Académique Documents
Professionnel Documents
Culture Documents
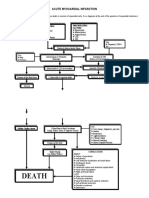
Pathophysiology Worksheet MI
Transféré par
pjbedelCopyright
Formats disponibles
Partager ce document
Partager ou intégrer le document
Avez-vous trouvé ce document utile ?
Ce contenu est-il inapproprié ?
Signaler ce documentDroits d'auteur :
Formats disponibles
Pathophysiology Worksheet MI
Transféré par
pjbedelDroits d'auteur :
Formats disponibles
Pathophysiology Worksheet
1. Disease (s): MI
2. Pathophysiology: (the disturbance of normal mechanical, physical, and biochemical functions, either caused by a
disease, or resulting from a disease or abnormal syndrome, or condition that may not qualify to be called a disease. Exactly what is the disease changing in the body?)
Most myocardial infarctions are caused by a disruption in the vascular endothelium associated with an unstable atherosclerotic plaque that stimulates the formation of an intracoronary thrombus, which results in coronary artery blood flow occlusion. If such an occlusion persists for more than 20 minutes, irreversible myocardial cell damage and cell death will occur. The development of atherosclerotic plaque occurs over a period of years to decades. The two primary characteristics of the clinically symptomatic atherosclerotic plaque are a fibromuscular cap and an underlying lipid-rich core. Plaque erosion can occur because of the actions of matrix metalloproteases and the release of other collagenases and proteases in the plaque, which result in thinning of the overlying fibromuscular cap. The action of proteases, in addition to hemodynamic forces applied to the arterial segment, can lead to a disruption of the endothelium and fissuring or rupture of the fibromuscular cap. The loss of structural stability of a plaque often occurs at the juncture of the fibromuscular cap and the vessel wall, a site otherwise known as the shoulder region. Disruption of the endothelial surface can cause the formation of thrombus via platelet-mediated activation of the coagulation cascade. If a thrombus is large enough to occlude coronary blood flow, an MI can result. The death of myocardial cells first occurs in the area of myocardium most distal to the arterial blood supply: the endocardium. As the duration of the occlusion increases, the area of myocardial cell death enlarges, extending from the endocardium to the myocardium and ultimately to the epicardium. The area of myocardial cell death then spreads laterally to areas of watershed or collateral perfusion. Generally, after a 6- to 8-hour period of coronary occlusion, most of the distal myocardium has died. The extent of myocardial cell death defines the magnitude of the MI. If blood flow can be restored to at-risk myocardium, more heart muscle can be saved from irreversible damage or death. The severity of an MI depends on three factors: the level of the occlusion in the coronary artery, the length of time of the occlusion, and the presence or absence of collateral circulation. Generally, the more proximal the coronary occlusion, the more extensive the amount of myocardium that will be at risk of necrosis. The larger the myocardial infarction, the greater the chance of death because of a mechanical complication or pump failure. The longer the period of vessel occlusion, the greater the chances of irreversible myocardial damage distal to the occlusion. STEMI is usually the result of complete coronary occlusion after plaque rupture. This arises most often from a plaque that previously caused less than 50% occlusion of the lumen. NSTEMI is usually associated with greater plaque burden without complete occlusion. This difference contributes to the increased early mortality seen in STEMI and the eventual equalization of mortality between STEMI and NSTEMI after 1 year.
3. Signs and Symptoms: (highlight those S&S exhibited by your client)
The onset of symptoms in myocardial infarction (MI) is usually gradual, over several minutes, and rarely instantaneous. Chest pain is the most common symptom of acute myocardial infarction and is often described as a sensation of tightness, pressure, or squeezing. Chest pain due to ischemia (a lack of blood and hence oxygen supply) of the heart muscle is termed angina pectoris. Pain radiates most often to the left arm, but may also radiate to the lower jaw, neck, right arm, and epigastrium, where it may mimic heartburn. Shortness of breath, diaphoresis, weakness, light-headedness, nausea, vomiting, and palpitations. MI in women include dyspnea (shortness of breath), weakness, and fatigue. Fatigue, sleep disturbances, and dyspnea have been reported as frequently occurring symptoms which may manifest as long as one month before the actual clinically manifested ischemic event. In women, chest pain may be less predictive of coronary ischemia than in men. Approximately one fourth of all myocardial infarctions are silent, without chest pain or other symptoms.
4. Diagnostics to confirm disease: Troponin I lab test, ECG (ST segment elevation)
5. Recommended Treatment: Antiplatelet meds, O2, nitrates, pain control meds, beta blockers, ace inhibitors, PCI & CABG 6. Nursing Assessments:
Assess chest, jaw, arm and epigastric pain. Assess SOB, HR, diaphoresis, clammy skin, dizziness, N/V, and confusion. Assess RR and heart sounds.
7. Nursing Interventions: Provide oxygen, monitor ECG 12 lead, give meds per physicians orders, monitor CP, monitor VS frequently
Vous aimerez peut-être aussi
- Obesity and Risk FactorDocument61 pagesObesity and Risk FactorSaad MotawéaPas encore d'évaluation
- Blank Welding Procedure Spec.Document1 pageBlank Welding Procedure Spec.pjbedelPas encore d'évaluation
- Angiogenesis and Direct Myocardial RevascularizationDocument364 pagesAngiogenesis and Direct Myocardial RevascularizationPerdana SidaurukPas encore d'évaluation
- Acute Myocardial InfarctionDocument14 pagesAcute Myocardial InfarctionJardee DatsimaPas encore d'évaluation
- Interpretation of Coronary Angiograms (ICOADocument110 pagesInterpretation of Coronary Angiograms (ICOAKelly YeowPas encore d'évaluation
- HyperlipidemiaDocument10 pagesHyperlipidemiaapi-345356257100% (1)
- NP3 4Document65 pagesNP3 4Edward Nicko GarciaPas encore d'évaluation
- Chronic GlomerulonephritisDocument8 pagesChronic GlomerulonephritisDaniel CornerPas encore d'évaluation
- Hemorrhagic Cerebro Vascular DiseaseDocument37 pagesHemorrhagic Cerebro Vascular Diseasejbvaldez100% (1)
- The Pathophysiology and Pharmacotherapy of Myocardial InfarctionD'EverandThe Pathophysiology and Pharmacotherapy of Myocardial InfarctionNabil El-SherifPas encore d'évaluation
- AWS D1-1 PQR-WPS Yes Pre QualifiedDocument2 pagesAWS D1-1 PQR-WPS Yes Pre QualifiedJRodengineerPas encore d'évaluation
- Myocardial Infarction Guide: Causes, Symptoms & TreatmentDocument28 pagesMyocardial Infarction Guide: Causes, Symptoms & Treatmentshaitabligan100% (1)
- Congestive Heart Failure PathophysiologyDocument16 pagesCongestive Heart Failure PathophysiologyDale LaurentePas encore d'évaluation
- Transdermal Delivery of Drugs ReviewDocument17 pagesTransdermal Delivery of Drugs ReviewRitha PratiwiPas encore d'évaluation
- Myocardial Infarction: Symptoms, Diagnosis, and ManagementDocument2 pagesMyocardial Infarction: Symptoms, Diagnosis, and ManagementChris T NaPas encore d'évaluation
- Intracerebral HemorrageDocument13 pagesIntracerebral HemorrageChristian JuarezPas encore d'évaluation
- Myocardial InfarctionDocument21 pagesMyocardial Infarctionanon_516349434Pas encore d'évaluation
- Nursing Management of CAD and ACSDocument9 pagesNursing Management of CAD and ACSfriendofnurse100% (4)
- Drug Study On Emergency DrugsDocument14 pagesDrug Study On Emergency DrugsRene John FranciscoPas encore d'évaluation
- WPS D1.3-2012 BlankDocument1 pageWPS D1.3-2012 BlankpjbedelPas encore d'évaluation
- Acute Glumerulo NephritisDocument13 pagesAcute Glumerulo NephritisNathan Vince CruzPas encore d'évaluation
- Asking Your Question (PICO) - NursingDocument5 pagesAsking Your Question (PICO) - NursingBentaigaPas encore d'évaluation
- Acute Coronary SyndromeDocument9 pagesAcute Coronary Syndromekimchi girlPas encore d'évaluation
- Right-Sided Heart FailureDocument4 pagesRight-Sided Heart FailureKhalid Mahmud ArifinPas encore d'évaluation
- Beta Blockers and Other Sympatholytic AgentsDocument43 pagesBeta Blockers and Other Sympatholytic AgentsAriel OlshevskyPas encore d'évaluation
- Pulmonary EmbolismDocument5 pagesPulmonary EmbolismNica Duco100% (2)
- Acute Myocardial InfarctionDocument32 pagesAcute Myocardial InfarctionListya Normalita100% (1)
- Community Acquired Pneumonia, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsD'EverandCommunity Acquired Pneumonia, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsPas encore d'évaluation
- Nursing Care Plan For Pulmonary Edema PDFDocument2 pagesNursing Care Plan For Pulmonary Edema PDFAsmaa100% (1)
- BFCDocument8 pagesBFCIrene GunongPas encore d'évaluation
- Myocardial InfarctionDocument18 pagesMyocardial InfarctionYanna Habib-MangotaraPas encore d'évaluation
- Myocarditis, (Inflamed Heart Muscles) A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsD'EverandMyocarditis, (Inflamed Heart Muscles) A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsPas encore d'évaluation
- Pathophy - Nephrotic SyndromeedDocument1 pagePathophy - Nephrotic Syndromeedianecunar100% (1)
- Left-Sided Heart FailureDocument3 pagesLeft-Sided Heart FailureKhalid Mahmud ArifinPas encore d'évaluation
- Prof Ad Day 1Document136 pagesProf Ad Day 1Kareen ArnaizPas encore d'évaluation
- Pathophysiology of ArrhythmiasDocument15 pagesPathophysiology of ArrhythmiasJonathan MontecilloPas encore d'évaluation
- NCP-Case Presentation (CHF)Document4 pagesNCP-Case Presentation (CHF)Jessamine EnriquezPas encore d'évaluation
- Discharge PlanDocument1 pageDischarge PlanKamille Bianca Macapagal ÜPas encore d'évaluation
- Acs Nstemi Vs Ua - PathoDocument2 pagesAcs Nstemi Vs Ua - PathoJerom YamatPas encore d'évaluation
- Examining root causes of poor health and diseaseDocument1 pageExamining root causes of poor health and diseaseDONITA DALUMPINESPas encore d'évaluation
- Multiple Organ Dysfunction Syndrome: Contemporary Insights On The Clinicopathological SpectrumDocument16 pagesMultiple Organ Dysfunction Syndrome: Contemporary Insights On The Clinicopathological SpectrumNurul Kamilah SadliPas encore d'évaluation
- End Stage Renal DiseaseDocument9 pagesEnd Stage Renal DiseaseShantanu DixitPas encore d'évaluation
- Pathophysiology (Risk Factors & Symptoms)Document20 pagesPathophysiology (Risk Factors & Symptoms)Ann Michelle TarrobagoPas encore d'évaluation
- Myocardial InfarctionDocument15 pagesMyocardial InfarctionameerPas encore d'évaluation
- Congenital Hypothyroidism Follow Up of A Case For 13 Years PDFDocument14 pagesCongenital Hypothyroidism Follow Up of A Case For 13 Years PDFMeutia sariPas encore d'évaluation
- Aneurysm PDFDocument20 pagesAneurysm PDFKV100% (1)
- Medical Management For PneumoniaDocument2 pagesMedical Management For PneumoniaSue Elaine100% (1)
- Cardiomyopathy Dilated CardiomyopathyDocument5 pagesCardiomyopathy Dilated Cardiomyopathym3d1k100% (1)
- NursingCare PlanDocument8 pagesNursingCare PlanSunSearra Kennedy RuffinPas encore d'évaluation
- Drug Study CovidDocument5 pagesDrug Study CovidR Hornilla Arcega0% (1)
- Impact of Pandemic To The Psychological Aspects of Nursing StudentsDocument25 pagesImpact of Pandemic To The Psychological Aspects of Nursing StudentsBrandon AretePas encore d'évaluation
- Myocardial Infarction Risk Factors and ComplicationsDocument4 pagesMyocardial Infarction Risk Factors and ComplicationsHearty ArriolaPas encore d'évaluation
- Acute Myocardial InfarctionDocument2 pagesAcute Myocardial InfarctionhailleyannPas encore d'évaluation
- Rheumatic Heart Disease IntroDocument3 pagesRheumatic Heart Disease IntroTrexy LozanoPas encore d'évaluation
- Buerger's DiseaseDocument13 pagesBuerger's DiseaseJoan JuradoPas encore d'évaluation
- EPIGLOTTITISDocument9 pagesEPIGLOTTITISanon_944507650Pas encore d'évaluation
- Hypertensive Cardiovascular Disease Also Known As Hypertensive Heart Disease Occurs Due To The Complication of Hypertension or High Blood PressureDocument3 pagesHypertensive Cardiovascular Disease Also Known As Hypertensive Heart Disease Occurs Due To The Complication of Hypertension or High Blood Pressurejoanneceline16Pas encore d'évaluation
- Buerger DiseaseDocument3 pagesBuerger DiseaseElmer DizonPas encore d'évaluation
- Rheumatic Heart Disease and Fever ExplainedDocument2 pagesRheumatic Heart Disease and Fever ExplainedDiaz RahmadiPas encore d'évaluation
- Case Study ReportDocument23 pagesCase Study Reportapi-290866384Pas encore d'évaluation
- Myocardial InfarctionDocument25 pagesMyocardial Infarctionfam111222Pas encore d'évaluation
- Pathophysiology of Angina PectorisDocument2 pagesPathophysiology of Angina PectorisLeroy LoyPas encore d'évaluation
- Human Diseases Case Study 18 ADocument4 pagesHuman Diseases Case Study 18 Aairickann100% (1)
- Tetralogy of FallotDocument33 pagesTetralogy of FallotjeenaejyPas encore d'évaluation
- ThrombocytopeniaDocument2 pagesThrombocytopeniaNeoMedica100% (1)
- Approach To The Diagnosis and Therapy of Lower Extremity Deep Vein ThrombosisDocument14 pagesApproach To The Diagnosis and Therapy of Lower Extremity Deep Vein ThrombosisWidi HadianPas encore d'évaluation
- Hypovolemic ShockDocument13 pagesHypovolemic ShockJed ProwellPas encore d'évaluation
- PT EducationDocument4 pagesPT Educationapi-248017509Pas encore d'évaluation
- Hyperosmolar Hyperglycemic State (HHS)Document21 pagesHyperosmolar Hyperglycemic State (HHS)Malueth AnguiPas encore d'évaluation
- Case Presentation GeriatricDocument35 pagesCase Presentation GeriatricNurdina AfiniPas encore d'évaluation
- AnsimarDocument2 pagesAnsimarcop_perPas encore d'évaluation
- Philippine Nursing Law of 2002 Ra # 9173Document15 pagesPhilippine Nursing Law of 2002 Ra # 9173Michael Maunda AmpuanPas encore d'évaluation
- Final Case StudyDocument13 pagesFinal Case StudyJen Gacula OsinPas encore d'évaluation
- WQTRD18 3Document1 pageWQTRD18 3pjbedelPas encore d'évaluation
- WPS D9.1Document1 pageWPS D9.1pjbedelPas encore d'évaluation
- 3 Patient AssessmentDocument499 pages3 Patient AssessmentRaul GascueñaPas encore d'évaluation
- Chest Pain Causes GuideDocument4 pagesChest Pain Causes Guidertishaii18Pas encore d'évaluation
- PBL 1 Chest PainDocument3 pagesPBL 1 Chest PainHo Yong WaiPas encore d'évaluation
- Drug StudyDocument3 pagesDrug Studyanon_11638632Pas encore d'évaluation
- Cardiovascular EmergenciesDocument2 pagesCardiovascular EmergenciesAli AbdullahiPas encore d'évaluation
- AtarDocument6 pagesAtarAnonymous Ga9KnnGPas encore d'évaluation
- ArginineDocument9 pagesArginine1976gt500Pas encore d'évaluation
- RC Handout: Passage 1Document7 pagesRC Handout: Passage 1charu2802Pas encore d'évaluation
- Care Plan 5Document13 pagesCare Plan 5مالك مناصرةPas encore d'évaluation
- Chinese MedicinesDocument19 pagesChinese Medicinesjuanitos111Pas encore d'évaluation
- STEMIDocument34 pagesSTEMIefendiPas encore d'évaluation
- Pharmacological Management of Ischaemic Heart DiseaseDocument50 pagesPharmacological Management of Ischaemic Heart DiseaseMuh Akbar BaharPas encore d'évaluation
- Uworld JournalDocument3 pagesUworld JournalJayPas encore d'évaluation
- Comparative Study of Serum and Biliary Lipid Profile in Libyan Gallstone PatientsDocument54 pagesComparative Study of Serum and Biliary Lipid Profile in Libyan Gallstone PatientsJagannadha Rao PeelaPas encore d'évaluation
- Advanced Cardiovascular Life Support (Acls)Document45 pagesAdvanced Cardiovascular Life Support (Acls)Erinne DefrianiPas encore d'évaluation
- Antianginal Student222Document69 pagesAntianginal Student222MoonAIRPas encore d'évaluation
- Drugs of FinalDocument85 pagesDrugs of FinalIbrahim AbueltaifPas encore d'évaluation
- Random Drug StudyDocument94 pagesRandom Drug Studykonzen456Pas encore d'évaluation
- Biggest Loser RegistrationDocument2 pagesBiggest Loser RegistrationDawn BrennanPas encore d'évaluation
- Research Poster PresentationDocument1 pageResearch Poster Presentationapi-328441669Pas encore d'évaluation