Académique Documents
Professionnel Documents
Culture Documents
Gerd DR Neneng
Transféré par
She JocelynDescription originale:
Titre original
Copyright
Formats disponibles
Partager ce document
Partager ou intégrer le document
Avez-vous trouvé ce document utile ?
Ce contenu est-il inapproprié ?
Signaler ce documentDroits d'auteur :
Formats disponibles
Gerd DR Neneng
Transféré par
She JocelynDroits d'auteur :
Formats disponibles
Pathophysiologic mechanisms : � Transient lower esophageal sphincter relaxations (tLESRs) � A hypotensive lower esophageal sphincter (LES) � Anatomic disruption
of the gastro esophageal junction, often associated with a hiatal hernia
Heart burn and regurgitation are The most common symptoms
How the Heartburn recognised?
Gastro-esophageal Refluks Disease (GERD)
Esophageal syndromes Symptomati c syndromes 1. Typical refluks syndrome 2. Refluks chest pain syndrome Syndromes with Esophageal injury Extra-Esophageal syndromes Established association Proposed Association
1. Pharyngitis 1. Refluks esophagitis 1. Refluks cough syndrome 2. Sinusitis 2. Refluks stricture 3. Barrets esophagus 2. Refluks laryngitis 3. Idiopathic syndrome Pulmonary fibrosis 4. Esophageal 4. Recurrent otitis Adenocarcinoma 3. Refluks astma syndrome media 4. Refluks dental erosion syndrome (Vakil etal., Am J Gastroenterol 2006; 101:1900-1920)
� � � � � � � �
Progressive dysphagia Odynophagia Weight loss (unintentional) Anemia (new onset) Hematemesis and/or melena Family history of gastric and/or esophageal cancer Chronic non-steroid anti-inflammatory drug use Age >40 years in areas of a high prevalence of gastric cancer
esofagitis
esofagitis
normal
Question
Frequency score (point) for symptome
0 day 1 day 1 1 2-3 day 2 2 4-7 day 3 3 0 0
1. How often did you have a burning feeling behind your breastbone (heartburn) ? 2. How did you have a stomach contents (liquid or food) moving upward tu your throat or mouth (regurgutation) ? 3. How often did you have a pain in the center of the upper stomach? 4. How often did you have nausea? 5. How often did you difficulty getting a good nights sleep because of your heartburn and/or your regurgutation ? 6. How often did you take additional medication for your heartburn and/or regurgutation? (such as Tums, Rolaids, Maalox?)
3 3 0
2 2 1
1 1 2
0 0 3
Alarm features present
Alarm features absent PPI therapy 4 week and Review at 2 to 4 week
REFER for EGD or H.pylori test Stop PPI at least 1 week
Symptomes persist
Symptomes respond Trial for Stop PPI Relapse
Frequent relapse, or Alarm features
On-demand therapy
Restart PPI
... and step down dosing
Conclusion: -On-demand therapy is a useful option in GERD but needs to be limited to selected patients -Severe Grade of esophagitis and Barrets esophagus are best managed with continuous therapy (Gjostedt et al. Aliment Pharmacol Ther 2005. 22: 183-91)
Patophysiologi of gastric-doodenal mucosa injury
Hp associated ulcer and cancer
NSAIDs associated ulcer and gastric erosion
� � � � � � �
Alterations in gastric mucosal barrier Prostaglandin synthesis Mucus and bicarbonate secretion Submucosal blood flow Mucosal ATP Cell turnover Platelet function (irreversible)
Ivey KJ. Am J Med. 1988;84:41-48.
Ulkus antrum
Ulkus duodenum
gastropathy
Number of deaths 25,000 20,000
1997 US mortality data for seven selected disorders
The silent epidemic
16500
15,000 10,000 5000 0 NSAID
Singh G et al G. Epidemiology of NSAID-induced GI complications. J Rheumatol 1999;26:Sup 26:18-24.
Wolfe et al Gastrointestinal Toxicity of Nonsteroidal Antiinflammatory Drugs. NEJM 1999; 340: 1888-99.
Hospitalisations/1000 person-years 25 20 15 10 5 0 20 30 40 50 60 70 80
female users male users
male non-users female non-users
Age (years)
List of Available NSAIDs: Prescription & OTC
* List
* of trade names is not exhaustive
NON-SALICYLATES
Diclofenac (Voltaren) (Celebrex) Diclofenac/Misoprostol (Arthrotec) (Vioxx) Etodolac (Lodine) (Bextra) Fenoprofen (Nalfon) Flurbiprofen (Ansaid) Ibuprofen a,b,c (Motrin, Advil) Indomethacin (Indocin) Ketoprofen a,b,c(Orudis) Ketorolac (Toradol)c Meclofenamate Mefenamic acid (Ponstel) Meloxicam (Mobic) Nabumetone (Relafen) Naproxen a,b,c(Naprosyn, Anaprox) Oxaprozin (Daypro) Piroxicam (Feldene) Sulindac (Clinoril) Tolmetin (Tolectin)
SALICYLATES
Aspirin a,c (Zorprin, Easprin) Diflunisal (Dolobid) Salsalate (Disalcid, Salflex)
COX-2 INHIBITORS
Celecoxib Rofecoxib Valdecoxib
Choline salicylate (Trilisate) Magnesium salicylate (Magan)
Comments on Over-the-Counter Preparations:
a
Also available as OTC preparations in U.S. b OTC dose is usually half of prescribed dose C All OTC NSAIDs are non-selective COX Inhibitors
� � �
PPI (omeprazole 20-40mg 1x1/d) > PGE1, Misoprostol (cytotec 200 g 1x3/d) > H2 receptor antagonist (famotidine 40mg 1x2/d or ranitidine 300 mg 1x2/d) Misoprostol good for prevention of gastric ulcer but causes diarrhea
Algoritm of dyspeptic patients
Diagnosis and outcome assessment by
urea breath test (off PPIs) if endoscopy not required. Serology least sensitive and specific Therapy should be according to best practice, not ad hoc combinations If first line failure, dont retreat with the same combination- use proven 2nd line Rx Consider PPI prophylaxis selectively
Standard PPI based triple therapy : 7-14 days PPI, amoxicillin 1 g, clarithromycin 500 mg twice daily PPI, metronidazole 400 mg, clarithromycin 500 mg twice daily PPI, amoxicillin 1 g, metronidazole 400 mg twice daily 1 line therapy in Quadriple therapy: 714 days Asia PPI twice daily, bismuth 240 mg twice daily, metronidazole 400 mg twice daily or three times daily, tetracycline 500 mg four times daily Levofloxacin-based triple therapy: 10 days PPI, levofloxacin 250 mg (or 500 mg), amoxicillin 1 g twice daily Rifabutin-based triple therapy: 710 days PPI, rifabutin 150 mg, amoxicillin 1 g twice daily
st
Fock KM, et al. Journal of Gastroenterology and Hepatology 24 (2009) 15871600
Low NSAID gut risk
High NSAID gut risk Consider non-NSAID therapy or Non-selective NSAID + PPI or COX-II NSAID (PPI) or
Low CV risk (No aspirin)
Consider non-NSAID therapy Non-selective NSAID
H. pylori test and treat
High CV risk Consider non-NSAID therapy Consider non-NSAID therapy or Non-selective NSAID (naproxen) PPI or Non-selective NSAID + PPI or Avoid NSAIDs
(On aspirin)
Adapted from Fendrick. Am J Manag Care 2004; 10: 740-741 and Sung JGH 2010; 25: 229-33
H.pylori : the Maastricht III Consensus Report
Recommendations PU (active or inactive) including past bleeding: eradicate H pylori (includes prior to NSAID use) In nave users of NSAIDs (without prior PU), H pylori eradication may prevent peptic ulcer and or bleeding Chronic NSAID users: H pylori eradication of value but is insufficient to prevent NSAID related ulcers completely Long term NSAID users with PU and/or ulcer bleeding, PPI maintenance is better than H pylori eradication in preventing ulcer recurrence Level of evidence 1a 1b Grade of recommendation A A
1b
1b
Malfertheiner P et al. Gut 2007; 56: 772-78.
Second AsiaPacific Consensus Guidelines for Helicobacter pylori infection 2009
H. pylori infection should be tested for and eradicated: Prior to long-term aspirin or NSAID therapy in patients at high risk for ulcers and ulcer-related complications To reduce the risk of peptic ulcer and upper gastrointestinal bleeding in NSAID-naive users
Fock KM, et al. Journal of Gastroenterology and Hepatology 24 (2009) 15871600
Feature of Gastric acid secretion
Vous aimerez peut-être aussi
- Shahid Athar, MD, FACP, Face Author, "Islamic Perspective in Medicine" (ATP)Document25 pagesShahid Athar, MD, FACP, Face Author, "Islamic Perspective in Medicine" (ATP)She JocelynPas encore d'évaluation
- Diabetic ThyDocument18 pagesDiabetic ThyRina OktavianaPas encore d'évaluation
- Curriculum Vitae: Name OccupationDocument21 pagesCurriculum Vitae: Name OccupationShe JocelynPas encore d'évaluation
- Pain 2Document106 pagesPain 2She JocelynPas encore d'évaluation
- The Endocrine Glands & Their HormonesDocument35 pagesThe Endocrine Glands & Their HormonesShe JocelynPas encore d'évaluation
- The Endocrine Glands & Their HormonesDocument35 pagesThe Endocrine Glands & Their HormonesShe JocelynPas encore d'évaluation
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeD'EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeÉvaluation : 4 sur 5 étoiles4/5 (5794)
- The Yellow House: A Memoir (2019 National Book Award Winner)D'EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Évaluation : 4 sur 5 étoiles4/5 (98)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryD'EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryÉvaluation : 3.5 sur 5 étoiles3.5/5 (231)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceD'EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceÉvaluation : 4 sur 5 étoiles4/5 (895)
- The Little Book of Hygge: Danish Secrets to Happy LivingD'EverandThe Little Book of Hygge: Danish Secrets to Happy LivingÉvaluation : 3.5 sur 5 étoiles3.5/5 (400)
- Shoe Dog: A Memoir by the Creator of NikeD'EverandShoe Dog: A Memoir by the Creator of NikeÉvaluation : 4.5 sur 5 étoiles4.5/5 (537)
- Never Split the Difference: Negotiating As If Your Life Depended On ItD'EverandNever Split the Difference: Negotiating As If Your Life Depended On ItÉvaluation : 4.5 sur 5 étoiles4.5/5 (838)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureD'EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureÉvaluation : 4.5 sur 5 étoiles4.5/5 (474)
- Grit: The Power of Passion and PerseveranceD'EverandGrit: The Power of Passion and PerseveranceÉvaluation : 4 sur 5 étoiles4/5 (588)
- The Emperor of All Maladies: A Biography of CancerD'EverandThe Emperor of All Maladies: A Biography of CancerÉvaluation : 4.5 sur 5 étoiles4.5/5 (271)
- On Fire: The (Burning) Case for a Green New DealD'EverandOn Fire: The (Burning) Case for a Green New DealÉvaluation : 4 sur 5 étoiles4/5 (74)
- Team of Rivals: The Political Genius of Abraham LincolnD'EverandTeam of Rivals: The Political Genius of Abraham LincolnÉvaluation : 4.5 sur 5 étoiles4.5/5 (234)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaD'EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaÉvaluation : 4.5 sur 5 étoiles4.5/5 (266)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersD'EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersÉvaluation : 4.5 sur 5 étoiles4.5/5 (344)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyD'EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyÉvaluation : 3.5 sur 5 étoiles3.5/5 (2259)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreD'EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreÉvaluation : 4 sur 5 étoiles4/5 (1090)
- The Unwinding: An Inner History of the New AmericaD'EverandThe Unwinding: An Inner History of the New AmericaÉvaluation : 4 sur 5 étoiles4/5 (45)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)D'EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Évaluation : 4.5 sur 5 étoiles4.5/5 (121)
- Her Body and Other Parties: StoriesD'EverandHer Body and Other Parties: StoriesÉvaluation : 4 sur 5 étoiles4/5 (821)
- Antipyretic: Drugs FeverDocument3 pagesAntipyretic: Drugs Feverumesh123patilPas encore d'évaluation
- Whole Pharmacology ReviewDocument17 pagesWhole Pharmacology ReviewEslam khedrPas encore d'évaluation
- Ofertas Buen Fin SulkaDocument76 pagesOfertas Buen Fin SulkaCarlos QuirozPas encore d'évaluation
- 1Document6 pages1Cmo ClínicaPas encore d'évaluation
- Lecture 3Document51 pagesLecture 3Melanie HendricksPas encore d'évaluation
- Pesanan Obat ApotikDocument11 pagesPesanan Obat ApotikDPP aghnia rahmiPas encore d'évaluation
- Daftar Nama ObatDocument13 pagesDaftar Nama Obatnana rukanaPas encore d'évaluation
- USI Pharmaceuticals IPS, UVASDocument10 pagesUSI Pharmaceuticals IPS, UVASHamza TECHPas encore d'évaluation
- Antispastice: Feminost ClimenumDocument2 pagesAntispastice: Feminost ClimenumMagdalena TomaPas encore d'évaluation
- Cara Efektif Melakukan Stock OpnameDocument126 pagesCara Efektif Melakukan Stock OpnameDita PrimandariPas encore d'évaluation
- PHVP Stoc 17.11.2020Document81 pagesPHVP Stoc 17.11.2020Andreea AndraPas encore d'évaluation
- Pretest P4 Khasiat Dan Golongan Obat SlideDocument4 pagesPretest P4 Khasiat Dan Golongan Obat SlideAFRINA FAJAR EKOWATIPas encore d'évaluation
- Nsaids BcqsDocument1 pageNsaids BcqsDR AbidPas encore d'évaluation
- 19 FebDocument2 pages19 FebNlm NaulakPas encore d'évaluation
- Images: All Videos Books News Maps FlightsDocument1 pageImages: All Videos Books News Maps FlightsChan ParinaPas encore d'évaluation
- Clinical Pathway Kejang DemamDocument2 pagesClinical Pathway Kejang Demambety_jalanita6382Pas encore d'évaluation
- Daftar Obat NaritaDocument45 pagesDaftar Obat NaritaHidayatulloh AriefPas encore d'évaluation
- Daftar Obat Zenith: Gol - AntibiotikaDocument3 pagesDaftar Obat Zenith: Gol - AntibiotikaNetriPas encore d'évaluation
- Daftar Obat Ethical FixDocument4 pagesDaftar Obat Ethical FixPanjalu YudaprajaPas encore d'évaluation
- Devi Ratnasari - Obat Golongan NSAIDDocument2 pagesDevi Ratnasari - Obat Golongan NSAIDDevi RatnasariPas encore d'évaluation
- Eximpulse PARACETAMOLDocument96 pagesEximpulse PARACETAMOLShantanu MannaPas encore d'évaluation
- Drug Table ChairDocument11 pagesDrug Table ChairAnonymous HH3c17osPas encore d'évaluation
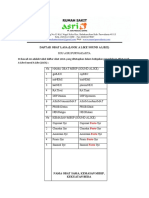
- Daftar Obat Lasa (Look A Like Sound A Like) : Forte Forte Forte Forte ForteDocument3 pagesDaftar Obat Lasa (Look A Like Sound A Like) : Forte Forte Forte Forte ForteNeng Tina PSPas encore d'évaluation
- Bola CommunityDocument5 pagesBola CommunityOladimeji Raphael OnibonPas encore d'évaluation
- Lista 15-01-2024 Drogueria BaronDocument198 pagesLista 15-01-2024 Drogueria Baronangel duranPas encore d'évaluation
- Resep Masuk TGL 12 Juni 2020Document8 pagesResep Masuk TGL 12 Juni 2020mirayelli bulkisPas encore d'évaluation
- Form Data Resep Inap BPJS Februari 2019Document42 pagesForm Data Resep Inap BPJS Februari 2019Muh ZakaPas encore d'évaluation
- No. Nama Obat Jumlah (Satuan/Kemasan) Total HargaDocument24 pagesNo. Nama Obat Jumlah (Satuan/Kemasan) Total HargaGusti KurniaPas encore d'évaluation
- Cotrimoxazole SyDocument4 pagesCotrimoxazole Syshanti apriyanthiPas encore d'évaluation
- Stock 20.06.22Document25 pagesStock 20.06.22dian elokPas encore d'évaluation