Académique Documents
Professionnel Documents
Culture Documents
Hypovolemic Shock Due To Massive Edema of A Pedunculated Uterine Myoma After Delivery
Transféré par
Ana Di JayaTitre original
Copyright
Formats disponibles
Partager ce document
Partager ou intégrer le document
Avez-vous trouvé ce document utile ?
Ce contenu est-il inapproprié ?
Signaler ce documentDroits d'auteur :
Formats disponibles
Hypovolemic Shock Due To Massive Edema of A Pedunculated Uterine Myoma After Delivery
Transféré par
Ana Di JayaDroits d'auteur :
Formats disponibles
doi:10.1111/j.1447-0756.2008.00986.
J. Obstet. Gynaecol. Res. Vol. 35, No. 4: 794796, August 2009
Hypovolemic shock due to massive edema of a pedunculated uterine myoma after delivery
jog_986 794..796
Keiko Koide, Akihiko Sekizawa, Masamitsu Nakamura, Ryu Matsuoka and Takashi Okai
Department of Obstetrics and Gynecology, Showa University School of Medicine, Tokyo, Japan
Abstract
Although most patients with uterine myomas are asymptomatic during pregnancy, profound enlargement of a pedunculated myoma has serious consequences. In the present case, gradual enlargement of a pedunculated myoma was observed throughout a womans pregnancy, worsening after delivery and causing hypovolemic shock, without evidence of external or intra-abdominal hemorrhage. Laparotomy revealed a severely edematous myoma containing a large amount of blood. It is speculated that partial occlusion had obstructed venous return, but not arterial blood ow, which caused rapid enlargement of the myoma. Key words: massive edema, myoma, pregnancy, uterus.
Case Report
A 37-year-old woman, gravida 0, was conrmed to be pregnant at 6 weeks of gestation and to have an 8 11 cm abdominal tumor. Transvaginal ultrasonography revealed a subserosal myoma located on the posterior of her uterus, which was solid and homogeneous. The myoma gradually increased to 15 15 cm at 19 weeks of gestation. The distance between the fundus of the uterus and the symphysis pubis was 37 cm at 32 weeks, 38 cm at 34 weeks, and 42 cm at 36 weeks. Because the cervical os faced upward and the position of the fetal head was high at 37 weeks, an elective cesarean section was performed. A transverse incision of the lower uterine segment was made and a viable male infant weighing 2918 g was delivered. The myoma was located at the posterior of the uterus and occupied the entire abdominal cavity. The connection between the uterus and the myoma could not be observed. A blood loss of 1565 mL with a hemoglobin level of 9.1 g/dL occurred immediately following the cesarean section.
Twelve hours after delivery of the infant, the woman became hypotensive (55/28 mmHg) and tachycardic (130 b.p.m.). Her blood pressure was restored after she was given a blood transfusion and albumin. However, she again developed hypotension (79/45 mmHg) and tachycardia (152 b.p.m.) 24 h after delivery. She was then transferred to our hospital with a diagnosis of hypovolemic shock. When the patient arrived at our hospital, her consciousness was deteriorating and her blood pressure was 112/67 mmHg with a pulse rate of 163 b.p.m. Her hemoglobin level was 5.6 g/dL with markedly reduced urine output. She was given 16 units of blood by transfusion. Her platelet counts and coagulation factor levels were slightly decreased. We replenished her coagulation factors by administering fresh frozen plasma and an anti-thrombin III preparation. The patient was presumed to have an intra-abdominal hemorrhage; transabdominal sonography did not show any intraperitoneal uid, but revealed a solid tumor occupying her entire abdominal cavity. A contrast computed tomography (CT) scan demonstrated a massive 23 25 cm myoma behind the uterus with no obvious
Received: October 4 2007. Accepted: September 8 2008. Reprint request to: Dr Akihiko Sekizawa, Department of Obstetrics and Gynecology, Showa University School of Medicine, 1-5-8 Hatanodai, Shinagawa-ku, Tokyo 142-8666, Japan. Email: sekizawa@med.showa-u.ac.jp
794
2009 The Authors Journal compilation 2009 Japan Society of Obstetrics and Gynecology
Massive edema of a uterine myoma
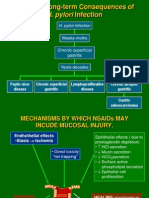
Ut i M Uterine Myoma
Figure 2 Haematoxylin-eosin staining of the myoma. (a) Magnication: 100. (b) Magnication: 400. Spindle tumor cells were observed with changes suggestive of hemorrhage, congestion, edema, and inammatory cellular inltration. The tumor cells resembled smooth muscle cells and broblasts.
Fallopian Tube Uterine Corpus PUBIS
Figure 1 Photograph taken during the surgery. The myoma was observed behind the uterus.
hematoma or ascites. Furthermore, intra-tumor bleeding was considered unlikely because the tumor appearance was not enhanced using contrast medium. The following day, the patient reported abdominal pain and slight dyspnea. Her hemoglobin level fell from 10.1 to 6.9 g/dL in the 36 h following delivery, at which point a second CT scan was performed. This scan showed that the tumor had increased to 25 27 cm in size with no ndings suggestive of intraabdominal or intra-tumor hemorrhage. We presumed that rapid enlargement of the tumor had led to the patients increasing dyspnea. Surgical removal of the tumor was performed on the third day of hospitalization. A small amount of ascites was observed with no hematoma within the abdominal cavity. The uterus was 10 10 12 cm in size and grayish-white in color, indicating ischemia. The patients ovaries were normal. Behind the uterus, a rm, dark red tumor was observed. The entire abdominal cavity was occupied by this tumor (Fig. 1), which was connected to the posterior of the uterus isthmus by a 4-cm pedicle. A hysterectomy was performed because we could not estimate the pathogenesis of the case. The weight of the resected specimen was 13 kg; this decreased to 9 kg 1 h after surgery due to deuxion of blood from the tumor. Total blood loss was 1915 mL and 14 units of blood were transfused during surgery. The patient was discharged from the hospital on postoperative day 10 with no complications.
The cut surface of the resected myoma was grayish and homogenous. Microscopically, spindle tumor cells with changes suggestive of hemorrhage, congestion, edema and inammatory cellular inltration were observed (Fig. 2). The tumor cells resembled smooth muscle cells and broblasts without necrotic features. The tumor characteristics resembled massive edema of the ovary.
Discussion
It is thought that uterine myoma size increases during pregnancy due to increasing estrogen levels and blood ow. In the present case, although the enlargement rate of the myoma was normal early in the pregnancy, the growth rate became abnormal later on. Furthermore, after delivery, rapid enlargement of the myoma caused hypovolemic shock, requiring a total of 30 units of blood. Pathologic analysis of the myoma revealed massive and diffuse intercellular edema within the myoma. The myoma was connected to the posterior wall of the lower uterine segment by a pedicle, which contained veins and feeding arteries. Some of the veins may have been compressed during the pregnancy, enhancing growth of the myoma. After delivery, partial compression may have obstructed venous return, but not arterial ow into the myoma. Thus, we speculated that hypovolemic shock following delivery was due to a large amount of blood sequestration from the maternal circulation into the myoma without overt hemorrhage. In the present case, the cause of partial occlusion is unknown. It is possible that after delivery, involution of the uterus and removal of the baby moved the tumor into a position that partially occluded venous blood from the pedicle. Therefore, it is suggested that
2009 The Authors Journal compilation 2009 Japan Society of Obstetrics and Gynecology
795
K. Koide et al.
hypovolemic shock might be avoided by removing pedunculated myomas, which may potentially undergo partial occlusion or torsion. A similar phenomenon has been described in the ovary.1,2 Kalstone et al. originally described partial torsion of the ovary leading to ovarian swelling.1 Microscopically, extensive parenchymal edematous change with occasional local stromal cell proliferation occurs in the ovary. One case of massive edema of a uterine myoma has been reported previously.3 In that case, rapid growth of the tumor was observed in the rst trimester, giving the impression of a malignant ovarian tumor. At 8 weeks of gestation, celiotomy revealed that the tumor was a uterine myoma connected to the fundus of the uterus by a pedicle. The tumor weighed 10 kg and its cut surface was grayish-white in color. Histologically, marked edematous change was noted. The tumor behaved similarly to that described in the present case. Although myomectomy performed during a cesarean section has been traditionally discouraged because
of a higher risk of bleeding, it has been reported that careful case selection could be benecial to patients. In the present case, subserosal myomectomy during a cesarean section was recommended to avoid subsequent partial occlusion or torsion. To the best of our knowledge, our case is only the second one of its kind to be reported. Although it occurs rarely, it is important to recognize that marked growth of a uterine myoma can occur in pregnancy and cause hypovolemic shock, particularly a subserosal myoma connected by a pedicle.
References
1. Kalstone CE, Jaffe RB, Abell MR. Massive edema of the ovary simulating broma. Obstet Gynecol 1969; 34: 564571. 2. Kanbour AI, Salazar H, Tobon H. Massive ovarian edema: A nonneoplastic pelvic mass of young women. Arch Pathol Lab Med 1979; 103: 4245. 3. Kawarabayashi T, Uchiyama Y, Nakamura S, Sugimori H. A huge rapidly growing leiomyoma in the rst trimester of pregnancy. Asia Oceania J Obstet Gynaecol 1985; 11: 557561.
796
2009 The Authors Journal compilation 2009 Japan Society of Obstetrics and Gynecology
Vous aimerez peut-être aussi
- Case Report on Dangerous Submucous Uterine MyomaDocument15 pagesCase Report on Dangerous Submucous Uterine MyomaOchabianconeriPas encore d'évaluation
- Unavoidable Myomectomy During Cesarean Section: A Case ReportDocument3 pagesUnavoidable Myomectomy During Cesarean Section: A Case ReportGuia Nina DuranPas encore d'évaluation
- Using Recombinant Activated Factor VII BDocument5 pagesUsing Recombinant Activated Factor VII BBagusHibridaPas encore d'évaluation
- A Rare Case of Abnormal Uterine Bleeding Caused by Cavernous Hemangioma: A Case ReportDocument3 pagesA Rare Case of Abnormal Uterine Bleeding Caused by Cavernous Hemangioma: A Case ReportprincessismaPas encore d'évaluation
- Jurnal Mioma UterusDocument6 pagesJurnal Mioma UterusHerlinaPas encore d'évaluation
- Spontaneous Rup-WPS OfficeDocument23 pagesSpontaneous Rup-WPS OfficePrithivi RajPas encore d'évaluation
- A Reading On HEMATOMA: Delivery Room Nursing RotationDocument7 pagesA Reading On HEMATOMA: Delivery Room Nursing RotationJulianePas encore d'évaluation
- Acute Non-Puerperal Uterine Inversion Case ReportDocument4 pagesAcute Non-Puerperal Uterine Inversion Case ReportALfuPas encore d'évaluation
- Management of Severe Postpartum Haemorrhage by Uterine Artery EmbolizationDocument4 pagesManagement of Severe Postpartum Haemorrhage by Uterine Artery EmbolizationAndi Tri SutrisnoPas encore d'évaluation
- Endocervical PolypDocument2 pagesEndocervical PolypRez007Pas encore d'évaluation
- Preventing Postpartum Hemorrhage: Prophylactic MeasuresDocument13 pagesPreventing Postpartum Hemorrhage: Prophylactic MeasuresAshish GuptaPas encore d'évaluation
- Discussion: Meigs' Syndrome and Pseudo-Meigs' SyndromeDocument3 pagesDiscussion: Meigs' Syndrome and Pseudo-Meigs' SyndromeFlapianne SimenceriauPas encore d'évaluation
- Case Report: Postpartum Uterine Wound Dehiscence Leading To Secondary PPH: Unusual SequelaeDocument4 pagesCase Report: Postpartum Uterine Wound Dehiscence Leading To Secondary PPH: Unusual SequelaemelisaberlianPas encore d'évaluation
- Placenta Increta Causing Um in The 26th Week of Pregnancy 2Document3 pagesPlacenta Increta Causing Um in The 26th Week of Pregnancy 2Kester ApostolPas encore d'évaluation
- Uterine Arteriovenous Malformation: Hilwati H, Ouzreiah NDocument5 pagesUterine Arteriovenous Malformation: Hilwati H, Ouzreiah NM Iqbal EffendiPas encore d'évaluation
- Tokushige 2017Document6 pagesTokushige 2017Mariela Mina RiveraPas encore d'évaluation
- A Case of Giant Uterine Fibroid in A Toung WomanDocument5 pagesA Case of Giant Uterine Fibroid in A Toung WomanTETINOUPas encore d'évaluation
- Couvelaire Uterus With Concealed Abruption Placenta A Case ReportDocument2 pagesCouvelaire Uterus With Concealed Abruption Placenta A Case ReportMDreamerPas encore d'évaluation
- Ectopic Mammary Tissue in The Axillary Region: A Case Report and Discussion of Diagnosis and ManagementDocument3 pagesEctopic Mammary Tissue in The Axillary Region: A Case Report and Discussion of Diagnosis and ManagementIJAR JOURNALPas encore d'évaluation
- Menstrual Disorders: Endometriosis, Dysmenorrhea and PMDDDocument37 pagesMenstrual Disorders: Endometriosis, Dysmenorrhea and PMDDOka ChintyaPas encore d'évaluation
- Post Partum Haemorrhage: M1, Fmbs DR Dohbit Sama Hgopy - FmbsDocument44 pagesPost Partum Haemorrhage: M1, Fmbs DR Dohbit Sama Hgopy - FmbsIdiAmadouPas encore d'évaluation
- Ectopic Pregnancy 2022 Edited 3Document40 pagesEctopic Pregnancy 2022 Edited 3apule geraldhumblePas encore d'évaluation
- Lipoma of The Uterine Corpus Exceptional Eventuality Combined With An Ovarian ThecomaDocument5 pagesLipoma of The Uterine Corpus Exceptional Eventuality Combined With An Ovarian ThecomaAlex HydronPas encore d'évaluation
- Benign Disorders and Breast DXDocument19 pagesBenign Disorders and Breast DXkurniafniatiPas encore d'évaluation
- Meigs' Syndrome and Pseudo-Meigs' Syndrome: Report of Four Cases and Literature ReviewsDocument6 pagesMeigs' Syndrome and Pseudo-Meigs' Syndrome: Report of Four Cases and Literature ReviewsAlfa FebriandaPas encore d'évaluation
- Laparoscopic Management of Cervical-Isthmic Pregnancy: A Proposal MethodDocument4 pagesLaparoscopic Management of Cervical-Isthmic Pregnancy: A Proposal MethodDinorah MarcelaPas encore d'évaluation
- Kondom Cateter EBMDocument3 pagesKondom Cateter EBMTeh NenkPas encore d'évaluation
- Postpartum Hemorrhage FinalDocument6 pagesPostpartum Hemorrhage FinalIanne Merh50% (2)
- Best practices for evaluating abnormal uterine bleedingDocument13 pagesBest practices for evaluating abnormal uterine bleedingVictoria Oliva ZúñigaPas encore d'évaluation
- Failure of Coil Embolization in Secondary Postpartum Hemorrhage A Case ReportDocument7 pagesFailure of Coil Embolization in Secondary Postpartum Hemorrhage A Case ReportInternational Journal of Innovative Science and Research TechnologyPas encore d'évaluation
- Uterine Fibroid Mimicking Ovarian TumorDocument3 pagesUterine Fibroid Mimicking Ovarian Tumorasshagab04Pas encore d'évaluation
- Postpartum Hemorrhage Post Placenta Previa Centralis-Conservative Management. Astrit M. GashiDocument4 pagesPostpartum Hemorrhage Post Placenta Previa Centralis-Conservative Management. Astrit M. GashiAstrit GashiPas encore d'évaluation
- Khing Journal...Document5 pagesKhing Journal...Khing AbatPas encore d'évaluation
- Abrasio PlacentaDocument3 pagesAbrasio Placentamuhammad azamPas encore d'évaluation
- Post Partum HemorrhageDocument38 pagesPost Partum Hemorrhageariani putri devantiPas encore d'évaluation
- Non-Puerperal Uterine Inversion Due To Submucous Myoma in A Young Woman: A CaseDocument3 pagesNon-Puerperal Uterine Inversion Due To Submucous Myoma in A Young Woman: A CaseMarc Lyndon CafinoPas encore d'évaluation
- Understanding Uterine FibroidsDocument52 pagesUnderstanding Uterine FibroidsDoctor JitPas encore d'évaluation
- International Journal of Pharmaceutical Science Invention (IJPSI)Document3 pagesInternational Journal of Pharmaceutical Science Invention (IJPSI)inventionjournalsPas encore d'évaluation
- 1 s2.0 S0015028201029004 MainDocument2 pages1 s2.0 S0015028201029004 MainMika OikuPas encore d'évaluation
- Giant Mucinous Cystadenoma Ovarii - Case ReportDocument12 pagesGiant Mucinous Cystadenoma Ovarii - Case ReportArio LukasPas encore d'évaluation
- Successful Use of Laparoscopic Myomectomy To Remove A Giant Uterine Myoma A Case ReportDocument4 pagesSuccessful Use of Laparoscopic Myomectomy To Remove A Giant Uterine Myoma A Case ReportnicabiPas encore d'évaluation
- 1749-7922-2-12 OvvDocument3 pages1749-7922-2-12 OvvomjoshPas encore d'évaluation
- Gynecology and Minimally Invasive Therapy: Case ReportDocument5 pagesGynecology and Minimally Invasive Therapy: Case ReportelenPas encore d'évaluation
- Endometriosis With Hemorrhagic AscitiesDocument5 pagesEndometriosis With Hemorrhagic AscitiesGavin TexeirraPas encore d'évaluation
- Department of Gynecology The Third Hospital Affiliated To Zhengzhou University LihongyuDocument44 pagesDepartment of Gynecology The Third Hospital Affiliated To Zhengzhou University Lihongyuapi-19916399Pas encore d'évaluation
- Abdominal Hysterectomy Is A Surgical Procedure in Which The Uterus Is Removed Through An Incision in The Lower AbdomenDocument6 pagesAbdominal Hysterectomy Is A Surgical Procedure in Which The Uterus Is Removed Through An Incision in The Lower AbdomenmajoharaPas encore d'évaluation
- Usui 2017Document6 pagesUsui 2017MochHabibEl-HuseinyPas encore d'évaluation
- Sigmoid Volvulus in Pregnancy: Case Report and Review OfliteratureDocument4 pagesSigmoid Volvulus in Pregnancy: Case Report and Review OfliteratureIJAR JOURNALPas encore d'évaluation
- Gynecology and Minimally Invasive Therapy: Shahul Hameed Mohamed Siraj, Bernard Su Min ChernDocument3 pagesGynecology and Minimally Invasive Therapy: Shahul Hameed Mohamed Siraj, Bernard Su Min ChernIrvin MarcelPas encore d'évaluation
- Case Report Large Uterine Fibroids in Pregnancy With Successful Caesarean MyomectomyDocument4 pagesCase Report Large Uterine Fibroids in Pregnancy With Successful Caesarean MyomectomyChidimma VictoryPas encore d'évaluation
- Chronic Uterine InversionDocument4 pagesChronic Uterine InversionnurelianaPas encore d'évaluation
- CDH Modern MXDocument11 pagesCDH Modern MXphobicmdPas encore d'évaluation
- Maternal Physiology-WilliamsDocument60 pagesMaternal Physiology-WilliamsRegina Marhadisony100% (1)
- Post Partum HemorrhageDocument18 pagesPost Partum Hemorrhageeric100% (1)
- Postpartum Hemorrhage GuideDocument6 pagesPostpartum Hemorrhage Guidevarshasharma05Pas encore d'évaluation
- Anesthetic Management of An Undiagnosed Advanced Extrauterine Pregnancy Under Combined Spinal-Epidural AnesthesiaDocument4 pagesAnesthetic Management of An Undiagnosed Advanced Extrauterine Pregnancy Under Combined Spinal-Epidural AnesthesiaHanayuki VizureiPas encore d'évaluation
- Lactating Adenoma A Case ReportDocument3 pagesLactating Adenoma A Case ReportInternational Journal of Innovative Science and Research TechnologyPas encore d'évaluation
- Complications of PostpartumDocument4 pagesComplications of PostpartumMargie Casicnan MabasaPas encore d'évaluation
- PlasentaDocument4 pagesPlasentaLois YunikePas encore d'évaluation
- 75178347Document5 pages75178347Ana Di JayaPas encore d'évaluation
- Renu GargDocument3 pagesRenu GargAna Di JayaPas encore d'évaluation
- A Pilot Evaluation of Saline Sonohysterography For Postmenopausal Bleeding With Thickened EndometriumDocument4 pagesA Pilot Evaluation of Saline Sonohysterography For Postmenopausal Bleeding With Thickened EndometriumAna Di JayaPas encore d'évaluation
- Viral Encephalitis: Etiology, Clinical Features, Diagnosis and ManagementDocument12 pagesViral Encephalitis: Etiology, Clinical Features, Diagnosis and ManagementAna Di JayaPas encore d'évaluation
- HydrotubationDocument4 pagesHydrotubationAna Di Jaya100% (1)
- Rountable Copd Jan 2012Document71 pagesRountable Copd Jan 2012Ana Di JayaPas encore d'évaluation
- Journal of Medical Case ReportsDocument4 pagesJournal of Medical Case ReportsAna Di JayaPas encore d'évaluation
- HydrotubationDocument4 pagesHydrotubationAna Di Jaya100% (1)
- Leiomyoma and Rhabdomyoma of The Vagina Vaginal MyomaDocument5 pagesLeiomyoma and Rhabdomyoma of The Vagina Vaginal MyomaAna Di JayaPas encore d'évaluation
- Case Report: Vaginal Myomectomy For A Thirteen-Centimeter Anterior MyomaDocument4 pagesCase Report: Vaginal Myomectomy For A Thirteen-Centimeter Anterior MyomaAna Di JayaPas encore d'évaluation
- Pengobatan Pada Tiap KomplikasiDocument6 pagesPengobatan Pada Tiap KomplikasiAna Di JayaPas encore d'évaluation
- Efficacy of Micronised Vaginal Progesterone Versus Oral Dydrogestrone in The Treatment of Irregular Dysfunctional Uterine Bleeding: A Pilot Randomised Controlled TrialDocument5 pagesEfficacy of Micronised Vaginal Progesterone Versus Oral Dydrogestrone in The Treatment of Irregular Dysfunctional Uterine Bleeding: A Pilot Randomised Controlled TrialAna Di JayaPas encore d'évaluation
- Cotrimoxazole Profilaxis Hiv Who Guidlines PDFDocument68 pagesCotrimoxazole Profilaxis Hiv Who Guidlines PDFAna Di JayaPas encore d'évaluation
- Who Guidlines Pregnancy Woman 2010 PDFDocument117 pagesWho Guidlines Pregnancy Woman 2010 PDFAna Di JayaPas encore d'évaluation
- WHO Dengue Guidelines 2013Document160 pagesWHO Dengue Guidelines 2013Jason MirasolPas encore d'évaluation
- 2 Pathogenesis TukakLambungDocument30 pages2 Pathogenesis TukakLambungAna Di JayaPas encore d'évaluation
- Vol361and2topic04 PDFDocument6 pagesVol361and2topic04 PDFAna Di JayaPas encore d'évaluation
- The Early Prevention of Stroke Heart Attack Perki SMG 05Document38 pagesThe Early Prevention of Stroke Heart Attack Perki SMG 05Ana Di JayaPas encore d'évaluation
- Case of A Womenwith Acute Onset of Chest Pain PDFDocument9 pagesCase of A Womenwith Acute Onset of Chest Pain PDFAna Di JayaPas encore d'évaluation
- Case of Adrenal Nodule in A 59 Yrs Old Women PDFDocument8 pagesCase of Adrenal Nodule in A 59 Yrs Old Women PDFAna Di JayaPas encore d'évaluation
- Case of Adrenal Nodule in A 59 Yrs Old Women PDFDocument8 pagesCase of Adrenal Nodule in A 59 Yrs Old Women PDFAna Di JayaPas encore d'évaluation
- Case of A Woman With Cough and Lung Nodule PDFDocument9 pagesCase of A Woman With Cough and Lung Nodule PDFAna Di JayaPas encore d'évaluation
- Case of Impaired Renal Funtion PDFDocument1 pageCase of Impaired Renal Funtion PDFAna Di JayaPas encore d'évaluation
- Case of A Woman With Obesity, DM An Hypertension PDFDocument10 pagesCase of A Woman With Obesity, DM An Hypertension PDFAna Di JayaPas encore d'évaluation
- Case of Bladder Carcinoma PDFDocument9 pagesCase of Bladder Carcinoma PDFAna Di JayaPas encore d'évaluation
- Case Report .Hepatic Failure PDFDocument4 pagesCase Report .Hepatic Failure PDFAna Di JayaPas encore d'évaluation
- Case of A Womenwith Acute Onset of Chest Pain PDFDocument9 pagesCase of A Womenwith Acute Onset of Chest Pain PDFAna Di JayaPas encore d'évaluation
- Case of Boy With Slowing Growth, Delayed Puberty PDFDocument11 pagesCase of Boy With Slowing Growth, Delayed Puberty PDFAna Di JayaPas encore d'évaluation
- Case of Bladder Carcinoma PDFDocument9 pagesCase of Bladder Carcinoma PDFAna Di JayaPas encore d'évaluation
- Vitamin B12 InfographicDocument2 pagesVitamin B12 InfographicIan WynnePas encore d'évaluation
- Sansure Biotech: Six Respiratory Pathogens Nucleic Acid Diagnostic Kit (PCR-Fluorescence Probing)Document4 pagesSansure Biotech: Six Respiratory Pathogens Nucleic Acid Diagnostic Kit (PCR-Fluorescence Probing)paulaPas encore d'évaluation
- Substance Abuse & PregnancyDocument2 pagesSubstance Abuse & PregnancyChelcee MagsinoPas encore d'évaluation
- RANZCO 2012 PosterDocument7 pagesRANZCO 2012 PosterGray Design GroupPas encore d'évaluation
- CASE 119 ScenarioDocument2 pagesCASE 119 Scenariojhan jhanPas encore d'évaluation
- Thromboembolic Disease in Pregnancy د.علية شعيبDocument50 pagesThromboembolic Disease in Pregnancy د.علية شعيبMohammad Belbahaith0% (1)
- Atls Trauma ThermalDocument36 pagesAtls Trauma ThermalsheisamarinkaPas encore d'évaluation
- Bacterial Infection of The Nervous SystemDocument16 pagesBacterial Infection of The Nervous Systemanisa rizkyPas encore d'évaluation
- PART I: Vocabulary (20 Items - 4,0 Pts - 0,2 PTS/ Item) Questions 1-5Document5 pagesPART I: Vocabulary (20 Items - 4,0 Pts - 0,2 PTS/ Item) Questions 1-5Nguyễn TavirelPas encore d'évaluation
- Screening Script and Procedure For Reception and SchedulingDocument3 pagesScreening Script and Procedure For Reception and SchedulingJobert NarvaezPas encore d'évaluation
- Prop Ae771263af039nwpDocument4 pagesProp Ae771263af039nwpPenielle SaguindanPas encore d'évaluation
- CV SAMEEP - PathologistDocument7 pagesCV SAMEEP - PathologistMumtaj AnsariPas encore d'évaluation
- Multi Lab Id ReportDocument12 pagesMulti Lab Id ReportMayuresh NaikPas encore d'évaluation
- Postpartum Period and ComplicationsDocument63 pagesPostpartum Period and ComplicationsSharmaineAnnePoliciosPas encore d'évaluation
- E000675 FullDocument37 pagesE000675 Fullmartina silalahiPas encore d'évaluation
- Sleep quality and daytime sleepiness in Arab diabeticsDocument9 pagesSleep quality and daytime sleepiness in Arab diabeticsYadi YudoyonoPas encore d'évaluation
- Prostate Cancer PDFDocument2 pagesProstate Cancer PDFkapczukPas encore d'évaluation
- Ischemic Heart Disease (IHD)Document70 pagesIschemic Heart Disease (IHD)Deborah AnnPas encore d'évaluation
- Cvspa01 Hypertension and AthrosclerosisDocument8 pagesCvspa01 Hypertension and AthrosclerosisRobert So JrPas encore d'évaluation
- How to Keep Your Heart HealthyDocument11 pagesHow to Keep Your Heart HealthyLarissa RevillaPas encore d'évaluation
- Untitled Presentation 4Document18 pagesUntitled Presentation 4sumegh sagarePas encore d'évaluation
- Health Assessment 9Document16 pagesHealth Assessment 9shannon c. lewisPas encore d'évaluation
- Preeclampsia With HELLP SyndromeDocument8 pagesPreeclampsia With HELLP SyndromeWely Tiffani YpPas encore d'évaluation
- Laporan-Diagnosa DesemberDocument421 pagesLaporan-Diagnosa DesemberPutri Annisa0% (1)
- MRCP NephrologyDocument394 pagesMRCP Nephrologyxplaind100% (8)
- Case Study PedsDocument11 pagesCase Study PedsGenesis Bicera100% (1)
- Urology MCQ Prometric 3Document138 pagesUrology MCQ Prometric 3Sara Badr57% (7)
- Diabetes Ada 2020 PDFDocument10 pagesDiabetes Ada 2020 PDFOrlando CuellarPas encore d'évaluation
- Prostate Cancer Symptoms, Screening, Stages and Treatment OptionsDocument45 pagesProstate Cancer Symptoms, Screening, Stages and Treatment OptionsNeethiselvam Devadoss100% (2)
- Cerebrospinal Fluid (CSF) Sample RequirementsDocument7 pagesCerebrospinal Fluid (CSF) Sample RequirementsDr.Nouf alhasawiPas encore d'évaluation