Académique Documents
Professionnel Documents
Culture Documents
διπολική διαταραχή και καταθλιψη
Transféré par
Eleni Tzanaki-ArnaoutakiCopyright
Formats disponibles
Partager ce document
Partager ou intégrer le document
Avez-vous trouvé ce document utile ?
Ce contenu est-il inapproprié ?
Signaler ce documentDroits d'auteur :
Formats disponibles
διπολική διαταραχή και καταθλιψη
Transféré par
Eleni Tzanaki-ArnaoutakiDroits d'auteur :
Formats disponibles
The case study of Susie: Dipolar 1 Disorder Case Study Susie is a 20-year-old sophomore at a small Midwestern college.
For the past five days she has gone without any sleep whatsoever and she has spent this time in a heightened state of activity which she herself describes as out of control. For the most part, her behavior is characterized by strange and grandiose ideas that often take on a mystical or sexual tone. For example, she recently proclaimed to a group of friends that she did not menstruate because she was a of a third sex, a gender above the human sexes. When her friends questioned her on this, she explained that she is a superwoman who can avoid human sexuality and still give birth. That is, she is a woman who does not require sex to fulfill her place on earth. Some of Susies bizarre thinking centers on the political, such as believing that she had somehow switched souls with the senior senator from her state. From what she believed were his thoughts and memories, she developed six theories of government that would allow her to single-handedly save the world from nuclear destruction. She went around campus, explaining these theories to friends and even to her professors and began to campaign for an elected position in the U.S. government (even though no elections were scheduled at the time). She feels that her recent experiences with switching souls with the senator would make her particularly well suited for a high position in government; perhaps even the presidency. Susie often worries that she will forget some of her thoughts and has begun writing notes to herself everywhere; in her notebooks, on her computer---even on the walls of her dormitory. Susies family and friends, who have always known her to be extremely tidy and organized, have been shocked to find her room in total disarray with frantic and incoherent messages written all over the walls and furniture. These messages reflect her disorganized, grandiose thinking about spiritual and sexual themes. Susie has experienced two previous episodes of wild and bizarre behavior similar to what she is experiencing now; both alternated with periods of intense depression. When she was in the depressed state, she could not bring herself to attend classes or any campus activities; she suffered from insomnia, poor appetite, and difficulty concentrating. At the lowest points of the depressive side of her disorder, Susie contemplated suicide.
Some background information; Susie grew up on what she terms a traditional Irish home with overprotective and demanding parents. Of the five children in her family, she was the one who always obeyed her parents and played the role of the good girl of the family, a role she describes as being Little Miss Perfect. Susie describes herself as being quite dependent on her parents, who treated her as if she were much younger than she actually was. In contrast to their passive obedience, Susie describes her siblings as rebellious. For example, her older sister told her parents that she was sexually active in high school. Susie describes her parents as exceptionally strict with respect to sexual matters; they never discussed issues related to sex except to make it clear that their children were to remain virgins until they were married. Throughout high school, Susies mother forbade her to wear makeup. She remembers being shocked and frightened when she began menstruating; she was very distressed at the loss of control that this entailed. Susie never dated in high school and has never had a steady boyfriend. Susies family history shows evidence of mood disorders; her maternal grandfather received electroconvulsive therapy (ECT) for depression and her fathers aunt was diagnosed with depression when she went through menopause. Bipolar Disorder The first step is to determine what form of bipolar that Susie is suffering from so that she can receive the proper treatment. The National Institute of Mental Health (NIMH) lists the four types of bipolar disorder in the Diagnostic and Statistical Manual of Mental Disorders (DSM-IV). These four types are bipolar I, bipolar II, bipolar not otherwise specified (BP-NOS), and cyclothymic disorder. Bipolar one includes symptoms of extreme mania, intense depression, or a mixture of the two that lasts a minimum of seven days. An acute bout of mania that requires immediate treatment in a hospital or mental health institution is another way to help a psychologist determine that the patient should be categorized as bipolar I. This mania or depression must be behavior that deviates from the persons normal behavior (NIMH, 2008). Something worth noting is that these episodes of mania and depression have been associated with mild or severe psychotic episodes (Appalachian State University, n.d). Bipolar II is usually diagnosed when a person switches back and forth between mildly manic (also referred to hypomania) and depressive episodes. In the bipolar II type there are not any mixed episodes nor does the person go into an extreme mania state. BP-NOS is considered when a person is displaying behavior out of the realm of what is normal for them but that does not meet the all of
the symptoms of either bipolar I or II. Cyclothymic disorder is merely a moderate form of bipolar that includes symptoms of hypomania and depression which switch back and forth over a period of two years or more, but not to the extremes that would place them in category I, II, or not otherwise specified. (NIMH, 2008). Susie is clearly displaying symptoms of bipolar I disorder. She believes that she is a superwoman who does not need a male to help her reproduce, therefore having no need for menstruation. She also believes that she was able to switch souls with a senator making her more than eligible for a position within the U.S. government. Finally, she is campaigning for an election that is not even taking place at the time. This all points to psychotic episodes, which is a symptom only present in the bipolar I category. She is displaying mania by writing all over her things and making notes to herself on her computer. In addition, she has deviated from her natural behavior which is evident through her disorganization. This is not Susies first episode of mania and in the past her mania was followed by a deep depression that even led her to suicidal thoughts. Genetics/Familial Traits Studies show that there is a clear link between genetics and bipolar disorder but have been unable to identify exactly what the abnormality is. There have been numerous studies on monozygotic (MZ) twins, first generation relatives (i.e. mothers, fathers, sisters, and brothers), and unrelated people. All studies dealing with family and those who suffer from a bipolar disorder show that the closer the genetic ties the more prevalent bipolar is in those studied. The chances of two people selected at random to have a propensity of bipolar is around only 1 percent, first generation relatives show about a 10 percent chance, and it is about 60% more likely for both monozygotic twins to develop bipolar disorder (Caddock & Jones, 1999). This rate of 60 percent is the highest known rate between those related to share the same genetic disorder (Durand & Barlow, 2007). There have also been links to family members who have other disorders such as manic depression and obsessive-compulsive disorder (NIMH, 2008). There have been many studies regarding what specific genetic dysfunction could cause people who are closely related to suffer from the same illness. Different studies have found links between various chromosomal abnormalities in related individuals. Several chromosomes in different studies have proven to be the culprit but no test has been able to be duplicated, which needs to occur before a definite link can be established. More recent studies have made use of DNA and the placement of markers to find a link but none have had successful duplicated results as of yet (Caddock & Jones, 1999).
In Susies case, as far as we know she is not a twin and none of her first generation relatives have bipolar disorder. However, she does have relatives on both the maternal and paternal sides of her family that have been treated for depression. The relatives were both second generation relatives (i.e. grandparent, aunt, uncle). The age at which her family members were diagnosed with depression is unclear, although it can be assumed that since it was during menopause that her aunt was in the later stages of her life. Susie is only twenty, so the genetic ties are not as clear in this case, but they do exist. Brain Abnormalities McLean hospital is associated with Harvard University. They dedicate a lot of time on researching brain abnormalities in people with bipolar disorder and schizophrenia. Their research team has found that during sleep there are many similar brain patterns in people who suffer from bipolar disorder and those who do not. They have also discovered that there are slight differences as well and are dedicated to discovering the cause of these. The McLean research team has found powerful differences in default mode special extent between their test subjects with bipolar disorder and their control group. These differences have been found during analysis of the whole brain on single patients discovered on parasagittal, cornal, and axial slices of the brain (McLean Hospital, 2011). As Susies psychologist, I would strongly suggest that she participate with the McLean hospitals for these studies while she is in the mania stage of the bipolar. I think that the best result in the study of brain abnormalities could come from studies done on a person exhibiting psychotic episodes. This could potentially lead to a breakthrough in the study of brain abnormalities in bipolar patients and even find a way to treat Susies symptoms quickly. Neurotransmitters It has been thought that the etiology of mood disorders such as bipolar disorder is the result of malfunctions in the neurotransmitters. If this were to be the case then the most likely candidates for problems are the norepinephrine (NE), serotonine (5-HT), dopamine, and gamma-aminobutyric acid (GABA) neurotransmitters. Generally, NE, 5-HT, and dopamine have been fingered in single cause models of theory. Most recently, GABA has been hypothesized to be part of multi-causal neurotransmitter theories (Appalachian State University, n.d.). Norepinephrine (NE) is responsible for a persons anxiety, arousal, and memory. In early studies it was thought that a deficit of NE would cause depression whereas a surplus could be contributed to manic episodes. Serotonine (5-HT) is accountable for a persons sexual desire, sleeping patterns, moods, appetite, and activity. A lack of 5-HT can cause a person be more apt for mood disorders such as
bipolar disorder. Dopamine is attributed to thought processes, body movements, and levels of hormones. Studies have shown that escalated dopamine neurotransmitters are responsible for the psychotic episodes associated with mania and that a deficiency of dopamine can cause depression. However, dopamine does not account for mania that doesnt include psychotic episodes (Appalachian State University, n.d.). Gammaaminobutyric acid (GABA) is a neurotransmitter that inhibits synaptic communication between neurons (Durand & Barlow, 1999). Low levels of GABA have been linked to both depression and mania, suggesting that GABA is needed for necessary neurotransmitters such as NE, 5-HT, and dopamine to be distributed to neurons successfully (Appalachian State University, n.d.) In a single model theory, Susie might suffer from an increase in dopamine since her symptoms include mania in conjunction with psychotic episodes. However, in the multi-neurotransmitter theory, the problem can be explained with several different neurotransmitters and as a result of low GABA levels. As her psychologist, it would be wise to suggest that she have blood tests taken to see if she is suffering from increased or decreased levels of any of these neurotransmitters so that the proper medication can be prescribed to her. Remedies/Medical Treatments Bipolar disorder is a life altering illness. It is not curable and those who suffer from it will suffer mania and depression several times throughout their lives. The best course of action for treatment is a proper medication and psychotherapy. These treatments are needed for a person with bipolar disorder from the time they are diagnosed throughout the remainder of their life. Mood stabilizing medications are the best course of action and include lithium (treats mania), depakote (treats mania), lamictal (for maintenance of the symptoms of bipolar disorder), and neurontin, topamax, and trileptal (all are anticonvulsant medications) (NIMH, 2008). Antipsychotic medications are also sometimes prescribed to treat bipolar disorder, although they are usually prescribed in conjunction of other medications. Olanzapine and Aripiprazole are often prescribed together with an antidepressant to help relieve symptoms of severe mania, psychosis, or a mixed episode (NIMH, 2008). Seroquel is used to treat the symptoms of sudden manic episodes and became the first antipsychotic to receive FDA approval for treating bipolar depressive episodes in 2006 (NIMH, 2008). Antidepressants such as Prozac, Paxil, Zoloft, and Wellbutrin are often prescribed to treat the symptoms of depression which occur those with bipolar disorder. Patients who take these antidepressants usually take a mood stabilizer, as well, which works to prevent the risk of switching to mania or hypomania or of developing symptoms which cycle rapidly (NIMH, 2008).
As a psychologist and taking into account Susies diagnosis of Bipolar I, her family history, and the seriousness of her symptoms, I would recommend a threepronged approach to treating her disorder. I believe that regular psychotherapy in combination with an antipsychotic such as Seroquel and a mood-stabilizer such as Lithium may make up an effective treatment. I would not start her on an antidepressant as a recent large-scale study has shown that for many people adding antidepressants to mood-stabilizers is no more effective than treating with only the mood-stabilizer (NIMH, 2008). If, after some time, Susie does not respond satisfactorily to the regiment, an antidepressant such as Prozac can be added to the mix. Conclusion As Susies case has demonstrated, bipolar disorder can affect a persons mood and cause changes in their behavior. These ups and downs can be very distracting and counterproductive to living a normal life. Many believe that bipolar disorder is overdiagnosed and is often used as a catch-all diagnosis for people with mood disorders. While this may be true, it is also true that many people do suffer from true bipolar disorder and many of those are undiagnosed and untreated. While there is no cure for the disorder, thorough investigation of the patients symptoms and family history along with proper treatment, including psychotherapy and prescription medications, can lead to successful management of manic and depressive episodes and the ability for the patient to live a normal life. As with most other psychological disorders, there is much to learn about the causes and most effective methods of treating bipolar disorder. However, research continues and the treatments for the disorder are continually being refined. : http://criminologyjust.blogspot.gr/2011/08/case-study-of-susie-bipolar-i-disorder.html _ by Tabetha Cooper
References Appalachian State University. (n.d.). Diagnostic Criteria: Bipolar I Disorder. Retrieved from: http://www1.appstate.edu/~hillrw/BipolarNeuro/BiPolar/pages/type1.ht ml Appalachian State University. (n.d.). Neurochemical Causal Model. Retrieved from: http://www1.appstate.edu/~hillrw/BipolarNeuro/BiPolar/pages/neuropat hology.html
Caddock, N., & Jones, I. (1999). Genetics of bipolar disorder. Retrieved from: http://www.ncbi.nlm.nih.gov/pmc/articles/PMC1762980/pdf/v036p0058 5.pdf Durand & Barlow. (2007). Essentials of abnormal psychology. Cengage Learning. Mason, Ohio. McLean Hospital. (2011). Clinical unit base research: schizophrenia and biplar disorder program.Retrieved from: http://www.mclean.harvard.edu/research/clinicalunit/sbdp.php National Institute of Mental Health. (2008). Bipolar Disorder. Retrieved from: http://www.nimh.nih.gov/health/publications/bipolar-disorder/completeindex.shtml
Major Depressive Disorder in Adolescence: a case study
Deepa Sekhar, Biomed 278 11/14/00
Lynda is a 16 year-old, white female admitted to Bradley Hospital on 10/3/00 because of active suicidal ideations manifested by holding a knife to her arm that morning. This was accompanied by thoughts of hanging herself by wrapping a telephone cord around her neck. Lynda has a history of suicidal ideation and has tried to cut herself in the past, but reported that the knife would not penetrate her skin. She was concerned that she would not be able to stop herself again. In 1994, suicide among prepubertal children and young adolescents (5-14 years) in the United States involved approximately 322 deaths, and suicide among adolescents (15-24 years) involved approximately 4956 deaths. Thus, the risk of suicide rises substantially at puberty (1). Suicidal behavior is strongly associated with major depressive disorder or dysthymia, disruptive disorder, oppositional defiant disorder, conduct disorder, schizophrenia and developmental disorder. There is also a strong correlation between substance abuse and suicide among adolescents, but in this case, Lynda denied any substance abuse history (1). Lynda reported depression for the past 2 years and an obsession with death since 8 th grade. She is an obese female who appeared sad, making poor eye contact and demonstrating poor social skills. Her affect was flat and apathetic. Lynda reported difficulty sleeping, decreased energy, irritable mood and trouble with her appetite. She also reported significant feelings of worthlessness, helplessness and hopelessness. These include five of the symptoms which must be present during at least a 2-week period to diagnose a major depressive episode (2). Major depressive disorder (MDD) is estimated to have a prevalence of 2% in children and 4-8% in adolescents. Though it presents in equal numbers in males and females in childhood, the male:female ratio is 1:2 in adolescence (3). MDD is frequently comorbid with dsythymic disorder (DD), a state of chronic depression which occurs for more of the day, or more days than not, in children for at least 1 year (3). This is significant because
if DD occurs before 21 years of age (early onset), an individual is more likely to develop subsequent major depressive episodes (2). In addition to the above symptoms, Lynda spoke about her imaginary friends, which she has had since 6 years of age. The characters are from television and movies, and she acts out their voices and argues with them. She recognizes that they are not real, but she will avoid her friends to spend time with her imaginary ones. She reported one auditory hallucination, a week before her admission, as a voice telling her to get out of bed to feel better. These symptoms suggest psychotic depression, which is MDD accompanied by mood congruent or incongruent hallucinations. In adolescence these may be auditory hallucinations and delusions. Patients presenting with psychotic depression typically have more severe depression, greater long-term morbidity, increased resistance to antidepressant monotherapy, low placebo response, increased risk of developing bipolar disorder, and a family history of bipolar and psychotic depression (3). Environmental factors are also linked to MDD (3). Lynda related that her depression had worsened in the past 2 weeks because her sister was living at home again. Her sister is abusive towards her (she started choking Lynda for using her television), and Lynda believes her mother does not punish her sister appropriately. Lyndas parents are divorced. Her mother is a victim of domestic violence, and her father is an alcoholic. Also, her aunt is in an institution, and her cousin has tried to commit suicide. Children with at least one depressed parent have a three times greater risk of development of MDD, compared with a child with non-depressed parents. Parents of depressed children also tend to have higher rates of other psychiatric disorders such as anxiety, substance use and personality disorders (3). There is a prevalence of 30-50% of depression in first-degree relatives of depressed children (3). Lynda was diagnosed at Bradley hospital with Axis I: Major Depressive Disorder Recurrent Severe with Psychotic Features and Axis V: GAF current 35 (highest in the past year 75). Axis II was not mentioned, but a learning disability was noted in her chart. She has asthma for which she takes albuterol, but this was not significant for classification under Axis III. Finally, though it was not mentioned, I believe she has several psychosocial and environmental problems based on the above information, which could be included in Axis IV. Additionally , Lynda was given the diagnoses of psychotic disorder - not otherwise specified, schizophrenia probability disorder, and dysthymia. As mentioned above, DD is frequently comorbid with MDD. Schizophrenia is difficult to diagnose in childhood (4). It has been suggested that auditory hallucinations, delusions, and irrational or magical thinking are important diagnostic features (4). Lynda mentioned an interest in witchcraft, and she appeared for her interview dressed in black with her fingernails painted black as well. Schizophrenia in adolescents may have an insidious onset with apathy, a change in hygiene and withdrawal (5). Lyndas chart indicated poor self care; she was not showering. In addition, schizophrenia may coexist with learning disabilities, mental retardation, conduct disorder and autism (4). Lynda has been diagnosed with a learning disability. However, her imaginary friends are not really hallucinations as she actively makes their voices. She has reported a single auditory hallucination. There is not enough information for a clear diagnosis, which is common in the early stages of the disease (2).
Antidepressant treatment was recommend for Lynda, but her parents refused. They consented to close follow-up for their daughter. There has been little research on treatment of MDD in children, so most treatment, efficacy and safety data are extrapolated from adults (3). Antidepressants may be indicated for children and adolescents with non-rapid-cycling bipolar depression, psychotic depression, and depression with symptoms that are unresponsive or preclude the use of psychotherapy. Selective serotonin reuptake inhibitors are recommended because of their safety, side effects profile, ease of administration and suitability for long-term treatment. However, pharmacotherapy cannot be used alone because even with a stabilization of the patients mood, the environmental and social problems remain. Parents should also be counseled to effectively manage their childs problems, and if indicated, parents should be offered treatment themselves (3). Lynda presents with a complex case exhibiting many of the risk factors and complications of childhood MDD. Since her family has refused medication, it is especially important that she receive adequate counseling along with their support to overcome her illness. Continued research into the treatment of childhood depression is important, especially as the medical community continues to recognize depression earlier in children. References 1. Pfeffer CR. Childhood Suicidal Behavior: A Developmental Perspective. Psychiatric Clinics of North America. 1997 Sept; 20(3):551-62. 2. American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, 4th Edition. Washington, DC. American Psychiatric Association, 2000. 3. Practice Parameters for the Assessment and Treatment of Children and Adolescents With Depressive Disorders. Journal of the American Academy of Child and Adolescent Psychiatry. 1998 Oct; 37(10 Supplement):63S-83S. 4. Volkmar FR. Childhood and Adolescent Psychosis: A Review of the Past 10 Years. Journal of the American Academy of Child and Adolescent Psychiatry. 1996; 35:843-51. 5. Andreasen NC and DW Black. Introductory Textbook of Psychiatry, 2nd Edition. Washington, DC. American Psychiatric Press, Inc., 1995.
Vous aimerez peut-être aussi
- Raleigh Psychiatric Clinic Progress Note TemplateDocument3 pagesRaleigh Psychiatric Clinic Progress Note Templatewarrenronald95% (41)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryD'EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryÉvaluation : 3.5 sur 5 étoiles3.5/5 (231)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)D'EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Évaluation : 4.5 sur 5 étoiles4.5/5 (119)
- Never Split the Difference: Negotiating As If Your Life Depended On ItD'EverandNever Split the Difference: Negotiating As If Your Life Depended On ItÉvaluation : 4.5 sur 5 étoiles4.5/5 (838)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaD'EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaÉvaluation : 4.5 sur 5 étoiles4.5/5 (265)
- The Little Book of Hygge: Danish Secrets to Happy LivingD'EverandThe Little Book of Hygge: Danish Secrets to Happy LivingÉvaluation : 3.5 sur 5 étoiles3.5/5 (399)
- Grit: The Power of Passion and PerseveranceD'EverandGrit: The Power of Passion and PerseveranceÉvaluation : 4 sur 5 étoiles4/5 (587)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyD'EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyÉvaluation : 3.5 sur 5 étoiles3.5/5 (2219)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeD'EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeÉvaluation : 4 sur 5 étoiles4/5 (5794)
- Team of Rivals: The Political Genius of Abraham LincolnD'EverandTeam of Rivals: The Political Genius of Abraham LincolnÉvaluation : 4.5 sur 5 étoiles4.5/5 (234)
- Shoe Dog: A Memoir by the Creator of NikeD'EverandShoe Dog: A Memoir by the Creator of NikeÉvaluation : 4.5 sur 5 étoiles4.5/5 (537)
- The Emperor of All Maladies: A Biography of CancerD'EverandThe Emperor of All Maladies: A Biography of CancerÉvaluation : 4.5 sur 5 étoiles4.5/5 (271)
- Autism HandbookDocument93 pagesAutism Handbookfllorinv7100% (5)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreD'EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreÉvaluation : 4 sur 5 étoiles4/5 (1090)
- Her Body and Other Parties: StoriesD'EverandHer Body and Other Parties: StoriesÉvaluation : 4 sur 5 étoiles4/5 (821)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersD'EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersÉvaluation : 4.5 sur 5 étoiles4.5/5 (344)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceD'EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceÉvaluation : 4 sur 5 étoiles4/5 (890)
- NICABM InfoG Window of ToleranceDocument1 pageNICABM InfoG Window of TolerancessjeliasPas encore d'évaluation
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureD'EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureÉvaluation : 4.5 sur 5 étoiles4.5/5 (474)
- The Unwinding: An Inner History of the New AmericaD'EverandThe Unwinding: An Inner History of the New AmericaÉvaluation : 4 sur 5 étoiles4/5 (45)
- The Yellow House: A Memoir (2019 National Book Award Winner)D'EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Évaluation : 4 sur 5 étoiles4/5 (98)
- Ketamine Infusion Therapy in Psychiatric DisordersDocument26 pagesKetamine Infusion Therapy in Psychiatric DisordersDia Rughoo100% (1)
- 2296 Shipon-Blum ElisaDocument96 pages2296 Shipon-Blum Elisadenisse gaboPas encore d'évaluation
- Conners PresentationDocument22 pagesConners PresentationMrigank AggarwalPas encore d'évaluation
- The Role of Ketamine in Eating Disorder TreatmentDocument18 pagesThe Role of Ketamine in Eating Disorder TreatmentyodoidPas encore d'évaluation
- On Fire: The (Burning) Case for a Green New DealD'EverandOn Fire: The (Burning) Case for a Green New DealÉvaluation : 4 sur 5 étoiles4/5 (73)
- MMP Handy Chart October 2011 V2Document37 pagesMMP Handy Chart October 2011 V2ColonPas encore d'évaluation
- Psychiatric NursingDocument58 pagesPsychiatric NursingNimrodPas encore d'évaluation
- Wsas ScaleDocument2 pagesWsas ScaleManju Goswami50% (2)
- When The Therapist's Traumas Emerge in A Psychotherapy Session: The Use of Trauma-Related CountertransferenceDocument9 pagesWhen The Therapist's Traumas Emerge in A Psychotherapy Session: The Use of Trauma-Related CountertransferenceMaroeska De Sutter100% (1)
- Autism Booklet PDFDocument16 pagesAutism Booklet PDFNiki GalaniPas encore d'évaluation
- Autism Booklet PDFDocument16 pagesAutism Booklet PDFNiki GalaniPas encore d'évaluation
- Case Study #1: The Depressed Teen: She Was Moody and Withdrawn.Document10 pagesCase Study #1: The Depressed Teen: She Was Moody and Withdrawn.Eleni Tzanaki-ArnaoutakiPas encore d'évaluation
- Case Study #1: The Depressed Teen: She Was Moody and Withdrawn.Document10 pagesCase Study #1: The Depressed Teen: She Was Moody and Withdrawn.Eleni Tzanaki-ArnaoutakiPas encore d'évaluation
- Case Study #1: The Depressed Teen: She Was Moody and Withdrawn.Document10 pagesCase Study #1: The Depressed Teen: She Was Moody and Withdrawn.Eleni Tzanaki-ArnaoutakiPas encore d'évaluation
- Social Phobia Case Study: Overcoming Anxiety Through Cognitive TherapyDocument4 pagesSocial Phobia Case Study: Overcoming Anxiety Through Cognitive TherapyEleni Tzanaki-ArnaoutakiPas encore d'évaluation
- Case Study #1: The Depressed Teen: She Was Moody and Withdrawn.Document10 pagesCase Study #1: The Depressed Teen: She Was Moody and Withdrawn.Eleni Tzanaki-ArnaoutakiPas encore d'évaluation
- Case Study #1: The Depressed Teen: She Was Moody and Withdrawn.Document10 pagesCase Study #1: The Depressed Teen: She Was Moody and Withdrawn.Eleni Tzanaki-ArnaoutakiPas encore d'évaluation
- Magic 03Document39 pagesMagic 03KneedeepPas encore d'évaluation
- A Lyk Ask Eidikes GlossesDocument1 pageA Lyk Ask Eidikes GlossesEleni Tzanaki-ArnaoutakiPas encore d'évaluation
- Braille system in GreekDocument5 pagesBraille system in GreekvaangosPas encore d'évaluation
- SybilDocument2 pagesSybilAldrine Albor Anyayahan IPas encore d'évaluation
- GNED 129 - Week 11 AssignmentDocument4 pagesGNED 129 - Week 11 AssignmentNehal GuptaPas encore d'évaluation
- Alcohol and Drug AbuseDocument6 pagesAlcohol and Drug AbusedeepapandeyPas encore d'évaluation
- Case Study Evaluation of SchizophreniaDocument14 pagesCase Study Evaluation of SchizophreniaMahammad Abd ElkarimPas encore d'évaluation
- Abnormal Psychology - Clinical Persps. On Psych. Disorders, 6th Ed. - R. Halgin, Et. Al., (McGraw-Hill, 2010 WW-10-15Document6 pagesAbnormal Psychology - Clinical Persps. On Psych. Disorders, 6th Ed. - R. Halgin, Et. Al., (McGraw-Hill, 2010 WW-10-15bella swanPas encore d'évaluation
- Psychiatry OutlineDocument13 pagesPsychiatry Outlinegemazy123Pas encore d'évaluation
- Case Study 1 - Mrs. SmithDocument3 pagesCase Study 1 - Mrs. SmithJulia CooperPas encore d'évaluation
- FearDocument6 pagesFearAlex MunyaoPas encore d'évaluation
- Ekman Et Al-2015-Scandinavian Journal of PsychologyDocument8 pagesEkman Et Al-2015-Scandinavian Journal of Psychologyiuliabucur92Pas encore d'évaluation
- Case Study of Bipolar DisorderDocument1 pageCase Study of Bipolar DisorderIrene Mae Villanueva Ariola0% (1)
- Hubungan Tingkat Kecemasan Dengan Kualitas Tidur Pasien Pre Operasi Di Rumah Sakit Umum Sundari MedanDocument9 pagesHubungan Tingkat Kecemasan Dengan Kualitas Tidur Pasien Pre Operasi Di Rumah Sakit Umum Sundari MedanElisabet Enga taraladuPas encore d'évaluation
- Anxiety and Its Disorders The Nature andDocument2 pagesAnxiety and Its Disorders The Nature andMagdalena ZuziakPas encore d'évaluation
- Asperger's Syndrome - Symptoms, Diagnosis and Treatment - NCDocument5 pagesAsperger's Syndrome - Symptoms, Diagnosis and Treatment - NCRoxan PacsayPas encore d'évaluation
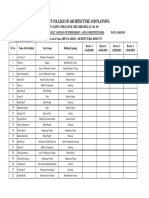
- Ayda Design Competition 2020 Marks Format - Iv & V YearsDocument2 pagesAyda Design Competition 2020 Marks Format - Iv & V YearsanushaPas encore d'évaluation
- DCP FP 5Document19 pagesDCP FP 5JAVERIA YAQOOBPas encore d'évaluation
- AmnesiaDocument4 pagesAmnesiaapi-351680270Pas encore d'évaluation
- Care Plan 27 Bipolar Disorder, Manic Episode: Risk For Other-Directed ViolenceDocument11 pagesCare Plan 27 Bipolar Disorder, Manic Episode: Risk For Other-Directed ViolenceTeanu TamayoPas encore d'évaluation
- Narcissistic Personality Disorder - StatPearls - NCBI BookshelfDocument5 pagesNarcissistic Personality Disorder - StatPearls - NCBI BookshelfDANIELAPas encore d'évaluation
- Nursing Care of Clients with Anxiety DisordersDocument6 pagesNursing Care of Clients with Anxiety DisordersJaylord VerazonPas encore d'évaluation