Académique Documents
Professionnel Documents
Culture Documents
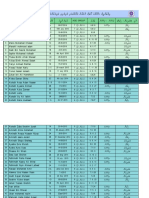
Immunisation Report
Transféré par
alvaro071302Description originale:
Copyright
Formats disponibles
Partager ce document
Partager ou intégrer le document
Avez-vous trouvé ce document utile ?
Ce contenu est-il inapproprié ?
Signaler ce documentDroits d'auteur :
Formats disponibles
Immunisation Report
Transféré par
alvaro071302Droits d'auteur :
Formats disponibles
Live, Attenuated Vaccines
Attenuated vaccines can be made in several different ways. Some of the most common methods involve passing the disease-causing virus through a series of cell cultures or animal embryos (typically chick embryos). Using chick embryos as an example, the virus is grown in different embryos in a series. With each passage, the virus becomes better at replicating in chick cells, but loses its ability to replicate in human cells. A virus targeted for use in a vaccine may be grown throughpassaged through upwards of 200 different embryos or cell cultures. Eventually, the attenuated virus will be unable to replicate well (or at all) in human cells, and can be used in a vaccine. All of the methods that involve passing a virus through a non-human host produce a version of the virus that can still be recognized by the human immune system, but cannot replicate well in a human host.
When the resulting vaccine virus is given to a human, it will be unable to replicate enough to cause illness, but will still provoke an immune response that can protect against future infection.
One concern that must be considered is the potential for the vaccine virus to revert to a form capable of causing disease. Mutations that can occur when the vaccine virus replicates in the body may result in more a virulent strain. This is very unlikely, as the vaccine viruss ability to replicate at all is limited; however, it is taken into consideration when developing an attenuated vaccine. It is worth noting that mutations are somewhat common with the oral polio vaccine (OPV), a live vaccine that is ingested instead of injected. The vaccine virus can mutate into a virulent form and result in rare cases of paralytic polio. For this reason, OPV is no longer used in the United States, and has been replaced on the Recommended Childhood Immunization Schedule by the inactivated polio vaccine (IPV).
Protection from a live, attenuated vaccine typically outlasts that provided by a killed or inactivated vaccine. Killed or Inactivated Vaccines
One alternative to attenuated vaccines is a killed or inactivated vaccine. Vaccines of this type are created by inactivating a pathogen, typically using heat or chemicals such as formaldehyde or formalin. This destroys the pathogens ability to replicate, but keeps it intact so that the immune system can still recognize it. (Inactivated is generally used rather than killed to refer to viral vaccines of this type, as viruses are generally not considered to be alive.)
Because killed or inactivated pathogens cant replicate at all, they cant revert to a more virulent form capable of causing disease (as discussed above with live, attenuated vaccines). However, they tend to provide a shorter length of protection than live vaccines, and are more likely to require boosters to create long-term immunity. Killed or inactivated vaccines on the U.S. Recommended Childhood Immunization Schedule include the inactivated polio vaccine and the seasonal influenza vaccine (in shot form). Toxoids
Some bacterial diseases are not directly caused by a bacterium itself, but by a toxin produced by the bacterium. One example is tetanus: its symptoms are not caused by the Clostridium tetani bacterium, but by a neurotoxin it produces (tetanospasmin). Immunizations for this type of pathogen can be made by inactivating the toxin that causes disease symptoms. As with organisms or viruses used in killed or inactivated vaccines, this can be done via treatment with a chemical such as formalin, or by using heat or other methods.
Immunizations created using inactivated toxins are called toxoids. Toxoids can actually be considered killed or inactivated vaccines, but are sometimes given their own category to highlight the fact that they contain an inactivated toxin, and not an inactivated form of bacteria.
Toxoid immunizations on the U.S. Recommended Childhood Immunization schedule include the tetanus and diphtheria immunizations, which are available in a combined form. Subunit and Conjugate Vaccines
Both subunit and conjugate vaccines contain only pieces of the pathogens they protect against.
Subunit vaccines use only part of a target pathogen to provoke a response from the immune system. This may be done by isolating a specific protein from a pathogen and presenting it as an antigen on its own. The acellular pertussis vaccine and influenza vaccine (in shot form) are examples of subunit vaccines.
Another type of subunit vaccine can be created via genetic engineering. A gene coding for a vaccine protein is inserted into another virus, or into producer cells in culture. When the carrier virus reproduces, or when the producer cell metabolizes, the vaccine protein is also created. The end result of
this approach is a recombinant vaccine: the immune system will recognize the expressed protein and provide future protection against the target virus. The Hepatitis B vaccine currently used in the United States is a recombinant vaccine.
Another vaccine made using genetic engineering is the human papillomavirus (HPV) vaccine. Two types of HPV vaccine are availableone provides protection against two strains of HPV, the other fourbut both are made in the same way: for each strain, a single viral protein is isolated. When these proteins are expressed, virus-like particles (VLPs) are created. These VLPs contain no genetic material from the viruses and cant cause illness, but prompt an immune response that provides future protection against HPV.
Conjugate vaccines are somewhat similar to recombinant vaccines: theyre made using a combination of two different components. Conjugate vaccines, however, are made using pieces from the coats of bacteria. These coats are chemically linked to a carrier protein, and the combination is used as a vaccine. Conjugate vaccines are used to create a more powerful, combined immune response: typically the piece of bacteria being presented would not generate a strong immune response on its own, while the carrier protein would. The piece of bacteria cant cause illness, but combined with a carrier protein, it can generate immunity against future infection. The vaccines currently in use for children against pneumococcal bacterial infections are made using this technique. More Information
Researchers continue to develop new vaccine types and improve current approaches. For more information about experimental vaccines and delivery techniques, see our article The Future of Immunization. Sources
Plotkin SA, Mortimer E. Vaccines. New York: Harper Perennial; 1988.
Plotkin SA, Orenstein WA, Offit PA, eds. Vaccines. Philadelphia: Saunders; 2008.
Last update 27 Jan 2014 Timeline Entry: 1962 Attenuated Measles Vaccine Developed Centers for Disease Control and Prevention Boy with measles Enlarge
Maurice Hilleman and colleagues developed an attenuated measles vaccine by passaging John Enderss measles virus strain over 80 times through different cell types.
The resulting vaccine, Rubeovax, was given with a dose of gamma globulin antibodies to reduce reactions (mainly fever and rash). See This Item In The Timeline Timeline Entry: 7/23/1986 Hepatitis B: Recombinant Vaccine Licensed Courtesy of Lorraine Hilleman Maurice Hilleman watches as his granddaughter receives the recombinant hepatitis B vaccine in 1999. Enlarge
The FDA licensed Mercks Recombivax HB. This hepatitis B vaccine was the first human vaccine produced by recombinant DNA methods.
A challenge in creating the vaccine involved avoiding the use of human blood products, as did Maurice Hillemans first hepatitis B vaccine. Therefore, Merck used an enzyme to remove the viruss surface protein (HBsAg, the Australia antigen). Researchers inserted the code for the antigen into yeast cells, which produced more of the surface protein. The yeast-derived surface protein produced immunity to the hepatitis B virus. See This Item In The doctors office
Vous aimerez peut-être aussi
- Shoe Dog: A Memoir by the Creator of NikeD'EverandShoe Dog: A Memoir by the Creator of NikeÉvaluation : 4.5 sur 5 étoiles4.5/5 (537)
- Albanian DialectsDocument5 pagesAlbanian DialectsMetaleiroPas encore d'évaluation
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeD'EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeÉvaluation : 4 sur 5 étoiles4/5 (5795)
- "A Study On Services Offered by State Bank of India": Final ProjectDocument59 pages"A Study On Services Offered by State Bank of India": Final ProjectShabana KarimPas encore d'évaluation
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceD'EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceÉvaluation : 4 sur 5 étoiles4/5 (895)
- Developing A Business Plan For Your Vet PracticeDocument7 pagesDeveloping A Business Plan For Your Vet PracticeMujtaba AusafPas encore d'évaluation
- The Yellow House: A Memoir (2019 National Book Award Winner)D'EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Évaluation : 4 sur 5 étoiles4/5 (98)
- Hunting the Chimera–the end of O'Reilly v Mackman_ -- Alder, John -- Legal Studies, #2, 13, pages 183-20...hn Wiley and Sons; Cambridge -- 10_1111_j_1748-121x_1993_tb00480_x -- 130f73b26a9d16510be20781ea4d81eb -- Anna’s ArchiveDocument21 pagesHunting the Chimera–the end of O'Reilly v Mackman_ -- Alder, John -- Legal Studies, #2, 13, pages 183-20...hn Wiley and Sons; Cambridge -- 10_1111_j_1748-121x_1993_tb00480_x -- 130f73b26a9d16510be20781ea4d81eb -- Anna’s ArchivePrince KatheweraPas encore d'évaluation
- Grit: The Power of Passion and PerseveranceD'EverandGrit: The Power of Passion and PerseveranceÉvaluation : 4 sur 5 étoiles4/5 (588)
- In-CIV-201 INSPECTION NOTIFICATION Pre-Pouring Concrete WEG Pump Area PedestalsDocument5 pagesIn-CIV-201 INSPECTION NOTIFICATION Pre-Pouring Concrete WEG Pump Area PedestalsPedro PaulinoPas encore d'évaluation
- The Little Book of Hygge: Danish Secrets to Happy LivingD'EverandThe Little Book of Hygge: Danish Secrets to Happy LivingÉvaluation : 3.5 sur 5 étoiles3.5/5 (400)
- BCLTE Points To ReviewDocument4 pagesBCLTE Points To Review•Kat Kat's Lifeu•Pas encore d'évaluation
- The Emperor of All Maladies: A Biography of CancerD'EverandThe Emperor of All Maladies: A Biography of CancerÉvaluation : 4.5 sur 5 étoiles4.5/5 (271)
- Prince Baruri Offer Letter-1Document3 pagesPrince Baruri Offer Letter-1Sukharanjan RoyPas encore d'évaluation
- Never Split the Difference: Negotiating As If Your Life Depended On ItD'EverandNever Split the Difference: Negotiating As If Your Life Depended On ItÉvaluation : 4.5 sur 5 étoiles4.5/5 (838)
- Crime and Punishment Vocabulary 93092Document2 pagesCrime and Punishment Vocabulary 93092Rebeca Alfonso Alabarta50% (4)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyD'EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyÉvaluation : 3.5 sur 5 étoiles3.5/5 (2259)
- Medieval Societies The Central Islamic LDocument2 pagesMedieval Societies The Central Islamic LSk sahidulPas encore d'évaluation
- On Fire: The (Burning) Case for a Green New DealD'EverandOn Fire: The (Burning) Case for a Green New DealÉvaluation : 4 sur 5 étoiles4/5 (74)
- Organizational Behavior: Chapter 6: Understanding Work TeamDocument6 pagesOrganizational Behavior: Chapter 6: Understanding Work TeamCatherinePas encore d'évaluation
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureD'EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureÉvaluation : 4.5 sur 5 étoiles4.5/5 (474)
- DLF New Town Gurgaon Soicety Handbook RulesDocument38 pagesDLF New Town Gurgaon Soicety Handbook RulesShakespeareWallaPas encore d'évaluation
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryD'EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryÉvaluation : 3.5 sur 5 étoiles3.5/5 (231)
- GOUP GO of 8 May 2013 For EM SchoolsDocument8 pagesGOUP GO of 8 May 2013 For EM SchoolsDevendra DamlePas encore d'évaluation
- Team of Rivals: The Political Genius of Abraham LincolnD'EverandTeam of Rivals: The Political Genius of Abraham LincolnÉvaluation : 4.5 sur 5 étoiles4.5/5 (234)
- 5 15 19 Figaro V Our Revolution ComplaintDocument12 pages5 15 19 Figaro V Our Revolution ComplaintBeth BaumannPas encore d'évaluation
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaD'EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaÉvaluation : 4.5 sur 5 étoiles4.5/5 (266)
- rp200 Article Mbembe Society of Enmity PDFDocument14 pagesrp200 Article Mbembe Society of Enmity PDFIdrilPas encore d'évaluation
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersD'EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersÉvaluation : 4.5 sur 5 étoiles4.5/5 (345)
- TDS Rate Chart For Financial Year 2022 23 Assessment Year 2023 24Document9 pagesTDS Rate Chart For Financial Year 2022 23 Assessment Year 2023 24Sumukh TemkarPas encore d'évaluation
- Notes (Part 1) : Accounting Policies, Changes in Estimates and ErrorsDocument13 pagesNotes (Part 1) : Accounting Policies, Changes in Estimates and ErrorsPaula Bautista100% (2)
- The Unwinding: An Inner History of the New AmericaD'EverandThe Unwinding: An Inner History of the New AmericaÉvaluation : 4 sur 5 étoiles4/5 (45)
- 10th Grade SAT Vocabulary ListDocument20 pages10th Grade SAT Vocabulary ListMelissa HuiPas encore d'évaluation
- The History of Land Use and Development in BahrainDocument345 pagesThe History of Land Use and Development in BahrainSogkarimiPas encore d'évaluation
- Specpro.09.Salazar vs. Court of First Instance of Laguna and Rivera, 64 Phil. 785 (1937)Document12 pagesSpecpro.09.Salazar vs. Court of First Instance of Laguna and Rivera, 64 Phil. 785 (1937)John Paul VillaflorPas encore d'évaluation
- Open Quruan 2023 ListDocument6 pagesOpen Quruan 2023 ListMohamed LaamirPas encore d'évaluation
- Loan AgreementDocument6 pagesLoan AgreementSachin ShastriPas encore d'évaluation
- 6 Chase Nat'l Bank of New York V BattatDocument2 pages6 Chase Nat'l Bank of New York V BattatrPas encore d'évaluation
- Glories of Srimad Bhagavatam - Bhaktivedanta VidyapithaDocument7 pagesGlories of Srimad Bhagavatam - Bhaktivedanta VidyapithaPrajot NairPas encore d'évaluation
- .. Anadolu Teknik, Teknik Lise Ve Endüstri Meslek LisesiDocument3 pages.. Anadolu Teknik, Teknik Lise Ve Endüstri Meslek LisesiLislePas encore d'évaluation
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreD'EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreÉvaluation : 4 sur 5 étoiles4/5 (1090)
- Types of Business LettersDocument11 pagesTypes of Business LettersernewstPas encore d'évaluation
- (MX) Public Figures, Private LivesDocument3 pages(MX) Public Figures, Private LivesbestatemanPas encore d'évaluation
- Beowulf Essay 1Document6 pagesBeowulf Essay 1api-496952332Pas encore d'évaluation
- Retirement SpeechDocument11 pagesRetirement SpeechRayan Castro100% (1)
- Daniel Salazar - PERSUASIVE ESSAYDocument2 pagesDaniel Salazar - PERSUASIVE ESSAYDaniel SalazarPas encore d'évaluation
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)D'EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Évaluation : 4.5 sur 5 étoiles4.5/5 (121)
- Turnaround ManagementDocument16 pagesTurnaround Managementpaisa321Pas encore d'évaluation
- Her Body and Other Parties: StoriesD'EverandHer Body and Other Parties: StoriesÉvaluation : 4 sur 5 étoiles4/5 (821)