Académique Documents
Professionnel Documents
Culture Documents
Diuretics
Transféré par
ashphoenix32Copyright
Formats disponibles
Partager ce document
Partager ou intégrer le document
Avez-vous trouvé ce document utile ?
Ce contenu est-il inapproprié ?
Signaler ce documentDroits d'auteur :
Formats disponibles
Diuretics
Transféré par
ashphoenix32Droits d'auteur :
Formats disponibles
PHARMACOLOGY:
DIURETICS
October 14, 2013 Dr. Gracielle Mia C. Banares
Learning Objectives
Describe the renal tubule system Determine the mechanisms of the renal tubule system Determine the drug action sites of diuretics Determine the mechanisms of action of diuretics
Distal convoluted tubule (DCT) Cortical collecting tubule (CCT) Medullary collecting duct
Review of terms Reabsorption - aka tubular reabsorption Flow of glomerular filtrate from the proximal tubule of the nephron into the peritubular capillaries, or from the urine into the blood Second time that the nutrients are being absorbed into the blood, the first time being from the small intestine into the villi Sodium transport from the lumen into the blood by the Na+/K+ATPase in the basolateral membrane of the epithelial cells
Glomerulus Formation of glomerular filtrate Extremely high water permeability No primary transporters and drug targets at apical membrane No diuretic with major action Proximal convoluted tubule (PCT) Reabsorption of 65% of filtered Na+/ K+/ CA2+, and Mg2+; 85% of NaHCO3 , and nearly 100% of glucose and amino acids Isosmotic reabsorption of water located in the cortex of the kidney Almost all the glucose, bicarbonate, amino acids, and other metabolites are reabsorbed Approximately two-thirds of the Na+ is also reabsorbed Sodium bicarbonate (NaHCO3 ), sodium chloride (NaCl), glucose, amino acids, and other organic solutes are reabsorbed via specific transport systems in the early proximal tubule (proximal convoluted tubule, PCT) Potassium ions (K+) are reabsorbed via the paracellular pathway Water is reabsorbed passively, maintaining the osmolality of proximal tubular fluid at a nearly constant level Sodium bicarbonate reabsorption by the PCT is initiated by the action of a Na+/H+ exchanger (NHE3) located in the luminal membrane of the proximal tubule epithelial cell This transport system allows Na+ to enter the cell from the tubular lumen in exchange for a proton (H+) from inside the cell. As in all portions of the nephron, Na+/K+ ATPase in the basolateral membrane pumps the reabsorbed Na+ into the interstitium so as to maintain a low intracellular Na+ concentration The H+ secreted into the lumen combines with bicarbonate (HCO3) to form H2CO3 (carbonic acid), which is rapidly dehydrated to CO2 and H2O by carbonic anhydrase
Page 1 of 5
Nephron Basic structural and functional unit of the kidney Antidiuretic Hormone (ADH) aka Arginine Vasopressin (AVP) Two primary functions are to retain water in the body and to constrict blood vessels Vasopressin regulates the bodys retention of water by acting to increase water absorption in the collecting ducts of the kidney nephron
Major Segments of the Nephron and Their Functions Major Segments of the Nephron Glomerulus Proximal convoluted tubule (PCT) Proximal tubule, straight segments Thin descending limb of Henles loop Thick ascending limb of Henles loop (TAL)
Transcribed by: John Harley, Karlo, Joker
Carbon dioxide produced by dehydration of H2CO3 enters the proximal tubule cell by simple diffusion where it is then rehydrated back to H2CO3, facilitated by intracellular carbonic anhydrase After dissociation of H2CO3, the H+ is available for transport by the Na+/H+ exchanger, and the HCO3 is transported out of the cell by a basolateral membrane transporter Bicarbonate reabsorption by the proximal tubule is thus dependent on carbonic anhydrase
cationsincluding magnesium and calciumvia the paracellular pathway Inhibition of salt transport in the TAL by loop diuretics, which reduces the lumen-positive potential, causes an increase in urinary excretion of divalent cations in addition to NaCl
Loop of Henle At the boundary between the inner and outer stripes of the outer medulla, the proximal tubule empties into the thin descending limb of Henle's loop Water is extracted from the descending limb of this loop by osmotic forces found in the hypertonic medullary interstitium As in the proximal tubule, impermeant luminal solutes such as mannitol oppose this water extraction The thin ascending limb is relatively waterimpermeable. Thick ascending limb (TAL) of the loop of Henle Actively reabsorbs NaCl from the lumen (about 25% of the filtered sodium), but unlike the proximal tubule and the thin descending limb of Henle's loop, it is nearly impermeable to water Salt reabsorption in the TAL dilutes the tubular fluid, and it is called a diluting segment Medullary portions of the TAL contribute to medullary hypertonicity also play an important role in concentration of urine by the collecting duct Na+/K+/2Cl cotransporter (called NKCC2 or NK2CL) NaCl transport system in the luminal membrane of the TAL Selectively blocked by diuretic agents known as "loop" diuretics Electrically neutral (two cations and two anions are cotransported), the action of the transporter contributes to excess K+ accumulation within the cell Na+/K+/2Cl cotransporter (called NKCC2 or NK2CL) Back diffusion of this K+ into the tubular lumen causes a lumen-positive electrical potential that provides the driving force for reabsorption of
John Harley, Karlo, Joker
Distal Convoluted Tubule (DCT) About 10% of the filtered NaCl is reabsorbed in the distal convoluted tubule (DCT) Like the TAL of Henle's loop, this segment is relatively impermeable to water and NaCl reabsorption further dilutes the tubular fluid Na+ and Cl cotransporter (NCC) The mechanism of NaCl transport in the DCT electrically neutral thiazidesensitive Distal Convoluted Tubule (DCT) Because K+ does not recycle across the apical membrane of the DCT as it does in the TAL, there is no lumen-positive potential in this segment, and Ca2+ and Mg2+ are not driven out of the tubular lumen by electrical forces Instead, Ca2+ is actively reabsorbed by the DCT epithelial cell via an apical Ca2+ channel and basolateral Na+/Ca2+ exchanger this process is regulated by parathyroid hormone Cortical Collecting Tubule (CCT) Responsible for only 25% of NaCl reabsorption by the kidney Important role in renal physiology and in diuretic action As the final site of NaCl reabsorption, the collecting tubule is responsible for tight regulation of body fluid volume and for determining the final Na+ concentration of the urine A site at which mineralocorticoids exert a significant influence Most important site of K+ secretion by the kidney and the site at which virtually all diuretic-induced changes in K+ balance occur Principal cells are the major sites of Na+, K+, and water transport Intercalated cells are the primary sites of H+ secretion Unlike cells in other nephron segments, the principal cells do not contain cotransport
Page 2 of 5
systems for Na+ and other ions in their apical membranes Principal cell membranes exhibit separate ion channels for Na+ and K+ These channels exclude anions, transport of Na+ or K+ leads to a net movement of charge across the membrane Because Na+ entry into the principal cell predominates over K+ secretion, a 1050 mV lumen-negative electrical potential develops Na+ that enters the principal cell from the tubular fluid is then transported back to the blood via the basolateral Na+/K+ ATPase The 1050 mV lumen-negative electrical potential drives the transport of Cl back to the blood via the paracellular pathway and draws K+ out of cells through the apical membrane K+ channel Diuretics that act upstream of the CCT increase Na+ delivery and enhance K+ secretion If the Na+ is delivered with an anion that cannot be reabsorbed as readily as Cl (eg, HCO3), the lumen-negative potential is increased, and K+ secretion is enhanced This mechanism, combined with enhanced aldosterone secretion due to volume depletion, is the basis for most diuretic-induced K+ wasting Aldosterone Regulates reabsorption of Na+ via the epithelial Na channel (ENaC) and its coupled secretion of K+ This steroid hormone, through its actions on gene transcription, increases the activity of both apical membrane channels and the basolateral Na+/K+ ATPase This leads to an increase in the transepithelial electrical potential and a dramatic increase in both Na+ reabsorption and K+ secretion
The collecting tubule is also the site at which the final urine concentration is determined Antidiuretic hormone (ADH, also called vasopressin, AVP) Controls the permeability of this segment to water by regulating the insertion of preformed water channels (aquaporin-2, AQP2) into the apical membrane via a G protein-coupled, cAMP-mediated process In the absence of ADH, the collecting tubule (and duct) is impermeable to water, and dilute urine is produced ADH markedly increases water permeability, and this leads to the formation of a more concentrated final urine ADH also stimulates the insertion of urea transporter UT1 molecules into the apical membranes of medullary collecting tubule cells
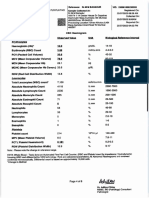
BASIC PHARMACOLOGY OF DIURETIC AGENTS Carbonic Anhydrase Inhibitors
Carbonic Anhydrase predominant location is the luminal membrane of the PCT, catalyzes the dehydration of H2CO3 By blocking carbonic anhydrase inhibitors block NaHCO3 reabsorption and cause diuresis Acetazolamide Prototypical carbonic anhydrase inhibitor
*** Ion transport pathways across the luminal and basolateral membranes of collecting tubule and collecting duct cells. Inward diffusion of Na+ via the epithelial sodium channel (ENaC) leaves a lumennegative potential, which drives reabsorption of Cl and efflux of K+. (R, aldosterone receptor.) *** Cortical Collecting Tubule (CCT)
Pharmacokinetics Well absorbed after oral administration An increase in urine pH from the HCO3 diuresis is apparent within 30 minutes, is maximal at 2 hours, and persists for 12 hours after a single dose Excretion of the drug is by secretion in the proximal tubule S2 segment Dosing must be reduced in renal insufficiency
Pharmacodynamics Inhibition of carbonic anhydrase activity profoundly depresses HCO3 reabsorption in the PCT
John Harley, Karlo, Joker
Page 3 of 5
Carbonic anhydrase inhibition causes significant HCO3 losses and hyperchloremic metabolic acidosis Diuretic efficacy of acetazolamide decreases significantly with use over several days
Clinical Indications GLAUCOMA Reduction of aqueous humor formation by carbonic anhydrase inhibitors decreases the intraocular pressure MOST common indication for use of carbonic anhydrase inhibitors Dorzolamide, Brinzolamide: topically active reduce intraocular pressure without producing detectable plasma levels diuretic and systemic metabolic effects are eliminated for the topical agents URINARY ALKALINIZATION Uric acid, cystine, and other weak acids are most easily reabsorbed from acidic urine renal excretion of cystine (in cystinuria) and other weak acids can be enhanced by increasing urinary pH with carbonic anhydrase inhibitors In the absence of continuous HCO3 administration, these effects of acetazolamide last only 23 days Prolonged therapy requires HCO3 administration METABOLIC ALKALOSIS Generally treated by correction of abnormalities in total body K+, intravascular volume, or mineralocorticoid levels However, when the alkalosis is due to excessive use of diuretics in patients with severe heart failure, replacement of intravascular volume may be contraindicated In these cases, acetazolamide can be useful in correcting the alkalosis as well as producing a small additional diuresis for correction of volume overload Can also be used to rapidly correct the metabolic alkalosis that may develop in the setting of respiratory acidosis ACUTE MOUNTAIN SICKNESS Weakness, dizziness, insomnia, headache, and nausea can occur in
John Harley, Karlo, Joker
mountain travelers who rapidly ascend above 3000 m In more serious cases, rapidly progressing pulmonary or cerebral edema can be life-threatening By decreasing cerebrospinal fluid formation and by decreasing the pH of the cerebrospinal fluid and brain, acetazolamide can increase ventilation and diminish symptoms of mountain sickness Used as adjuvants in the treatment of epilepsy and in some forms of hypokalemic periodic paralysis and to increase urinary phosphate excretion during severe hyperphosphatemia
Toxicity HYPERCHLOREMIC METABOLIC ACIDOSIS Acidosis predictably results from chronic reduction of body HCO3 stores by carbonic anhydrase inhibitors and limits the diuretic efficacy of these drugs to 2 or 3 days Unlike the diuretic effect, acidosis persists as long as the drug is continued RENAL STONES Phosphaturia and Hypercalciuria occur during the bicarbonaturic response to inhibitors of carbonic anhydrase Renal excretion of solubilizing factors (eg, citrate) may also decline with chronic use Calcium salts are relatively insoluble at alkaline pH, which means that the potential for renal stone formation from these salts is enhanced RENAL POTASSIUM WASTING Can occur because the increased Na+ presented to the collecting tubule (with HCO3) is partially reabsorbed, increasing the lumen-negative electrical potential in that segment and enhancing K+ secretion This effect can be counteracted by simultaneous administration of potassium chloride K+ wasting is theoretically a problem with any proximal tubule diuretic that presents increased Na+ to the collecting tubule
Page 4 of 5
Drowsiness and Paresthesias are common following large doses of acetazolamide Carbonic anhydrase inhibitors may accumulate in patients with renal failure, leading to nervous system toxicity Hypersensitivity reactions (fever, rashes, bone marrow suppression, and interstitial nephritis) may also occur
Contraindications Hyperammonemia and Hepatic encephalopathy in patients with cirrhosis Carbonic anhydrase inhibitorinduced alkalinization of the urine decreases urinary excretion of NH4+ (by converting it to rapidly reabsorbed NH3)
Loop Diuretics
Selectively inhibit NaCl reabsorption in the TAL Because of the large NaCl absorptive capacity of this segment and the fact that the diuretic action of these drugs is not limited by development of acidosis, as is the case with the carbonic anhydrase inhibitors Most efficacious diuretic agents currently available Furosemide, Ethacrynic acid Prototype drugs Ethacrynic acidnot a sulfonamide derivativeis a phenoxyacetic acid derivative containing a ketone and methylene group Bumetanide, Torsemide sulfonamide loop diuretics
Pharmacokinetics Rapidly absorbed Eliminated by the kidney by glomerular filtration and tubular secretion Effect for furosemide is usually 23 hours and that of torsemide is 46 hours Half-life depends on renal function
John Harley, Karlo, Joker
Page 5 of 5
Vous aimerez peut-être aussi
- Environmental SanitationDocument9 pagesEnvironmental Sanitationashphoenix32Pas encore d'évaluation
- DeciduaDocument14 pagesDeciduaashphoenix32Pas encore d'évaluation
- Microbiology TableDocument29 pagesMicrobiology TableRoot GiralaoPas encore d'évaluation
- Medications Used To Treat Clotting Disorders: Antiplatelet AgentsDocument9 pagesMedications Used To Treat Clotting Disorders: Antiplatelet Agentsashphoenix32Pas encore d'évaluation
- Parasitology Question ReviewerDocument1 pageParasitology Question Reviewerashphoenix32100% (2)
- Uterus DidelphysDocument3 pagesUterus Didelphysashphoenix32Pas encore d'évaluation
- 2011 06 MICRO Intro To VirologyDocument8 pages2011 06 MICRO Intro To VirologydtimtimanPas encore d'évaluation
- Healthcare DeliveryDocument2 pagesHealthcare Deliveryashphoenix32Pas encore d'évaluation
- Medical MnemonicsDocument158 pagesMedical MnemonicsBeryl de la CruzPas encore d'évaluation
- A Water HandbookDocument116 pagesA Water HandbookGreater Charlotte Harbor Sierra ClubPas encore d'évaluation
- A Water HandbookDocument116 pagesA Water HandbookGreater Charlotte Harbor Sierra ClubPas encore d'évaluation
- Prayer Before The ExamDocument3 pagesPrayer Before The Examashphoenix32Pas encore d'évaluation
- Prayer Before The ExamDocument3 pagesPrayer Before The Examashphoenix32Pas encore d'évaluation
- History of Medicine TimelineDocument6 pagesHistory of Medicine Timelineashphoenix32Pas encore d'évaluation
- North Central Texas Trauma Regional Advisory CouncilDocument9 pagesNorth Central Texas Trauma Regional Advisory Councilashphoenix32Pas encore d'évaluation
- NCLEXReview Set 4 FA09Document5 pagesNCLEXReview Set 4 FA09ashphoenix32Pas encore d'évaluation
- Plasma Concentration of C-Reactive Protein and Risk of Developing Peripheral Vascular DiseaseDocument8 pagesPlasma Concentration of C-Reactive Protein and Risk of Developing Peripheral Vascular Diseaseashphoenix32Pas encore d'évaluation
- Muscle Origins and InsertionsDocument9 pagesMuscle Origins and Insertionsnoisytaost92% (12)
- Ethics Sept 7Document1 pageEthics Sept 7ashphoenix32Pas encore d'évaluation
- The Yellow House: A Memoir (2019 National Book Award Winner)D'EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Évaluation : 4 sur 5 étoiles4/5 (98)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceD'EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceÉvaluation : 4 sur 5 étoiles4/5 (895)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeD'EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeÉvaluation : 4 sur 5 étoiles4/5 (5794)
- The Little Book of Hygge: Danish Secrets to Happy LivingD'EverandThe Little Book of Hygge: Danish Secrets to Happy LivingÉvaluation : 3.5 sur 5 étoiles3.5/5 (399)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaD'EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaÉvaluation : 4.5 sur 5 étoiles4.5/5 (266)
- Shoe Dog: A Memoir by the Creator of NikeD'EverandShoe Dog: A Memoir by the Creator of NikeÉvaluation : 4.5 sur 5 étoiles4.5/5 (537)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureD'EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureÉvaluation : 4.5 sur 5 étoiles4.5/5 (474)
- Never Split the Difference: Negotiating As If Your Life Depended On ItD'EverandNever Split the Difference: Negotiating As If Your Life Depended On ItÉvaluation : 4.5 sur 5 étoiles4.5/5 (838)
- Grit: The Power of Passion and PerseveranceD'EverandGrit: The Power of Passion and PerseveranceÉvaluation : 4 sur 5 étoiles4/5 (588)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryD'EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryÉvaluation : 3.5 sur 5 étoiles3.5/5 (231)
- The Emperor of All Maladies: A Biography of CancerD'EverandThe Emperor of All Maladies: A Biography of CancerÉvaluation : 4.5 sur 5 étoiles4.5/5 (271)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyD'EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyÉvaluation : 3.5 sur 5 étoiles3.5/5 (2259)
- On Fire: The (Burning) Case for a Green New DealD'EverandOn Fire: The (Burning) Case for a Green New DealÉvaluation : 4 sur 5 étoiles4/5 (73)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersD'EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersÉvaluation : 4.5 sur 5 étoiles4.5/5 (344)
- Team of Rivals: The Political Genius of Abraham LincolnD'EverandTeam of Rivals: The Political Genius of Abraham LincolnÉvaluation : 4.5 sur 5 étoiles4.5/5 (234)
- The Unwinding: An Inner History of the New AmericaD'EverandThe Unwinding: An Inner History of the New AmericaÉvaluation : 4 sur 5 étoiles4/5 (45)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreD'EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreÉvaluation : 4 sur 5 étoiles4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)D'EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Évaluation : 4.5 sur 5 étoiles4.5/5 (121)
- Her Body and Other Parties: StoriesD'EverandHer Body and Other Parties: StoriesÉvaluation : 4 sur 5 étoiles4/5 (821)
- Preterm Prelabour Rupture of MembranesDocument12 pagesPreterm Prelabour Rupture of MembranesSeptiany Indahsari DjanPas encore d'évaluation
- Perio QuestionsDocument32 pagesPerio QuestionsSoha Jan KhuhawarPas encore d'évaluation
- Lecture 1. Advanced Biochemistry. Introduction.Document70 pagesLecture 1. Advanced Biochemistry. Introduction.Cik Syin100% (1)
- A Color Atlas of Poultry Diseases by J.L VegadDocument131 pagesA Color Atlas of Poultry Diseases by J.L VegadAbubakar Tahir Ramay95% (63)
- AUB - Microscopic Analysis of UrineDocument4 pagesAUB - Microscopic Analysis of UrineJeanne Rodiño100% (1)
- BTS Sarcoidosis Clinical StatementDocument17 pagesBTS Sarcoidosis Clinical StatementDarrin WiebePas encore d'évaluation
- Full Text of RA 7719Document4 pagesFull Text of RA 7719camz_hernandezPas encore d'évaluation
- Formulation and Evaluation of Herbal Lip Rouge.: Research ArticleDocument5 pagesFormulation and Evaluation of Herbal Lip Rouge.: Research ArticleTynPas encore d'évaluation
- Beauty Care 1st Summative TestDocument4 pagesBeauty Care 1st Summative TestLlemor Soled SeyerPas encore d'évaluation
- China Animal Healthcare: The Healing TouchDocument19 pagesChina Animal Healthcare: The Healing TouchBin WeiPas encore d'évaluation
- Adult Early Warning Score Observation Chart For Cardiothoracic UnitDocument1 pageAdult Early Warning Score Observation Chart For Cardiothoracic UnitalexipsPas encore d'évaluation
- Adobe Scan Jul 28, 2023Document6 pagesAdobe Scan Jul 28, 2023Krishna ChaurasiyaPas encore d'évaluation
- Tes TLMDocument16 pagesTes TLMAmelia RosyidaPas encore d'évaluation
- Quantifying The Health Economic Value AsDocument1 pageQuantifying The Health Economic Value AsMatiasPas encore d'évaluation
- Slcog Abstracts 2012Document133 pagesSlcog Abstracts 2012Indika WithanagePas encore d'évaluation
- Aac-Augmentative and Alternative CommunicationDocument35 pagesAac-Augmentative and Alternative Communicationrenuka aurangabadkerPas encore d'évaluation
- DR Ololade 038Document13 pagesDR Ololade 038Andrawus DanjumaPas encore d'évaluation
- Jurnal Bahasa InggrisDocument9 pagesJurnal Bahasa InggrisNur Riza Maulidina100% (1)
- DSM OcdDocument2 pagesDSM Ocdnmyza89Pas encore d'évaluation
- Punjab Municipal Corporation Act, 1976 PDFDocument180 pagesPunjab Municipal Corporation Act, 1976 PDFSci UpscPas encore d'évaluation
- Aynı MakaleDocument95 pagesAynı MakalesalihcikkPas encore d'évaluation
- How Swab Testing of Kitchen SurfacesDocument3 pagesHow Swab Testing of Kitchen SurfacesSIGMA TESTPas encore d'évaluation
- Criminal SociologyDocument53 pagesCriminal SociologyJackielyn cabayaoPas encore d'évaluation
- Infective Endocarditis (IE)Document76 pagesInfective Endocarditis (IE)Mahesh RathnayakePas encore d'évaluation
- Cell Types Animal Tissue ReviewerDocument6 pagesCell Types Animal Tissue ReviewerShane LaluPas encore d'évaluation
- StyeDocument21 pagesStyenur syafiqah kamaruzamanPas encore d'évaluation
- The Human Magnet Syndrome Why We Love PeDocument8 pagesThe Human Magnet Syndrome Why We Love Peapi-316440587Pas encore d'évaluation
- Postpartum Headache: Diagnostic Considerations: Sue Yin Lim, Nikos Evangelou, Sibylle JürgensDocument8 pagesPostpartum Headache: Diagnostic Considerations: Sue Yin Lim, Nikos Evangelou, Sibylle JürgensJamie LittlePas encore d'évaluation
- Eaves Nickolas A 201211 MASc ThesisDocument69 pagesEaves Nickolas A 201211 MASc Thesisrajeev50588Pas encore d'évaluation
- An Mrna Vaccine Against Sars-Cov-2 - Preliminary Report: Original ArticleDocument12 pagesAn Mrna Vaccine Against Sars-Cov-2 - Preliminary Report: Original ArticleSalvador Francisco Tello OrtízPas encore d'évaluation