Académique Documents
Professionnel Documents
Culture Documents
Bays Adisopathy
Transféré par
Chikezie OnwukweCopyright
Formats disponibles
Partager ce document
Partager ou intégrer le document
Avez-vous trouvé ce document utile ?
Ce contenu est-il inapproprié ?
Signaler ce documentDroits d'auteur :
Formats disponibles
Bays Adisopathy
Transféré par
Chikezie OnwukweDroits d'auteur :
Formats disponibles
10.1517/14796678.1.1.
39 2004 Future Medicine Ltd ISSN 1479-6678 Future Cardiology (2005) 1(1), 3959 39
REVI EW
For reprint orders, please contact:
reprints@futuremedicine.com
Adiposopathy: sick fat causes high blood
sugar, high blood pressure and dyslipidemia
Harold Bays MD, FACP
,
Nicola Abate MD,
Manisha Chandalia MD
Author for correspondence
Medical Director/President
L-MARC Research Center
Louisville KY, USA
hbaysmd@aol.com
Keywords: adipose
autodysharmonia, adiposopathy,
diabetes, Food and Drug
Administration, hypertension,
obesity metabolic cycle,
metabolic syndrome, obesity,
regulatory
Adiposopathy is defined as pathological adipose tissue function that may be promoted and
exacerbated by fat accumulation (adiposity) and sedentary lifestyle in genetically
susceptible patients. Adiposopathy is a root cause of some of the most common metabolic
diseases observed in clinical practice, including Type 2 diabetes mellitus, hypertension and
dyslipidemia. The most common term for the metabolic consequences of adiposopathy is
currently the metabolic syndrome. Drug usage to treat the metabolic syndrome has focused
on the safety and efficacy of treatments directed towards individual components of the
metabolic syndrome, and not so much upon adiposopathy itself. However, enough is known
about the pathophysiology of adiposopathy to propose diagnostic criteria. Regulatory issues
are important obstacles to the research and development of new drug treatments for the
metabolic syndrome. It is hoped that these obstacles can, to some extent, be addressed and
overcome by clearly defining and increasing our understanding of adiposopathy.
It is well known amongst clinicians that
genetically predisposed patients who acquire
excess body fat and maintain a sedentary lifestyle
are at increased risk of developing a number of
disease states [1], many which constitute impor-
tant atherosclerotic coronary heart disease (CHD)
risk factors that may lead to CHD events
(Figure 1). Among the more common metabolic
disorders often associated with excessive body fat
are abnormalities of glucose metabolism (such as
diabetes mellitus), hypertension and dyslipidemia.
However, the relationship between excessive body
fat and adverse metabolic consequences is not
absolute. Obesity alone does not always result in
clinical metabolic disease, and not all patients
with these metabolic diseases are overweight.
Recent and ongoing research into adipose func-
tion and dysfunction seem to be confirming these
basic and common clinical observations. Studies
are now supporting the concept that it is not the
presence of excess adipose tissue alone, adiposity,
that is causally related, but rather it is the dysfunc-
tion of adipose tissue, here termed adiposopathy,
that should be identified as the root mechanistic
etiology of disorders of glucose metabolism, blood
pressure and lipid metabolism. The implications
of this alteration in emphasis is certainly of signif-
icance for mechanistic research, and is also of great
practical significance for the clinician.
Adiposopathy: replacing the term
metabolic syndrome
Many authors and scientific organizations have
characterized and applied terminology to the
constellation of metabolic abnormalities often
associated with the accumulation of excessive
body fat. Unfortunately, not everyone agrees on
any particular characterization, nor do they
always agree upon the definition.
For example, the most common current term
that refers to the cluster of metabolic
abnormalities associated with disorders in glucose
metabolism, hypertension and dyslipidemia is the
metabolic syndrome. A similar clinical presenta-
tion has also been termed atherothrombogenic
syndrome, beer-belly syndrome, cardiovascular
metabolic syndrome, chronic cardiovascular risk
factor clustering syndrome, deadly quartet (obes-
ity, hyperinsulinemia, hypertension and dyslipi-
demia), disharmonious quartet, dysmetabolic
syndrome, dysmetabolic syndrome X, insulin
resistance syndrome, insulin resistance-dyslipi-
demia syndrome, metabolic cardiovascular syn-
drome, metabolic syndrome, metabolic syndrome
X, multiple metabolic syndrome, plurimetabolic
syndrome, Reavens syndrome, and syndrome X
[24]. The variety of different terms for a similar or
related condition reflects the difficulty in applying
one name to a constellation of related, and some-
times unrelated metabolic abnormalities, and
reflects an unsatisfying attempt to identify one
root pathophysiologic cause of all of these.
Futher complicating the matter is that differ-
ing organizations have different definitions for
the same condition. The National Cholesterol
Education Program, Adult Treatment Panel III
(NCEP ATP III) [5] and the World Health
Organization (WHO) [6] have established the
most widely used definitions of the metabolic
syndrome (Table 1). The criteria differ in many
REVI EW Bays, Abate & Chandalia
40 Future Cardiology (2005) 1(1)
respects; for example, while waist circumference
is a criteria included in the NCEP ATP III defi-
nition, waist:hip ratio or body mass index (BMI)
ratio is used in the WHO definition. The NCEP
ATP III definition does not include glucose
intolerance or insulin resistance, while these are
important criteria in the WHO definition. The
NCEP ATP III does not include albuminuria,
while this is a criteria recommended by WHO.
The differing nomenclature and criteria for
diagnosis is not without consequence. Obesity is
the most common metabolic disease in
developed nations. According to the WHO, over
1 billion adults are overweight on a worldwide
basis, with at least 300 million being obese [101].
In the USA, the unabated epidemic of obesity is
now such that over 30% of adults are obese and
over 60% of adults are either overweight or obese
[7]. Of equal concern is that the high prevalence
of obesity among children and adolescents con-
tinues to increase a trend that suggests that the
obesity epidemic will continue to increase in the
future [8]. Largely as a consequence of the obesity
epidemic, the increased prevalence of the meta-
bolic syndrome might also be considered an
epidemic in that it has been estimated that at
least 47 million adults (22% of the population)
in the USA are affected [9].
Figure 1. Adiposity and adiposopathy in the development of atherosclerotic coronary artery disease [2].
Short-term release of free fatty acids (FFAs) may increase pancreatic insulin release. Chronic, long-term FFA exposure may result in decreased
insulin secretion.
Positive caloric balance
Genetic predisposition
Sedentary lifestyle
Adiposity and adiposopathy
Increased release of FFA
Release of adipocyte hormones,
adipokines, and other factors
Insulin resistance:
(1) Skeletal muscle
(genetically predisposed)
Insulin resistance:
(2) Liver
(genetically predisposed)
(3) Pancreatic -cells
(genetically predisposed)
Hyperglycemia Hyperglycemia
Hyperglycemia
dyslipidemia
Decreased release of insulin
:
Lumen
Damaged vessel
Atherosclerotic plaque
Vascular damage
www.futuremedicine.com 41
Adiposopathy REVI EW
Given the enormity of this disease burden and
the known public health consequences, it would
seem reasonable that extraordinary efforts be
made towards preventing, treating, and poten-
tially curing the metabolic syndrome. However,
the conduct and reporting of clinical trials to
demonstrate efficacy in the treatment of the
metabolic syndrome have been hampered by the
lack of consistent terminology, the lack of
uniform diagnostic definitions and the different
criteria reported in different clinical studies. For
example, in recognition that increased body fat is
often directly related to the development of the
metabolic syndrome, investigators have often
substituted BMI for measurement of waist cir-
cumference, which is a listed criteria according
to the NCEP ATP. Sometimes, the substitution
cutoff value has been greater than 30 kg/m
2
,
while at other times greater than 25 kg/m
2
has
been used [2]. This is because from a practical
standpoint, BMI is routinely obtained in clinical
trials, while waist circumference is not.
Further complicating the matter is that not all
clinicians are clear on the similarities and
differences between the metabolic syndrome and
other associated conditions. Not all clinicians are
aware that patients with Type 2 diabetes may or
may not have metabolic syndrome, and patients
with metabolic syndrome may or may not have
diabetes. Moreover, even researchers are not cer-
tain whether insulin resistance syndrome and
metabolic syndrome are the same, or have the
same treatment goals [3].
In addition, the criteria to define the
metabolic syndrome is largely based on
epidemiological and cross-sectional observations
mainly obtained in European descent popula-
tion, and were subsequently generalized to vari-
ous ethnic groups. Subsequent studies have
revealed that aspects of the metabolic syndrome
profoundly differ among ethnic groups. Even
within the European descent populations, there
are additional features of the metabolic syn-
drome that could be a better predictor of risk of
metabolic and CHD risk.
It is also noteworthy that the scientific
organizations that have defined metabolic
syndrome have not required that the components
of the metabolic syndrome be due to any unifying
and underlying metabolic process. Yet an increase
in abdominal girth, hypertriglyceridemia, low
high-density lipoprotein cholesterol (HDL-C)
levels, high blood pressure and elevated glucose
can all individually be the result of diseases and
conditions that are entirely unrelated to one
another, and thus not reasonably be connected to
any one causality or syndrome. This may help to
explain why the diagnosis of the metabolic syn-
drome may not be a predictor of 11 year CHD
mortality among patients with Type 2 diabetes
mellitus, and its diagnosis may not provide further
predictive value compared with knowledge of its
Table 1. Comparison of NCEP ATP III and WHO criteria for
Metabolic Syndrome.
NCEP ATP III
Three or more of the following must be present:
Waist circumference
Men
Women
> 102 cm (>40 inches)
> 88 cm (>35 inches)
Plasma TG Men/women 1.7 mmol/L ( 150 mg/dL)
Plasma HDL cholesterol Men
Women
< 1.0 mmol/L (< 40 mg/dL)
< 1.3 mmol/L (<50 mg/dL)
Blood pressure Men/women 130/ 85 mmHg
Fasting blood glucose Men/women 6.1 mmol/L ( 110 mg/dL)
WHO
At least one of the following must be present:
Impaired fasting
glycemia
Men/women 6.1 mmol/L ( 110 mg/dL) and
< 7.0 mmol/L (< 126 mg/dL)
Impaired glucose
tolerance
Fasting
Post-load
< 7.0 mmol/L (< 126 mg/dL) and
7.8 mmol/L (140 mg/d:L)
Diabetes Fasting
Post-load
7.0 mmol/L ( 126 mg/dL)
11.1 mmol/L ( 200 mg/dL)
Insulin resistance Men/women Glucose uptake below lowest
quartile for background
population under investigation
In addition, two or more of the following:
Arterial blood pressure Men/women 140/90 mmHg
Lipid abnormalities:
Plasma TG
or
Plasma HDL cholesterol
Men/women
Men
Women
1.7 mmol/L ( 150 mg/dL)
< 0.9 mmol/L (<35 mg/dL)
< 1.0 mmol/L (<39 mg/dL)
Central obesity:
Waist:hip ratio
or
BMI
Men
Women
Men/women
> 0.9
> 0.85
> 30 kg/m
2
Microabuminuria:
Urinary albumin
excretion rate
or
Albumin:creatinine ratio
Men/women
Men/women
20 g/min
30 mg/g
In Asian populations, these values are commonly revised to a waist circumference in
men and women of 90 cm and 80 cm, respectively.
See Lancet 363, 157163 (2004) for the WHO BMI definition for Asians.
BMI: Body Mass Index; HDL: High-density lipoprotein; NCEP ATP: National Cholesterol
Education Program Adult Treatment Panel; TG: Triglyceride; WHO: World Health
Organization. (Reprinted with permission from [2] by permission of Cambridge
Medical Publications, all rights reserved).
REVI EW Bays, Abate & Chandalia
42 Future Cardiology (2005) 1(1)
single components [10]. In fact, even in patients
without diabetes mellitus, diagnosis of the
metabolic syndrome appears to be inferior to
established prediction models for either Type 2
diabetes or CHD, such as the Diabetes Predicting
Model and Framingham Risk Score [11].
The bottomline is that most clinicians know
from their clinical practice experience that select
patients with the metabolic syndrome are at high
risk for development of atherosclerotic CHD and
diabetes mellitus. To some extent, these conse-
quences are supported in the medical literature
[12]. Clinicians also have the intuitive sense that a
long-term commitment towards treating these
multiple metabolic risk factors improves the
health of their patients, which is again supported
by the medical literature [13]. However, while reg-
ulatory agencies such as the US Food and Drug
Administration (FDA) recognize the existence of
the metabolic syndrome, they have yet to estab-
lish criteria in order to grant an indication for its
treatment. This lack of indication criteria for the
treatment of the metabolic syndrome impairs the
development of pharmaceutical agents to treat the
underlying root cause and/or pathophysiology,
and instead promotes continued research efforts
focusing on drug treatment for the components
of the metabolic syndrome. In other words, while
specific regulatory criteria exists for granting
approval for an indication for treatment of the
components of the metabolic syndrome (such as
Type 2 diabetes mellitus, hypertension and dysli-
pidemia), no such approvable indication criteria
exists for treatment of the metabolic syndrome
itself, that often reflects underlying metabolic
processes that may promote these conditions.
Accumulating scientific data suggest that in
most patients, it is the dysfunction of adipose tis-
sue (adiposopathy) that is the root mechanistic
aetiology of abnormalities of glucose metabolism,
blood pressure and lipid metabolism (Figure 1).
These scientific data are substantiated by the com-
mon clinical observation that many patients who
gain weight develop these metabolic abnormali-
ties, and if these same patients subsequently lose
weight, then these metabolic abnormalities
improve or may potentially resolve. If it becomes
generally accepted that dysfunction of adipose tis-
sue is the root mechanistic pathophysiologic etiol-
ogy of the metabolic abnormalities that compose
the metabolic syndrome in the majority of
patients, then it may be time to replace the term
metabolic syndrome (a term largely reflective of
sometimes unrelated consequence), and replace it
with adiposopathy (a term more focused on
unified underlying causality). It may then be time
to focus on adiposopathy as a primary treatment
target, and to establish clear criteria for its diagno-
sis, and for granting an indication for its treat-
ment. It may be time to acknowledge that
adiposopathy is not only a disease, but a genetic
disease state of a specific organ that:
Can be worsened by poor dietary and lifestyle
habits, concurrent diseases, and perhaps cer-
tain drugs, such as corticoid steroids and some
psychotropic drugs [1];
A disease that leads to significant morbidity
and mortality;
A disease that can be improved with favorable
dietary and lifestyle habits and pharmaceutical
agents; and
A disease whose correction will decrease
morbidity and mortality
Subsequently, clinical trials can be better
designed and directed towards establishing a
more rational direction of treatment compared
with the current focus upon the often unrelated
components of the metabolic syndrome.
Sick fat (adiposopathy) causes Type 2
diabetes mellitus
Overall, only approximately 12% of US adult
patients with a BMI 27 kg/m
2
have Type 2
diabetes mellitus [102]. Conversely, 67% of US
patients diagnosed with Type 2 diabetes mellitus
have a BMI 27 kg/m
2
, while 46% have a BMI
greater than 30 kg/m
2
[103]. Thus, not all patients
who are overweight have Type 2 diabetes mellitus,
in fact only a minority do, (Figure 2) and not all
patients with Type 2 diabetes mellitus are over-
weight, although the majority are. Therefore,
while excessive body fat clearly increases the risk of
Type 2 diabetes mellitus, excess body fat alone is
not sufficient towards development of Type 2 dia-
betes mellitus.
Admittedly, adiposopathy is not the only
cause of Type 2 diabetes mellitus. Other causes
would include metabolic disorders that affect
pancreatic function, such as some cases of hemo-
chromatosis and chronic pancreatitis. Known
metabolic abnormalities that might directly pro-
mote insulin resistance include hypercortisolism,
excessive growth hormone and hyperthyroidism.
Furthermore, certain populations exist that may
have an inherent decrease in pancreatic function.
However, for the majority of patients it is
reasonable to conclude that it is the combination
of adiposity, genetic predisposition and perhaps a
sedentary lifestyle that leads to fat dysfunction,
www.futuremedicine.com 43
Adiposopathy REVI EW
and it is this adiposopathy that results in Type 2
diabetes mellitus (Figure 1).
While in the past adipose tissue was thought
to mainly function as an inert storage organ,
adipose tissue is now known to be a very active
organ from many metabolic standpoints (Table 2)
[14]. Several fat-derived metabolites, hormones,
enzymes, cytokines and other factors may have
varying degrees of effects upon the activity of
insulin, including the induction of insulin
resistance (Table 3) [15,16].
One of the most well-described consequences
of adiposopathy, if not one of the most well-
described results of abnormal fat function, is the
abnormal increase in the fasting and postpran-
dial release of nonesterified or free fatty acids
(FFAs) [15]. Short-term (2 to 6 h) elevations in
FFA levels may enhance insulin secretion.
However, longer term FFA exposure is detrimen-
tal, and may result in insulin resistance in the
liver and muscle, as well as diminished
pancreatic -cell insulin production which has
sometimes been termed lipotoxicity [15]. The
excessive release of FFA from fat cells appears to
be more prevalent in patients genetically
predisposed to development of Type 2 diabetes
mellitus, and a reduction in FFA levels has been
shown to improve insulin activity [15].
In addition to the abnormal release of FFA,
adiposopathy is also manifest by the abnormal
release of cytokines and other factors that con-
tribute to diminished insulin activity (Table 3).
Finally, adiposopathy often appears to be mani-
fested by not only abnormalities in fat function,
but also abnormalities in fat distribution.
Patients with visceral, upper body fat (android)
distribution tend to have more insulin resistance
and hyperinsulinemia compared with those with
more lower body fat (gynoid) [15]. In fact, it
might be argued that the accumulation of vis-
ceral and subcutaneous truncal fat reflects a dys-
functional adipose organ, and is a gross
anatomical manifestation of adiposopathy.
Just as there is great variance in the
functionality and dysfunctionality of adipose
tissue, there is also variance in the distribution of
Figure 2. Prevalence of common weight-related metabolic diseases based upon
body mass index [102,104].
Tested fasting plasma glucose of equal to or greater than 126 mg/dl or self-reported as having responded
positively to "Have you ever been told by a doctor that you have diabetes or sugar diabetes?" Excludes
gestational and Type 1 diabetes.
Tested BP of equal to or greater than 140 mmHg systolic or 90 mmHg diastolic or selfreported as having
responded positively to "Have you ever been told by a doctor or health professional that you had
hypertension, also called high blood pressure?"
Tested total cholesterol of 240 mg/dl or self-reported as having responded positively to "Have you ever
been told by a doctor or health professional that your blood cholesterol level was high?"
BMI: Body mass index.(Reprinted with permission from [2] by permission of Cambridge Medical Publications, all
rights reserved).
Type 2 diabetes
Hypertension
Hypercholesterolemia
0
10
20
30
40
50
60
%
o
f
a
d
u
l
t
s
b
y
B
M
I
c
a
t
e
g
o
r
y
BMI (kg/m
2
)
18.524.9 25.026.9 27.029.9 30.034.9 35
Comorbidities increase with increasing BMI
REVI EW Bays, Abate & Chandalia
44 Future Cardiology (2005) 1(1)
body fat among individuals and populations, and
adipose tissue function and distribution are
related. For example, some obese patients are
metabolically healthy, and have been
characterized as metabolically healthy, but obese
(MHO). [17]. These obese patients appear to be
protected or resistant [17] to the typical
metabolic consequences often associated with
excess body fat. It has been suggested that MHO
is not an unusual presentation, accounting for as
much as 20% of the obese population [17]. While
it may initially seem counterintuitive that so
many obese patients could present with the
absence of impaired glucose intolerance, hyper-
tension or dyslipidemia, one might speculate that
those with MHO simply represent individuals
who have little to no genetic predisposition to
adiposopathy. In other words, irrespective of their
increased body fat, MHO patients are likely to
maintain normally functional adipose tissue as
their fat mass increases. In fact, the additional adi-
pose tissue in these individuals may provide addi-
tional healthy fat functionality, and thus
account for a protective effect. As such, it has
been suggested that weight loss in these patients
might be counterproductive and potentially
harmful [17,19].
By maintaining favorable fat function and
avoiding the adverse metabolic consequences of
adiposopathy, MHO patients do not develop
high blood pressure, or abnormalities of glucose
and/or lipid abnormalities. With regard to fat dis-
tribution, it is interesting that MHO patients
have been shown to have less visceral fat than
obese patients with obesity-related metabolic
abnormalities, such as those found with the met-
abolic syndrome [17]. Thus, a significant percent-
age of the general population appears not to be
predisposed to adiposopathy, irrespective of the
onset of obesity. This lack of adiposopathy pre-
disposition is manifested by a lack of obesity-
related pathological fat dysfunction, a lack of
obesity-related high blood pressure and metabolic
abnormalities of glucose and lipid metabolism
and a relative lack of accumulation of visceral fat.
Another subgroup of patients that under-
scores the need to focus on fat function and/or
dysfunction includes those who are metaboli-
cally obese, but normal weight (MONW).
These individuals are often young, normal
weight individuals with premature signs of insu-
lin resistance, hyperinsulinemia and dyslipi-
demia [17]. It has been suggested that the fat
dysfunction of these individuals correlates to an
increase in intra-abdominal, or visceral fat, and
that increased visceral fat (relative to
subcutaneous peripheral fat) is dysfunctional
Table 2. Examples of endocrine and metabolic factors released
from fat cells [1,15,18].
Examples of hormones/adipokines released from adipose tissue
Leptin
Adiponectin (adipoQ or adipocyte complement-related protein of
30 kDa/Acrp30)
Interleukin-6
Resistin (FIZZ3 or Serine/cysteine rich adipocyte-specific secretory factor/ADSF)
Tumor necrosis factor
Examples of other enzymes, molecules, or factors described
as being released from adipose tissue
Acylation-stimulating protein (ASP)
Adipophilin
Adipsin
Agouti protein
Angiotensinogen
Apolipoprotein E
Calumenin
Calvasculin
Cholesteryl ester transfer protein (CETP)
Collagen type VI alpha 3
Complement factor C3
Endothelin
Entactin/nidogen
Estrogen
Fasting-induced adipose factor (FIAF)
Free fatty acids
Gelsolin
Galectin-12
Haptoglobin
Hippocampal cholinergic neurostimulating peptide (HCNP)
Insulin-like growth factor (IGF-1)
Lactate
Lipocalins
Lipoprotein lipase
Macrophage inhibitory factor (MIF)
Metalloproteases
Metallotionein
Monobutyrin
Nitric oxide synthase
Osteonectin (Secreted protein, acidic and rich in cysteine / SPARC)
Perilipins
Phospho-enolpyruvate carboxykinase (PEPCK)
Phospholipid transfer protein
Pigment epithelium-derived factor
Plasminogen activator inhibitor (PAI-1)
Pref-1
Protease inhibitors (such as cystatin C and colligin-1)
Prostaglandins I2 & F2 prostacyclins
Retinol-binding protein
Serine protease inhibitors
Stromal cell-derived factors, such as stromal cell-derived 1 precursor (SDF-1
or pre-B growth stimulating factor)
Tissue factor
Transforming growth factor beta (TGF-)
www.futuremedicine.com 45
Adiposopathy REVI EW
and metabolically harmful [17,20,21]. It has also
been suggested that fat dysfunction may corre-
late with subcutaneous truncal, but not
subcutaneous peripheral fat accumulation
[2023]. Thus, adiposopathy appears to be not
only associated with abnormalities in secretion
of adipocyte hormones, cytokines, factors, and
other molecules, but also associated with an
increase in intra-abdominal or possibly subcuta-
neous truncal fat which all leads to an increased
risk of. high blood pressure, and abnormalities
of glucose and lipid metabolism.
Taken together, MHO and MONW patients
demonstrate the point that it is not simply the
abnormal increase in normal adipose tissue that
reliably predicts subsequent adverse metabolic
consequences of adiposopathy. Instead, it is the
sufficient presence of or sufficient increase in
inadequately functional or blatantly dysfunc-
tional adipose tissue that is the essential,
underlying pathology. Emerging from this
paradigm are two other concepts: the obesity
metabolic cycle and adipose autodysharmonia.
As noted above, the predisposition to
dysfunctional adipose tissue is largely genetic, and
in many cases exacerbated by adiposity and seden-
tary lifestyle (Figure 1). One of the more important
consequences of adiposopathy is the promotion of
insulin resistance and hyperinsulinemia. In an
environment where adipose tissue remains rela-
tively sensitive to insulin (a growth factor) while
other organs such as skeletal muscle and liver
become more and more insensitive to insulin,
hyperinsulinemia may ensue, which in turn may
lead to increased adipose tissue and subsequent
worsening of adipose function. This worsening
adiposopathy may cause yet further insulin resist-
ance among other body organs. Adiposopathy,
followed by insulin resistance and hyperinsuline-
mia, followed by worsening adiposity and adi-
posopathy, followed by even greater insulin
resistance has been termed the obesity metabolic
cycle [1]. The fact that increased insulin levels may
increase adipose tissue mass may help to explain
why antidiabetes drugs that lower blood sugar
through increased insulin levels may further
increase body weight, while antidiabetes drugs
that lower blood sugar through increasing insulin
sensitivity (without increase or perhaps decrease in
insulin levels) are often associated with no weight
gain, or perhaps modest weight loss [1].
Also as noted above, the location of adiposity
may provide clues as to when adipose
dysfunction is most likely to occur. Indeed, stud-
ies of human fat depots (abdominal subcutane-
ous, mesenteric and omental) have shown that
even after multiple doublings, preadipocytes
retain the characteristics of the fat depots from
which they had originated [24]. This suggests that
subcutaneous and visceral fat may be genetically
predisposed to have significantly different func-
tions. Thus, within the same individual, various
fat depots may exhibit functional conflicts in
which well-functioning subcutaneous peripheral
fat may be providing favorable metabolic bene-
fits, while at the same time, malfunctioning
subcutaneous truncal and visceral fat may be
Table 3. Examples of adipose tissue-derived hormones,
enzymes and other factors that have been associated with
changes in insulin activity
(adapted from [16]).
Factor Selected functions Associated
insulin activity
Examples of adipocyte hormones
Leptin Signals CNS to decrease
appetite/nutrient intake
Signals the CNS to increase caloric
expenditure
Increases insulin sensitivity
Adiponectin Increased adiponectin increases
insulin sensitivity
Associated with decreased hepatic
glucose production
Resistin May increase insulin resistance
Examples of adipocyte cytokines
TNF- Increases tissue resistance to insulin,
particularly during sepsis and cancer
IL-6 Regulates T- and B-cell function
Increases insulin resistance
Examples of other select adipocyte proteins or factors
Angiotensinogen Converted in the circulation to
angiotensin II, resulting in
vasoconstriction and subsequently:
- May increase blood pressure
- May increase insulin resistance
- May decrease pancreatic insulin
secretion
Plasminogen
activator
inhibitor-1
Inhibits tissue plasminogen activator
Inhibits activation of fibrinolytic
cascade
May increase the risk of thrombosis
May interfere with insulin signaling
(?)
Adipsin and
acylation
stimulating
protein
Increases clearance of circulating
free fatty acids, triglyceride synthesis
and glucose uptake in adipose
tissue.
These effects upon insulin activity are largely based upon animal studies, and not always
definitively known to occur, nor be of significance in humans.
IL: Interleukin; TNF: Tumor necrosis factor.
(Reprinted from [2] by permission of Cambridge Medical Publications, all rights reserved).
REVI EW Bays, Abate & Chandalia
46 Future Cardiology (2005) 1(1)
inciting detrimental metabolic effects, a fracas
situation that might be termed adipose
autodysharmonia.
An extreme clinical example on how
dysfunction of adipose tissue may result in
diabetes mellitus, even in absence of obesity, is
demonstrated in patients with lipodystrophy, a
disease where lack of adipose tissue and leptin
deficiency results in excessive caloric intake,
increased plasma nonesterified free fatty acids
and elevated triglycerides concentrations. In
many individuals who lack sufficient functional
fat, ectopic fat is deposited in skeletal muscle
and liver, with post-receptor defects in insulin
action at the level of skeletal muscle [26]. In other
words, lipodystrophy is an example of how the
metabolic abnormalities of fat metabolism in
absence of obesity may result in similar
consequences on glucose disposal typically seen
in many obese patients.
Yet another illustrative example of how
abnormal function of fat tissue (adiposopathy)
results in metabolic consequences leading to an
increased predisposition to Type 2 diabetes and
CHD can be found amongst Asian Indians.
Many persons originating from the Indian
subcontinent manifest insulin resistance, even in
the absence of obesity [2729]. A study of this
population has revealed that FFA levels are higher
and insulin-mediated FFA suppression is
impaired in Asian Indian men compared with
Caucasians [27]. In addition, leptin levels are
higher and adiponectin levels are lower in Asian
men compared with Caucasians [27].
Furthermore, non-obese Asian Indians typically
exhibit high levels of C-reactive protein [29]. From
these scientific observations, it has been proposed
that the increased genetic predisposition to adi-
posopathy, coupled with increasing body fat (adi-
posity), that accounts for the increased prevalence
of Type 2 diabetes mellitus and CHD in this eth-
nic group [27]. Thus, this is an illustrative example
of how adiposopathy (not necessarily adiposity)
has been shown to be the root mechanistic cause
of many of the same metabolic abnormalities
found with the metabolic syndrome in a specific
ethnic group. In fact, it has even been suggested
that the metabolic syndrome may not be so
uncommon even among the general US popula-
tion of mildly overweight adults [32]. Some esti-
mate that the prevalence of the so-called MONW
patients may be as high as 1318% [17].
Sick fat (adiposopathy) causes high
blood pressure
Among overweight adult patients with a BMI
between 25 kg/m
2
and less than 30 kg/m
2
,
2233% have hypertension, and among patients
with BMI 30 kg/m
2
, greater than 40% have
hypertension [103]. Conversely, the prevalence of
hypertension among adults who are not over-
weight (BMI less than 25 kg/m
2
), is less than
Table 4. Mean plasma lipid levels at diagnosis of Type 2 diabetes in the UK
Prospective Diabetes Study [25].
Men Women
Lipid variable Type 2
diabetes
(n = 2139)
Nondiabetic
control
(n = 52)
Type 2
diabetes
(n = 1574)
Nondiabetic
control
(n = 143)
TC mg/dL (mmol/L) 213 (5.5) 205 (5.3) 224 (5.8) 217 (5.6)
LDL-C mg/dL (mmol/L) 139 (3.6) 132 (3.4) 151 (3.9)
135 (3.5)
HDL-C mg/dL
(mmol/L)
39 (1.0)
43 (1.1) 43 (1.1)
55. (1.4)
TG mg/dL (mmol/L) 159 (1.8)
103 (1.2) 159 (1.8)
95 (1.1)
p < 0.02;
p < 0.001 versus control.
HDL-C: High-density lipoprotein cholesterol; LDL-C: Low-density lipoprotein cholesterol; TC: Total cholesterol; TG:
Triglyceride. (Reprinted from [2] by permission of Cambridge Medical Publications, all rights reserved).
Table 5. LDL subclass phenotypes in Type 2 diabetes [30,31].
LDL subclass (%)
Population n A Intermediate B
Men
Diabetic
Nondiabetic
29
87
28
47
21
29
51
24
Women
Diabetic
Nondiabetic
54
543
34
85
30
9
36
6
Patterns A, Intermediate and B were determined by LDL diameter measurement
Pattern A: larger, potentially less atherogenic particles.
Patten B: small, dense, potentially more atherogenic particles
LDL: Low-density lipoprotein.(Reprinted from [2] by permission of Cambridge
Medical Publications, all rights reserved).
www.futuremedicine.com 47
Adiposopathy REVI EW
25%, yet hypertension is still found in these
nonoverweight individuals [102,103,105]. So while
BMI is directly associated with high blood
pressure, particularly among patients less than
60 years of age [33], not all patients who are
overweight have hypertension (although many
do) (Figure 2), and not all patients with hyperten-
sion are overweight. Therefore, while excessive
body fat clearly increases the risk of hypertension,
excess body fat alone is not sufficient towards
development of hypertension.
Admittedly, adiposopathy is not the only
cause of hypertension. Other causes would
include pheochromocytoma, primary
hyperaldosteronism, hypercortisolism, hyperthy-
roidism, renal artery stenosis and various kidney
diseases. Furthermore, certain familial or genetic
syndromes exists that strongly predispose
individuals to hypertension.
However, the majority of patients (> 90%)
with high blood pressure have what is called
essential hypertension. Adiposity is perhaps the
greatest risk factor for essential hypertension.
Excessive body fat may lead to promoters of
increased blood pressure, such as fat cell
secretory products that result in increase
mineralocorticoid release [34], and effects upon
the reninangotensin system (Table 2), and
sympathetic nervous system, all which represent
adipose dysfunction (adiposopathy). Further-
more, independent of adipose function or dys-
function, excess body fat may physically
compress the kidney and increase the incidence
of sleep apnea associated with obesity which
also may increase the risk of hypertension.
Sick fat (adiposopathy) causes
dyslipidemia
Among US adult patients with a BMI between
25 kg/m
2
and 30 kg/m
2
, 1930% have
hypercholesterolemia ( 240 mg/dl). Among
patients with a BMI > 30 kg/m
2
, greater than
2030% have hypercholesterolemia [103,105].
Conversely, among US adults who are not over-
weight (BMI < 25 kg/m
2
), less than 25% have
hypercholesterolemia, although hypercholestero-
lemia is still present in these nonoverweight indi-
viduals [102,103,105]. So while BMI is directly
associated with dyslipidemia, particularly among
patients less than 60 years of age [33], not all
patients who are overweight have hypercholeste-
rolemia, although many do (Figure 2), and not all
patients with hypercholesterolemia are over-
weight. Therefore, while excessive body fat
increases the risk of hypercholesterolemia, excess
body fat alone is not sufficient towards develop-
ment of hypercholesterolemia. Furthermore,
while there does appear to be a linear relation-
ship between adiposity and blood pressure, glu-
cose levels and waist circumference (with an
inverse linear relationship with HDL-C levels),
this relationship appears to peak within a BMI
range of 3040 kg/m
2
for alipoprotein B, low
density lipoprotein cholesterol (LDL-C) and
triglycerides, with subsequent decreased levels
with increasing obesity. This suggests that mor-
bidly obese patients may have some lipid risk
profiles more favorable than less obese patients
[35], and again underscores the complexity of the
relationship of adiposity with fat function.
Admittedly, adiposopathy is not the only cause
of dyslipidemia. Other secondary causes would
include hypothyroidism, diabetes mellitus and
certain types of liver or kidney diseases.
Furthermore, specific genetic abnormalities may
be present, such as familial hypercholesterolemia,
which is due to defective or absent LDL particle
Table 6. The atherogenic effect of diabetes dyslipidemia.
Potential atherogenic effects of small dense LDL:
Increased susceptibility of LDL particles to undergo oxidation
Increased permeability of arterial endothelia to LDL particles
Conformational change in apolipoprotein B in small, dense LDL particles
leading to decreased affinity for LDL receptor.
Present in association with insulin resistance syndrome
Present in association with high TG and low HDL cholesterol
Abnormalities associated with elevated TG levels and thus potential
for increased CHD risk:
Accumulation of lipoprotein (chylomicron and VLDL) remnants
Association with presence of small, dense LDL particles
Association with presence of low HDL cholesterol levels
Increased risk of thrombosis coagulability:
- Increased PAI-1
- Increased Factor VIIc
- Activation of prothrombin to thrombin
Abnormalities associated with low HDL cholesterol levels and
potential for increased CHD risk:
Reduction of direct antioxidant/anti-inflammatory effects on the vessel
wall via impaired HDL-mediated:
- Stabilization of prostacyclin production and/or prolongation of prostacyclin
half-life.
- Decrease in endothelial expression of cell adhesion molecules in response to
cytokines and otherwise restoration of endothelial dysfunction.
Reduced endothelial nitric oxide production and reduce antiplatelet and
anticoagulant effects
Reduced peripheral cholesterol transport/flux.
CHD: Coronary heart disease; HDL: High-density lipoprotein; LDL: Low-density
lipoprotein; PAI-1: Plasminogen activator inhibitor-1; TG: Triglyceride.VLDL: Very-low-
density lipoprotein.
(Reproduced from [2] by permission of Cambridge Medical Publications, all rights
reserved and adapted with kind permission from Baylor College of Medicine, Houston,
TX, USA [106]).
REVI EW Bays, Abate & Chandalia
48 Future Cardiology (2005) 1(1)
receptors, and results in severe
hypercholesterolemia irrespective of body fat.
Although hypercholesterolemia may be
associated with adiposity, the type of
dyslipidemia most associated with the metabolic
syndrome and Type 2 diabetes mellitus is fasting
hypertriglyceridemia, low HDL-C levels (Table 4),
and abnormalities of lipoprotein particle size and
subclass distribution (Table 5) [2,36]. Figure 3 illus-
trates how adiposopathy may lead to increased
FFA release, fatty liver, and then to fasting hyper-
triglyceridemia as the result of increased very-
low-density lipoprotein (VLDL) particle produc-
tion. The subsequent exchange of cholesterol
with triglycerides between VLDL and HDL par-
ticles through cholesteryl ester transfer protein, as
well as LDL particles, results in triglyceride-rich
HDL and LDL particles. This process also leads
to cholesterol-rich VLDL and IDL-atherogenic
remnant particles. Once the triglyceride-rich
HDL particles undergo lipolysis through various
lipases, the HDL particle becomes smaller and
more dense, leading to increased renal clearance
and decreased HDL blood levels; this is associ-
ated with an increased risk of CHD. Once the
triglyceride-rich LDL particles undergo lipolysis
through various lipases, the LDL particle
becomes more small and dense, leading to what is
termed pattern B; this is also associated with an
increase risk of risk of CHD (Table 6).
Thus, it is reasonable to conclude that it is the
combination of adiposity, genetic predisposition,
and perhaps sedentary lifestyle that leads to fat
dysfunction, and it is this adiposopathy that
results in an atherogenic dyslipidemia [39].
Adiposopathy: treatments
Current treatments for adiposopathy include
those that treat obesity (as it is obesity that often
exacerbates the root cause of the metabolic
Figure 3. Fasting atherogenic lipid profile associated with metabolic syndrome and
Type 2 diabetes mellitus (elevated TG, decreased HDL-C and increased prevalence of
small dense LDL particles).
Adapted from [37]. This figure does not depict the important contribution of postprandial
hypertriglyceridemia, which often occurs in these same patients wherein elevated postprandial chylomicrons
(from the intestine) may also contribute to hypertriglyceridemia, the atherogenic lipid profile described
above, and the creation of chylomicron remnant particles, which may be significantly atherogenic [38].
TG
Small
dense LDL
FFA
Adiposopathy
CETP
CETP
Cholesterol Cholesterol
Cholesterol Cholesterol
TG TG
TG
Lipases
Lipases
HDL
VLDL
LDL LDL
Renal clearance
Fatty liver
TG
Small
dense HDL
TG
www.futuremedicine.com 49
Adiposopathy REVI EW
syndrome) and those that treat the metabolic
consequences, such as drug treatments for Type 2
diabetes mellitus, hypertension and dyslipidemia.
Antiobesity agents
Adiposity, along with sedentary lifestyle in
genetically susceptible individuals, leads to
worsening adiposopathy. It has been theorized
that enlargement of fat cells alone might largely
account for fat cell dysfunction [15]. In fact, it is
the enlargement of fat cells that best correlates
with insulin resistance as compared with other
measures of adiposity, and enlarged fat cells are a
strong, independent predictor of the develop-
ment of Type 2 diabetes mellitus [15]. Current
antiobesity agents such as orlistat (Xenical
) and
sibutramine (Reductil
, Merida
) have both
been shown to reduce body weight and also
improve many metabolic abnormalities of glu-
cose and lipid metabolism that are otherwise
associated with increased CHD risk [1]. This
illustrates an important principle that: the devel-
opment of any effective antiobesity agent must
not only reduce fat mass (adiposity), but must
also correct fat dysfunction (adiposopathy) in
order to maximize metabolic health [1]. Some
investigational antiobesity agents in
development have already demonstrated reduc-
tion in the incidence of the metabolic syndrome
[1]. In order to gain approval for clinical use,
other antiobesity agents in development will
likely have to demonstrate similar improvements
in metabolic function.
Antidiabetes drugs
Antidiabetes drugs may also improve glucose
metabolism, and thus improve the
hyperglycemia consequence of adiposopathy.
Current antidiabetes agents have little impact
upon blood pressure, and varying effects upon
lipid levels (Table 7) [40]. It is with special interest
that some antidiabetes agents may improve fat
differentiation and function, while at the same
time, paradoxically increase body weight.
Through a large number of DNA microarrays, it
has been shown that large differences exist
between lean and obese mice in expression of
genes. Specifically, the expression of many genes
normally associated with adipocyte differentia-
tion appeared to be downregulated with obesity
[41]. Recruitment of functional fat cells through
differentiation is one potential treatment option
towards improving glucose metabolism through
improved fat function and reduction of the
metabolic consequences of adiposopathy.
Peroxisome proliferator-activated receptor
(PPAR) agonists [16], such as thiazolidinediones
(TZDs), represent antidiabetes agents that
improve glycemic control, enhance hepatic and
muscle insulin sensitivity, and improve -cell
function. TZDs are associated with weight gain
directly proportional to the reduction in hemo-
globin A1c (HbA1c) [15]. Additionally, obese
individuals appear to respond better to TZDs
than lean subjects. This may be attributable to
the fact that PPAR is a critical transcription fac-
tor in the differentiation of preadipocytes into
adipocytes [42]. Thus, by recruiting more
functional fat cells, TZDs cause a marked
reduction in plasma FFA concentration and
inhibit lipolysis in patients with Type 2 diabetes
mellitus [15]. TZDs may also:
Inhibit the expression of the leptin gene in adi-
pocytes with a decline in leptin levels;
Improve fat distribution with a decrease in
intra-abdominal fat;
Table 7. Effects of antidiabetes agents upon lipid levels.
Treatment Triglycerides High-density
lipoprotein cholesterol
Low-density particle
size
Low-density particle
number
Lifestyle changes Potential decrease Potential increase Potential decrease Potential decrease
Insulin secretagogues No change No change No change No change
Metformin Inconsistent;
occasionally decreased
Inconsistent; occasionally
increased
No change or minimal
increase
No change or minimal
decrease
-Glucosidase
inhibitors
No change No change No change No change
Thiazolidinediones No change with
rosiglitazone;
1520% decrease
with pioglitazone
510% increase Probable to substantial
increase
5% increase with
rosiglitazone; no
change with
pioglitazone
Insulin Decrease No change Probable increase No change
(Reproduced from [16,40]).
REVI EW Bays, Abate & Chandalia
50 Future Cardiology (2005) 1(1)
Decrease hepatic fat content associated with an
improvement in hepatic insulin sensitivity; and
Decrease in intracellular concentration of
metabolites of muscle triglycerides that best
predicts the improvement in muscle sensitivity
to insulin.
Although some of the weight gain associated with
TZDs is due to an increase in fluid retention, it is
Table 8. Prevention trials of lipid-altering therapy including patients with diabetes.
Trial Diabetic
number
Total number in
study
Lipid-altering drug
(mg/day)
CHD risk versus placebo in diabetic
patients (%)
Primary prevention
CARDS* 2838 2838 Atorvastatin 10 -37 (p = 0.001)
AFCAPS 155
6605 Lovastatin 40
-44 (p = NS)
HPS 2912 7150 Simvastatin 40 -33 (p = 0.0003)
ASCOT 2532 10,305 Atorvastatin 10 -16 (p = NS)
PROSPER 623 5804 Pravastatin 40 +27 (p = NS)
HHS 135 4081 Gemfibrozil 1200 -68 (p = NS)
Secondary prevention
4S
Re-analysis
202
483
4444 Simvastatin 2040 -55 (p = 0.002)
-42(p = 0.001)
CARE 586 4159 Pravastatin 40 -25 (p = 0.05)
LIPID** 1077 9014 Pravastatin 40 -19 (p = NS)
LIPS 202 1677 Fluvastatin 80 -47 (p = 0.04)
HPS 3051 13,386 Simvastatin 40 -18 (p = 0.002)
4D
1255 1255 Atorvastatin 20 -8 (p = NS)
VA-HIT
769 2351 Gemifbrozil 1200 -32 (p0.004)
DAIS
418 418 Fenofibrate 200 -23 (p = NS)
Diabetes trials in progress
FIELD 9795 9795 Fenofibrate 200
ASPEN 2200 2200 Atorvastatin 10
Prevention trials of lipid-altering therapy including patients with metabolic syndrome.
Primary
WOSCOPS 1691
6595 Pravastatin 40 27% Reduction in CHD risk
Secondary
4S post hoc
analysis
458
4444 Simvastatin 2040 52% reduction (p = 0.00009) in major
coronary events
CDP 563
8341 Niacin 3000 9% reduction in total 5-year mortality
25% reduction in risk of nonfatal
myocardial infarction in metabolic
syndrome patients without HDL-C
criterion
An additional analysis noted that the
most pronounced benefits of treatment
were seen in metabolic syndrome
patients with low HDL-C (< 40 mg/dl)
*CARDS was the only primary prevention trial in this group that was prospective.
Mean dose was 30mg.
The figure of 155 in AFCAPS/TexCAPS
includes subjects with diagnosis of diabetes (n = 71 placebo and 84 drug treated). However, an alternative figure often cited is a 239 figure that
included subjects with diagnosis of diabetes mellitus or fasting glucose than 126 mg/dL (n = 113 placebo and n = 126 drug treated).
The 483
patients represented a re-analysis wherein diabetes was defined according to fasting glucose 126 mg/dl. **782 patients identified themselves as
having diabetes, with another 295 having probable undiagnosed diabetes based upon fasting glucose levels for a total of 1077.
Of the patients
on this study, 627 had history of diabetes, with another 142 found to have fasting glucose levels 126 mg/dl at baseline. This gives the total of 769
patients.
These were prospective trials, and not post hoc analysis (as were the rest of the studies in this secondary prevention group.
Number
of patients with the metabolic syndrome). NS: Not significant
(Reprinted from [2] by permission of Cambridge Medical Publications, all rights reserved).
www.futuremedicine.com 51
Adiposopathy REVI EW
also true that through the successful recruitment
of preadipocytes into adipocytes, some of the
resulting fat weight gain is an indicator of the
efficacy of the TZD. Other indicators of
improvement in adiposopathy with the creation
of healthier fat with TZDs are:
The reduction in FFA levels;
Inhibition of resistin, tumor necrosis factor,
and plasminogen activator inhibitor (PAI)-1
gene expression in adipocytes and reduction
in their circulating levels;
Stimulation of adiponectin gene expression in
adipocytes and increase in adiponectin levels;
Improvement in pancreatic -cell function
with a reduction in islet fat content and pres-
ervation of islet cell histology and -cell mass.
In addition to TZDs, investigational
antidiabetes drugs are in development, such as
dual PPAR / agents (e.g., tezaglitazar, muragl-
itazar) [16,43,44] that likewise, have actions upon
molecular targets with the potential to improve
glucose metabolism, improve dyslipidemia,
reduce lipotoxicity, and generally improve
adiposopathy [16,50].
Antihypertensive drugs
Antihypertensive drugs have been shown to
reduce CHD events in patients with diabetes
mellitus, as well as reduction in other
complications of diabetes mellitus [51], with the
best choice of first agents being those that might
improve endothelial dysfunction (such as with
angiotensin-converting enzyme inhibitors and
aldosterone receptor antagonists), followed by the
liberal use of addition antihypertensive agents in
order to maximize blood pressure control [52].
Lipid-altering drugs
Lipid-altering drugs are also one of the few drug
treatments that have been shown to reduce CHD
outcomes in patients with glucose abnormalities
[16] (Table 8). Thus, lipid-altering drugs will con-
tinue to be recommended for high risk metabolic
syndrome patients [5], and will continue to be an
important treatment option to reduce CHD
events in patients with adiposopathy.
Conclusion
Abnormal fat function, termed adiposopathy, is a
major contributing factor in the development of
the most common metabolic diseases encountered
in the clinical practice of medicine. Through a
better understanding of the pathophysiology, and
through established criteria for its diagnosis, the
treatment of adiposopathy holds promise for the
reduction in morbidities and mortality particu-
larly through a reduction in CHD, and a reduc-
tion in the presence or onset of Type 2 diabetes
mellitus, hypertension and dyslipidemia.
Table 9. Regulatory considerations for granting approval of a treatment indication
for a new metabolic drug [45].
General principles for approval of a new drug
Must have reasonable clinical trial data conducted through adequate and applicable methods that
demonstrate the drug is safe and effective under the conditions of use when prescribed,
recommended or suggested in the proposed labeling.
Specific principles for metabolic drugs
Although in most cases, no minimum level of efficacy is established for approval of metabolic drug
treatments [45,46], in general, these drugs usually require certain objective minimum improvement in
target metabolic parameters as weighed against potential risk.
Approved antihypertensive drugs have generally achieved > 45 mm/Hg reduction in blood
pressure [47,48].
Approved antidiabetes drugs have generally achieved at least about a 1% reduction in
hemoglobin A1c.
Approved systemic lipid-altering drugs must generally achieve an LDL-C lowering of at least 15%,
and perhaps lower (12%) for non-systemic lipid-altering drugs [45].
Approved anti-obesity drugs must generally achieve mean placebo-subtracted weight loss 5%
at the end of 1 year, with the proportion of subjects who lose 5% of baseline body weight is
greater in drug- vs placebo-treated group [49].
The mechanism of action and known experience of the metabolic drug must be scientifically and
reasonably expected to improve patient outcomes, and in cases of new drugs with novel mechanisms
of action, demonstrate at least surrogate outcome benefits irrespective of the efficacy on the
metabolic treatment target. For example, a novel HDL-raising drug would require at least 2 different
imaging modalities to obtain an initial approved indication for HDL-raising, possibly with postapproval
confirmatory clinical endpoint studies.
REVI EW Bays, Abate & Chandalia
52 Future Cardiology (2005) 1(1)
Adiposopathy: future perspectives &
regulatory considerations
While regulatory indications exist for treatment
of the components of metabolic syndrome (e.g.,
diabetes mellitus, hypertension, and
dyslipidemia), an indication for the treatment of
the metabolic syndrome itself remains elusive.
The approval of drugs for treatment of
adiposopathy and the metabolic syndrome
present special challenges. No clinical trial has
demonstrated patient outcomes that benefit from
a single drug which improves multiple CHD risk
factors, and thus regulatory agencies have not
found global risk factor reduction as an
acceptable criterion to grant drug approval,
labeling or promotion [45]. Examples of suggested
regulatory criteria that must be met in order to
grant approval of a specific indication for a new
drug are listed in Table 9.
As can be seen from this table, other metabolic
disease drugs (such as antihypertensive drugs, anti-
diabetes agents and lipid-altering drugs), have
fairly clear criteria to obtain an approvable
indication. The main reason as to why these drug
Table 10. The 1982 revised criteria for classification of systemic lupus erythmatosis.
Criterion
definition
1. Malar rash
a) Fixed erythema, flat or raised, over the malar eminences, tending to spare the nasolabial folds
2. Discoid rash
a) Erythematous raised patches with adherent keratotic scaling and follicular plugging; atrophic
scarring may occur in older lesions
3. Photosensitivity
a) Skin rash as a result of unusual reaction to sunlight, by patient history or physician observation
4. Oral ulcers
a) Oral or nasopharyngeal ulceration, usually painless, observed by physician
5. Arthritis
a) Nonerosive arthritis involving 2 or more peripheral joints, characterized by tenderness, swelling, or
effusion
6. Serositis
a) Pleuritis convincing history of pleuritic pain or rubbing heard by a physician or evidence of pleural
effusion or
b) Pericarditis documented by ECG or rub or evidence of pericardial effusion
7. Renal disorder
a) Persistent proteinuria > 0.5 g/day or > 3+ if quantitation not performed or
b) Cellular casts may be red cell, hemoglobin, granular, tubular, or mixed
8. Neurologic disorder
a) Seizures in the absence of offending drugs or known metabolic derangements, e.g., uremia,
ketoacidosis, or electrolyte imbalance or
b) Psychosis in the absence of offending drugs or known metabolic derangements, e.g., uremia,
ketoacidosis, or electrolyte imbalance
9. Hematologic disorder
a) Hemolytic anemia with reticulocytosis or
b) Leukopenia < 4000/mm
3
total on 2 or more occasions or
c) Lymphopenia < 1500/mm
3
on 2 or more occasions or
d) Thrombocytopenia < 100,000/mm
3
in the absence of offending drugs
10. Immunologic disorder
a) Positive LE cell preparation or
b) Anti-DNA: antibody to native DNA in abnormal titer or
c) Anti-Sm: presence of antibody to Sm nuclear antigen or
d) False positive serologic test for syphilis known to be positive for at least 6 months and confirmed
by Treponema pallidum immobilization or fluorescent treponemal antibody absorption test
11. Antinuclear antibody
a) An abnormal titer of antinuclear antibody by immunofluorescence or an equivalent assay at any
point in time and in the absence of drugs known to be associated with "drug-induced lupus"
syndrome
The classification is based on 11 criteria. For the purpose of identifying patients in clinical studies, a person shall be
said to have systemic lupus erythematosus if any 4 or more of the 11 criteria are present, serially or simultaneously,
during any interval of observation [53].
www.futuremedicine.com 53
Adiposopathy REVI EW
treatments have specific criteria and metabolic
syndrome drugs do not, is because currently, the
metabolic syndrome is not itself a treatment target.
As a result, the FDA does not recognize a single,
universal, measurable, and directly treatable root
pathogenic mechanism underlying the syndrome
that would establish the metabolic syndrome per
se, as a specific treatment target [45]. However, if
adiposopathy becomes accepted as a directly meas-
urable and treatable root pathogenic mechanism
for the vast majority of patients with the metabolic
syndrome, this opens the possibility of guidance
Table 11. Proposed diagnostic criteria for the diagnosis of adiposopathy.
Criterion
definition
Major criteria
1. Adiposity
Body mass index (BMI) 30 kg/m2
or
Waist circumference > 102 cm (> 40 in) in men, or > 88 cm (> 35 in) in women or
Waist:hip ratio > 0.9 in men, or > 0.85 in women
2. Abnormalities in glucose metabolism
Fasting glucose blood levels 100 mg/dl (6.0 mmol/l) or
1 h post oral 75 g glucose load glucose blood level 140 mg/dl (mmol/l) or
Use of antidiabetes drug treatment in Type 2 diabetes mellitus
3. Hypertension
Systolic blood pressure 130 mm/Hg or diastolic blood pressure 85 mg/Hg or
Use of antihypertensive drug treatment for high blood pressure
4. Dyslipidemia
Fasting triglyceride level > 150 mg/dl (>1.7 mmol/l) or
Fasting HDL-C level < 40 mg/dl (<1.0 mmol/l) in men or < 50 mg/dl (<1.3 mmol) in women or
Use of lipid-altering drug treatment for high triglycerides or low HDL-C levels
Minor criteria
1. Microalbuminuria
Urinary albumin excretion rate > 20 g/min or
Albumin:creatinine ratio 30 mg/g
2. Onset of androgenemia in women, especially with signs and symptoms of polycystic ovarian syndrome
Elevated total testosterone or DHEAS in women, and possibly an increase in prolactin levels
3. Hepatosteatosis
Otherwise unexplained elevated hepatic transaminases, possibly with hepatic imaging revealing
findings consistent with fatty liver
4. Hypercoagulable state
Otherwise unexplained thrombotic clinical event in patients with elevated BMI, with possibly an
increase in plasminogen activator inhibitor (PAI-1)
5. Abnormalities of lipoprotein particle size and subclass distribution [36]
Decreased LDL particle size with increased prevalence of "pattern B"
6. Hormone abnormalities of fat cell dysfunction
Elevated fasting insulin levels, elevated leptin levels, and or decreased adiponectin levels
or
Elevated insulin/leptin to adiponectin ratio
7. Metabolic markers of fat cell dysfunction
Elevated fasting or postprandial free fatty acid levels
8. Inflammatory markers of fat cell dysfunction
Elevated cytokine production (tumor necrosis factor and/or interleukin-6), with elevated
C-reactive protein
The presence of major and minor criteria to diagnose adiposopathy require that these findings are clinically not
entirely due to etiologies other than dysfunctional adipose tissue. For example, an increase in waist circumference
solely due to ascites, increase in blood sugars solely due to chronic pancreatitis, hypertension solely due to
pheochromocytoma, and dyslipidemia solely due to familial dyslipidemia syndromes would not be included in the
diagnostic criteria for adiposopathy. Also it should be noted that although an increase in cancer risk has been
described with adiposity, and although this increase in cancer risk may be associated with adiposopathy, an increase
in cancer risk is not included in this proposed diagnostic criteria.
BMI may not be as accurate as waste
circumference & waist:hip ratio in assessing adiposopathy at the highest weight individuals ( 40 kg/m
2
), and
possibly lower weight individuals ( 25 kg/m
2
).
Albuminuria might be considered a surrogate for microvascular
disease, and is a diagnostic criteria in the WHO classification of the Metabolic Syndrome.
The relationship of
elevated leptin levels and obesity are well-established [1]. In obese humans, adiponectin may be more consistently
related to insulin sensitivity as opposed to other adipokines such as resistin, TNF-, and IL-6 [54].
REVI EW Bays, Abate & Chandalia
54 Future Cardiology (2005) 1(1)
towards the research and development of drugs
that improve fat function and thus treatments for
the metabolic abnormalities associated with the
metabolic syndrome.
Such an acceptance would allow scientific
organizations to first define adiposopathy.
Although adiposopathy would likely have a variety
of both phenotypic and laboratory criteria for
diagnosis that would change over time, this kind
of approach and diagnostic criteria is not unprece-
dented. Systemic lupus erythematosis (SLE) has
both phenotypic and serologic criteria for diagno-
sis, and this classification allows more uniform
conduct of clinical trials for drug treatment
(Table 10). Similar guidance in the conduct of clini-
cal trials of drug treatment could be achieved
through an accepted definition of adiposopathy,
that would also likely evolve over time.
So how would adiposopathy best be defined?
Table 11 is a proposal for diagnostic criteria of adi-
posopathy that incorporates both major and
minor criteria. As with the SLE criteria described
above, clinical, observational and serological find-
ings are included in the diagnostic criteria. One
could therefore speculate that a proposed classifi-
cation of adiposopathy could be based upon anal-
ogous criteria. Particularly for the purpose of
identifying patients in clinical studies and
response to therapy, a person could be said to
have adiposopathy if any three or more of the
major criteria, with two minor criteria equivalent
to one major criteria.
But obviously, much remains to be done to
determine which criteria best select for
adiposopathy, with particular attention to which
aspects of abnormal fat function lead to an
increase in CHD risk the most common cause
of mortality in patients so affected, although can-
cer risk may also be increased. Furthermore, it
would be important to discover which
consequences of adiposopathy, if appropriately
treated with diet, physical exercise or drugs, are
most associated with a reduction in clinical mor-
bidity and mortality. But clearly, a greater focus on
identifying and evaluating the treatment of fat
dysfunction that often leads to the many of com-
ponents of the metabolic syndrome holds promise
as a superior approach in the targeted manage-
ment of patients. It would allow for a more
focused evaluation of the efficacy of interventions
such as diet, exercise, and related pharmaceutical
agents upon a common, unifying etiology of the
most common metabolic diseases of our time.
In other words, clinical trials directed at
correcting fat dysfunction (adiposopathy) would
be easier targeted and conducted, compared with
clinical trials directed at an array of abnormalities
associated with the metabolic syndrome. This is
because the trials would then be focused on the
underlying root pathophysiologic cause. Once
improvement in adiposopathy was shown to
improve patient outcomes, then pharmacologic
agents might be able to obtain an indication for
treatment of adiposopathy, without necessarily
having to always prove more hard outcomes
benefits for each drug that is developed.
For example, the FDA does not require
outcome data for approval of an antidiabetes
agent [45]. This is because improving glucose
metabolism alone is accepted as being beneficial
to patients. Thus, the approved indication of a
new antidiabetes agent is most often for the
improvement in high glucose levels alone, whose
presence may be asymptomatic in many patients.
Demonstration of improvement in patient out-
comes is not required, such as a reduction in
adverse end-organ events attributed to diabetes.
Similarly, new antihypertensive drugs can obtain
an approved indication for the treatment of high
blood pressure alone, despite presenting no
clinical symptoms in many patients. Demonstra-
tion of improvement in patient outcomes is not
always required, such as proven cardiovascular or
renal outcomes benefits. Lipid-altering drugs have
often been granted an approved indication for
improvement of lipid levels, (despite presenting
no clinical symptoms in many patients), without
proven benefits towards reduction in CHD.
Just as with the above metabolic diseases, the
presence of adiposopathy may also be largely
asymptomatic in many individuals. However
If it was accepted that adiposopathy was the root
pathophysiologic cause of many, if not most
cases of patients who express the metabolic syn-
drome (even without specific symptoms);
If it could be shown that adiposopathy was a
well-validated predictor of morbidity and
mortality;
If it can be shown and accepted that
improvement in fat dysfunction improves
patient metabolic health (such as an
improvement in, or a reduction in the onset of
Type 2, high blood pressure and dyslipidemia);
and
If it could be demonstrated that correction of
adiposopathy resulted in improved patient hard
outcomes, (such as reduction in CHD events);
then it is conceivable that drugs could obtain
approval for the indication of treatment of
www.futuremedicine.com 55
Adiposopathy REVI EW
adiposopathy alone. Once the above were
established using the model of diabetes mellitus,
hypertension and dyslipidemia therapies, drugs
with indications for the treatment of adiposopathy
would then not necessarily always require very
large, difficult and sometimes prohibitively expen-
sive CHD outcomes studies in order for the
approval to potentially benefit patients who now
number in epidemic proportions.
While the impact upon the clinical and
research community of such an approach would
be substantial, it would not necessarily be over-
whelming. In a practical research example, the
future of antiobesity agent development would
likely require two parallel programs: one clinical
trial program focused upon treatment of obesity
itself through fat reduction (adiposity), and
another clinical trial program focused upon
improvement in fat dysfunction (adiposopathy)
(Figure 4). To a large extent, this is already being
done. Existing antiobesity agents, such as orlistat
and sibutramine, have both demonstrated
improvement in weight reduction, as well as
improvements in many metabolic parameters
with reductions in CHD risk factors [1].
It is also noteworthy that rimonabant
(currently an investigational selective cannabinoid
[CB]-1 receptor antiobesity antagonist [1]) has
also essentially followed this parallel development
programme approach. Rimonabant has been
shown to cause significant weight reduction after
1 year, and thus was effective in reducing adipos-
ity [55]. This weight loss benefit was subsequently
found to be extended to 2 years [56]. Rimonabant
has also been shown to improve functional
parameters associated with adiposopathy:
From an adipose tissue organ standpoint,
rimonabant decreased waist circumference
(presumably resulting in less subcutaneous
truncal and visceral fat) [55,56];
From an overall metabolic standpoint, rimona-
bant increased HDL-C levels, reduced triglyc-
eride levels, improved LDL particle size,
improved insulin sensitivity (as determined by
glucose tolerance testing and homeostasis
model assessment), and reduced C-reactive
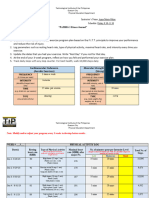
Figure 4. Proposed parallel investigational antiobesity agent development program.
Investigational antiobesity
agent
Reduction in adiposity
Improvement in adiposopathy
Mean placebo-subtracted weight loss
5% at the end of 1 year
Proportion of subjects who lose 5% of
baseline body weight greater in drug-
vs placebo-treated group
Sustained weight loss for at least 2 years
Improvement in adipose organ distribution
Reduction in waist circumference
Reduction in waist:hip ratio
Improvement in body metabolism
Improvement in glucose metabolism
Reduction in blood pressure
Improvement in dyslipidemia
Approval for clinical use
Improvement in adipocyte function
Reduction or lack of worsening of albuminuria
Improvement in phenotypic and biochemical
findings consistent with polycystic ovarian syndrome
Reduction in liver enzymes in patients with
"fatty liver"
Reduction in thrombotic risk or reduction in
elevated PAI-1 levels
Improvement in lipoprotein particle size and
subclass distribution
Decreased insulin levels
Decrease leptin and/or increase in adiponectin
levels, or decrease in insulin/leptin:adiponectin
ratio
REVI EW Bays, Abate & Chandalia
56 Future Cardiology (2005) 1(1)
protein levels; and
From an adipocyte standpoint, rimonabant
increased adiponectin levels, and decreased lep-
tin levels [55,56].
It has been suggested that the metabolic benefits of
rimonabant may not totally be explained through
weight reduction [56], with the implication that, in
addition to its appetite suppressive effects upon
the central nervous system [1], CB-1 receptor
antagonism may also have direct adipocyte activ-
ity. Indeed, animal studies have found that CB-1
receptors are found in adipose tissue [57]. This
raises the possibility that the overall efficacy of
rimonabant is the result of both body weight
reduction through CB-1 antagonism-induced
reduction of appetite by its central nervous system
effects [1], and direct favorable hormonal and met-
abolic changes through CB-1 antagonism directly
targeted at the adipocyte [57]. Thus, this has been
an illustrative example of a parallel antiobesity
development programme that has been focused
not only on the treatment of adiposity, but also in
the treatment of adiposopathy.
Acknowledgements
Harold Bays MD, FACP
There was no outside funding/support for this review. In over a
decade of clinical research, Dr Bays has served as an Clinical
Investigator for (and has received research grants from) phar-
maceutical companies such as Alteon, Aventis, Bayer, Boe-
hringer Ingelheim, Boehringer Mannheim, Bristol-Myers
Squibb, Fujisawa, Ciba-Geigy, GelTex, Glaxo, Genetech,
Hoechst Roussel, KOS, Lederle, Marion Merrell Dow, Merck,
Merck Schering-Plough, Miles, Novartis, Parke-Davis, Pfizer,
Purdue, Reliant, Roche, Rorer, Regeneron, Sandoz, Sankyo,
Sanofi, Shering Plough, Searle, SmithKline Beacham,
Takeda, TAP, UpJohn, Upsher Smith, Warner-Lambert,
Wyeth-Ayerst, and AstraZenca. He has also served as a consult-
ant, speaker, and/or adviser to and for pharmaceutical compa-
nies such as AstraZeneca, Aventis, Bayer, Bristol-Myers
Squibb, KOS, Merck, Merck Schering-Plough, Novartis,
Ortho-McNeil, Parke-Davis, Pfizer, Roche, Sandoz, Sankyo,
Sanofi, Shering Plough, SmithKline Beacham, Takeda,
UpJohn, and Warner-Lambert. Nicola Abate MD & Mani-
sha Chandalia MD Grants: NIH grants K23-RR16075;
MO1-RR-00633 (NIH/DHS/DHHS); CDC
H75/CCH523202; AHA 0465017Y.
Executive summary
Background
Abnormal fat function, termed adiposopathy, results in the pathological release of hormones, cytokines and molecules that cause
dysfunction of target tissues.
Adiposopathy: replacing the term metabolic syndrome
Adiposopathy is most often caused by excessive body fat, but the amount of excessive body fat that results in fat dysfunction is widely
variable among individuals, and even variable among patient populations.
Adiposopathy is a major contributing factor in the development of the most common metabolic diseases encountered in the
clinical practice of medicine many of which are now incorporated in the term metabolic syndrome.
Sick fat (adiposopathy) causes Type 2 diabetes mellitus
Adiposopathy causes, or at least contributes to, elevated blood sugars and Type 2 diabetes mellitus in genetically
predisposed individuals.
Sick fat (adiposopathy) causes high blood pressure
Adiposopathy causes, or at least contributes to, elevated blood pressure (hypertension) in genetically predisposed individuals.
Sick fat (adiposopathy) causes dyslipidemia
Adiposopathy causes, or at least contributes to, dyslipidemia in genetically predisposed individuals.
Adiposopathy: treatments
In many cases, adiposopathy can be corrected through interventions that result in fat reduction, such as through diet, physical
exercise and antiobesity agents.
Some aspects of adiposopathy can also be improved through agents that result in increased adipose tissue, such as through
peroxisome proliferator-activated receptor (PPAR) agonists.
Through a better understanding of the pathophysiology, and through established criteria for its diagnosis, the treatment of
adiposopathy holds promise for the reduction in mortality particularly through a reduction in coronary heart disease (CHD), and
a reduction in the presence or onset of Type 2 diabetes mellitus, hypertension and dyslipidemia.
Adiposopathy: future perspectives & regulatory considerations
If its treatment can be shown to reduce CHD risk, or reduction in other hard clinical endpoints such as cancer, and/or a reduction
in subsequent morbidities (such as Type 2 diabetes mellitus, hypertension and dyslipidemia), then adiposopathy may some day
become a primary treatment target.
If regulatory agencies would grant indications for drugs to treat adiposopathy, then this would promote and accelerate research
interest and investment towards improving fat function, with the end result being beneficial new treatment modalities for
patients who currently have detrimental metabolic consequences of adiposity and adiposopathy.
www.futuremedicine.com 57
Adiposopathy REVI EW
Bibliography
Papers of special note have been highlighted as
either of interest () or of considerable interest ()
to readers.
1. Bays HE: Current and Investigational
AntiObesity Agents and Obesity
Therapeutic Treatment Targets. Obesity
Research 12(8), 11971211 (2004).
Comprehensive review of current
antiobesity agents in development, and
their physiological rationale. May be most
interesting to those involved in antiobesity
clinical trials.
2. Bays H, Shepherd J: Diabetes, Metabolic
Syndrome and Dyslipidemia. Management
Strategies in Diabetes. Cambridge Medical
Publications. ISBN 0 904052 88 5.
128 (2004).
3. Reaven G: The metabolic syndrome or the
insulin resistance syndrome? Different
names, different concepts, and different
goals. Endocrinol. Metab. Clin. North Am.
33(2), 283303 (2004).
4. Ford ES: Prevalence of the metabolic
syndrome in US populations. Endocrinol.
Metab. Clin. North Am. 33(2),
333350 (2004).
5. Third Report of the National Cholesterol
Education Programme (NCEP) Expert
Panel on Detection, Evaluation, and
Treatment of High Blood Cholesterol in
Adults (Adult Treatment Panel III) final
report. Circulation 106, 31433421 (2002).
6. Alberti KG, Zimmet PZ: Definition, diagnosis
and classification of diabetes mellitus and its
complications. Part 1: diagnosis and
classification of diabetes mellitus provisional
report of a WHO consultation. Diabet. Med.
15, 539553 (1998).
7. Flegal KM, Carroll MD, Ogden CL,
Johnson CL: Prevalence and trends in
obesity among US adults, 19992000.
JAMA 288, 17231727 (2002).
8. Hedley AA, Ogden CL, Johnson CL,
Carroll MD, Curtin LR, Flegal KM:
Prevalence of overweight and obesity among
US children, adolescents, and adults,
19992002. JAMA 291, 28472850
(2004).
9. Ford ES, Giles WH, Dietz WH: Prevalence
of the metabolic syndrome among US
adults: findings from the third National
Health and Nutrition Examination Survey.
JAMA 287, 356359 (2002).
Standard paper quantifying the epidemic of
obesity
10. Bruno G, Merletti F, Biggeri A et al.:
Metabolic Syndrome as a Predictor of All-
Cause and Cardiovascular Mortality in Type
2 Diabetes. Diabetes Care 27,
26892694 (2004).
11. Stern MP, Williams K, Gonzalez-
Villalpando et al.: Does the Metabolic
Syndrome Improve Identification of
Individuals at Risk of Type 2 Diabetes
and/or Cardiovascular Disease. Diabetes
Care 27, 26762681 (2004).
12. Isomaa B, Almgren P, Tuomi T et al.:
Cardiovascular Morbidity and Mortality
Associated with the Metabolic Syndrome.
Diabetes Care 24, 683689 (2001).
13. Gaede P, Vedel P, Larsen N et al.:
Multifactorial Intervention and
Cardiovascular Disease in Patients with Type
2 Diabetes. 348 (5), 383393 (2003).
14. Fruhbeck G, Ambrosi JG, Muruzabal FJ,
Burrell MA: The adipocyte: a model for
integration of endocrine and metabolic
signaling in energy metabolism regulation.
Am. J. Physiol. Endocrinol. Metab. 280,
E827E847 (2001).
15. Bays H, Mandarino L, DeFronzo RA. Role of
the Adipocyte, FFA, and Ectopic Fat in
Pathogenesis of Type 2 Diabetes Mellitus. J.
Clin. Endocrinol. Metab. 89, 463478 (2004).
Describes the authors perspective with
regard to adipocyte function and
dysfunction in the pathogenesis of Type 2
diabetes mellitus, with an emphasis on
thiazolidinediones.
16. Bays HE, Stein EA: Pharmacotherapy for
Dyslipidemia Current Therapies and
Future Agents. Expert Opin. Pharmacother. 4
(11), 19011938 (2003).
Comprehensive review of lipid-altering
drugs in development, and their
physiological rationale. May be most
interesting to those invovled in lipid-
altering drug clinical trials.
17. Karelis AD, St-Pierre DH, Conus F et al.:
Metabolic and Body Composition Factors in
Subgroups of Obesity: What Do We Know?
J. Endocrinol. Metab. 89(6),
25692575 (2004).
The relationship of obesity to metabolic
consequences and adipose tissue
composition varies among obesity
subgroups.
18. Kratchmarova I, Kalume DE, Blagoev B
et al.: A Proteomic Approach for
Identification of Secreted Proteins During
the Differentiation of 3T3-L1 Preadipocytes
to Adipocytes. Mol. Cell. Proteomics 1,
213222 (2002).
Using a systematic proteomic approach to
purify and identify secreted factors that are
differentially expressed in preadipocytes
versus adipocytes, various novel secreted
proteins were found.
19. Sims EA: Are there persons who are obese,
but metabolically healthy? Metabolism
50(12), 14991504 (2001).
20. Abate N, Garg A, Peshock RM, Stray-
Gundersen J, Adams-Huet B, Grundy SM:
Relationship of generalized and regional
adiposity to insulin sensitivity in men with
NIDDM. Diabetes 45(12),
16841693 (1996).
21. Abate N, Garg A, Peshock RM, Stray-
Gundersen J, Grundy SM: Relationships of
generalized and regional adiposity to insulin
sensitivity in men. J. Clin. Invest. 96(1),
8898 (1995).
Subcutaneous truncal fat plays a major role
in obesity-related insulin resistance in
healthy, non-diabetic men.
22. Goodpaster BH, Thaete FL, Simoneau JA,
Kelley DE: Subcutaneous abdominal fat and
thigh muscle composition predict insulin
sensitivity independently of visceral fat.
Diabetes 46(10), 15791585 (1997).
23. Smith SR, Lovejoy JC, Greenway F et al.:
Contributions of total body fat, abdominal
subcutaneous adipose tissue compartments,
and visceral adipose tissue to the metabolic
complications of obesity. Metabolism 50(4),
425435 (2001).
24. Tchkonia T, Pirtskhalava T, Giorgadze N
et al.: Human Preadipocyte Strains Derived
from Single Cells by Stably Expressing
Telomerase Retain Fat Depot-Specific
Characteristics. Oral Presentation.
NAASOs 2004 Annual Meeting. Volume
12. October 2004 supplements Programme
Abstracts. Oral Presentation November
1418, 2004 Las Vegas, USA.
25. UK Prospective Diabetes Study 27. Plasma
lipids and lipoproteins at diagnosis of
NIDDM by age and sex. Diabetes Care 20,
16831687 (1997).
26. Garg A: Acquired and inherited
lipodystrophies. N. Engl. J. Med. 350 (12),
12201234 (2004).
27. Abate N, Chandalia M, Snell PG, Grundy
SM: Adipose tissue metabolites and insulin
resistance in nondiabetic Asian Indian men.
J. Clin. Endocrinol. Metab. 89(6),
27502755 (2004).
In absence of obesity, South Asians have
changes in plasma adipokines similar to
what is found in obese Caucasians.
28. Chandalia M, Abate N, Garg A, Stray-
Gundersen J, Grundy SM: Relationship
between generalized and upper body obesity to
insulin resistance in Asian Indian men. J. Clin.
Endocrinol. Metab. 84, 23292335, (1999).
South Asians are more insulin resistant than
Caucasians, even when not obese and with
even with similar body fat distribution.
REVI EW Bays, Abate & Chandalia
58 Future Cardiology (2005) 1(1)
29. Chandalia M. Cabo-Chan A.V., Devaraj S.,
Jialal I., Grundy S.M: Elevated plasma high-
sensitivity C-reactive protein concentrations
in Asian Indians living in the United States.
J. Clin. Endocrinol. Metab. 88,
37733776, (2003).
South Asians have increased plasma
concentrations of hs-CRP even when not
obese and even in the absence of type 2
diabetes mellitus.
30. Feingold KR, Grunfeld C, Pang M, Doerrler
W, Krauss RM: LDL subclass phenotypes
and triglyceride metabolism in non-insulin-
dependent diabetes. Arterioscler. Thromb. 12,
14961502 (1992).
31. Selby JV, Austin MA, Newman B, Zhang D,
Quesenberry CP Jr, Mayer EJ et al.: LDL
subclass phenotypes and the insulin
resistance syndrome in women. Circulation
88, 381387 (1993).
32. St. Onge MP, Janssen I, Heymsfield SB:
Metabolic syndrome in normal-weight
Americans. Diabetes Care 27,
22222228 (2004).
33. Brown CD, Higgins M, Donato KA et al.:
Body Mass Index and the Prevalence of
Hypertension and Dyslipidemia. Obes. Res.
8(9), 605619 (2000).
34. Bornstein ME, Zepter VL, Schraven A, et al.:
Human adipocytes secrete mineralocorticoid-
releasing factors. Proc. Natl Acad. Sci. USA
100(24), 1421114216 (2003).
35. Livingston E: Serum Lipids are Paradoxically
Decreased with Increasing Obesity. Poster
493-P. Volume 12 October 2004 Abstracts
NAASOs 2004 Annual Meeting November
1418 2004 Las Vegas, Nevada, USA.
An increase in BMI does not always have a
linear relationship with associated
metabolic consequences normally
associated with obesity.
36. Bays HE, McGovern ME: Once-Daily
Niacin Extended-Release/Lovastatin
Combination Tablet has More Favorable
Effects on Lipoprotein Particle Size and
Subclass Distribution Compared to
Atorvastatin and Simvastatin. Prev. Cardiol.
6, 179188 (2003).
37. Bays H: Niacin Extended-Release/Lovastatin:
The First Combination Product for
Dyslipidemia. Expert Rev. Cardiovasc. Ther.
2(4), 89105 (2004).
38. Taskinen MR: Diabetic dyslipidaemia: from
basic research to clinical practice.
Diabetologia 46, 733749 (2003).
39. Bays HE: Atherogenic Dyslipidaemia in
Type 2 Diabetes and Metabolic Syndrome:
Current and Possible Future Treatment
Options. Br. J. Diabetes Vasc. Dis. 3(5)
356360 (2003).
40. Buse J: Lipid changes associated with
diabetes therapy. Practical Diabetology 2429
(2003).
41. Nadler ST, Stoehr JP, Schueler KL et al.: The
expression of adipogenic genes is decreased
in obesity and diabetes mellitus. PNAS
97(21), 1137111376 (2000).
Murine study in which the expression level
of over 11,000 transcripts were analyzed,
demonstrating 214 transcript differences in
between lean and obese mice.
42. Gregoire FM, Smas CM, Sul HS:
Understanding adipocyte differentiation.
Physiol. Rev. 78(3), 783809 (1998).
43. Hegarty BD, Furler SM, Oakes N et al.:
Peroxisome Proliferator-Activated
Receptor (PPAR) Activation Induces
Tissue-Specific Effects on Fatty Acid
Uptake and Metabolism in vitro A Study
Using the Novel PPAR / Agonist
Tesaglitazar. Endocrinology 145,
31583164 (2004).
44. Bayes M, Rabasseda X, Prous JR: Gateway to
clinical trials. Methods Find. Exp. Clin.
Pharmacol. 26(7), 587612 (2004).
45. Isaacsohn JL, Troendle AJ, Orloff DG:
Regulatory issues in the approval of new
drugs for diabetes mellitus, dyslipidemia,
and the metabolic syndrome. Am. J. Cardiol.
93(11A), 49C52C (2004).
A very important review which includes an
author who is a member of the US Food
and Drug Administration.
46. Fleming A: FDA approach to the regulation
of drugs for diabetes. Am. Heart J. 138(5 Pt
1), S338S345 (1999).
47. Pasquali SK, Sanders SP, Li JS: Oral
antihypertensive trial design and analysis
under the pediatric exclusivity provision.
Am. Heart J. 144(4), 608614 (2002).
48. Draft Consensus Document. The European
Agency for the Evaluation of Medicinal
Products. Evaluation of Medicines for Human
Use. ICH Topic E 12 A. Principles for Clinical
Evaluation of New Antihypertensive Drugs.
London, 17, 29 June 2000.
49. Orloff DG: FDA 2004: Revisiting the 1996
Obesity Drug Guidance. PowerPoint
Presentation. Endocrinologic and metabolic
Drugs Advisory Committee
September 8, 2003.
50. Moller DE: New drug targets for Type 2
diabetes and the metabolic syndrome.
Nature 414, 821827 (2001).
51. Ginsberg HN. Treatment for patients with
the metabolic syndrome. Am. J. Cardiol.
91(7A), 29E39E (2003).
52. Garber AJ: The Metabolic Syndrome.
Med. Clin. North Am. 88(4), 837846
(2004).
53. Tan EM, Cohen ES, Fries JF et al.: The
1982 revised criteria for the classification of
systemic lupus erythematosus. Arthritis
Rheum. 25, 12711277 (1982).
54. Shadid S, Stehouwer C, Jensen M: Evidence
Against an Endocrine Role for Resistin, TNF-
and IL-6 in Upper Body Obesity. Oral
Presentation. NAASOs 2004 Annual Meeting.
Volume 12. October 2004 supplements
Programme Abstracts. Oral Presentation
November 1418, 2004 Las Vegas, USA.
55. Dale L, Anthenelli R, Despres J-P, Golay A,
Sjostrom L: Effects of rimonabant in the
reduction of major cardiovascular risk
factors. Results from the STRATUS-US
Trial (Smoking Cessation in Smokers
Motivated to Quit) and the RIO-LIPIDS
Trial (Weight Reducing and Metabolic
Effects in Overweight/Obese Patients with
Dyslipidemia). Late-Breaking Clinical Trials
II. American College of Cardiology
Scientific Session 2004, March 710, 2004,
New Orleans, Louisiana, USA
56. Pi-Sunyer FX: Effect of rimonabant on
weight reduction and weight maintenance:
RIO-NORTH AMERICA (RIO-NA) trial.
Late-Breaking Clinical Trials III, American
Heart Association Scientific Sessions 2004,
November 710, 2004, New Orleans,
Louisiana, USA.
57. Bensaid M, Gary-Bobo M, Esclangon A
et al.: The cannabinoid CB1 receptor
antagonist SR141716 increases Acrp30
mRNA expression in adipose tissue of obese
fa/fa rats and in cultured adipocyte cells.
Mol. Pharmacol. 63(4), 908914 (2003).
Websites
101. World Health Organization. Obesity and
overweight facts.
www.who.int/hpr/NPH/docs/gs_obesity.pdf
(Accessed December 2004).
102. Orlistat website
www.xenical.com/hcp/2_hrod.asp Health
risks of obesity.
(Accessed December 2004).
103. National Institute of Diabetes & Digestive
& Kidney Diseases.
www.niddk.nih.gov/stastistics/index.htm.
Prevalence statistics related to overweight
and obesity.
(Accessed December 2004)
104. National Center for Health Statistics.
http://cdc.gov/nchs/products/elec_prods/su
bject/nhanes3.htm Third National Health
and Nutrition Examination Survey
(NHANES III) Public Use Data Files.
(Accessed December 2004).
Provides striking data and facts from
NHANES III regarding obesity.
www.futuremedicine.com 59
Adiposopathy REVI EW
105. National heart lung and blood institute. The
practical guide to the identification,
evaluation and treatment of overweight and
obesity in adults.
www.nhlbi.nih.gov/guidelines/obesity/prctg
d_b.pdf
(Accessed December 2004).
Represents a consensus statement from the
National Institute of Health, National
Heart, Lung and Blood Institute and the
North American Association for the Study
of Obesity.
106. www.lipidsonline.org/
(Accessed December 2004)
Ginsberg, H. Diabetic Dyslipidemia and
Atherosclerosis
Affiliations
Harold Bays MD, FACP
Medical Director/President, L-MARC Research
Center, Louisville, KY, USA
hbaysmd@aol.com
Nicola Abate MD
Associate Professor of Internal Medicine, Division
of Endocrinology and Metabolism & Clinical
Nutrition, Director of UT Southwestern Lipid &
Heart Disease Risk Management Clinic Risk
Management Clinic, Center for Human Nutri-
tion, Dallas, Texas, USA
nicola.abate@utsouthwestern.edu
Manisha Chandalia MD
Associate Professor of Internal Medicine, Division
of Endocrinology and Metabolism & Clinical
Nutrition, UT Southwestern Lipid & Heart Dis-
ease Risk Management Clinic, Risk Management
Clinic, Center for Human Nutrition, Dallas,
Texas, USA
manisha.chandalia@utsouthwestern.edu
Vous aimerez peut-être aussi
- Viral Haem Fevers Nigeria PDFDocument60 pagesViral Haem Fevers Nigeria PDFChikezie OnwukwePas encore d'évaluation
- WHO-SEARO Snakebite Guidelines 2010Document162 pagesWHO-SEARO Snakebite Guidelines 2010Galantry Ahmad AzhariPas encore d'évaluation
- MRCP EcgDocument52 pagesMRCP EcgHasan Mahmud100% (1)
- Guidelines For Dissertation FormatsDocument4 pagesGuidelines For Dissertation FormatsChikezie OnwukwePas encore d'évaluation
- Guidelines For Dissertation FormatsDocument4 pagesGuidelines For Dissertation FormatsChikezie OnwukwePas encore d'évaluation
- MDGs-SDGs2015 Toc PDFDocument10 pagesMDGs-SDGs2015 Toc PDFChikezie OnwukwePas encore d'évaluation
- CDC Document Ebola Nigeria PDFDocument32 pagesCDC Document Ebola Nigeria PDFChikezie OnwukwePas encore d'évaluation
- Medicine As A BusinessDocument33 pagesMedicine As A BusinessChikezie OnwukwePas encore d'évaluation
- Arafah ReviewDocument21 pagesArafah ReviewChikezie OnwukwePas encore d'évaluation
- Adrenal Gland Disorders PDFDocument12 pagesAdrenal Gland Disorders PDFChikezie OnwukwePas encore d'évaluation
- Tiozzo HDL Subfractions and Carotid PlaqueDocument7 pagesTiozzo HDL Subfractions and Carotid PlaqueChikezie OnwukwePas encore d'évaluation
- HI76933 - Daily Meal Planning Guide - EnglishDocument5 pagesHI76933 - Daily Meal Planning Guide - EnglishChikezie OnwukwePas encore d'évaluation
- Guias para El Diagnostico y Tratamiento de Acromegalia AACE 2011Document44 pagesGuias para El Diagnostico y Tratamiento de Acromegalia AACE 2011Ricardo HemurPas encore d'évaluation
- Gender Nigeria2012Document99 pagesGender Nigeria2012Chikezie OnwukwePas encore d'évaluation
- Mittendorf Giant InsulinomaDocument6 pagesMittendorf Giant InsulinomaChikezie OnwukwePas encore d'évaluation
- Tests in EndocrinologyDocument1 pageTests in EndocrinologyChikezie OnwukwePas encore d'évaluation
- Nigeria PHC TextDocument86 pagesNigeria PHC TextChikezie OnwukwePas encore d'évaluation
- Stephens Performance of Two New AlgorithmsDocument7 pagesStephens Performance of Two New AlgorithmsChikezie OnwukwePas encore d'évaluation
- Bariatric GuidelinesDocument83 pagesBariatric Guidelinessavvy_as_98100% (1)
- PSRDocument169 pagesPSRvitogbadosPas encore d'évaluation
- Abdulraheem Et Al PHC in NigeriaDocument9 pagesAbdulraheem Et Al PHC in NigeriaChikezie OnwukwePas encore d'évaluation
- Civil Service ServicomDocument71 pagesCivil Service ServicomChikezie OnwukwePas encore d'évaluation
- Kahaly Polyglandular Autoimmune SyndromesDocument10 pagesKahaly Polyglandular Autoimmune SyndromesChikezie OnwukwePas encore d'évaluation
- Canadian Lipid Guidelines Update: FacultyDocument4 pagesCanadian Lipid Guidelines Update: FacultyChikezie OnwukwePas encore d'évaluation
- Clinical Guideines For The MGT of DsdsDocument73 pagesClinical Guideines For The MGT of DsdsChikezie OnwukwePas encore d'évaluation
- Hassan Doing A Pilot StudyDocument4 pagesHassan Doing A Pilot StudyChikezie OnwukwePas encore d'évaluation
- Association Between Glycaemic Control and Erectile Dysfunction PDFDocument2 pagesAssociation Between Glycaemic Control and Erectile Dysfunction PDFAlmira Shabrina SaraswatiPas encore d'évaluation
- Maurice Nicoll The Mark PDFDocument4 pagesMaurice Nicoll The Mark PDFErwin KroonPas encore d'évaluation
- The Yellow House: A Memoir (2019 National Book Award Winner)D'EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Évaluation : 4 sur 5 étoiles4/5 (98)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceD'EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceÉvaluation : 4 sur 5 étoiles4/5 (895)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeD'EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeÉvaluation : 4 sur 5 étoiles4/5 (5794)
- The Little Book of Hygge: Danish Secrets to Happy LivingD'EverandThe Little Book of Hygge: Danish Secrets to Happy LivingÉvaluation : 3.5 sur 5 étoiles3.5/5 (399)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaD'EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaÉvaluation : 4.5 sur 5 étoiles4.5/5 (266)
- Shoe Dog: A Memoir by the Creator of NikeD'EverandShoe Dog: A Memoir by the Creator of NikeÉvaluation : 4.5 sur 5 étoiles4.5/5 (537)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureD'EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureÉvaluation : 4.5 sur 5 étoiles4.5/5 (474)
- Never Split the Difference: Negotiating As If Your Life Depended On ItD'EverandNever Split the Difference: Negotiating As If Your Life Depended On ItÉvaluation : 4.5 sur 5 étoiles4.5/5 (838)
- Grit: The Power of Passion and PerseveranceD'EverandGrit: The Power of Passion and PerseveranceÉvaluation : 4 sur 5 étoiles4/5 (588)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryD'EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryÉvaluation : 3.5 sur 5 étoiles3.5/5 (231)
- The Emperor of All Maladies: A Biography of CancerD'EverandThe Emperor of All Maladies: A Biography of CancerÉvaluation : 4.5 sur 5 étoiles4.5/5 (271)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyD'EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyÉvaluation : 3.5 sur 5 étoiles3.5/5 (2259)
- On Fire: The (Burning) Case for a Green New DealD'EverandOn Fire: The (Burning) Case for a Green New DealÉvaluation : 4 sur 5 étoiles4/5 (73)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersD'EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersÉvaluation : 4.5 sur 5 étoiles4.5/5 (344)
- Team of Rivals: The Political Genius of Abraham LincolnD'EverandTeam of Rivals: The Political Genius of Abraham LincolnÉvaluation : 4.5 sur 5 étoiles4.5/5 (234)
- The Unwinding: An Inner History of the New AmericaD'EverandThe Unwinding: An Inner History of the New AmericaÉvaluation : 4 sur 5 étoiles4/5 (45)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreD'EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreÉvaluation : 4 sur 5 étoiles4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)D'EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Évaluation : 4.5 sur 5 étoiles4.5/5 (121)
- Her Body and Other Parties: StoriesD'EverandHer Body and Other Parties: StoriesÉvaluation : 4 sur 5 étoiles4/5 (821)
- EcardDocument2 pagesEcardBITI Education Pvt. Ltd.Pas encore d'évaluation
- The START and JumpSTART MCI Triage ToolsDocument54 pagesThe START and JumpSTART MCI Triage ToolsAdreiTheTripleAPas encore d'évaluation
- Risoles Rendah ProteinDocument6 pagesRisoles Rendah ProteinYavanisa Safira R.Pas encore d'évaluation
- Standard 8Document8 pagesStandard 8Bridget GumboPas encore d'évaluation
- Homework Policy ScotlandDocument9 pagesHomework Policy Scotlandafmtdenav100% (1)
- 1 Shiong LW SARCOPENIA UPDATEDocument8 pages1 Shiong LW SARCOPENIA UPDATEdavidtuanandartuaPas encore d'évaluation
- POLYPHASE 678 SdsDocument8 pagesPOLYPHASE 678 SdsMarianna JassoPas encore d'évaluation
- POC and Concepts Maps Week 12Document23 pagesPOC and Concepts Maps Week 12Michelle CollinsPas encore d'évaluation
- IDocument14 pagesIjasdeepkaurnagra100% (1)
- UCSD Internal Medicine Handbook 2011Document142 pagesUCSD Internal Medicine Handbook 2011ak100007100% (5)
- Example of Health GenogramDocument1 pageExample of Health Genogramapi-322059527Pas encore d'évaluation
- 3a DnDestiny - BestiaryoftheWilds - v0.5Document46 pages3a DnDestiny - BestiaryoftheWilds - v0.5HectorPas encore d'évaluation
- Advertising Solutions From Oxford University PressDocument12 pagesAdvertising Solutions From Oxford University PressGeorge FelintoPas encore d'évaluation
- Argumentative Essay: Is Meat Murder?Document2 pagesArgumentative Essay: Is Meat Murder?Petra Gabriella PatakiPas encore d'évaluation
- Operational Excellence Management SystemDocument20 pagesOperational Excellence Management SystemChevano Luna100% (1)
- Landscaping MechanicsDocument3 pagesLandscaping MechanicsArchimedes Magsayo Casama80% (5)
- Anglais 2ndeDocument33 pagesAnglais 2ndeMario RobillardPas encore d'évaluation
- Medical OncologyDocument41 pagesMedical Oncologylavadey2Pas encore d'évaluation
- Chap 2Document92 pagesChap 2Nur IffatinPas encore d'évaluation
- Risk AssessmentDocument9 pagesRisk AssessmentSabheeh Ali100% (1)
- Medical Health Care PowerPoint TemplatesDocument88 pagesMedical Health Care PowerPoint Templateslily beautyPas encore d'évaluation
- PSA Blueprint June2016Document21 pagesPSA Blueprint June2016Byron Lu MorrellPas encore d'évaluation
- Term Paper-Draft Social Anxiety Disorder (Sad) Among AdultsDocument13 pagesTerm Paper-Draft Social Anxiety Disorder (Sad) Among AdultsWafiPas encore d'évaluation
- Group 01: Articles For ReviewDocument4 pagesGroup 01: Articles For ReviewPrincess Krenzelle BañagaPas encore d'évaluation
- NGT FeedingDocument74 pagesNGT FeedingGoddy Manzano100% (1)
- Family Planning PPTDocument22 pagesFamily Planning PPTLance De Leon100% (1)
- Quiz 2Document3 pagesQuiz 2air france bargamentoPas encore d'évaluation
- General Dentistry Informed Consent FormDocument3 pagesGeneral Dentistry Informed Consent FormNishtha KumarPas encore d'évaluation
- Application of Recombinant DNADocument2 pagesApplication of Recombinant DNANathan B. MhinePas encore d'évaluation
- Doroga Bahrm21s1 Pe003 Fitness Journal LogDocument4 pagesDoroga Bahrm21s1 Pe003 Fitness Journal LogJeah Joyce LagrimasPas encore d'évaluation