Académique Documents
Professionnel Documents
Culture Documents
Natriuresis
Transféré par
Erin TrianaCopyright
Formats disponibles
Partager ce document
Partager ou intégrer le document
Avez-vous trouvé ce document utile ?
Ce contenu est-il inapproprié ?
Signaler ce documentDroits d'auteur :
Formats disponibles
Natriuresis
Transféré par
Erin TrianaDroits d'auteur :
Formats disponibles
Natriuresis induced by mild hypernatremia in humans.
Andersen LJ, Andersen JL, Pump B, Bie P. Source
Department of Medical Physiology, Panum Institute, University of Copenhagen, DK2200 Copenhagen, Denmark.
Abstract
The hypothesis that increases in plasma sodium induce natriuresis independently of changes in body fluid volume was tested in six slightly dehydrated seated subjects on controlled sodium intake (150 mmol/day). NaCl (3.85 mmol/kg) was infused intravenously over 90 min as isotonic (Iso) or as hypertonic saline (Hyper, 855 mmol/l). After Hyper, plasma sodium increased by 3% (142.0 +/- 0.6 to 146.2 +/- 0.5 mmol/l). During Iso a small decrease occurred (142.3 +/- 0.6 to 140.3 +/- 0.7 mmol/l). Iso increased estimates of plasma volume significantly more than Hyper. However, renal sodium excretion increased significantly more with Hyper (291 +/- 25 vs. 199 +/- 24 micromol/min). This excess was not mediated by arterial pressure, which actually decreased slightly. Creatinine clearance did not change measurably. Plasma renin activity, ANG II, and aldosterone decreased very similarly in Iso and Hyper. Plasma atrial natriuretic peptide remained unchanged, whereas plasma vasopressin increased with Hyper (1.4 +/- 0.4 to 3.1 +/0.5 pg/ml) and decreased (1.3 +/- 0.4 to 0.6 +/- 0.1 pg/ml) after Iso. In conclusion, the natriuretic response to Hyper was 50% larger than to Iso, indicating that renal sodium excretion may be determined partly by plasma sodium concentration. The mechanism is uncertain but appears independent of changes in blood pressure, glomerular filtration rate, the renin system, and atrial natriuretic peptide.
PMID: 12010758 [PubMed - indexed for MEDLINE]
Studies on the Mechanism of Hypernatriuresis in Essential Hypertension in Relation to Measurements of Plasma Renin Concentration, Body Fluid Compartments and Renal Function
M. A. D. H. Schalekamp, X. H. Krauss, M. P. A. Schalekamp Kuyken, G. Kolsters and W. H. Birkenhger Department of Internal Medicine, Zuiderziekenhuis, Rotterdam
Correspondence: Dr W. H. Birkenhger, Zuiderziekenhuis, Groeneveld 15, Rotterdam, Netherlands.
1. In twenty-two patients representing different stages of benign essential hypertension, hyperosmotic saline was administered intravenously. Determinations of intra-arterial pressure, renal plasma flow, glomerular filtration rate and plasma renin concentration were carried out before and, in the majority, also during and after saline infusion. Changes in cardiac output were followed in ten patients. Plasma volume and extracellular volume were determined in the control period only, although haemodilution was assessed by haematocrit readings. 2. Excess of sodium excretion showed a wide range and was related to the patient's age, as well as to a set of parameters reflecting intrarenal pressure patterns; hypernatriuresis consistently occurred in older patients, in whom renal vascular resistance and nitration fraction were elevated and plasma renin was suppressed. It could not be clarified whether hypernatriuresis together with renin suppression were determined by intrarenal pressure relationships or by an independent age-related factor in the hypertensive patient. 3. Excess of sodium excretion was not related to increments in arterial pressure, cardiac output, renal blood flow or glomerular filtration rate. 4. Plasma renin concentration failed to show consistent changes after hyperosmotic saline infusion. 5. It is concluded that natriuresis is not mediated by changes in the activity of the renin-angiotensin system. Hypernatriuresis appears to be a feature of progressive benign hypertension.
On the renal basis for essential hypertension: nephron heterogeneity with discordant renin secretion and sodium excretion causing a hypertensive vasoconstriction-volume relationship.
Sealey JE, Blumenfeld JD, Bell GM, Pecker MS, Sommers SC, Laragh JH. Source
Cardiovascular Center, New York Hospital-Cornell Medical Center, New York, New York 10021.
Abstract
We propose herein that there are two functionally abnormal nephron populations in essential hypertension: (1) a group of ischemic nephrons with impaired sodium excretion which chronically hypersecrete renin. Numerically, these ischemic nephrons comprise a minor subgroup since most patients with essential hypertension exhibit no overt evidence of renal insufficiency. (2) In reaction to this, a more numerous group of normal nephrons appears in adaptive hypernatriuresis. They have an increased distal sodium supply and consequently, a chronically suppressed renin secretion. One difference between patients with
renovascular hypertension and those with essential hypertension is the intermingling of these two populations of nephrons. In our hypothesis, the adapting hyperfiltering normal nephrons accomplish the hypernatriuresis in response to saline infusion, that is characteristic of all essential hypertension. However, the unsuppressed secretion of renin, that arises from the ischemic nephron population attenuates this compensatory natriuresis in the following ways: (1) by inappropriately acting on the hyperfiltering nephrons to enhance proximal tubular sodium reabsorption; (2) by activating TGF-mediated afferent constriction in these nephrons, and (3) simultaneously, the reactive secretion of renin from ischemic nephrons is diluted by non-participation of the adapting hypernatriuretic nephrons so that plasma renin settles at a level which is insufficient to fully compensate GFR in the ischemic nephrons. These adaptive responses provide a basis for the observation that the inhibition of renin activity with converting enzyme inhibitors in essential hypertension increases renal blood flow and sodium excretion. They also explain why converting enzyme inhibitors can effectively reduce blood pressure, even when renin levels are not absolutely elevated, since any circulating renin imposed upon the adapting hypernatriuretic nephrons inappropriately impairs their sodium excretion. In addition, the theory explains why basal renin secretion is either not suppressed or inadequately suppressed in patients with essential hypertension. As a result, whole kidney homeostatic function is compromised because individual nephrons are responding to their individual stimuli to fulfil their individual need, rather than acting in concert with other nephrons. The net effect of this uncoordinated response is to shift total renal function so that systemic arterial hypertension is sustained by abnormal sodium retention for the inappropriately high plasma renin level, or vice versa.(ABSTRACT TRUNCATED AT 400 WORDS)
Vous aimerez peut-être aussi
- Shoe Dog: A Memoir by the Creator of NikeD'EverandShoe Dog: A Memoir by the Creator of NikeÉvaluation : 4.5 sur 5 étoiles4.5/5 (537)
- Grit: The Power of Passion and PerseveranceD'EverandGrit: The Power of Passion and PerseveranceÉvaluation : 4 sur 5 étoiles4/5 (587)
- Jurnal MataDocument8 pagesJurnal MataErin TrianaPas encore d'évaluation
- Genetic and Epigenetic Factors Contribute To Activation of The Mucosal Immune System After Antigen ExposureDocument1 pageGenetic and Epigenetic Factors Contribute To Activation of The Mucosal Immune System After Antigen ExposureErin TrianaPas encore d'évaluation
- Genetic and Epigenetic Factors Contribute To Activation of The Mucosal Immune System After Antigen ExposureDocument1 pageGenetic and Epigenetic Factors Contribute To Activation of The Mucosal Immune System After Antigen ExposureErin TrianaPas encore d'évaluation
- JOURNAL Emergency Airway ManagementDocument8 pagesJOURNAL Emergency Airway ManagementErin Triana0% (1)
- SinobrokialDocument15 pagesSinobrokialErin TrianaPas encore d'évaluation
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceD'EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceÉvaluation : 4 sur 5 étoiles4/5 (890)
- The Yellow House: A Memoir (2019 National Book Award Winner)D'EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Évaluation : 4 sur 5 étoiles4/5 (98)
- The Little Book of Hygge: Danish Secrets to Happy LivingD'EverandThe Little Book of Hygge: Danish Secrets to Happy LivingÉvaluation : 3.5 sur 5 étoiles3.5/5 (399)
- On Fire: The (Burning) Case for a Green New DealD'EverandOn Fire: The (Burning) Case for a Green New DealÉvaluation : 4 sur 5 étoiles4/5 (73)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeD'EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeÉvaluation : 4 sur 5 étoiles4/5 (5794)
- Never Split the Difference: Negotiating As If Your Life Depended On ItD'EverandNever Split the Difference: Negotiating As If Your Life Depended On ItÉvaluation : 4.5 sur 5 étoiles4.5/5 (838)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureD'EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureÉvaluation : 4.5 sur 5 étoiles4.5/5 (474)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryD'EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryÉvaluation : 3.5 sur 5 étoiles3.5/5 (231)
- The Emperor of All Maladies: A Biography of CancerD'EverandThe Emperor of All Maladies: A Biography of CancerÉvaluation : 4.5 sur 5 étoiles4.5/5 (271)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreD'EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreÉvaluation : 4 sur 5 étoiles4/5 (1090)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyD'EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyÉvaluation : 3.5 sur 5 étoiles3.5/5 (2219)
- Team of Rivals: The Political Genius of Abraham LincolnD'EverandTeam of Rivals: The Political Genius of Abraham LincolnÉvaluation : 4.5 sur 5 étoiles4.5/5 (234)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersD'EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersÉvaluation : 4.5 sur 5 étoiles4.5/5 (344)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaD'EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaÉvaluation : 4.5 sur 5 étoiles4.5/5 (265)
- The Unwinding: An Inner History of the New AmericaD'EverandThe Unwinding: An Inner History of the New AmericaÉvaluation : 4 sur 5 étoiles4/5 (45)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)D'EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Évaluation : 4.5 sur 5 étoiles4.5/5 (119)
- Her Body and Other Parties: StoriesD'EverandHer Body and Other Parties: StoriesÉvaluation : 4 sur 5 étoiles4/5 (821)
- Simple Squamous: Epithelial Tissue A. Simple /unstratified SINGLE LAYER OF CELLS IDocument5 pagesSimple Squamous: Epithelial Tissue A. Simple /unstratified SINGLE LAYER OF CELLS IMedical HardikPas encore d'évaluation
- Collins - Integrated Science For The Caribbean 3 PDFDocument233 pagesCollins - Integrated Science For The Caribbean 3 PDFIn need67% (15)
- Urinary System: Tsedalu Yirsa (DVM, MSC, Assist Prof.)Document18 pagesUrinary System: Tsedalu Yirsa (DVM, MSC, Assist Prof.)Mohammed OumerPas encore d'évaluation
- Urine TestsDocument398 pagesUrine TestsAliMohamad100% (1)
- Lab Report Bio560Document39 pagesLab Report Bio560Syar QamPas encore d'évaluation
- RAAS: (Renin Angiotensin Aldosterone System) : How Does This System Work?Document3 pagesRAAS: (Renin Angiotensin Aldosterone System) : How Does This System Work?Sameen FatimaPas encore d'évaluation
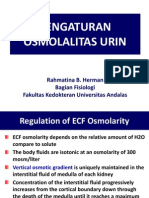
- Kuliah 3. Pengaturan Osmolalitas UrinDocument19 pagesKuliah 3. Pengaturan Osmolalitas UrinAnnisa DamayantiPas encore d'évaluation
- Cardiovascular System: Anatomy and Functions of the Heart, Blood Vessels, Blood Circulation, and Regulation of Blood Pressure</TITLEDocument85 pagesCardiovascular System: Anatomy and Functions of the Heart, Blood Vessels, Blood Circulation, and Regulation of Blood Pressure</TITLEEbrahem ShaheinPas encore d'évaluation
- MCAT Content Outline TrackerDocument83 pagesMCAT Content Outline TrackerNoelani-Mei AscioPas encore d'évaluation
- Case Study: Acute GlomerulonephritisDocument28 pagesCase Study: Acute GlomerulonephritisMa Rafaela Rosales Palompon91% (11)
- SLCC Anatomy CH 27: Urinary System: Study Online atDocument2 pagesSLCC Anatomy CH 27: Urinary System: Study Online atBrendaJooYeePas encore d'évaluation
- Zoology II (Em) BLM 21-22Document99 pagesZoology II (Em) BLM 21-22GANESH KANDAGATLAPas encore d'évaluation
- (PHYSIO B) 1.2 Renal Physio Pt. 3Document8 pages(PHYSIO B) 1.2 Renal Physio Pt. 3miguel cuevasPas encore d'évaluation
- HomeostasisDocument30 pagesHomeostasisSana MostofaPas encore d'évaluation
- Chapter One A CellDocument46 pagesChapter One A CellLeon MarkoPas encore d'évaluation
- Biomarkers in Progressive Chronic Kidney Disease. Still A Long Way To GoDocument13 pagesBiomarkers in Progressive Chronic Kidney Disease. Still A Long Way To GoconstanzanazarethPas encore d'évaluation
- CARDIODocument38 pagesCARDIOAishwarya Bharath100% (1)
- Function of The Renal and Urinary Tract System: Medical-Surgical Nursing, 4/eDocument117 pagesFunction of The Renal and Urinary Tract System: Medical-Surgical Nursing, 4/eBryJos tiongsonPas encore d'évaluation
- Grade 10 CH 6 Assertion Reason QuestionsDocument5 pagesGrade 10 CH 6 Assertion Reason QuestionsVidhun 8APas encore d'évaluation
- Robert W Schrier Atlas of Diseases of The Kidney PDFDocument178 pagesRobert W Schrier Atlas of Diseases of The Kidney PDFdanPas encore d'évaluation
- Expression Profiling of Fibroblasts in Chronic And.11Document15 pagesExpression Profiling of Fibroblasts in Chronic And.11Arista RachmaPas encore d'évaluation
- Anatomi Dan Fisiologi GinjalDocument32 pagesAnatomi Dan Fisiologi GinjalAlamul Huda100% (1)
- 2008 Kedah SPM Biology AnsDocument24 pages2008 Kedah SPM Biology Ansjee2kkPas encore d'évaluation
- David Shier - Ricki Lewis - Jackie Butler - Hole's Human Anatomy & Physiology-Mcgraw Hill Education (2019)Document1 025 pagesDavid Shier - Ricki Lewis - Jackie Butler - Hole's Human Anatomy & Physiology-Mcgraw Hill Education (2019)stephcruz0726Pas encore d'évaluation
- Nephrotic Syndrome GuideDocument12 pagesNephrotic Syndrome GuidePutra Fatkhul Rizqi QoroidPas encore d'évaluation
- G-10 Biology, 3.5 HomeostasisDocument11 pagesG-10 Biology, 3.5 Homeostasisjohn nigussiePas encore d'évaluation
- BMAT 2022 Section 2 Question PaperDocument24 pagesBMAT 2022 Section 2 Question PaperGeorge ChanPas encore d'évaluation
- Excretion ProcessDocument3 pagesExcretion ProcessRatheesh HrishikeshPas encore d'évaluation
- Diuretic Drugs Review QuestionsDocument30 pagesDiuretic Drugs Review QuestionsSagar KhairwalPas encore d'évaluation
- Anatomi Fisiologi Sistem PerkemihanDocument65 pagesAnatomi Fisiologi Sistem PerkemihanMakkatul HikmahPas encore d'évaluation