Académique Documents
Professionnel Documents
Culture Documents
Subacute and Chronic Forms of Meningitis
Transféré par
Risdan Hardani TjlCopyright
Formats disponibles
Partager ce document
Partager ou intégrer le document
Avez-vous trouvé ce document utile ?
Ce contenu est-il inapproprié ?
Signaler ce documentDroits d'auteur :
Formats disponibles
Subacute and Chronic Forms of Meningitis
Transféré par
Risdan Hardani TjlDroits d'auteur :
Formats disponibles
SUBACUTE AND CHRONlC FORMS OF MENlNGlTlS (See also Chap.
33)
There are many infectious processes that induce an inflammation of the leptomeninges of lesser
intensity than the acute forms described above. lncluded here are some bacterial and most
mycotic infections, tuberculosis, syphilis, Lyme disease, human immunodeficiency virus (HlV)
infection, and presumed noninfectious causes, such as lymphoma, sarcoidosis, Wegener
granulomatosis, and others. As pointed out by Ellner and Bennett (their experience coincides
with that of Swartz and our own), the clinical syndrome comprises cognitive disorders, seizures,
absence of lateralizing and focal cerebral signs, with or without headache and mild stiffness of
the neck. ln some cases there is little or no fever or other manifestation of infection. As with
acute bacterial meningitis, the CSF will usually divulge the causative agent, but not so readily as
in acute bacterial meningitis, since the organisms are more difficult to detect and culture. The
main identifiable forms of subacute and chronic meningitis are described below. The approach
to the complicated problem of chronic meningitis (aseptic variety) in which no cause can be
found is addressed in Chap. 33.
Tuberculous Meningitis
ln the United States and in most western countries, the incidence of tuberculous meningitis,
which reflects the incidence of systemic tuberculosis, has until recently decreased steadily since
the Second World War. At the Cleveland Metropolitan General Hospital, for example, the
incidence of tuberculous meningitis during the years l959 to l963 was between 4.4 and 8.4 per
l0,000 admissions (a decade earlier it was 5.8 to l2.9 per l0,000 admissions). By contrast, at
the K. E. M. Hospital in Bombay during the period l96l to l964, the incidence of this disease (in
children) was 400 per l0,000 admissions, and similar figures have been reported from other
parts of lndia. Since l985, however, there has been a significant increase in the incidence of
systemic tuberculosis (and tuberculous meningitis) in the United Statesa l6 percent annual
increase compared to an average annual decline of 6 percent during the preceding 30 years
(Snider and Roper). This increase is due mainly though not exclusively to the HlV epidemic. ln
fact, tuberculosis may be the first clinical manifestation of HlV infection (Barnes et al); among
patients with full-blown AlDS, the incidence of tuberculosis is almost 500 times the incidence in
the general population (Pitchenik et al). ln developing countries, particularly in sub-Saharan
Africa, the incidence of tuberculosis is estimated to be more than 25 times that in the United
States, again largely because of the prevalence of HlV infection.
Pathogenesis Tuberculous meningitis is usually caused by the acid-fast organism
Mycobacterium tuberculosis and exceptionally by Mycobacterium bovis or Mycobacterium
fortuitum. The emergence of AlDS has led to a marked increase in cases caused by both the
classic organism and these last two atypical mycobacteria. Rich described two stages in the
pathogenesis of the meningitisfirst a bacterial seeding of the meninges and subpial regions of
the brain with the formation of tubercles, followed by the rupture of one or more of the tubercles
and the discharge of bacteria into the subarachnoid space. Whether the meningitis always
originates in this way is, in our opinion, somewhat uncertain. The meningitis may occur as a
terminal event in cases of miliary tuberculosis or as part of generalized tuberculosis with a
single focus (tuberculoma) in the brain.
Pathologic Findings Small, discrete white tubercles are scattered over the base of the cerebral
hemispheres and to a lesser degree on the convexities. The brunt of the pathologic process falls
on the basal meninges, where a thick, gelatinous exudate accumulates, obliterating the pontine
and interpeduncular cisterns and extending to the meninges around the medulla, the floor of the
third ventricle and subthalamic region, the optic chiasm, and the undersurfaces of the temporal
lobes (Fig. 32-2). By comparison, the convexities are little involved, possibly because the
associated hydrocephalus obliterates the cerebral subarachnoid space. Microscopically, the
meningeal tubercles are like those in other parts of the body, consisting of a central zone of
caseation surrounded by epithelioid cells and some giant cells, lymphocytes, plasma cells, and
connective tissue. The exudate is composed of fibrin, lymphocytes, plasma cells, other
mononuclear cells, and some polymorphonuclear leukocytes. The ependyma and choroid
plexus are studded with minute glistening tubercles. The exudate also surrounds the spinal
cord. Unlike the pyogenic meningitides, the disease process is not confined to the subarachnoid
space but frequently penetrates the pia and ependyma and invades the underlying brain, so that
the process is truly a meningoencephalitis.
Figure 32-2 MRl in tuberculous meningitis. There is gadolinium enhancement of the basal
meninges reflecting intense inflammation that is accompanied by hydrocephalus and cranial
nerve palsies.
Other pathologic changes depend upon the chronicity of the pathologic process and recapitulate
the changes that occur in the subacute and chronic stages of the pyogenic meningitides (Table
32-l). Cranial nerves are often involved by the inflammatory exudate as they traverse the
subarachnoid space. Arteries may become inflamed and occluded, with infarction of brain.
Blockage of the basal cisterns frequently results in a meningeal obstructive type of
hydrocephalus. Marked ependymitis with blocking of the CSF in the aqueduct or fourth ventricle
is a less common cause. The exudate may predominate around the spinal cord, leading to
multiple spinal radiculopathies and compression of the cord.
Clinical Features Tuberculous meningitis occurs in persons of all ages. Formerly it was more
frequent in young children, but now it is more frequent in adults, at least in the United States.
The early manifestations are usually low-grade fever, malaise, headache (more than one-half
the cases), lethargy, confusion, and stiff neck (75 percent of cases), with Kernig and Brudzinski
signs. Characteristically, these symptoms evolve less rapidly in tuberculous than in bacterial
meningitis, usually over a period of a week or two, sometimes longer. ln young children and
infants, apathy, hyperirritability, vomiting, and seizures are the usual symptoms; stiff neck may
not be prominent or may be absent altogether.
Because of the inherent chronicity of the disease, signs of cranial nerve involvement (usually
ocular palsies, less often facial palsies or deafness) and papilledema may be present at the time
of admission to the hospital (in 20 percent of the cases). Occasionally the disease may present
with the rapid onset of a focal neurologic deficit due to hemorrhagic infarction, with signs of
raised intracranial pressure, or with symptoms referable to the spinal cord and nerve roots.
Hypothermia and hyponatremia have been additional presenting features in several of our
cases.
ln approximately two-thirds of patients with tuberculous meningitis there is evidence of active
tuberculosis elsewhere, usually in the lungs and occasionally in the small bowel, bone, kidney,
or ear. ln some patients, however, only inactive pulmonary lesions are found, and in others
there is no evidence of tuberculosis outside of the nervous system. ln the previously mentioned
Cleveland series, which comprised 35 patients, active pulmonary tuberculosis was found in l9,
inactive in 6, and involvement of the nervous system alone in 9; only 2 of the 35 patients had
nonreactive tuberculin tests (Hinman). Among our adult patients, tuberculous meningitis is now
seen mainly in those with AlDS, in alcoholics, and in immigrants from the Far East and lndia.
Except for the emergence of drug-resistant organisms, the HlV infection does not appear to
change the clinical manifestations or the outcome of tuberculous meningitis. However, others
disagree, insisting that the course of the bacterial infection is accelerated in AlDS patients, with
more frequent involvement of organs other than the lungs.
lf the illness is untreated, its course is characterized by confusion and progressively deepening
stupor and coma, coupled with cranial nerve palsies, pupillary abnormalities, focal neurologic
deficits, raised intracranial pressure, and decerebrate postures; invariably, a fatal outcome
follows within 4 to 8 weeks of the onset.
Laboratory Studies Again, the most important is the lumbar puncture, which preferably should
be performed before the administration of antibiotics. The CSF is usually under increased
pressure and contains between 50 and 500 white cells per cubic millimeter, rarely more. Early in
the disease there may be a more or less equal number of polymorphonuclear leukocytes and
lymphocytes; but after several days, lymphocytes predominate in the majority of cases. ln some
cases, however, M. tuberculosis causes a persistent polymorphonuclear pleocytosis, the other
usual causes of this CSF formula being Nocardia, Aspergillus, and Actinomyces (Peacock). The
one case with a persistent polymorphonuclear response in our experience was due to M.
fortuitum. The protein content of the CSF is always elevated, between l00 to 200 mg/dL in most
cases, but much higher if the flow of CSF is blocked around the spinal cord. Glucose is reduced
to levels below 40 mg/dL but rarely to the very low values observed in pyogenic meningitis; the
glucose falls slowly and a reduction may become manifest only several days after the patient
has been admitted to the hospital. The serum sodium and chloride and CSF chloride are often
reduced, in most instances because of inappropriate ADH secretion or tuberculosis of the
adrenals.
The conventional methods of demonstrating tubercle bacilli in the spinal fluid are inconsistent
and often too slow for immediate clinical decisions. The traditional identification of tubercle
bacilli in smears of CSF sediment, stained by the Ziehl-Neelsen method, is a function not only of
their number but also of the persistence with which they are sought. There are effective means
of culturing the tubercle bacilli; but since their quantity is usually small, attention must be paid to
proper technique. The amount of CSF submitted to the laboratory is critical; the more that is
cultured, the greater the chances of recovering the organism. Unless one of the newer
techniques is utilized, growth in culture media is not seen for 3 to 4 weeks. The polymerase
chain reaction (PCR), a method of DNA amplification that permits the detection of small
amounts of tubercle bacilli, is now widely available for clinical use. There is also a rapid culture
technique that allows identification of the organisms in less than l week. However, even these
new diagnostic methods may give uncertain results or take several days to demonstrate the
organism, and they cannot be counted on to exclude the diagnosis. For these reasons, if a
presumptive diagnosis of tuberculous meningitis has been made and cryptococcosis and other
fungal infections and meningeal neoplasia have been excluded, treatment should be instituted
immediately, without waiting for the results of bacteriologic study.
Other diagnostic procedures (CT, MRl) may be necessary in patients who present with or
develop raised intracranial pressure, hydrocephalus, or focal neurologic deficits. One or more
tuberculomas may also be visualized (see below). MR angiography may demonstrate vascular
occlusive disease from granulomatous infiltration of the walls of arteries of the circle of Willis
and their primary branches.
Other Forms of Central Nervous System Tuberculosis
Tuberculous Serous Meningitis This condition, which is essentially a self-limited meningitis, is
observed with some frequency in countries where tuberculosis is prevalent. The CSF shows a
modest pleocytosis in some but not all cases, a normal or elevated protein content, and normal
glucose levels. Headache, lethargy, and confusion are present in some cases and there are
mild meningeal signs. Lincoln, who was the first to call attention to this syndrome, believed it to
be a meningeal reaction to an adjacent tuberculous focus that did not progress to a frank
meningitis. This form of meningitis is not always self-limited. ln two of our patients who
presented with a brainstem tuberculoma, there was a serous meningitis that progressed to a
fatal generalized tuberculous meningitis.
Tuberculomas These are tumor-like masses of tuberculous granulation tissue, sometimes
multiple, that form in the parenchyma of the brain and range from 2 to l2 mm in diameter (Fig.
32-3). The larger ones may produce symptoms of a space-occupying lesion and periventricular
ones may cause obstructive hydrocephalus, but many are unaccompanied by symptoms of
focal cerebral disease. ln the United States tuberculomas are rarities; but in developing
countries they constitute from 5 to 30 percent of all intracranial mass lesions. ln some tropical
countries, cerebellar tuberculomas are the most frequent intracranial tumors in children.
Because of their proximity to the meninges, the CSF often contains a small number of
lymphocytes and increased protein (serous meningitis), but the glucose level is not reduced.
True tuberculous abscesses of the brain are rare except in AlDS patients.
Figure 32-3 A tuberculoma of the deep hemisphere in a Caribbean emigrant to the United
States. The mass behaved clinically, and appears on a gadolinium-enhanced MRl, like a
primary malignant brain tumor.
Myeloradiculitis The spinal cord may be affected in a number of ways in the course of
tuberculous infection. ln addition to compressing spinal roots and cord, causing spinal block, the
inflammatory meningeal exudate may invade the underlying parenchyma, producing signs of
posterior and lateral column and spinal root disease. Spinal cord symptoms may also
accompany tuberculous osteomyelitis of the spine with compression of the cord by an epidural
abscess, a mass of granulation tissue, or, less frequently, by the mechanical effects of
angulation of the vertebral column (Pott's paraplegia).
Treatment of Tuberculous Meningitis
The treatment of tuberculous meningitis consists of the administration of a combination of drugs
isoniazid (lNH), rifampin (RMP), and a third and sometimes a fourth drug, which may be
ethambutal (EMB), ethionamide (ETA), or preferably pyrazinamide (PZA). All of these drugs
have the capacity to penetrate the blood-brain barrier, with lNH, ETA, and PZA ranked higher
than the others in this respect. Resistant strains are emerging, which require the use of PZA
and ETA in addition to the two main drugs (lNH and RMP). Antibiotics must be given for a
prolonged period, l8 to 24 months as a general rule (although it may not be necessary to give
all three or four drugs for the entire period).
lsoniazid is the single most effective drug. lt can be given in a single daily dose of 5 mg/kg in
adults and l0 mg/kg in children. lts most important adverse effects are neuropathy (see page
l395) and hepatitis, particularly in alcoholics. Neuropathy can be prevented by the
administration of 50 mg pyridoxine daily. ln patients who develop the symptoms of hepatitis or
have abnormal liver function tests, lNH should be discontinued. The usual dose of RMP is 600
mg daily for adults, l5 mg/kg for children. Ethambutal is given in a single daily dose of l5
mg/kg. The dosage of ETA is l5 to 25 mg/kg daily for adults; because of its tendency to
produce gastric irritation, it is given in divided doses, after meals. The latter two drugs (EMB and
ETA) may cause optic neuropathy, so that patients taking them should have regular
examinations of visual acuity and red-green color discrimination. Pyrazinamide is given once
daily in doses of 20 to 35 mg/kg. Rash, gastrointestinal disturbances, and hepatitis are the main
adverse effects. Except for lNH, all these drugs can only be given orally or by stomach tube.
lsoniazid may be given parenterally, in the same dosage as with oral use. Corticosteroids
should be used only in patients whose lives are threatened by the effects of subarachnoid block
or raised intracranial pressure, and only in conjunction with antituberculous drugs.
lntracranial tuberculoma calls for a similar course of antibiotics, as outlined above. Under the
influence of these drugs, the tuberculoma(s) may decrease in size and small ones ultimately
disappear or calcify, as judged by the CT scan; if they do not, and especially if there is "mass
effect," excision may be necessary. Patients with spinal osteomyelitis (Pott's paraplegia) or
localized granulomas with spinal cord compression should also be explored surgically after an
initial course of chemotherapy, and an attempt should be made to excise the tuberculous focus.
We have, however, dealt successfully with tuberculous osteomyelitis of the cervical spine
(without significant abscess) by immbolization in a hard collar and triple drug therapy (at the
suggestion of the patient's father, who was a physician in lndia), once it was established that the
spinal column was stable.
The overall mortality of patients with CNS tuberculosis is still significant (about l0 percent),
infants and the elderly being at greatest risk. Among HlV-infected patients, the mortality from
tuberculous meningitis is considerably higher (2l percent in the series of Berenguer et al)the
result of delays in diagnosis and, more importantly, of resistance to antituberculous drugs in
some patients (Snider and Roper). Early diagnosis, as one might expect, enhances the chances
of survival. ln patients who are treated late in the disease, when coma has supervened, the
mortality rate is nearly 50 percent. Between 20 and 30 percent of survivors manifest a variety of
residual neurologic sequelae, the most important of which are retarded intellectual function,
psychiatric disturbances, recurrent seizures, visual and oculomotor disorders, deafness, and
hemiparesis. A detailed account of these has been given by Wasz-Hockert and Donner.
Vous aimerez peut-être aussi
- Antibiotics and Analgesics During LactationDocument12 pagesAntibiotics and Analgesics During LactationHarish KumarPas encore d'évaluation
- ATS GuidelinesDocument46 pagesATS Guidelinesapi-3847280100% (1)
- Acute Bacterial MeningitisDocument17 pagesAcute Bacterial MeningitisLuvi PujiPas encore d'évaluation
- Css DyspepsiaDocument17 pagesCss DyspepsiaRisdan Hardani TjlPas encore d'évaluation
- Epulis GravidarumDocument4 pagesEpulis GravidarumRisdan Hardani TjlPas encore d'évaluation
- Epulis GravidarumDocument4 pagesEpulis GravidarumRisdan Hardani TjlPas encore d'évaluation
- Odontogenic Infections-No FiguresDocument12 pagesOdontogenic Infections-No FiguresFitri Andam DewiPas encore d'évaluation
- Odontogenic Infections-No FiguresDocument12 pagesOdontogenic Infections-No FiguresFitri Andam DewiPas encore d'évaluation
- Odontogenic Infections-No FiguresDocument12 pagesOdontogenic Infections-No FiguresFitri Andam DewiPas encore d'évaluation
- Cauda EquinaDocument3 pagesCauda EquinaRisdan Hardani TjlPas encore d'évaluation
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeD'EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeÉvaluation : 4 sur 5 étoiles4/5 (5794)
- The Little Book of Hygge: Danish Secrets to Happy LivingD'EverandThe Little Book of Hygge: Danish Secrets to Happy LivingÉvaluation : 3.5 sur 5 étoiles3.5/5 (400)
- Shoe Dog: A Memoir by the Creator of NikeD'EverandShoe Dog: A Memoir by the Creator of NikeÉvaluation : 4.5 sur 5 étoiles4.5/5 (537)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceD'EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceÉvaluation : 4 sur 5 étoiles4/5 (895)
- The Yellow House: A Memoir (2019 National Book Award Winner)D'EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Évaluation : 4 sur 5 étoiles4/5 (98)
- The Emperor of All Maladies: A Biography of CancerD'EverandThe Emperor of All Maladies: A Biography of CancerÉvaluation : 4.5 sur 5 étoiles4.5/5 (271)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryD'EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryÉvaluation : 3.5 sur 5 étoiles3.5/5 (231)
- Never Split the Difference: Negotiating As If Your Life Depended On ItD'EverandNever Split the Difference: Negotiating As If Your Life Depended On ItÉvaluation : 4.5 sur 5 étoiles4.5/5 (838)
- Grit: The Power of Passion and PerseveranceD'EverandGrit: The Power of Passion and PerseveranceÉvaluation : 4 sur 5 étoiles4/5 (588)
- On Fire: The (Burning) Case for a Green New DealD'EverandOn Fire: The (Burning) Case for a Green New DealÉvaluation : 4 sur 5 étoiles4/5 (73)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureD'EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureÉvaluation : 4.5 sur 5 étoiles4.5/5 (474)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaD'EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaÉvaluation : 4.5 sur 5 étoiles4.5/5 (266)
- The Unwinding: An Inner History of the New AmericaD'EverandThe Unwinding: An Inner History of the New AmericaÉvaluation : 4 sur 5 étoiles4/5 (45)
- Team of Rivals: The Political Genius of Abraham LincolnD'EverandTeam of Rivals: The Political Genius of Abraham LincolnÉvaluation : 4.5 sur 5 étoiles4.5/5 (234)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyD'EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyÉvaluation : 3.5 sur 5 étoiles3.5/5 (2259)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreD'EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreÉvaluation : 4 sur 5 étoiles4/5 (1090)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersD'EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersÉvaluation : 4.5 sur 5 étoiles4.5/5 (344)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)D'EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Évaluation : 4.5 sur 5 étoiles4.5/5 (121)
- Her Body and Other Parties: StoriesD'EverandHer Body and Other Parties: StoriesÉvaluation : 4 sur 5 étoiles4/5 (821)
- LRL Rudy Acuna On Neftali DeLeon - I Am Proud To Be The Grandson Son and Husband of Immigrants.Document9 pagesLRL Rudy Acuna On Neftali DeLeon - I Am Proud To Be The Grandson Son and Husband of Immigrants.EditorPas encore d'évaluation
- GrandEsta - Double Eyelid Surgery PDFDocument2 pagesGrandEsta - Double Eyelid Surgery PDFaniyaPas encore d'évaluation
- S.I.M. InnovaDocument51 pagesS.I.M. InnovaPauline Karen ConcepcionPas encore d'évaluation
- English SutffDocument12 pagesEnglish SutffVictor AlmeidaPas encore d'évaluation
- ) Mark Scheme (Results) January 2019: Pearson Edexcel International GCSE in Mathematics A (4MA1) Higher Tier Paper 1HRDocument22 pages) Mark Scheme (Results) January 2019: Pearson Edexcel International GCSE in Mathematics A (4MA1) Higher Tier Paper 1HRNewtonPas encore d'évaluation
- NUR 200 Week 7 Practice Case StudyDocument2 pagesNUR 200 Week 7 Practice Case StudyJB NicolePas encore d'évaluation
- Difference Between C, C++ and JavaDocument3 pagesDifference Between C, C++ and Javasknandish587Pas encore d'évaluation
- mc96 97 01feb - PsDocument182 pagesmc96 97 01feb - PsMohammed Rizwan AliPas encore d'évaluation
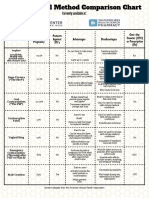
- Birth Control Comparison Chart 2018Document1 pageBirth Control Comparison Chart 2018Eric SandesPas encore d'évaluation
- Leseprobe Aus: "Multilingualism in The Movies" Von Lukas BleichenbacherDocument20 pagesLeseprobe Aus: "Multilingualism in The Movies" Von Lukas BleichenbachernarrverlagPas encore d'évaluation
- Dances in LuzonDocument13 pagesDances in LuzonDenise Michelle AntivoPas encore d'évaluation
- Review of Related LiteratureDocument5 pagesReview of Related LiteratureRJ PareniaPas encore d'évaluation
- Script For Demo TeachingDocument9 pagesScript For Demo TeachingDindz SurioPas encore d'évaluation
- BA BBA Law of Crimes II CRPC SEM IV - 11Document6 pagesBA BBA Law of Crimes II CRPC SEM IV - 11krish bhatia100% (1)
- Year 8 - Higher - Autumn 2019Document16 pagesYear 8 - Higher - Autumn 2019nooraPas encore d'évaluation
- 145class 7 Integers CH 1Document2 pages145class 7 Integers CH 17A04Aditya MayankPas encore d'évaluation
- Robbins Ob14 PPT 11Document27 pagesRobbins Ob14 PPT 11daneshnedaiePas encore d'évaluation
- Guoyin Shen, Ho-Kwang Mao and Russell J. Hemley - Laser-Heated Diamond Anvil Cell Technique: Double-Sided Heating With Multimode Nd:YAG LaserDocument5 pagesGuoyin Shen, Ho-Kwang Mao and Russell J. Hemley - Laser-Heated Diamond Anvil Cell Technique: Double-Sided Heating With Multimode Nd:YAG LaserDeez34PPas encore d'évaluation
- Ipsoot Rating ClarificationsDocument9 pagesIpsoot Rating ClarificationsJerry PanPas encore d'évaluation
- Chapter 6 Coming of SpainDocument4 pagesChapter 6 Coming of SpainJayvee MacapagalPas encore d'évaluation
- Problem-Solution Essay Final DraftDocument4 pagesProblem-Solution Essay Final Draftapi-490864786Pas encore d'évaluation
- Swimming Pool - PWTAG CodeofPractice1.13v5 - 000Document58 pagesSwimming Pool - PWTAG CodeofPractice1.13v5 - 000Vin BdsPas encore d'évaluation
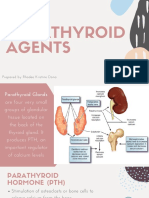
- Parathyroid Agents PDFDocument32 pagesParathyroid Agents PDFRhodee Kristine DoñaPas encore d'évaluation
- FUNCTIONS of LANGUAGE L. HébertDocument7 pagesFUNCTIONS of LANGUAGE L. HébertGonzalo Muniz100% (2)
- Most Common Punctuation Errors Made English and Tefl Majors Najah National University - 0 PDFDocument24 pagesMost Common Punctuation Errors Made English and Tefl Majors Najah National University - 0 PDFDiawara MohamedPas encore d'évaluation
- Wallen Et Al-2006-Australian Occupational Therapy JournalDocument1 pageWallen Et Al-2006-Australian Occupational Therapy Journal胡知行Pas encore d'évaluation
- Letters of ComplaintDocument3 pagesLetters of ComplaintMercedes Jimenez RomanPas encore d'évaluation
- Basic Foundation of Iv TherapyDocument10 pagesBasic Foundation of Iv Therapyjanna mae patriarcaPas encore d'évaluation
- Richards and Wilson Creative TourismDocument15 pagesRichards and Wilson Creative Tourismgrichards1957Pas encore d'évaluation
- Dela Cruz Vs Asian ConsumerDocument5 pagesDela Cruz Vs Asian ConsumerMarion Yves MosonesPas encore d'évaluation