Académique Documents
Professionnel Documents
Culture Documents
Case Study
Transféré par
api-240695207Titre original
Copyright
Formats disponibles
Partager ce document
Partager ou intégrer le document
Avez-vous trouvé ce document utile ?
Ce contenu est-il inapproprié ?
Signaler ce documentDroits d'auteur :
Formats disponibles
Case Study
Transféré par
api-240695207Droits d'auteur :
Formats disponibles
Case Study: Post-Surgical Rehabilitation of Bankart and Hill-Sachs Labral Lesions with a Ruptured Biceps Tendon.
By: Wade B. Price; ATS
INTRODUCTION Labral tears are an extremely common injury amongst athletes, especially athletes that participate in sports that involve extensive over-head arm motion. There are multiple types of labral tears that involve varying aspects of the glenohumeral joint. A Bankart lesion is a detachment of the capsuloligamentous complex from the glenoid rim, and it accounts for 87-100% of first time anterior shoulder dislocations.1 A Hill-Sachs lesion is an impression fracture of the posterolateral humeral head upon dislocation, and it accounts for 64-100% of first time anterior shoulder dislocations. 1 Most of these types of injuries present symptomatically with pain, possible clicking in the shoulder, weakness, and instability. According to the literature1 , combined lesions have become a more recognized and reported pathology. There is also a relationship between the location of the origin of the long head of the biceps and the types of labral injuries sustained.2 There are multiple forms of treatment for these varying labral injuries, many of them involving surgical procedures to repair the damaged labrum. The purpose of this report is to present the surgical treatment and rehabilitation process used in the case of a 21-year-old male wrestler, who had sustained both a Bankart and Hill-Sachs lesion along with a biceps tendon rupture, in comparison to what the most updated research suggests. See figure 1 below for a lateral view of a normal shoulder complex.
Phase of Rehabilitation Phase 1 Phase Specific Goals Allow soft tissue healing Decrease pain and inflammation Initiate protective range of motion (ROM) Prevent muscular atrophy Restore full pain-free ROM Increase dynamic stability and muscular strength Normalize arthrokinematics Improve strength, power, and endurance Enhance neuromuscular control Functional activities to prepare athlete for throwing motions
Phase 2
Phase 3
For exercises in phase three, the patient will continue to perform all stretches done previously including AROM exercises and passive stretching. Consistent with the literature we placed a great emphasis on getting the patients ROM completely reestablished, especially external rotation.12 Losses in external rotation ROM increases the occurrences of osteoarthritis, so all attempts to regain this motion should be made.12The physicians protocol also calls for neuromuscular control and dynamic stabilization drills. The loss of stability at the shoulder joint results in a lack of stimulation of the mechano-receptors at the shoulder.13 This in turn causes a lack of proprioceptive input to the central nervous center which can lead to abnormal muscle firing patterns and changes in joint stiffness.13 In addition to proprioceptive exercises, rehabilitation in phase three should involve strengthening for sports specific functions coupled with proprioceptive and kinesthetic exercises.14The physicians protocol was in line with this too. In addition, based on the physicians recommendations, the patient began more aggressive strengthening exercises such as the Throwers Ten program, isotonics, and progressive plyometrics. The patient also started an interval sports program to start to re-acclimate the patient back into sport.
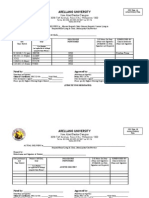
Figure 2: Above is a table that covers all of the rehabilitation goals as written by the acting physician for this particular case. DISCUSSION Athletes that participate in sports that involve repetitive overhead motions have a predisposition for shoulder injuries because of the constant use in these extreme ranges of motion.5 In this particular case, as most wrestlers experience, the patient was put into an extreme overhead ROM which caused the patient to dislocate his right shoulder. The patient had a long history of anterior instability of his right shoulder. Anterior subluxations are often the source of overhead athletes problems such as limited range of motion or in severe cases labral pathologies.5 Even though there have been rehabilitation programs developed to treat anterior instability conservatively, operative intervention still may be required.5 It is also common for biceps brachii long head tendon injuries to occur in conjunction with tears of the glenoid labrum.4,6 In the case of our patient, he sustained a biceps tendon rupture in conjunction with his Bankart (the most common pathology from anterior shoulder instability)6 and Hill-Sachs lesions. He did require operative intervention in the form of a Bankart Repair. Post-operatively, during the first phase of rehabilitation (weeks 1-8) the patient was instructed to stay immobilized in a sling for the first 4 weeks as outlined in the literature.3 The patient completed exercises that focused on range of motion and stabilization. For the first 4 weeks, while still immobilized, the patient conducted isometric exercises in the sling for shoulder flexion, extension, abduction, internal rotation, and external rotation. Isometrics are extremely effective with strengthening the stabilizing muscles of the shoulder complex. 3,5 They also help the patient to regain neuromuscular control.3 The sling was discontinued after the first 4 weeks of the patients phase one program. The isometrics were still continued and more stabilizer muscle strengthening exercises were introduced. These exercises consisted of rhythmic stabilizations at 90 degrees of shoulder flexion, in abduction, and in scaption. These exercises, as recommended 5, were done with the patients hand pressed against an exercise ball which was pushed against a wall. Range of motion exercises were also introduced at this time. These exercises include assisted active range of motion (with the aid of a cane) for shoulder flexion to 90 degrees, abduction to 75 degrees, internal rotation(scapular plane) to 45 degrees, and external rotation(scapular plane) to 20 degrees. These exercises were limited to such small degrees, avoiding long arm lever motions for this stage of the rehabilitation process.5 The use of ice and electrical stimulation was continued throughout this phase, as instructed by the attending physician. The progression from phase one of this patients shoulder rehabilitation, post Bankart repair, to phase two was based upon the completion of his phase one program and exercises, as well as being cleared by the acting physician. As stated in the phase one analysis, this patient underwent a Bankart repair after suffering a labral tear while competing in the first wrestling match of the season. A typical Bankart repair has a standard healing time of about six months which is the approximate goal time span for this particular case.8 The phase two program for this patient was outlined by the physician to be within weeks 8-22. The primary goal for most all phase two programs is to try and return the patient to normal levels of flexibility and strength. As outlined by the physician, the phase two program was broken up into three progressive segments. The first segment is weeks 8-12, in which all exercises remained the same as phase one. All ROM exercises were progressed in degree. The second segment was weeks 12-16, in which all exercises remained the same and ROM was progressed further. The third segment was weeks 16-22, in which all exercises and ROM remained the same. In this final segment of phase two more aggressive techniques were cleared by the physician to start muscular strengthening. This phase two protocol differs from the literature as it does not yet involve whole body and core exercises. According to the literature, it is beneficial to include kinetic chain shoulder rehabilitation exercises to encourage flexibility and strength gains in more functional movements, along with improving neuromuscular function.7 Much of what has been outlined by the acting physician does, however, agree with the literature for phase two goals. As the research shows phase two is the time to become more aggressive in ROM and to increase the patients strength and neuromuscular function.9 The literature agrees with the physicians protocol on this matter including the means of achieving these goals through the use of isotonic dumbbell exercises.9 Another exercise that could be added in addition to the acting physicians phase two protocol would be a progressive series of Codmans pendulum exercises. Codmans exercises are a very beneficial method of distraction of the joint to allow an increased flow of nutrients into the joint space, as well as getting good motion out of the joint to help increase neuromuscular control.10 Overall, the physicians rehabilitation program for the patients phase two does agree quite well with the available literature. That being said, there are many other beneficial techniques that are not being utilized by this current program that could and possibly should be explored for this particular case. As the patient enters the third and final stage of rehabilitation, the focus turns more towards exercises to prepare the athlete for returning to competition. The goals for this patients phase three rehabilitation plan, according to the acting physicians protocol, are to improve muscular strength, power, and endurance, enhance neuromuscular control, and to start incorporating functional activities. Current literature completely agrees with the physicians goals for this phase as they too have their main phase three goals as improvement of strength, power, endurance, and neuromuscular control.11 In accordance with the physicians protocol, the patient could only enter into phase three after he has achieved full pain-free ROM, has no pain or tenderness, and has muscular strength at 80% of the contralateral side. This protocol varies very slightly from what is stated in literature. Research states that most post-surgical patients can enter into phase three once they have nearly full pain-free ROM and they must have 70% muscle strength compared to the contralateral side.11 The patient is currently still in his phase three protocol and doing very well with his rehabilitation. CONCLUSION Through the processes I have done to complete this case study including all of the research that went into this, I have learned a great deal about the complexities of designing a rehabilitation program for a post-operative shoulder as well as how to more efficiently create a basic rehabilitation program in general. To give my own recommendations as how to handle this situation, I would agree with most of this particular rehabilitation protocol. The physicians protocol almost entirely agreed with what I read throughout my research. It is within his phase two protocol that I differ from him. The research showed that integrating core and whole body exercises including closed kinetic chain shoulder exercises is a great way to start the strengthening process. I would also include Codmans exercises in my phase two. These exercises not only help with distraction of the joint encouraging nutrient flow, but they also help increase neuromuscular control through enhanced proprioception. I would leave all other exercises and protocols listed with this case study as stated.
REFERENCES IN AMA FORMAT: 1. Dickens J, Kilcoyne K, Giuliani J, Owens B. Circumferential Labral Tears Resulting From a Single Anterior Glenohumeral Instability Event: A Report of 3 Cases in Young Athletes. American Journal Of Sports Medicine [serial online]. January 2012;40(1):213-217. Available from: SPORTDiscus with Full Text, Ipswich, MA. Accessed January 28, 2013. 2. Jakanani G, Botchu R, Rennie W. The MR arthrographic anatomy of the biceps labral insertion and its morphological significance with labral tears in patients with shoulder instability. European Journal Of Radiology [serial online]. November 2012;81(11):3390-3393. Available from: CINAHL Plus with Full Text, Ipswich, MA. Accessed February 4, 2013. 3. Mcdonough A, Funk L. Critical reflection of the advanced rehabilitation of an elite rugby league player sustaining a posterior Bankart lesion. Phys Ther Sport. 2013;14(1):60-7. 4. Miller T, Jones G. Arthroscopic evaluation and treatment of biceps brachii long head tendon injuries: A survey of the MOON shoulder group. Int J Shoulder Surg. 2011;5(3):68-71. 5. Levine, W. N. (1999). New approaches to the care of the athlete's shoulder. Sports Medicine & Arthroscopy Review, 7(2), 128-133. 6. Jancosko JJ, Kazanjian JE. Shoulder injuries in the throwing athlete. Phys Sportsmed. 2012;40(1):84-90. 7. Mcmullen J, Uhl TL. A kinetic chain approach for shoulder rehabilitation. J Athl Train. 2000;35(3):329-37. 8. Miles JW, Tasto JP. Arthroscopic Bankart repair of anterior shoulder instability in the athlete. Operative Techniques in Sports Medicine. 2004;12(2):126-134. 9. Mccarty EC, Ritchie P, Gill HS, Mcfarland EG. Shoulder instability: return to play. Clin Sports Med. 2004;23(3):335-51, vii-viii. 10. Ellsworth AA, Mullaney M, Tyler TF, Mchugh M, Nicholas S. Electromyography of Selected Shoulder Musculature During Un-weighted and Weighted Pendulum Exercises. N Am J Sports Phys Ther. 2006;1(2):73-9. 11. Mccarty EC, Ritchie P, Gill HS, Mcfarland EG. Shoulder instability: return to play. Clin Sports Med. 2004;23(3):335-51, vii-viii. 12. Itoi E, Watanabe W, Yamada S, Shimizu T, Wakabayashi I. Range of motion after Bankart repair. Vertical compared with horizontal capsulotomy. Am J Sports Med. 2001;29(4):441-5. 13. Gibson J. (iii) Rehabilitation after shoulder instability surgery. Current Orthopaedics. 2004;18(3):197-209. 14. Stein T, Linke RD, Buckup J, et al. Shoulder sport-specific impairments after arthroscopic Bankart repair: a prospective longitudinal assessment. Am J Sports Med. 2011;39(11):2404-14. 15. Available at: http://www.therafit.com/Injuries-Conditions/Shoulder/Shoulder-Anatomy/a~361/article.html. Accessed April 23, 2013.
Figure 1: Above is a picture of the skeletal anatomy of a normal shoulder complex from a lateral view.15 This view gives a great depiction of the areas that were affected in this case, the labrum and the insertion of the long head of the biceps tendon.
BACKGROUND This patient is a 21-year-old male Indiana University wrestler. He presented with right shoulder anteroinferior instability. He participated in a wrestling match on the weekend of November 3rd, where he had two events where his right shoulder dislocated and had to be manually relocated. The wrestler said that he has had over 30 episodes of subluxation on his right shoulder previously. An MRI was ordered for his shoulder which showed a large Bankart detachment with a Hill-Sachs lesion. He had a positive anterior apprehension relocation test during his physical examination. This special test was the only performed. DIFFERENTIAL DIAGNOSIS For this particular case, possible injuries expected before proper evaluation were a SLAP tear, Bankart lesion, Hill-Sachs lesion, and a ruptured biceps tendon. TREATMENT After a physical examination with the physician, an MRI was ordered which revealed that the patient had a Bankart detachment with a Hill-Sachs lesion. It was also discovered that he had a biceps tendon rupture with disruption of the superior labrum. Upon discussion with the physician, the patient decided to proceed with the right shoulder arthroscopic Bankart repair. During the operation, the patients shoulder was examined again while he was under anesthesia. During examination the patient demonstrated 3+ anterior instability, and had no inferior or posterior instability. The surgeon performed an arthroscopic Bankart repair where a total of three anchors were placed into the anterio-inferior quadrant of the labrum. An arthroscopic superior labral repair was also performed at this time. Post-operatively, sterile dressings were applied, followed by a shoulder immobilizer. The patient tolerated the procedures well and had no complications. The surgery was performed on 11-8-12. On November 13, 2012 the patients sutures were removed and the physician cleared him to begin the first phase of his rehabilitation program. Since then, the patient has been advanced to the next phase of his rehabilitation program on 12-4-12. Specifics of the different phases for this patients rehabilitation will be discussed in the discussion section. For more information see figure 2 at top. UNIQUENESS Labral injuries among athletes are not uncommon by any means. This particular case, however, presented with unique characteristics as it involved more structures than the common labral pathology. The patient had a Bankart and Hill-Sachs lesion together which is rare but the most unique characteristic of this injury was that it also involved a complete rupture of the long-head biceps tendon.
Vous aimerez peut-être aussi
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeD'EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeÉvaluation : 4 sur 5 étoiles4/5 (5794)
- Shoe Dog: A Memoir by the Creator of NikeD'EverandShoe Dog: A Memoir by the Creator of NikeÉvaluation : 4.5 sur 5 étoiles4.5/5 (537)
- Case Study AbstractDocument1 pageCase Study Abstractapi-240695207Pas encore d'évaluation
- General Medical Case StudyDocument1 pageGeneral Medical Case Studyapi-240695207Pas encore d'évaluation
- Billing ChartDocument1 pageBilling Chartapi-240695207Pas encore d'évaluation
- Cip 9Document1 pageCip 9api-240695207Pas encore d'évaluation
- Soap NoteDocument1 pageSoap Noteapi-240695207Pas encore d'évaluation
- Cip 9Document1 pageCip 9api-240695207Pas encore d'évaluation
- Soap NoteDocument1 pageSoap Noteapi-240695207Pas encore d'évaluation
- Soap Note BackDocument1 pageSoap Note Backapi-240695207Pas encore d'évaluation
- Jessica DoeDocument1 pageJessica Doeapi-240695207Pas encore d'évaluation
- Culture PowerpointDocument9 pagesCulture Powerpointapi-240695207Pas encore d'évaluation
- Sop Sickle CellDocument2 pagesSop Sickle Cellapi-240695207Pas encore d'évaluation
- The Yellow House: A Memoir (2019 National Book Award Winner)D'EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Évaluation : 4 sur 5 étoiles4/5 (98)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceD'EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceÉvaluation : 4 sur 5 étoiles4/5 (895)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersD'EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersÉvaluation : 4.5 sur 5 étoiles4.5/5 (344)
- The Little Book of Hygge: Danish Secrets to Happy LivingD'EverandThe Little Book of Hygge: Danish Secrets to Happy LivingÉvaluation : 3.5 sur 5 étoiles3.5/5 (399)
- Grit: The Power of Passion and PerseveranceD'EverandGrit: The Power of Passion and PerseveranceÉvaluation : 4 sur 5 étoiles4/5 (588)
- The Emperor of All Maladies: A Biography of CancerD'EverandThe Emperor of All Maladies: A Biography of CancerÉvaluation : 4.5 sur 5 étoiles4.5/5 (271)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaD'EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaÉvaluation : 4.5 sur 5 étoiles4.5/5 (266)
- Never Split the Difference: Negotiating As If Your Life Depended On ItD'EverandNever Split the Difference: Negotiating As If Your Life Depended On ItÉvaluation : 4.5 sur 5 étoiles4.5/5 (838)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryD'EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryÉvaluation : 3.5 sur 5 étoiles3.5/5 (231)
- On Fire: The (Burning) Case for a Green New DealD'EverandOn Fire: The (Burning) Case for a Green New DealÉvaluation : 4 sur 5 étoiles4/5 (73)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureD'EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureÉvaluation : 4.5 sur 5 étoiles4.5/5 (474)
- Team of Rivals: The Political Genius of Abraham LincolnD'EverandTeam of Rivals: The Political Genius of Abraham LincolnÉvaluation : 4.5 sur 5 étoiles4.5/5 (234)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyD'EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyÉvaluation : 3.5 sur 5 étoiles3.5/5 (2259)
- The Unwinding: An Inner History of the New AmericaD'EverandThe Unwinding: An Inner History of the New AmericaÉvaluation : 4 sur 5 étoiles4/5 (45)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreD'EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreÉvaluation : 4 sur 5 étoiles4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)D'EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Évaluation : 4.5 sur 5 étoiles4.5/5 (120)
- Her Body and Other Parties: StoriesD'EverandHer Body and Other Parties: StoriesÉvaluation : 4 sur 5 étoiles4/5 (821)
- Herniated Nucleus Pulposus in Dr. Hasan Sadikin General Hospital Bandung IndonesiaDocument7 pagesHerniated Nucleus Pulposus in Dr. Hasan Sadikin General Hospital Bandung Indonesiawulan dwi yulistiaPas encore d'évaluation
- Albumin Guidelines UHS April 2010Document5 pagesAlbumin Guidelines UHS April 2010dradrianramdhanyPas encore d'évaluation
- White Paper IONMDocument77 pagesWhite Paper IONMJiebo LuPas encore d'évaluation
- Respiratory Diseases Chapter From Nelson Textbook of PediatricsDocument312 pagesRespiratory Diseases Chapter From Nelson Textbook of PediatricsMilan Andrejevic100% (1)
- Posterior Palatal SealDocument7 pagesPosterior Palatal SealÄpriolia SuPas encore d'évaluation
- MiofuncionalDocument9 pagesMiofuncionalKaterine TrillosPas encore d'évaluation
- 2016 S 0042 108641 PDFDocument29 pages2016 S 0042 108641 PDFMadalina StoicescuPas encore d'évaluation
- Tooth Discolour at Ion PedoDocument28 pagesTooth Discolour at Ion PedoFourthMolar.comPas encore d'évaluation
- Vata Constitution AyurvedaDocument11 pagesVata Constitution AyurvedaElla Miu100% (1)
- Imt 2Document6 pagesImt 2Imran KhanPas encore d'évaluation
- The Use of Bisphosphonates in Children. Review of The Literature and Guidelines For Dental ManagementDocument11 pagesThe Use of Bisphosphonates in Children. Review of The Literature and Guidelines For Dental ManagementHemil Dario Rosales MolinaPas encore d'évaluation
- Daftar TindakanDocument3 pagesDaftar TindakanSri DevianaPas encore d'évaluation
- Arellano University: Jose Abad Santos CampusDocument7 pagesArellano University: Jose Abad Santos CampusLloyd VargasPas encore d'évaluation
- CC NICU Rabu Malam 16 Jan 19Document41 pagesCC NICU Rabu Malam 16 Jan 19Primadiati Nickyta SariPas encore d'évaluation
- Crossroads Summer 08Document62 pagesCrossroads Summer 08jason.garber100% (4)
- Decompensated Liver Cirrhosis by DR - DoaaDocument24 pagesDecompensated Liver Cirrhosis by DR - DoaaAyu DewiPas encore d'évaluation
- Cerebral PalsyDocument11 pagesCerebral PalsyprasadPas encore d'évaluation
- MalpresentationDocument16 pagesMalpresentationwaw jonasPas encore d'évaluation
- Mnemonics ShortDocument139 pagesMnemonics ShortKelly HernandezPas encore d'évaluation
- Blood Culture CompetencyDocument6 pagesBlood Culture CompetencyWilson CarandangPas encore d'évaluation
- Table of Comparison For Performing CPR For Adult, Child, Infant, and Pregnant WomenDocument3 pagesTable of Comparison For Performing CPR For Adult, Child, Infant, and Pregnant WomenNichole Audrey SaavedraPas encore d'évaluation
- Campus Map Building List PDFDocument1 pageCampus Map Building List PDFRicky Quizzagan MaguigadPas encore d'évaluation
- 9781907816444Document12 pages9781907816444Dr.yeasin Arafat100% (1)
- Erb's PalsyDocument18 pagesErb's PalsyMegha PataniPas encore d'évaluation
- Dr. Chisholm Shoulder Dystocia 062607Document51 pagesDr. Chisholm Shoulder Dystocia 062607kusumarizky89Pas encore d'évaluation
- QMC Notes Teaching Package Aug08Document22 pagesQMC Notes Teaching Package Aug08madimadi11Pas encore d'évaluation
- African Adventure: by Margaret Iggulden Streamline Graded Readers Level 3 1000 HeadwordsDocument8 pagesAfrican Adventure: by Margaret Iggulden Streamline Graded Readers Level 3 1000 Headwordsjluis1980Pas encore d'évaluation
- Airway-RSI Pocket CardDocument4 pagesAirway-RSI Pocket CardbellerevoltePas encore d'évaluation
- Medical AttendanceDocument9 pagesMedical AttendanceamritPas encore d'évaluation
- The Complete Bed Wetting BookDocument97 pagesThe Complete Bed Wetting BookTimothy PangaPas encore d'évaluation