4/5 (5794)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceD'EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceÉvaluation : 4 sur 5 étoiles4/5 (890)
- The Yellow House: A Memoir (2019 National Book Award Winner)D'EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Évaluation : 4 sur 5 étoiles4/5 (98)
- The Little Book of Hygge: Danish Secrets to Happy LivingD'EverandThe Little Book of Hygge: Danish Secrets to Happy LivingÉvaluation : 3.5 sur 5 étoiles3.5/5 (399)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryD'EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryÉvaluation : 3.5 sur 5 étoiles3.5/5 (231)
- Never Split the Difference: Negotiating As If Your Life Depended On ItD'EverandNever Split the Difference: Negotiating As If Your Life Depended On ItÉvaluation : 4.5 sur 5 étoiles4.5/5 (838)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureD'EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureÉvaluation : 4.5 sur 5 étoiles4.5/5 (474)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersD'EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersÉvaluation : 4.5 sur 5 étoiles4.5/5 (344)
- Grit: The Power of Passion and PerseveranceD'EverandGrit: The Power of Passion and PerseveranceÉvaluation : 4 sur 5 étoiles4/5 (587)
- On Fire: The (Burning) Case for a Green New DealD'EverandOn Fire: The (Burning) Case for a Green New DealÉvaluation : 4 sur 5 étoiles4/5 (73)
- The Emperor of All Maladies: A Biography of CancerD'EverandThe Emperor of All Maladies: A Biography of CancerÉvaluation : 4.5 sur 5 étoiles4.5/5 (271)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaD'EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaÉvaluation : 4.5 sur 5 étoiles4.5/5 (265)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreD'EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreÉvaluation : 4 sur 5 étoiles4/5 (1090)
- Team of Rivals: The Political Genius of Abraham LincolnD'EverandTeam of Rivals: The Political Genius of Abraham LincolnÉvaluation : 4.5 sur 5 étoiles4.5/5 (234)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyD'EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyÉvaluation : 3.5 sur 5 étoiles3.5/5 (2219)
- The Unwinding: An Inner History of the New AmericaD'EverandThe Unwinding: An Inner History of the New AmericaÉvaluation : 4 sur 5 étoiles4/5 (45)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)D'EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Évaluation : 4.5 sur 5 étoiles4.5/5 (119)
- Her Body and Other Parties: StoriesD'EverandHer Body and Other Parties: StoriesÉvaluation : 4 sur 5 étoiles4/5 (821)
- Pratt & Whitney Engine Training ResourcesDocument5 pagesPratt & Whitney Engine Training ResourcesJulio Abanto50% (2)
- B1 Grammar and VocabularyDocument224 pagesB1 Grammar and VocabularyTranhylapPas encore d'évaluation
- Duties of Trustees ExplainedDocument39 pagesDuties of Trustees ExplainedZia IzaziPas encore d'évaluation
- Council Of Architecture Scale Of ChargesDocument4 pagesCouncil Of Architecture Scale Of ChargesAshwin RajendranPas encore d'évaluation
- Geometry First 9 Weeks Test Review 1 2011Document6 pagesGeometry First 9 Weeks Test Review 1 2011esvraka1Pas encore d'évaluation
- MS0800288 Angh enDocument5 pagesMS0800288 Angh enSeason AkhirPas encore d'évaluation
- Hold-Up?" As He Simultaneously Grabbed The Firearm of Verzosa. WhenDocument2 pagesHold-Up?" As He Simultaneously Grabbed The Firearm of Verzosa. WhenVener MargalloPas encore d'évaluation
- FedSupport Codebook FY2020Document259 pagesFedSupport Codebook FY2020Aaron BlackmonPas encore d'évaluation
- Deep Work Book - English ResumoDocument9 pagesDeep Work Book - English ResumoJoão Pedro OnozatoPas encore d'évaluation
- ICE Professional Review GuidanceDocument23 pagesICE Professional Review Guidancerahulgehlot2008Pas encore d'évaluation
- Internship 2021: BY: Shantanu Anil MehareDocument8 pagesInternship 2021: BY: Shantanu Anil MehareShantanu MeharePas encore d'évaluation
- QuizInfo8 6 10Document373 pagesQuizInfo8 6 10Gill BeroberoPas encore d'évaluation
- Is the Prime Minister Too Powerful in CanadaDocument9 pagesIs the Prime Minister Too Powerful in CanadaBen YuPas encore d'évaluation
- Repeaters XE PDFDocument12 pagesRepeaters XE PDFenzzo molinariPas encore d'évaluation
- Mock-B1 Writing ReadingDocument6 pagesMock-B1 Writing ReadingAnonymous 0uBSrduoPas encore d'évaluation
- VB6 ControlDocument4 pagesVB6 Controlahouba100% (1)
- Project Notes PackagingDocument4 pagesProject Notes PackagingAngrej Singh SohalPas encore d'évaluation
- Innovations in Teaching-Learning ProcessDocument21 pagesInnovations in Teaching-Learning ProcessNova Rhea GarciaPas encore d'évaluation
- Lived Experiences of Science Teachers of Pangasinan Ii in The New Normal Education: A Phenomenological StudyDocument10 pagesLived Experiences of Science Teachers of Pangasinan Ii in The New Normal Education: A Phenomenological StudyIJAR JOURNALPas encore d'évaluation
- Shah Wali Ullah Syed Haji Shariat Ullah Ahmad Barelvi (Notes)Document2 pagesShah Wali Ullah Syed Haji Shariat Ullah Ahmad Barelvi (Notes)Samreen KapasiPas encore d'évaluation
- Diagnostic Laboratory TestsDocument6 pagesDiagnostic Laboratory TestsKiana Mae Wong Diwag100% (1)
- MATHS UNDERSTANDINGDocument15 pagesMATHS UNDERSTANDINGNurul IzzaPas encore d'évaluation
- Ar 318Document88 pagesAr 318Jerime vidadPas encore d'évaluation
- Assignment No1 of System Analysis and Design: Submitted To Submitted byDocument7 pagesAssignment No1 of System Analysis and Design: Submitted To Submitted byAnkur SinghPas encore d'évaluation
- The Dynamic Law of ProsperityDocument1 pageThe Dynamic Law of Prosperitypapayasmin75% (4)
- Specification For Corrugated Bitumen Roofing Sheets: Indian StandardDocument10 pagesSpecification For Corrugated Bitumen Roofing Sheets: Indian StandardAmanulla KhanPas encore d'évaluation
- Brother LS2300 Sewing Machine Instruction ManualDocument96 pagesBrother LS2300 Sewing Machine Instruction ManualiliiexpugnansPas encore d'évaluation
- Munslow, A. What History IsDocument2 pagesMunslow, A. What History IsGoshai DaianPas encore d'évaluation
- ĐỀ MINH HỌA 15-19Document25 pagesĐỀ MINH HỌA 15-19Trung Vũ ThànhPas encore d'évaluation
- Blood TestsDocument3 pagesBlood TestsMarycharinelle Antolin MolinaPas encore d'évaluation