Académique Documents
Professionnel Documents
Culture Documents
Jurnal Formulasi Mikrokapsul 1
Transféré par
Astri Hardianti RahimDescription originale:
Titre original
Copyright
Formats disponibles
Partager ce document
Partager ou intégrer le document
Avez-vous trouvé ce document utile ?
Ce contenu est-il inapproprié ?
Signaler ce documentDroits d'auteur :
Formats disponibles
Jurnal Formulasi Mikrokapsul 1
Transféré par
Astri Hardianti RahimDroits d'auteur :
Formats disponibles
African Journal of Pharmacy and Pharmacology Vol. 6(28), pp. 2091-2099, 29 July, 2012 Available online at http://www.academicjournals.
org/AJPP DOI: 10.5897/AJPP11.649 ISSN 1996-0816 2012 Academic Journals
Full Length Research Paper
Preparation and evaluation of a sustained-release suspension containing theophylline microcapsules
Jaber Emami1, Jaleh Varshosaz1, Mohammadreza Amirsadri1 and Fatemeh Ahmadi2,3*
Department of Pharmaceutics, Faculty of Pharmacy and Pharmaceutical Sciences, Isfahan University of Medical Sciences, Isfahan, Iran. 2 Department of Pharmaceutics, Faculty of Pharmacy, Shiraz University of Medical Sciences, Shiraz, Iran. 3 Cardiovascular Research Centre, Fasa University of Medical Sciences, Fasa, Iran.
Accepted 9 July, 2012
1
A great effort has been devoted to the preparation of sustained-release formulations of theophylline to prevent large fluctuations of serum concentration and increasing the therapeutic efficacy followed by patient compliance. In the present study, microcapsules of theophylline with ethyl cellulose (EC) were prepared by emulsion-solvent evaporation method in different polymer to drug ratios. Size, morphology, drug loading and release behavior of microcapsules were also studied. Microcapsules were then formulated into suspensions to provide an oral liquid dosage form for drug and resulting suspensions were examined for stability and release characteristics in various storage times. Results showed that microcapsules prepared in drug to polymer ratio 1:1.4 by emulsifying polymer solution in liquid paraffin presented the sustained-release properties which met the United States Pharmacopeia (USP) (2007) requirements (t50% and t80% of these microparticles were 150 and 360 min, respectively). The suspensions prepared by these microcapsules were also stable in the study period and their release profiles were consistent to the original microcapsules. The results allow for the conclusion that the formulated suspension can be used as a sustained-release formulation for theophylline in treatment of obstructive pulmonary disorders. Key words: Theophylline, microencapsulation, suspension, sustained-release, ethyl cellulose.
INTRODUCTION Theophylline is a methylxanthine alkaloid which is used as bronchodilator in treatment of chronic obstructive pulmonary disorders especially asthma. Although, it is used for about 70 years, the complications associated with its use are still unsolved (Obeidat et al., 2009; Soni et al., 2010). Theophylline is a narrow therapeutic index drug with a short half-life. Conventional dosage forms of theophylline should be administered 3 to 4 times a day to provide effective concentration and to avoid large fluctuations in blood concentration. This leads to poor patient compliance and enhanced risk of gastrointestinal (GI) and cardiovascular adverse effects. Sustainedrelease formulations would provide steady blood concentrations with minimum fluctuation and results in higher therapeutic efficacy and lower risk of toxicity (Roy et al., 2007; Zhang et al., 2008). Among sustained-release drug delivery systems, microcapsules have received much attention because of uniform distribution in GI tract which leads to uniform absorption and decreasing risk of local effects on GI tract. Another advantage of microparticulate systems is their feasibility to be incorporated into liquid dosage forms such as suspensions. In addition to sustain the drug release, microencapsulation of theophylline can decrease its irritating effect on GI mucosa and mask drug taste (Lavasanifar et al., 1997). Due to ease of swallowing and flexibility in dosage adjustment, liquid dosage forms are preferred especially in pediatric and geriatric patients (Bodmeier et al., 1991; Cua et al., 2000). Different techniques of microencapsulation have been developed for controlled delivery of different drugs including
*Corresponding author. E-mail: ahmadi_f@sums.ac.ir. Tel: +98 (711) 2424128 (Ext 272). Fax: +98 (711) 2424126.
2092
Afr. J. Pharm. Pharmacol.
emulsion-solvent evaporation for terbutaline (Cua et al., 2000), in-situ gelation for theophylline (Miyazaki et al., 2000), emulsion-solvent diffusion for ibuprofen (Kawashima et al., 1991) and spray drying for paclitaxel (Mu et al., 2005). Choosing a suitable microencapsulation method is highly dependent on the drug characteristics, type of polymer used and economic considerations. Emulsion-solvent evaporation technique is one of early methods of microencapsulation which has been widely studied for preparation of polymeric microcapsules. In this technique, a polymer solution which drug substance is dissolved or dispersed in is emulsified in the external phase. By evaporation of the solvent, polymeric capsules are formed around the drug particles. The size and state of the particle in the internal phase play an important role in the final status of the microparticles. The choice of the internal and the external phase of the emulsion, type of emulsifier and method of homogenizing two phases will effectively determine the characteristics of the final microparticles (Matsumoto et al., 2008). Therefore, the method is very flexible for different types of polymers and hydrophilic and lipophilic drugs, and by selecting suitable solvent and emulsifier; various combinations of drug substances and polymers could be applied. We selected ethyl cellulose (EC) as the sustaining polymer since it is a water-insoluble polymer with good film forming ability, durability and low cost and extended drug release properties (Shi et al., 2008; 2009). EC is a nonbiodegradable and biocompatible and gastro-resistant polymer which has been extensively used as drug release retardant which easily forms microcapsules with a one-step encapsulation method (Das and Rao, 2006; Sudhamani et al., 2010). Taking all these into consideration, we aimed at preparing sustained release microcapsules of theophylline by emulsion-solvent evaporation technique using EC. Although theophylline encapsulation in EC microspheres for sustained delivery have been reported in several studies (Pachuau et al., 2008; Thakare et al., 2011), incorporating the microcapsules into the suspension base was not reported elsewhere. The novelty of our work was to provide a microparticle containing oral liquid sustained release dosage form for easy use in pediatric and geriatric patients.
MATERIALS AND METHODS The following materials were obtained from commercial sources: EC (ethoxy content 46%, Aldrich, USA), acetone, dichloromethane, liquid paraffin, acacia, ammonium hydroxide 25%, methyl paraben, propyl paraben, sodium lauryl sulfate (SLS), theophylline and sucrose (Merck, Germany), sorbitol syrup 70% and tragacanth (Modarres, Iran). All other chemicals and solvents were of analytical grade.
technique with two strategies. First strategy was based on an oil-inwater (o/w) emulsion which prepared after examining large number of variables. For preparing the oil phase, required amount of EC (in three ratios to drug; 1, 2 and 3) was completely dissolved in dichloromethane and 800 mg theophylline was thoroughly dispersed in the mixture by stirring. The oil phase was emulsified into the aqueous phase (1.5% SLS solution in water) under stirring at 300 rpm. The resulting emulsion was stirred for 45 min at room temperature to remove dichloromethane completely. The formed microcapsules were filtered, washed and dried at room temperature. Second strategy was based on emulsifying the drug-containing EC solution in an oil phase. The optimum condition was selected after performing a set of experiments and evaluating the size and drug loading percentage of the particles. The internal phase of the emulsion contained required amount of theophylline dispersed in the EC solution in acetone. The internal phase was then incorporated into the external phase contained 1.3% Tween 80 in 100 ml liquid paraffin. The mixture was stirred at room temperature for 5h to remove acetone and the resulting microcapsules were then filtered and washed with n-hexane and dried at room temperature. Eight formulations (f1 to f8) were prepared by this strategy in the drug to polymer ratios of 1:1, 1:1.2, 1:1.3, 1:1.4, 1:1.5 and 1:2.
Morphological studies of microcapsules In order to demonstrate the formation of microcapsules and preliminary studies of their shape, resulting microcapsules were studied using a simple optical microscope (HM-LUX3, Leitz, Germany). Samples of microcapsules were selected randomly. Size of microcapsules was also determined using hemocytometer.
Determination of drug loading of microcapsules The drug content of microcapsules was determined according to USP 30 method for testing content uniformity of sustained-release capsules of theophylline (USP, 2007). Briefly, a sample of microcapsules containing 100 mg of drug was triturated with 20 ml of water, transferred to a 100 ml volumetric flask, 25 ml of 6 N ammonium hydroxide added, sonicated for about 45 min, and cooled to room temperature. The mixture was diluted to volume and mixed. The mixture was then filtered and diluted with water and the absorbance of this solution and a standard solution of theophylline, similarly prepared was read at 270 nm with ultraviolet (UV)-visible spectrophotometer (550SE, Perkin-Elmer, USA). The concentration of drug in the sample was then determined according to the standard solution of theophylline.
Preparation of suspensions Microcapsules with the optimum range of dissolution (dissolution test will be discussed in following sections) and shape were selected to be formulated in suspensions. Two suspension formulations were prepared as the medium of suspensions (Table 1), either contains 100 mg theophylline / 5 ml (Kawashima et al., 1991).
Characterization of suspensions Rheology
Preparation of microcapsules Microcapsules were prepared by emulsion-solvent evaporation The rheology of the suspensions was determined using a Brookfield rotational viscometer (Metler RM180) with measuring bob No.2 and
Emami et al.
2093
Table 1. Formulation details and composition of the medium of two suspensions.
Materials Simple syrup, NF Sorbitol syrup 70% Deionized distilled water Tragacanth Tween 80 Methyl paraben Propyl paraben
Uses Sweetening agent Sweetening agent Vehicle Suspending agent, Thickening agent Nonionic moisturizing agent Preservative Preservative
Amount in suspensions Suspension I Suspension II 1 Part 2 Parts 1 Part 2 Parts 3 Parts 1 part 0.6% 0.6% 0.02% 0.02% 0.1% 0.1% 0.1% 0.1%
measuring tube No.2.
Drug release studies The USP paddle method was used for testing the release of theophylline from microcapsules and suspensions. Experiments were performed according to dissolution test No. II for sustainedrelease theophylline preparation using a USP dissolution apparatus (Pharma test, PTZWS3, Germany). The dissolution medium was consisted of 900 ml phosphate buffer (pH 4.5) maintained at 37C stirred at rate of 75 rpm. An amount of microcapsule or suspension containing 100 mg theophylline was used for each dissolution experiment. At appropriate time intervals, 20, 40, 60, 90, 120, 180, 240, 300, 360, 420 and 480 min, a 3 ml sample of dissolution medium was withdrawn and replaced by an equal volume of medium to maintain the volume constant. Samples were filtered, diluted, and analyzed for theophylline concentration at 270 nm to characterize the dissolution profiles. For reading the absorbance of samples obtained from the dissolution of suspensions, dissolution media containing drug free suspension was used as the blank. Dissolution efficiency percentage after 8 h (DE8%) was considered as a basis for comparing the dissolution profiles. DE% was calculated based on the following equation:
Sedimentation volume The sedimentation volume (F) was obtained based on the following equation:
V1 , V0
V1 is the equilibrium volume of sediment and V0 is the total volume of suspension before sedimentation. Equilibrium volume of sediment is the volume which remains unchanged for 3 weeks (Gennaro, 2000; Sinko, 2006).
Degree of flocculation Degree of flocculation () was estimated using this equation:
F F ,
F is the sedimentation volume of the flocculated suspension, and F is the sedimentation volume of the suspension when deflocculated (Gennaro, 2000; Sinko, 2006). Ease of redispersibility: The number of shears required to redisperse a sedimented suspension in a cylindrical glass graduate is an indicator of ease of redispersibility (N) (Jones et al., 1970).
DE%
y.dt
ty100
100 100
DE is the ratio of area under the dissolution curve at a given time to the total area at the same time once the entire content is released (Khan, 1975).
Freeze/Thaw cycles Physical and microscopic changes of suspensions under sudden thermal changes were investigated. Suspensions were kept in a 40C oven for 24 h and then transferred to a 0C freezer for 24 h (Lieberman, 1990).
Kinetic models analysis The release data were fitted to different kinetic models in Microsoft Excel 2007 software as follows to determine the model which better described the kinetics of the release behavior: First-order kinetic ln W ln W0 k1t , Hixson-Crowells cube root of time
W 1 / 3 W01 / 3 k 2 t , and square-root of time W W0 kt1 / 2 , where
Normal temperature fluctuation Inspection of physical and microscopic changes of the suspension during a gradual decrease in temperature from 40 to -5C was also performed. For this purpose, suspensions were kept for 24 h in each temperature (Sinko, 2006). pH of suspensions: pH of suspensions was determined using a Rotring pH meter (Dalal and Narurkar, 1991). W is the amount of drug remaining to be released and W 0 is the initial amount of drug (Sprockel and Price, 1989).
Statistical analysis SPSS software version 12 was used for all statistical analysis. Student t-test and one-way analysis of variance (ANOVA) followed by a Duncan post hoc test, was used for comparison between DE%
2094
Afr. J. Pharm. Pharmacol.
Table 2. Drug loading percentage of the microcapsules prepared by two strategies (n = 6).
Preparation strategy Aqueous Aqueous Aqueous Oil Oil Oil Oil Oil Oil
Polymer to drug ratio 1 2 3 1 1.2 1.3 1.4 1.5 2
Type of stirrer Propeller stirrer Propeller stirrer Propeller stirrer Magnet stirrer Magnet stirrer Magnet stirrer Magnet stirrer Magnet stirrer Magnet stirrer
Loading percentage (Mean SD) 89.9 0.9 85.6 0.4 80.1 0.7 72.0 0.7 70.1 0.6 69.2 0.7 68.8 0.9 66.9 0.7 62.0 0.9
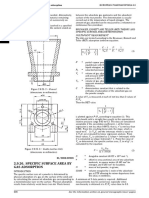
Figure 1. Release profile of microcapsules prepared in aqueous phase (n = 6).
Figure 2. Release profiles of microcapsules prepared in oil phase with different polymer to drug ratios (n = 6).
and other parameters between two or more than two formulations, respectively. P-value less than 0.05 was considered significant.
ratios of 1:1.4, 1:1.5 and 1:2. Drug loading and release studies
RESULTS Microscopic studies of microcapsules Inspection of microcapsules by optical microscopy showed that microcapsules prepared by first strategy in aqueous phase were smaller with a rough surface, while microcapsules prepared in oil phase were spherical with a smooth uniform surface and acceptable degree of homogeneity. Size of microcapsules prepared in aqueous phase was in the range 200 to 230 m which was increased by increasing polymer to drug ratio. The size of microcapsules prepared in oil phase were in the range of 480 to 530 m for drug to polymer ratios 1:1, 1:1.2 and 1:1.3 while it suddenly decreased to 240-265 m for Results of loading percentage of microcapsules prepared by two strategies are shown in Table 2. Loading was higher in microcapsules prepared in aqueous phase (80 to 90%) compared to ones prepared in oil phase (62 to 72%). It was decreased as the polymer to drug ratio increased and this trend was observed for microcapsules prepared by both strategies. Figure 1 shows the release profiles of microcapsules prepared in aqueous phase. Results of DE% of these microcapsules are not presented, because the release profile was not controlled and the formulation did not satisfy the goal of preparation of sustained release formulation of theophylline. Release profiles of microcapsules prepared by second strategies are shown in Figure 2. By increasing polymer
Emami et al.
2095
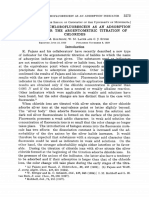
(a)
was slower compared with the microcapsules prepared by the first strategy. Release behavior of both suspensions met the requirements presented in USP and no significant difference (P > 0.05) was observed in release profiles and DE% for both suspensions on first day and after 12 weeks which indicates the stability of suspensions. Figure 3 shows the release profiles of suspensions in different storage times. Results of DE8% are also listed in Table 3. Fitting the release data to the different kinetic models showed that the release kinetics of microcapsules with different polymer to drug ratios were significantly different (P < 0.05) and by increasing the ratio of polymer to drug, kinetic was changed from Higuchi to Hixson-Crowell. In contrast, the values of kinetic constant, K, and correlation coefficient, R, calculated for both suspensions were not significantly different between kinetic models (P > 0.05). Values of correlation coefficients and kinetic constants (K) obtained by fitting data to different kinetic models are shown in Table 4.
Characterization of suspensions As shown in Figure 4, both suspensions showed a thixotropic rheogram with shear thinning behavior. Suspension I presented higher thixotropy and lower viscosity than suspension II. pH values for suspension I and II were 5.98 0.04 and 7.16 0.05, respectively, which is suitable for an oral suspension of theophylline according to the pKa of the drug. Results of physical tests performed on suspensions are shown in Table 5 which indicates the suitability of the suspension properties. Sedimentation volume of suspensions was less than 0.9 and the suspensions were easily redispersed by 2 or 3 revolutions. No changes were observed in flocculation and crystallization of both suspensions during freeze / thaw cycles and normal temperature fluctuation tests. DISCUSSION Emulsion-solvent evaporation technique in aqueous systems for preparation of microcapsules is preferred over non-aqueous systems because of economic considerations and easier final clean-up of the system (Torres et al., 1998). Preparation of EC microcapsules by this method was not provided a continuous polymeric wall around the drug particles. This is mostly due to the limitation in selecting a solvent for dispersing polymer which is immiscible with the aqueous external phase of the emulsion. The preparation method in the oil phase was more reproducible and flexible and acetone was used instead of dichloromethane which is less toxic. The resulting microcapsules of this method were free flowing. The difference in shape of microcapsules prepared by these methods might be a consequence of difference in
(b)
Figure 3. Release profiles of microcapsules prepared in oil phase with polymer to drug ratio 1.4 formulated in (a) Suspension I and (b) Suspension II after various storage times (n = 6).
to drug ratio, release rate decreased and the formulation prepared by drug to polymer ratio 1:2, released less than 10% of drug in 20 min and the total release percentage in 8 h was 70%. All formulations except the one prepared in ratio 1:1 (which showed a burst release of 50% in 20 min), provided sustained-release profile with similar trend. DE8% for these formulations was also decreased from 89.22% for drug to polymer ratio 1:1 to 44.78% for ratio 1:2, significantly (P < 0.05). Although drug loading was lower for microcapsules prepared by this method, the release rate of theophylline from these microcapsules
2096
Afr. J. Pharm. Pharmacol.
Table 3. DE8% obtained for various microcapsules prepared in oil phase and resulting suspensions (n = 6).
Formulation Microcapsules with polymer to drug ratio 1 Microcapsules with polymer to drug ratio 1.2 Microcapsules with polymer to drug ratio 1.3 Microcapsules with polymer to drug ratio 1.4 Microcapsules with polymer to drug ratio 1.5 Microcapsules with polymer to drug ratio 2 Suspension I, after 24 h Suspension I, after 1 week Suspension I, after 3 weeks Suspension I, after 6 weeks Suspension I, after 9 weeks Suspension I, after 12 weeks Suspension II, after 24 h Suspension II, after 1 week Suspension II, after 3 weeks Suspension II, after 6 weeks Suspension II, after 9 weeks Suspension II, after 12 weeks
% DE8, Dissolution efficiency percentage after 8 h.
% DE8 Mean 89.22 68.49 62.73 58.27 51.27 44.78 58.27 58.42 58.56 58.72 58.94 59.11 59.19 59.23 58.75 58.66 58.33 58.22 SD 0.10 0.26 0.19 0.43 0.29 0.30 0.86 0.78 0.82 0.45 0.68 0.48 0.22 0.35 0.72 0.23 0.37 0.29
Table 4. Values of correlation coefficients (R) and kinetic constants (K) obtained by fitting data to different kinetic models.
Formulation Microcapsules with polymer to drug ratio 1 Microcapsules with polymer to drug ratio 1.2 Microcapsules with polymer to drug ratio 1.3 Microcapsules with polymer to drug ratio 1.4 Microcapsules with polymer to drug ratio 1.5 Microcapsules with polymer to drug ratio 2 Suspension I, after 24 h Suspension II, after 24 h
Values are presented as mean SD (n = 6).
First order K/2.303 (1/min) R 0.0041 0.0001 0.9572 0.0019 0.0034 0.0001 0.9495 0.0022 0.0028 0.0001 0.9707 0.0147 0.0022 0.0001 0.9911 0.0037 0.0016 0.0000 0.9954 0.0024 0.0011 0.0001 0.9947 0.0016 0.0022 0.0001 0.9892 0.0030 0.0022 0.0001 0.9874 0.0077
Higuchi K (min ) 2.7572 0.0219 5.0032 0.0166 5.0353 0.0325 4.9300 0.0270 4.5201 0.0193 3.7472 0.0349 4.8541 0.0930 4.8710 0.0674
1/2
R 0.9164 0.0016 0.9898 0.0017 0.9986 0.0004 0.9988 0.0004 0.9987 0.0004 0.9965 0.0006 0.9981 0.0008 0.9980 0.0003
Hixson-Crowell K (1/min) R 0.0088 0.0001 0.9603 0.0005 0.0078 0.0001 0.9576 0.0019 0.0061 0.0002 0.9951 0.0033 0.0053 0.0001 0.9980 0.0009 0.0043 0.0001 0.9982 0.0008 0.0031 0.0001 0.9911 0.0010 0.0052 0.0002 0.9975 0.0010 0.0052 0.0001 0.9967 0.0025
Emami et al.
2097
(a)
(b)
Figure 4. Rheograms of (a) Suspension I and (b) Suspension II prepared from microcapsules of oil phase with polymer to drug ratio 1.4. Rheology of the suspensions was characterized using a Brookfield viscometer (Metler RM180) with measuring bob No.2 and measuring tube No.2.
the evaporation rate of the solvent. Similar results were obtained in microencapsulation of terbutaline-loaded ion exchange resins (Cua et al., 2000). Rapid evaporation of the solvent results in microcapsules with a rough surface (Radwan et al., 1995). Surface of microcapsules with lower drug loading was smoother because of lower amount of drug crystals on the surface. Increasing the
size of the particles with increasing polymer to drug ratio may be due to the higher concentration of the polymer in the dispersed phase which results in increased viscosity of the solution and therefore enhanced volume occupied by the polymer. Microcapsules with sizes around 200 m are easily dispersed in a liquid suspension without a gritty sensation (Cua et al., 2000). Two strategies were used for microencapsulation to examine the effect of hydrophilicity of the internal and external phase on drug loading. Sine theophylline is a hydrophilic drug; there may be some partitioning of drug out to the aqueous phase and lower loading in this strategy as reported for zidovudine encapsulated EC microspheres (Das and Rao, 2006). Using oil phase would increase the loading, however, this was not observed in our results and the drug loading was higher by the first strategy in aqueous phase. As reported elsewhere, entrapment of drug in the microcapsules is dependent on the continuity and integrity of the particle wall which is controlled by polymer to drug ratio (Halder and Sa, 2006). As shown in Figure 1, while increasing polymer to drug ratio, decreased the dissolution rate, the three sets of microcapsules did not provide the sustained release and 90% of drug was released in 20 min. The difference between three formulations was not significant. The release profile of these microcapsules was not controlled and the formulation did not satisfy the goal of preparation of sustained release formulation of theophylline. Higher release rate of microcapsules prepared by this strategy may be due to the smaller size and therefore larger surface area of the particles (Guyot and Fawaz, 1998). Dependency of release to polymer to drug ratio, has also been reported for furosemide-loaded (Akbuga, 1991) and tramadol-loaded EC microspheres (Naeem Aamir et al., 2011), which is due to the increased hydrophobic thickness of the polymeric wall followed by the longer passage way of the drug through the encapsulating wall (Naeem Aamir et al., 2011). Although drug loading was lower for microcapsules prepared by this method, the slower rate of release of theophylline from these microcapsules is related to the larger size of particles and more uniform structure of the polymeric wall. This observation has also been reported before, that release from EC microcapsules was dependent on size and loading of particles (Bodmeier et al., 1994). According to USP (2007), sustained-release formulations of theophylline should release 10 to 30% of their drug content in the first hour and a minimum of 80% after 8 h. Therefore, the microcapsules prepared in drug to polymer ratio 1:1.4 in oil phase were used to formulate suspensions. The release profile was better fitted to Higuchi model which means that the release is mostly controlled by diffusion. Release of EC microspheres loaded with furosemide, tramadol and zidovudine was also reported to be proportional to the square root of time (Akbuga, 1991; Das and Rao, 2006; Naeem Aamir et al.,
2098
Afr. J. Pharm. Pharmacol.
Table 5. Results of physical parameters evaluated for characterization of suspensions.
Suspension number Suspension I Suspension II
3.97 0.04 3.80 0.04
F 0.79 0.01 0.84 0.01
N 2 3
State of flocculation Flocculated Flocculated
, Degree of flocculation; F, sedimentation volume; N, ease of redispersibility.
2011). A new report also presents that release of theophylline loaded EC microcapsules followed the Higuchi model which supports the formation of a monolithic system which releases the drug by Fickian diffusion (Thakare et al., 2011). The second objective of our study was to formulate the microcapsules into an oral liquid suspension. An ideal suspension medium should be able to prevent drug leakage during the storage time and should not affect the original properties of the microspheres. It should be provide uniform dispersion of microspheres without caking and instability or any unacceptable effect on release properties and bioavailability of the drug. Therefore, the microcapsules should be formulated in medium containing suspending agent, which prevents drug loss to the suspension medium (Bodmeier et al., 1991; Kawashima et al., 1991). Release of theophylline form suspensions in different storage times was consistent to the original microspheres alone. It shows that there was no leakage of the drug from the microspheres to the suspension medium and the medium did not influence the drug release properties of the microcapsules. The two formulated suspensions were acceptable based on physical properties, stability and release behavior. By comparing the rheograms, results of physical tests and release studies, suspension I was selected as the suitable formulation and its release profile did not change during the storage time. In summary, microcapsules prepared in oil phase and drug to polymer ratio 1:1.4, provided the most ideal sustained release profile for drug which is consistent to USP requirements for sustained release preparations of theophylline. The suspension I prepared from desired microcapsules presented expected qualities for uniform dispersibility, preventing drug loss and adequate stability over the 6 month storage time without any unwanted effect on release behavior of microcapsules.
ACKNOWLEDGEMENT This work has been supported by Research Council of Isfahan University of Medical Sciences.
REFERENCES Akbuga J (1991). Furosemide-loaded ethyl cellulose microspheres prepared by spherical crystallization technique: Morphology and release characteristics. Int. J. Pharm. 76:193-198.
Bodmeier R, Chen H, Tyle P, Jarosz P (1991). Pseudoephedrine HCl microspheres formulated into an oral suspension dosage form. J. Control Release 15:65-77. Bodmeier R, Wang H, Herrmann J (1994). Microencapsulation of chlorpheniramine maleate, a drug with intermediate solubility properties, by a non-aqueous solvent evaporation technique. STP. Pharma Sci. 4:275-281. Cua M, Vila Jato JL, Torres D (2000). Controlled-release liquid suspensions based on ion-exchange particles entrapped within acrylic microcapsules. Int. J. Pharm. 199:151-158. Dalal PS, Narurkar MM. (1991). In vitro and in vivo evaluation of sustained release suspensions of ibuprofen. Int. J. Pharm. 73:157162. Das MK, Rao KR (2006). Evaluation of zidovudine encapsulated ethylcellulose microspheres prepared by water-in-oil-in-oil (w/o/o) double emulsion solvent diffusion technique. Acta Pol. Pharm. Drug Res. 63:141-148. Gennaro A (2000). Remington: The science and practice of pharmacy. Mack publishing company, Easton. P. 318. Guyot M, Fawaz F (1998). Nifedipine loaded-polymeric microspheres: Preparation and physical characteristics. Int. J. Pharm. 175:61-74. Halder A, Sa B. (2006). Preparation and in vitro evaluation of polystyrene-coated diltiazem-resin complex by oil-in-water emulsion solvent evaporation method. AAPS Pharm. Sci. Tech. 7:E105-E112. Jones RDC, Matthews BA, Rhodes CT (1970). Physical stability of sulfaguanidine suspensions. J. Pharm. Sci. 59:518-520. Kawashima Y, Iwamoto T, Niwa T, Takeuchi H, Itoh Y (1991). Preparation and characterization of a new controlled release ibuprofen suspension for improving suspendability. Int. J. Pharm. 75:25-36. Khan KA (1975). The concept of dissolution efficiency. J. Pharm. Pharmacol. 27:48-49. Lavasanifar A, Ghalandari R, Ataei Z, Zolfaghari ME, Mortazavi SA (1997). Microencapsulation of theophylline using ethylcellulose: In vitro drug release and kinetic modelling. J. Microencapsul. 14:91-100. Lieberman L (1990). Pharmaceutical dosage forms: Disperse systems. Marcel Dekker, New York, pp. 93-149. Matsumoto A, Matsukawa Y, Nishioka Y, Harada M, Horikiri Y, Yamahara H (2008). A new method of preparing TRH derivativeloaded poly(dl-lactide-co-glycolide) microspheres based on a solid solution system. Drug Discov. Ther. 2:45-51. Miyazaki S, Kubo W, Attwood D (2000). Oral sustained delivery of theophylline using in-situ gelation of sodium alginate. J. Control Release 67:275-280. Mu L, Teo MM, Ning HZ, Tan CS, Feng SS (2005). Novel powder formulations for controlled delivery of poorly soluble anticancer drug: Application and investigation of TPGS and PEG in spray-dried particulate system. J. Control Release 103:565-575. Naeem Aamir M, Ahmad M, Akhtar N, Murtaza G, Khan SA, Shahiquz Z, Nokhodchi A (2011). Development and in vitro-in vivo relationship of controlled-release microparticles loaded with tramadol hydrochloride. Int. J. Pharm. 407(1-2):38-43. Obeidat W, Obeidat S, Alzoubi N (2009). Investigations on the physical structure and the mechanism of drug release from an enteric matrix microspheres with a near-zero-order release kinetics using SEM and quantitative FTIR. AAPS Pharm. Sci. Tech. 10:615-623. Pachuau L, Sarkar S, Mazumder B (2008). Formulation and evaluation of matrix microspheres for simultaneous delivery of salbutamol sulphate and theophylline. Trop. J. Pharm. Res. 7:995-1002. Radwan MA, Price JC, Tackett RL (1995). In vitro release of disopyramide from cellulose acetate butyrate microspheres. Drug
Emami et al.
2099
Dev. Ind. Pharm. 21:1453-1462. Roy C, Vega-Gonzlez A, Subra-Paternault P (2007). Theophylline formulation by supercritical antisolvents. Int. J. Pharm. 343:79-89. Shi P, Li Y, Zhang L (2008). Fabrication and property of chitosan film carrying ethyl cellulose microspheres. Carbohydr. Polym. 72:490499. Shi P, Zuo Y, Zou Q, Shen J, Zhang L, Li Y, Morsi YS (2009). Improved properties of incorporated chitosan film with ethyl cellulose microspheres for controlled release. Int. J. Pharm. 375:67-74. Sinko PJ (2006). Martin's physical pharmacy and pharmaceutical sciences. 5th ed. Lippincott Williams & Wilkins, Philadelphia. Pp. 502503. Soni MK, Kumar M, Namdeo KP (2010). Sodium alginate microspheres for extending drug release: Formulation and in vitro evaluation. Int. J. Drug Del. 2:64-68. Sprockel OL, Price JC (1989). Evaluation of sustained release aqueous suspensions containing microencapsulated drug-resin complexes. Drug Dev. Ind. Pharm. 15:1275-1287.
Sudhamani T, Noveenkumar reddy K, Ravi Kumar VR, Revathi R, Ganesan V (2010). Preparation and evaluation of ethyl cellulose microspheres of ibuprofen for sustained drug delivery. Int. J. Pharm. Res. Dev. Online. Publication Ref No.:IJPRD/2010/PUB/ARTI/VOV2/ISSUE-8/OCT/019. Thakare M, Israel B, Garner ST, Ahmed H, Garner P, Elder D, Price JC, Capomacchia AC (2011). Pharm. Dev. Technol. Article in Press. Doi:10.3109/10837450.2011.620969. The United States Pharmacopeia (USP) (2007). United States Pharmacopeial Convention Inc., Rockville. Torres D, Boado L, Blanco D, Vila-Jato JL (1998). Comparison between aqueous and non-aqueous solvent evaporation methods for microencapsulation of drug-resin complexes. Int. J. Pharm. 173:171182. Zhang W, Chen X, Li P, He Q, Zhou H (2008). Preparation and characterization of theophylline loaded chitosan/ -cyclodextrin microspheres. J. Mater. Sci. Mater. Med. 19:305-310.
Vous aimerez peut-être aussi
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryD'EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryÉvaluation : 3.5 sur 5 étoiles3.5/5 (231)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)D'EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Évaluation : 4.5 sur 5 étoiles4.5/5 (119)
- Never Split the Difference: Negotiating As If Your Life Depended On ItD'EverandNever Split the Difference: Negotiating As If Your Life Depended On ItÉvaluation : 4.5 sur 5 étoiles4.5/5 (838)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaD'EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaÉvaluation : 4.5 sur 5 étoiles4.5/5 (265)
- The Little Book of Hygge: Danish Secrets to Happy LivingD'EverandThe Little Book of Hygge: Danish Secrets to Happy LivingÉvaluation : 3.5 sur 5 étoiles3.5/5 (399)
- Grit: The Power of Passion and PerseveranceD'EverandGrit: The Power of Passion and PerseveranceÉvaluation : 4 sur 5 étoiles4/5 (587)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyD'EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyÉvaluation : 3.5 sur 5 étoiles3.5/5 (2219)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeD'EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeÉvaluation : 4 sur 5 étoiles4/5 (5794)
- Team of Rivals: The Political Genius of Abraham LincolnD'EverandTeam of Rivals: The Political Genius of Abraham LincolnÉvaluation : 4.5 sur 5 étoiles4.5/5 (234)
- Shoe Dog: A Memoir by the Creator of NikeD'EverandShoe Dog: A Memoir by the Creator of NikeÉvaluation : 4.5 sur 5 étoiles4.5/5 (537)
- The Emperor of All Maladies: A Biography of CancerD'EverandThe Emperor of All Maladies: A Biography of CancerÉvaluation : 4.5 sur 5 étoiles4.5/5 (271)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreD'EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreÉvaluation : 4 sur 5 étoiles4/5 (1090)
- Her Body and Other Parties: StoriesD'EverandHer Body and Other Parties: StoriesÉvaluation : 4 sur 5 étoiles4/5 (821)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersD'EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersÉvaluation : 4.5 sur 5 étoiles4.5/5 (344)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceD'EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceÉvaluation : 4 sur 5 étoiles4/5 (890)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureD'EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureÉvaluation : 4.5 sur 5 étoiles4.5/5 (474)
- The Unwinding: An Inner History of the New AmericaD'EverandThe Unwinding: An Inner History of the New AmericaÉvaluation : 4 sur 5 étoiles4/5 (45)
- The Yellow House: A Memoir (2019 National Book Award Winner)D'EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Évaluation : 4 sur 5 étoiles4/5 (98)
- On Fire: The (Burning) Case for a Green New DealD'EverandOn Fire: The (Burning) Case for a Green New DealÉvaluation : 4 sur 5 étoiles4/5 (73)
- Smart Biomaterials PDFDocument380 pagesSmart Biomaterials PDFcris100% (1)
- Metabolisme Bilirubin Blok 11 2016Document22 pagesMetabolisme Bilirubin Blok 11 2016Astri Hardianti RahimPas encore d'évaluation
- Corrosion Management in Gas Processing FacilitiesDocument44 pagesCorrosion Management in Gas Processing Facilitiescoolguy12345Pas encore d'évaluation
- Jurnal EnzimDocument12 pagesJurnal EnzimAstri Hardianti RahimPas encore d'évaluation
- University of Wisconsin Department of Family Medicine Nasal Irrigation InstructionsDocument2 pagesUniversity of Wisconsin Department of Family Medicine Nasal Irrigation InstructionsAstri Hardianti RahimPas encore d'évaluation
- Taste and Chorda TympaniDocument11 pagesTaste and Chorda TympaniAstri Hardianti RahimPas encore d'évaluation
- IntoksikasiDocument10 pagesIntoksikasiAstri Hardianti RahimPas encore d'évaluation
- Aria 2013Document15 pagesAria 2013Astri Hardianti RahimPas encore d'évaluation
- Jurnal AEW ModelDocument12 pagesJurnal AEW ModelAstri Hardianti RahimPas encore d'évaluation
- Jurnal GastroretentiveDocument8 pagesJurnal GastroretentiveAstri Hardianti RahimPas encore d'évaluation
- Kuliah 5 - Derajat Kehalusan SerbukDocument47 pagesKuliah 5 - Derajat Kehalusan SerbukAstri Hardianti RahimPas encore d'évaluation
- MSc Analytical Chemistry SyllabusDocument66 pagesMSc Analytical Chemistry SyllabusJPas encore d'évaluation
- Advantages:: DisadvantagesDocument10 pagesAdvantages:: DisadvantagesZahir Rayhan JhonPas encore d'évaluation
- Physics 274 Final ExamDocument6 pagesPhysics 274 Final ExamCurt FreePas encore d'évaluation
- Basics of Convection of Heat Transfer ModeDocument105 pagesBasics of Convection of Heat Transfer ModeSamir YehyaPas encore d'évaluation
- An Overview of The Production and Use of Ammonia in NSR + SCR CoupledDocument11 pagesAn Overview of The Production and Use of Ammonia in NSR + SCR CoupledCicero LimaPas encore d'évaluation
- Band Theory of SolidsDocument40 pagesBand Theory of SolidsCharan ReddyPas encore d'évaluation
- Volumetric Gas Adsorption Technique - Magnesium Stearate - EP6.0 - 01 - 231Document4 pagesVolumetric Gas Adsorption Technique - Magnesium Stearate - EP6.0 - 01 - 231Debahis BosePas encore d'évaluation
- Instrumental Methods of Analysis TechniquesDocument2 pagesInstrumental Methods of Analysis TechniquesUadPas encore d'évaluation
- Principles of Fluid Chillers: Design for Reliable OperationDocument7 pagesPrinciples of Fluid Chillers: Design for Reliable OperationAzim AdamPas encore d'évaluation
- Rubber Blooms GuideDocument5 pagesRubber Blooms Guidealperen52Pas encore d'évaluation
- Paper 2 Jun 2000 PhysicsDocument4 pagesPaper 2 Jun 2000 Physicssolarixe100% (3)
- First Order ReactionDocument5 pagesFirst Order ReactionShayPas encore d'évaluation
- Assignment 2Document1 pageAssignment 2Ankit OlaPas encore d'évaluation
- Electrochemical Degradation of Safranin T DyeDocument12 pagesElectrochemical Degradation of Safranin T DyeLeidy StefanyPas encore d'évaluation
- Forced ConvectionDocument5 pagesForced ConvectionRahul NairPas encore d'évaluation
- Test Bank For Chemistry A Molecular Approach 4th Edition by Tro ISBN 0134112830 9780134112831Document36 pagesTest Bank For Chemistry A Molecular Approach 4th Edition by Tro ISBN 0134112830 9780134112831shawnramirez06042001jzc100% (23)
- Test For Anions (Chemistry)Document22 pagesTest For Anions (Chemistry)abby jacksonPas encore d'évaluation
- Horita, Wesolowski - 1994 - Liquid-Vapor Fractionation of Oxygen and Hydrogen Isotopes of Water From Freezing To The Critical TemperaturDocument13 pagesHorita, Wesolowski - 1994 - Liquid-Vapor Fractionation of Oxygen and Hydrogen Isotopes of Water From Freezing To The Critical TemperaturMichelle CastroPas encore d'évaluation
- Cambridge International Advanced Subsidiary and Advanced LevelDocument12 pagesCambridge International Advanced Subsidiary and Advanced LevelRahi FurqanPas encore d'évaluation
- Chemistry Textbook For Atoms by MitDocument2 pagesChemistry Textbook For Atoms by MitdsfdsfdPas encore d'évaluation
- BismuthDocument20 pagesBismuthjosevitorromualdoPas encore d'évaluation
- EDAPLAN ® 490 - MunzingDocument4 pagesEDAPLAN ® 490 - MunzingLong An Đỗ0% (1)
- 10 - Chapter5Document50 pages10 - Chapter5Mahdi AL-oqilyPas encore d'évaluation
- Introduction to Chemical Engineering Thermodynamics IDocument58 pagesIntroduction to Chemical Engineering Thermodynamics IGlory UsoroPas encore d'évaluation
- Sodium HyaluronateDocument4 pagesSodium HyaluronateAldo Ilyan Perez MendezPas encore d'évaluation
- Kolthoff 1929Document5 pagesKolthoff 1929ipark2025Pas encore d'évaluation
- Talk 5-3-1 CST Euc 2012Document175 pagesTalk 5-3-1 CST Euc 2012Anonymous 3GE9cFCPas encore d'évaluation
- Chemistry ks4 Lesson CHM Y11 U1 l10Document19 pagesChemistry ks4 Lesson CHM Y11 U1 l10Sri WahyuningsihPas encore d'évaluation