Académique Documents
Professionnel Documents
Culture Documents
Tugas Yuk Ya
Transféré par
Dian Cahaya UtamiDescription originale:
Copyright
Formats disponibles
Partager ce document
Partager ou intégrer le document
Avez-vous trouvé ce document utile ?
Ce contenu est-il inapproprié ?
Signaler ce documentDroits d'auteur :
Formats disponibles
Tugas Yuk Ya
Transféré par
Dian Cahaya UtamiDroits d'auteur :
Formats disponibles
Specific vasopressor agents
An evidence-based consensus of vasopressor and inotropic support in septic shock was published in
2008 by a subcommitte of the Surviving Sepsis Campaign [5]. In this context, we examine additional
recent evidence regarding use of vasoactive agents that has been published in the last year.
Vasopressin
Vasopressin is an endogenously released stress hormone that is important during shock. The
rationale for its use in the ICU is that there is a vasopressin deficiency in vasodilatory shock and that
exogenously administered vasopressin can restore vascular tone [2].
What is the role of vasopressin in septic shock?
The Vasopressin and Septic Shock Trial (VASST) was a multicenter,randomized,blinded trial of
vasopressin vs. Norepinephrine [6]. Patients having septic shock were allocated to either low-dose
vasopressin (0.01-0.03 u/min) or norepinephrine infusion (5-15 ug/min) in addition to open-label
vasopressors. All vasopressors were titrated and weaned according to protocols to maintain a target
blood pressure. Patients were analyzed according to the a priori strata of more severe and less
severe septic shock, based on the level of vasopressor use at baseline. A total of 779 patients were
randomized and infused with the study drug (vasopressin n=397, norepinephrine n=382). The study
was prospectively powered to detect an absolute difference in 28-day mortality of 10% from an
expected 60%. The observed mortality rates were considerably lower than predicted in the
vasopressin and norepinephrine groups, compared with previous reports perhaps because of overall
improvements in the care of patients who have septic shock.
The was no difference in the primary outcome, 28-day mortality, between vasopressin (35.4%) and
norepinephrine (39.3%, P=0.26). there were no differences in the overall rates of serious adverse
events. In the prospectively defined stratum of less severe septic shock in vasst, mortality was
significantly lower in the vasopressin-treated group at 28 days (26.5 vs. 35.7%, P=0.05). vasst
confirmed the relative deficiency of vasopressin in septic shock and low-dose vasopressin infusion
(0.01-0.30U/min) restored plasma vasopressin to an appropriate level in septic shock.
In summary, the vasst did not find a difference between low-dose vasopressin with norepinephrine
and norepinephrine alone suggesting that either approach is reasonable. However, vasopressin may
be beneficial in the less severe septic shock subgroup (patients on < 15 ug/min norepinephrine at
baseline).
Epinephrine
Epinephrine is a potent -adrenergic and -adrenergic agent that is not considered first-line therapy
for septic shock due to its detrimental effects on regional circulation and blood lactate levels [1]. The
Surviving sepsis guidelines suggest that epinephrine should be reserved for cases of extreme
hemodynamic collapse [5]. How-ever, epinephrine continues to be widely used, particularly in low-
income countries where alternative, more expensive drugs such as norepinephrine are restricted or
unavailable.
Is there a difference between norepinephrine and epinephrine in management of septic shock?
To address this question, the CAT study investigators conducted a multicenter randomized
controlled trial of norepinephrine in septic shock [7]. In four ICUs, 280 patients requiring vasopressor
support for any reason were randomized to receive either epinephrine or norepinephrine. There was
no difference in the primary outcome (MAP) or the secondary outcomes (28-day or 90-day
mortality). The findings were the same in the a priori subgroup of patients with severe sepsis at
baseline (no difference in outcomes). Epinephrine was associated with the development of
significant tachycardia, lactic acidosis and increased insulin requirements for the first 24h of the
study, after which there was no difference between the two drugs. The authors conclude that either
norepinephrine or epinephrine can be used effectively in the ICU and that the use of epinephrine
presents a cost-effective alternative to norepibephrine in low-income countries.
Phenylephrine
Previous findings suggest that a delayed administration of phenylephrine replacing norepinephrine
in septic shock patients causes a more pronounced hepatosplanchnic vasoconstriction as compared
with norepinephrine. In a prospective, randomized controlled trial, 32 septic shock patients were
randomly allocated to treatment with either norepinephrine or phenylephrine infusion [8]. Data
from right heart catheterization, a thermodilution cathere, gastric tonometry, acid-base
homeostasis, as well as creatinine clearance and cardiac troponin were obtained at baseline and
after 2h. No differences were found in any of the investigated parameters. This study suggests there
are no differences in terms of cardiopulmonary performance, global oxygen transport and regional
hemodynamics when phenylephrine was administered instead of norepinephrine in the initial
hemodynamic support of septic shock.
Terlipressin
Terlipressin, an analogue of vasopressin with a longer duration of action, is under investigation for
the treatment of hypotension not responsive to conventional
Vous aimerez peut-être aussi
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeD'EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeÉvaluation : 4 sur 5 étoiles4/5 (5795)
- Glaukoma Fakolitik: ReferatDocument4 pagesGlaukoma Fakolitik: ReferatDian Cahaya UtamiPas encore d'évaluation
- Grit: The Power of Passion and PerseveranceD'EverandGrit: The Power of Passion and PerseveranceÉvaluation : 4 sur 5 étoiles4/5 (588)
- International Seminar On Sports Science 2012: Marsiyem Lecturer Sriwijaya University Dear Ms MarsiyemDocument2 pagesInternational Seminar On Sports Science 2012: Marsiyem Lecturer Sriwijaya University Dear Ms MarsiyemDian Cahaya UtamiPas encore d'évaluation
- The Yellow House: A Memoir (2019 National Book Award Winner)D'EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Évaluation : 4 sur 5 étoiles4/5 (98)
- Kungfu Panda 2Document3 pagesKungfu Panda 2Dian Cahaya UtamiPas encore d'évaluation
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceD'EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceÉvaluation : 4 sur 5 étoiles4/5 (895)
- Green, Pink and Yellow: OrientationDocument4 pagesGreen, Pink and Yellow: OrientationDian Cahaya UtamiPas encore d'évaluation
- Shoe Dog: A Memoir by the Creator of NikeD'EverandShoe Dog: A Memoir by the Creator of NikeÉvaluation : 4.5 sur 5 étoiles4.5/5 (537)
- Administration Staff - Palembang: Posted By: Telcojob Posted Date: 18-Nov-2011 Location: Simpang Polda / TMP - PalembangDocument2 pagesAdministration Staff - Palembang: Posted By: Telcojob Posted Date: 18-Nov-2011 Location: Simpang Polda / TMP - PalembangDian Cahaya UtamiPas encore d'évaluation
- The Emperor of All Maladies: A Biography of CancerD'EverandThe Emperor of All Maladies: A Biography of CancerÉvaluation : 4.5 sur 5 étoiles4.5/5 (271)
- Scenario B Block 1: 1. Term ClarificationDocument3 pagesScenario B Block 1: 1. Term ClarificationDian Cahaya UtamiPas encore d'évaluation
- The Little Book of Hygge: Danish Secrets to Happy LivingD'EverandThe Little Book of Hygge: Danish Secrets to Happy LivingÉvaluation : 3.5 sur 5 étoiles3.5/5 (400)
- GAD Case Manuscript BSN 3Y2 1A Group 5 1Document25 pagesGAD Case Manuscript BSN 3Y2 1A Group 5 1Melody B. MiguelPas encore d'évaluation
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureD'EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureÉvaluation : 4.5 sur 5 étoiles4.5/5 (474)
- Chorioamnionitis by DR Simon ByonanuweDocument31 pagesChorioamnionitis by DR Simon ByonanuweDr Simon ByonanuwePas encore d'évaluation
- On Fire: The (Burning) Case for a Green New DealD'EverandOn Fire: The (Burning) Case for a Green New DealÉvaluation : 4 sur 5 étoiles4/5 (74)
- WC BPR - Prevention and Management of Diabetic Foot Ulcers 1573r4e FinalDocument68 pagesWC BPR - Prevention and Management of Diabetic Foot Ulcers 1573r4e FinalArumDesiPratiwiPas encore d'évaluation
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersD'EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersÉvaluation : 4.5 sur 5 étoiles4.5/5 (345)
- Lecture CasesDocument12 pagesLecture CasesGLEE ANN UYCOCOPas encore d'évaluation
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryD'EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryÉvaluation : 3.5 sur 5 étoiles3.5/5 (231)
- Aero-Digestive & Respiratory Changes Post TraheostomyDocument36 pagesAero-Digestive & Respiratory Changes Post Traheostomyrahaf abusalahPas encore d'évaluation
- Never Split the Difference: Negotiating As If Your Life Depended On ItD'EverandNever Split the Difference: Negotiating As If Your Life Depended On ItÉvaluation : 4.5 sur 5 étoiles4.5/5 (838)
- Study. RSUD Soetomo Surabaya. Vol. 26. No 3. Universitas AirlanggaDocument2 pagesStudy. RSUD Soetomo Surabaya. Vol. 26. No 3. Universitas AirlanggaKhoirunnisaSPazkaPas encore d'évaluation
- Ebook PDF Wongs Nursing Care of Infants and Children 11th Edition PDFDocument47 pagesEbook PDF Wongs Nursing Care of Infants and Children 11th Edition PDFalan.greer58697% (32)
- Team of Rivals: The Political Genius of Abraham LincolnD'EverandTeam of Rivals: The Political Genius of Abraham LincolnÉvaluation : 4.5 sur 5 étoiles4.5/5 (234)
- Bacillus Cereus and Related SpeciesDocument15 pagesBacillus Cereus and Related SpeciesxloupatiaPas encore d'évaluation
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaD'EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaÉvaluation : 4.5 sur 5 étoiles4.5/5 (266)
- Moderately HighLY Protein Bound DrugsDocument10 pagesModerately HighLY Protein Bound DrugsArah MomoPas encore d'évaluation
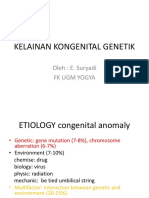
- Kelainan Kongenital GenetikDocument39 pagesKelainan Kongenital GenetikvictorPas encore d'évaluation
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyD'EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyÉvaluation : 3.5 sur 5 étoiles3.5/5 (2259)
- Milestones 201803cannabisDocument4 pagesMilestones 201803cannabisapi-444357076Pas encore d'évaluation
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreD'EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreÉvaluation : 4 sur 5 étoiles4/5 (1091)
- DrugDocument3 pagesDrugPeace Andong PerochoPas encore d'évaluation
- DR Evert Solomon Pangkahila, Spog K, M Biomed Rekomendasi PenggunaanDocument37 pagesDR Evert Solomon Pangkahila, Spog K, M Biomed Rekomendasi PenggunaannandaPas encore d'évaluation
- Encefalitis 2022Document10 pagesEncefalitis 2022SMIBA MedicinaPas encore d'évaluation
- IPOL Package InsertDocument28 pagesIPOL Package InsertHeather X RhodesPas encore d'évaluation
- Regional Obstetric Early Warning Score ChartDocument2 pagesRegional Obstetric Early Warning Score ChartDaeng Farahnaz100% (2)
- The Unwinding: An Inner History of the New AmericaD'EverandThe Unwinding: An Inner History of the New AmericaÉvaluation : 4 sur 5 étoiles4/5 (45)
- Bahan ReferatDocument17 pagesBahan ReferatGisma CPas encore d'évaluation
- 5 HVGSDocument3 pages5 HVGSkrishnamoorthy abiramanPas encore d'évaluation
- Ascaris LumbricoidesDocument14 pagesAscaris LumbricoidesLuis MercadoPas encore d'évaluation
- Yic Com - English Skills Ii Final ExamDocument6 pagesYic Com - English Skills Ii Final ExamWeldu GebruPas encore d'évaluation
- Delirium Screening PRISMEDocument1 pageDelirium Screening PRISMEWardah Fauziah El SofwanPas encore d'évaluation
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)D'EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Évaluation : 4.5 sur 5 étoiles4.5/5 (121)
- Immunization Decline CASE STUDYDocument9 pagesImmunization Decline CASE STUDYRon Isabelle D. TabelonaPas encore d'évaluation
- Rapid Laboratory Diagnosis of Cholera in The Field 0035-9203 (89) 90733-5Document2 pagesRapid Laboratory Diagnosis of Cholera in The Field 0035-9203 (89) 90733-5JUAN HERNANDEZPas encore d'évaluation
- Pediatric Nursing Week 1Document3 pagesPediatric Nursing Week 1Jonah MaasinPas encore d'évaluation
- Lateral and Medial EpicondylitisDocument40 pagesLateral and Medial EpicondylitisVijay PradeepPas encore d'évaluation
- Grieving & BereavementDocument44 pagesGrieving & Bereavementsarah alzgPas encore d'évaluation
- World Issues - Vaccine Preventable Diseases - EssayDocument3 pagesWorld Issues - Vaccine Preventable Diseases - EssaymikaylaPas encore d'évaluation
- Daftar Pustaka Responsi BsDocument2 pagesDaftar Pustaka Responsi BsghaziaPas encore d'évaluation
- Kenacort A 10Document5 pagesKenacort A 10JOHA1408Pas encore d'évaluation
- A. What Is Amnesia?Document7 pagesA. What Is Amnesia?byun syahiraPas encore d'évaluation
- Her Body and Other Parties: StoriesD'EverandHer Body and Other Parties: StoriesÉvaluation : 4 sur 5 étoiles4/5 (821)