Académique Documents
Professionnel Documents
Culture Documents
Genomic and Precision Medicine
Transféré par
allblubber2223Copyright
Formats disponibles
Partager ce document
Partager ou intégrer le document
Avez-vous trouvé ce document utile ?
Ce contenu est-il inapproprié ?
Signaler ce documentDroits d'auteur :
Formats disponibles
Genomic and Precision Medicine
Transféré par
allblubber2223Droits d'auteur :
Formats disponibles
Genomic and Precision Medicine
The human genome has 3.2 billion bp of DNA, since we have 2 copies (one from each parent)
we have 6.4 billion bp. The function of most of the DNA in the human genome is unknown.
- We have SINEs and LINEs, make up about 30% of the genome, thought to be involved
in packaging, segregation and replication of chromosomes.
- 5% of the genome is conserved across multiple species, suggesting its vitally important
to survival somehow.
- 1.5% of the genome is for protein-coding genes.
- Its thought 80% of the genome is functional, but we dont know the function yet.
Genes are the blueprint for the production of proteins (enzymes, structural elements, signaling
molecules.
Gene structure includes: introns, exons (coding) and regulatory regions.
Average gene size is 20 kb, but highly variable
An estimated 22,000 genes somewhere in the genome.
Genes are important for protein synthesis. DNA molecule is transcribed into mRNA, splicing
out the introns to make mRNA that has only exons. Then the mRNA message is read and
translated into an amino acid sequence (protein).
We used to think 1 gene= 1 protein, but alternative splicing has disproven that. Alternative
splicing makes the gene have an alternative transcriptional start site, thereby changing the
protein, or by skipping certain exons. It is quite common, occurs in 90+ % of genes in the
human genome.
All cells have the exact same DNA and the exact same genes. Cells with identical DNA can
look and behave differently because of differences in gene expression, i.e. which genes are
turned on in which cells.
Expression of genes in wrong cell at wrong time or in wrong amount can lead to disease.
Gene expression is regulated in a number of ways:
1. Protein regulatory molecules that bind to the gene and either turn the gene on or off
2. RNA regulatory molecules that bind to the gene and either turn the gene on or off
3. Epigenetic mechanisms: methyl groups and other things that bind to the regulatory region
and silence the gene
Structural variants are changes in the DNA
- Aneuploidies: addition or deletion of chromosomes (numerical variants). Due to
nondisjunction, usually cause spontaneous abortion unless trisomy 21, 13 or 18 or
klinefelter or turner syndromes.
- Translocations: rearranged DNA, usually harmless, unless breakpoint is in a gene.
- CNVs: copy number variants: deletions or duplications, typically 1-10 kb, but can be
several Mb in size, single or multiple copies in tandem. Can involve genes (about 2/3
overlap with genes). Large CNVs can affect multiple genes. The large ones tend to be
less polymorphic (usually only one duplication or deletion). They are less common in the
population but are more likely to be pathogenic since they affect more genes. They are
more likely de novo and cause disease by causing too little or too much gene product or
by unmasking a deleterious recessive trait, one gene is deleted2 hit theory.
- SNVs, single nucleotide variants, common in the general population, average person has
about 4 million DNA sequence variants, most of which are SNVs, can use SNVs to trace
human migration. Depending on the location, they can have big effects, or be invisible.
Ex: if they are at regulatory region, can affect gene expression; if at a splice site, can
disrupt splicing; if in a coding region can affect amino acid composition.
- Insretions/deletions of one or more nucleotides in coding region of a gene can result in a
shift in the reading frame that can dramatically alter the sequence of amino acids in the
protein.
Random mutations arise naturally during cell division
Mutations in gametes (germline) have the potential to be transmitted to offspring, but somatic
mutations do not
Human mutation rate is about 10
-8
per bp per generation, 50-100 new mutations in average
newborn.
Polymorphism: mutation with allele frequency >1% in the general population
Alleles inherited in a haplotype are said to be in linkage disequilibrium (LD), correlation
between SNPs. LD is stronger when distance between variants is short. LD is shaped by
recombination. LD allows prediction of alleles. For two variants in strong LD, alleles at one
location provide information about alleles at another location.
Haplotypes: combinations of alleles at different location and their correlation with each other.
We see that haplotype blocks are punctuated by regions of recombination. Strong correlation
within a haplotype block, but not between blocks.
Haplotype blocks are regions within which there is strong LD, or correlation between variants.
One variant can capture information about another variant, either known or unknown. This has
big implications for GWAS
Mendelian disorders are present in about 2-3% of all newborns, although disease may not show
up for years, if ever.
Typical Mendelian disorder inheritance patterns:
- Autosomal dominant: an affected individual will have a 50-50 chance of passing on an
affected gene to each child. Children only need one dominant gene to show the trait
- Autosomal recessive: an affected individual will have a 50-50 chance of passing on an
affected gene to each child. Children need to have two copies of the recessive gene to
show the trait
- X-linked: defected copy of the gene is carried on the X chromosome
Complications to Mendelian inheritance patterns:
- New mutation
- Mosaicisim (not every cell has the same DNA)
- Reduced penetrance: disease genotype without phenotype
- Disease in carriers of recessive disorders-not always silent, higher risk for other
diseases
Recognizing a Mendelian disorder:
- Recurs in the family
- Multiple close relatives are affected
- Tends to be earlier onset than non-Mendelian forms of the same disease
- If a cancer syndrome, may affect bilateral structures
- Consanguinity
Why do genetic testing?
- Make a diagnosis and infer prognosis
- Provide an explanation and end a diagnostic odyssey
- Guide management
- Identify which other family members are or are not at risk for the disease
- Inform reproductive decision making including pre-implantation or prenatal diagnosis
Traditional sequencing amplifies the exons by primers, then sequences and looks for
abnormalities. This does not find deletions/duplications.
Cytogenomic array has a chip, each spot contains copies of a short strand of single-stranded
DNA that is specific to a unique location in the genome. Put control and patient DNA in, each
tagged with a different color so if they are the same, youll see yellow (green for patient plus red
for control), if loss or deletion, youll only see the red from the control, if there is a gain or
duplication youll only see the green from the patient.
Why newborn screening?
Many disorders are not obvious or readily diagnosable in a newborn, leading to delay in
instituting effective interventions that can prevent or ameliorate irreparable harm.
Criteria for newborn screening:
1. An important health problem whose natural history is understood
2. Facilities for diagnosis and treatment are available
3. Suitable and acceptable test and treatment
4. A latent or early symptomatic stage exists during which intervention improves outcomes
5. The cost of case-finding (including diagnosis and treatment) is economically balanced in
relation to possible expenditure on medical care as a whole
Newborn screening varies by state. There is a uniform panel of 31 core disorders and 26
secondary disorders, all states screen for 30+ disorders
Prenatal genetic screening:
- For Down syndrome and other neural tube defects
- Other birth defects and abnormalities
Screening tests: maternal age, biochemical screening (maternal blood/serum), cell free DNA
testing, ultrasound
Diagnostic tests: amniocentesis, CVS (Chorionic villus sampling), preimplantation genetic
diagnosis, ultrasound
Nuchal translucency: fluid behind the fetal neck in the late first trimester (11-14 weeks), birth
defects tend to have more fluid.
Reasons for prenatal testing
Increased risk of aneuploidy:
- Maternal age
- Abnormal serum screening
- Abnormal cell free DNA results
- Ultrasound abnormalities
- Parent carries chromosomal translocation
Elevated MSAFP
- Increased risk for open fetal defects
Increased risk of genetic disease
- Family history
- Carrier of genetic disorder by screening
Maternal request
Amniocentesis:
Sample of amniotic fluid (20cc) removed by insertion of needle through maternal abdomen into
uterus. Miscarriage risk was the standard quoted loss rate historically was 1/200, but not based
on reliable data, more recent studies show 1/350 or 1/769
Chorionic villus sampling: performed between 10-13 weeks. Villi removed from developing
placenta (transvervical or transbdominal) indications same as for amniocentesis, except that AFP
testing of amniotic fluid cant be performed, primary advantage is that it is earlier in the
pregnancy. Risk often quoted 0.5-1%, but recently shown to be similar to 1/350 like amnio
Cell free fetal DNA: in 1997 shown there was fetal DNA in serum of pregnant women. Big
advance allowing cfDNA testing has been development of next generation sequencing. cfDNA
comes from apoptosis, mostly of the placenta. Makes up about 10% of total DNA in maternal
plasma, much higher percentage than intact fetal cells. cffDNA made up of short DNA
fragments, reliabley detected after 7 weeks, very short half-life. False negatives and not enough
sample failed results. Placental or maternal mosaicism, contamination can also skew results.
Chromosomal microarray (CMA) for prenatal diagnosis. Molecular karyotype.
Carrier screening:
Heterozygote screening, usually for autosomal recessive disorders. Carriers are usually
asymptomatic, usually no family history, equally common in both genders, if both parents are
carrier, chance with each pregnancy the child will be affected.
Tay sachs disease: lysosomal storage disease caused by hexosaminidase A deficiency, resultant
accumulation of GM2 gangliosides results in progressive neurodegeneration, death in early
childhood. Screening for tay sachs was one of the first public health programs, very successful.
Cystic fibrosis: most common autosomal recessive disorder among caucasions (1/3300), 1 in 25
caucasionas with no family history are carriers. Caused by a mutation in the CFTR gene which
directs chloride transport, tenacious mucus in lungs and pancreas. Average life span is 37.
Nearly 2000 gene mutations identified, standard recommendation is a 23 mutation panel which is
pretty accurate for ashkenazis, Caucasians and Hispanics, lower for African and Asian
americans.
Fragile X syndrome: most common inherited form of mental retardation, most common single
gene defect associated with autism affects about 1/4000 males, 1/8000 women. Associated with
many other clinical features. Population screening is not currently recommended because the
genetic counseling is complicated. Carriers have a permutation that can expand to a full
mutation. Full mutation in males and some females causes fragile x syndrome. Outcome in
females is unpredictable from typical fragile x to asymptomatic.
Multiplex panel screening/universal screening. Multiplex screening allows for >100 tests at
once, costs about $99. Pros: cost effect, efficient, allows universal screening without regard to
ethnicity. Cons: 35% of people have unexpected findings so their partners/family also have to be
tested, makes it more expensive, disorders rare, or complicated to explain.
Whole genome analysis: a genome-wide search for disease-causing variants
- Karyotype: chromosomes under the microscope
- Cytogenomic arrays for large deletions/duplications
- Whole exome sequencing (WES)
- Whole genome sequencing (WGS)
Sequencing: begin with a collection of DNA, broken into fragments and sequenced. Align all
the sequences and get a de novo alignment, can align the sequence to a referene sequence
There is no single human genome. There is no normal genome, there are billions of
different genomes. To provide some sort of standard a reference genome was constructed as a
consensus among multiple sequences. Any persons genome differs from the reference at
millions of sites, ranging from single nucleotide differences up to hundreds of thousands, even
millions of base pairs. Reference still has gaps in regions where no sequence could be obtained.
Exome ccapture for WES: take DNA, make fragments recognizing about 2% of fragments are
from exons. Make short, synthetic DNA molecules that are complementary to all exons in the
genome, tag them with magnetic beads, they bind to the exons, take a magnet and you can pull
out all the exons and align or compare to a reference sequence.
Why study just the exome?
- More predictable effect of mutations
- More than 85% of known mutations for rare Mendelian disorders occur in the exome.
- Cheaper, faster and easier to analyze just 2% than the entire genome
WES can reliable detect: small variants (SNVs or small indels), some CNVs, NOT larger indels
or trinucleotide repeats, exon deletions are hit-or-miss depending on depth of coverage measures.
But, the technology is changing really quickly, so it will change soon.
Typical individual differences from reference: 5-10 million SNVs (varies by population), 2-5
hundred thousand indels, hundreds-thousands CNVs
What you want to know about variants:
- Gene name (if in a gene)
- Chromosome location of the change (position in reference genome)
- Location of the change within the mRNA/cDNA
- Location of the amino acid change in the protein
- Effect on protein (if in a gene)
- Variant dependent methods
o Allele frequency
o Predicted effect of variant on protein
o Evolutionary conservation, protein structure, amino acid properties
o Functional characterization of variant (in vitro and/or in vivo
- Disease dependent methods
o Mode of inheritance
o Cosegregation with disease in families
o Prior association of the gene with disease
o Pathway analysis
For a suspected Mendelian disease, a variant observed in the general, healthy population is
assumed non-pathogenic
Predicting the effect of a variant is CHALLENGING
- Probably damaging :stop-loss, stop-gained, frameshift, splice disruptor
- Possibly damaging: non-synonymous amino acid change, in-frame indel
- Likely not damaging: 5`/3` UTR, synonymous, intergenic, intronic, non-coding genes
Is the variant conserved in evolution? What effect does it have on protein structure? What are
the amino acid properties? These criteria are applied together by various computer algorithms to
assess how damaging a change might be
Mutations in conserved positions are more likely deleterious
Not all amino acid changes are equivalent. Conservative changes less likely to affect protein
structure/function. Location of change within protein matters as well.
Variant dependent methods vary in their ability to predict the effect of a variant on gene or
protein function. Some are highly predictive, others are, at best, suggestive or circumstantial.
Typical classification scheme:
- Known pathogenic
- Likely pathogenic
- Variant of unknown significance (VOUS or VUS)
- Likely benign
- benign
NGS: next generation sequencing
Mode of inheritance:
- dominant: one copy of the gene is affected and the person has the phenotype
- recessive: both copies of the gene are affected and the person has the phenotype
- new mutation: new variant in the patient not present in either parent
Vous aimerez peut-être aussi
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeD'EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeÉvaluation : 4 sur 5 étoiles4/5 (5794)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreD'EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreÉvaluation : 4 sur 5 étoiles4/5 (1090)
- Never Split the Difference: Negotiating As If Your Life Depended On ItD'EverandNever Split the Difference: Negotiating As If Your Life Depended On ItÉvaluation : 4.5 sur 5 étoiles4.5/5 (838)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceD'EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceÉvaluation : 4 sur 5 étoiles4/5 (895)
- Grit: The Power of Passion and PerseveranceD'EverandGrit: The Power of Passion and PerseveranceÉvaluation : 4 sur 5 étoiles4/5 (588)
- Shoe Dog: A Memoir by the Creator of NikeD'EverandShoe Dog: A Memoir by the Creator of NikeÉvaluation : 4.5 sur 5 étoiles4.5/5 (537)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersD'EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersÉvaluation : 4.5 sur 5 étoiles4.5/5 (345)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureD'EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureÉvaluation : 4.5 sur 5 étoiles4.5/5 (474)
- Her Body and Other Parties: StoriesD'EverandHer Body and Other Parties: StoriesÉvaluation : 4 sur 5 étoiles4/5 (821)
- The Emperor of All Maladies: A Biography of CancerD'EverandThe Emperor of All Maladies: A Biography of CancerÉvaluation : 4.5 sur 5 étoiles4.5/5 (271)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)D'EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Évaluation : 4.5 sur 5 étoiles4.5/5 (121)
- The Little Book of Hygge: Danish Secrets to Happy LivingD'EverandThe Little Book of Hygge: Danish Secrets to Happy LivingÉvaluation : 3.5 sur 5 étoiles3.5/5 (400)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyD'EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyÉvaluation : 3.5 sur 5 étoiles3.5/5 (2259)
- The Yellow House: A Memoir (2019 National Book Award Winner)D'EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Évaluation : 4 sur 5 étoiles4/5 (98)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaD'EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaÉvaluation : 4.5 sur 5 étoiles4.5/5 (266)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryD'EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryÉvaluation : 3.5 sur 5 étoiles3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnD'EverandTeam of Rivals: The Political Genius of Abraham LincolnÉvaluation : 4.5 sur 5 étoiles4.5/5 (234)
- On Fire: The (Burning) Case for a Green New DealD'EverandOn Fire: The (Burning) Case for a Green New DealÉvaluation : 4 sur 5 étoiles4/5 (74)
- The Unwinding: An Inner History of the New AmericaD'EverandThe Unwinding: An Inner History of the New AmericaÉvaluation : 4 sur 5 étoiles4/5 (45)
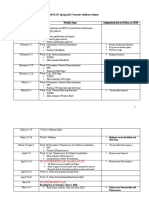
- Cytogenetics Course Syllabus SY 2020Document5 pagesCytogenetics Course Syllabus SY 2020J Pao Bayro Lacanilao100% (1)
- Clinical Molecular Diagnostic Techniques: A Brief ReviewDocument19 pagesClinical Molecular Diagnostic Techniques: A Brief ReviewSorin LazarPas encore d'évaluation
- Learning Unit 2 Prokaryotic Genome SystemDocument22 pagesLearning Unit 2 Prokaryotic Genome SystemgengkapakPas encore d'évaluation
- RT-PCR ProtocolDocument3 pagesRT-PCR ProtocolSusheePas encore d'évaluation
- Group 2 - Europe (Barcelona)Document22 pagesGroup 2 - Europe (Barcelona)mapuanxxivPas encore d'évaluation
- Biology Investigatory ProjectDocument21 pagesBiology Investigatory ProjectSubhiksha100% (1)
- Genetics, Lecture 11 (Lecture Notes)Document16 pagesGenetics, Lecture 11 (Lecture Notes)Ali Al-QudsiPas encore d'évaluation
- Chapter 4 ProteinDocument11 pagesChapter 4 ProteinAmbreen GhafoorPas encore d'évaluation
- Hypersensitive Response in PlantsDocument18 pagesHypersensitive Response in PlantsMehak MattooPas encore d'évaluation
- Golgi Apparatus - WikipediaDocument17 pagesGolgi Apparatus - WikipediaPrakashananda ThakurPas encore d'évaluation
- Gene Therapy - A Review ArticleDocument7 pagesGene Therapy - A Review ArticleKLPas encore d'évaluation
- Certificate For COVID-19 Vaccination: Beneficiary DetailsDocument1 pageCertificate For COVID-19 Vaccination: Beneficiary DetailsANIL100% (1)
- DNA Replication and Protein SynthesisDocument34 pagesDNA Replication and Protein SynthesisJessa Mae Infante PadillaPas encore d'évaluation
- General BiologyDocument82 pagesGeneral BiologyNanashiPas encore d'évaluation
- 301-4868, Rev. D Xpert Test Quality Control FlyerDocument2 pages301-4868, Rev. D Xpert Test Quality Control FlyerDiskosNinjicPas encore d'évaluation
- The Different Between Animal DNA and Planets DNADocument4 pagesThe Different Between Animal DNA and Planets DNAzezoo egPas encore d'évaluation
- TranscriptionDocument72 pagesTranscriptionMurthy MandalikaPas encore d'évaluation
- 26 Biology 2-16-08 Cellular RespirationDocument48 pages26 Biology 2-16-08 Cellular Respirationpotato macchiatoPas encore d'évaluation
- AP Q Chapter 3Document68 pagesAP Q Chapter 3Mahra AlketbiPas encore d'évaluation
- MCB 253 Spring 2021 SyllabusDocument2 pagesMCB 253 Spring 2021 Syllabuswakka987Pas encore d'évaluation
- Aiats Schedule For Class Xii (CF + Oym) 2023-24Document2 pagesAiats Schedule For Class Xii (CF + Oym) 2023-24Rita NayakPas encore d'évaluation
- North Carolina Biology EOC Study GuideDocument38 pagesNorth Carolina Biology EOC Study GuideRaquel Galdamez-GaldamezPas encore d'évaluation
- DR Lal Pathlabs: LPL - Lpl-Rohini (National Reference Lab) Sector - 18, Block - E Rohini Delhi 110085Document2 pagesDR Lal Pathlabs: LPL - Lpl-Rohini (National Reference Lab) Sector - 18, Block - E Rohini Delhi 110085Nehul PatilPas encore d'évaluation
- Bio CH4 F4 StudywithadminDocument16 pagesBio CH4 F4 StudywithadminRathi MalarPas encore d'évaluation
- AS Bio MS Answers PDFDocument34 pagesAS Bio MS Answers PDFGame ZonePas encore d'évaluation
- History of Genetic Transformation Chapter 2020Document32 pagesHistory of Genetic Transformation Chapter 2020Anuj PahalPas encore d'évaluation
- Nucleic Acids: AP BiologyDocument29 pagesNucleic Acids: AP BiologyRenante DavisPas encore d'évaluation
- Chromosomes and DnaDocument5 pagesChromosomes and DnaS. AnsariPas encore d'évaluation
- Worksheet - Dna Protein SynthesisDocument2 pagesWorksheet - Dna Protein Synthesisapi-270403367100% (1)
- Life 11 00257Document15 pagesLife 11 00257AzzahraPas encore d'évaluation