Académique Documents
Professionnel Documents
Culture Documents
Dental Report FINAL
Transféré par
Statesman JournalCopyright
Formats disponibles
Partager ce document
Partager ou intégrer le document
Avez-vous trouvé ce document utile ?
Ce contenu est-il inapproprié ?
Signaler ce documentDroits d'auteur :
Formats disponibles
Dental Report FINAL
Transféré par
Statesman JournalDroits d'auteur :
Formats disponibles
Oregon Health & Science University
University of Washington
Prepared by:
Benjamin Sun, MD, MPP
Donald L. Chi, DDS, PhD
1
Emergency Department Visits
for Non-Traumatic Dental Problems
in Oregon State
Part I: Emergency Department Claims Analysis
Part II: Qualitative Interview Analysis
Report to the Oregon Oral Health Funders Collaborative
March 17, 2014
Oregon Health & Science University
University of Washington
Prepared by:
Benjamin Sun, MD, MPP
Donald L. Chi, DDS, PhD
ii
Acknowledgements
The Oral Health Funders Collaborative of Oregon and Southwest Washington determined the need for
this study and several funders pooled resources to provide a grant for this work, including The Ford Family
Foundation, Kaiser Permanente, Northwest Health Foundation, The Oregon Community Foundation,
PacifcSource Foundation for Health Improvement, Ronald McDonald House Charities of Oregon and
Southwest Washington, Ronald McDonald House Charities Global and Samaritan Health Services.
While the authors accept full responsibility for its contents, we also wish to acknowledge the intellectual
as well as the fnancial support of the Collaborative. Many members reviewed an early draft of this report
and provided valuable feedback, as well as support with the logistical challenges of recruiting hospitals and
communities to participate in the project.
Oral Health Funders Collaborative
Vision: Outstanding Oral Health for All
The Oral Health Funders Collaborative of Oregon and Southwest Washington is a partnership of ten regional
philanthropic organizations that are coordinating their eforts to identify, advocate and invest in oral health
solutions. Steering Committee members include Cambia Health Foundation, Dental Foundation of Oregon,
The Ford Family Foundation, Grantmakers of Oregon and Southwest Washington, Kaiser Permanente,
Northwest Health Foundation, The Oregon Community Foundation, Providence Health & Services, Ronald
McDonald House Charities of Oregon and Southwest Washington and Samaritan Health Services. More
information can be found at this website: http://www.oregoncf.org/ocf-initiatives/ohfc
iii
iii
Table of Contents
Section
Part 1: Executive Summary . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .. . . . 1
Part 2: Executive Summary . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .. . . . 2
PART 1
Background . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 3
Methods . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 3
Findings
Table 1. Top Primary Non-Trauma Dental Diagnoses, All Patients . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 4
Figure 1. Predictors of ED Dental Visits. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 5
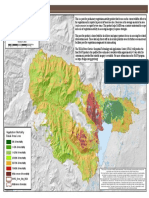
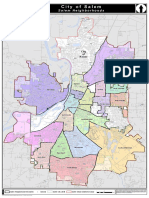
Figure 2. Number of ED Dental Visits by Patient Residential Zip Code (APAC) . . . . . . . . . . . . . . . . . . . . . . . . 6
Figure 3. Number of ED Dental Visits per Patient . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 7
Conclusions . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 8
ED Claims Analysis Study Team . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 9
Appendix
Study Methods . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 10
Appendix Table 1 ICD-9 Discharge Codes for Non-Traumatic Dental Problems . . . . . . . . . . . . . . . . . . . . . . . 13
Appendix Table 2 Participating and Non-Participating Hospitals . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 14
Appendix Figure 1 Participating and Non-Participating Hospitals . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 17
Appendix Table 3 Comparison of Participating and Non-Participating Hospitals. . . . . . . . . . . . . . . . . . . . . .18
Appendix Table 4 Characteristics of ED Dental and Non-Dental Visits. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 19
Appendix Table 5 Top 20 Primary Dental Diagnoses, Discharged Patients . . . . . . . . . . . . . . . . . . . . . . . . . . . 20
Appendix Table 6 Top Primary Dental Diagnoses, Admitted Patient . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 21
Appendix Table 7 Top 20 Secondary Dental Diagnoses, All Patients . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 22
Appendix Table 8 Top 20 Secondary Dental Diagnoses, Discharged Patients . . . . . . . . . . . . . . . . . . . . . . . . 24
Appendix Table 9 Top 20 Secondary Dental Diagnoses, Admitted Patients . . . . . . . . . . . . . . . . . . . . . . . . . . 26
Appendix Table 10 Prescription Medications Dispensed After ED Dental Visit . . . . . . . . . . . . . . . . . . . . . . . . . 28
Appendix Table 11 Procedures Associated with ED Dental Visits . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 29
Appendix Figure 2 Number of ED Dental Visits in 2010 by Patient Residential Zip Code,
Oregon Health Plan Benefciaries (APAC) . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 30
Appendix Figure 3 Number of ED Dental Visits in 2010 by Patient Residential Zip Code,
All Payers (Hospital Data) . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 31
Appendix Figure 4 Number of ED Dental Visits in 2010 by Patient Residential Zip Code,
Oregon Health Plan Benefciaries and Uninsured (Hospital Data) . . . . . . . . . . . . . . . . . . 32
References . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 33
Page
iv Part 1
PART 2
Section
Background . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 35
Data . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 36
Main Findings . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 37
Preliminary Conceptual Model on NTDC-Related ED use . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 43
Policy Recommendations . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 44
Conclusions . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 45
Study Team . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 46
References . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 47
Page
1 Part 1
Part I: Executive Summary
Part I summarizes the analysis of two complementary data sources for the year 2010: data from 24 Oregon
hospitals representing 745,348 Emergency Department (ED) visits and statewide data on insured patients
visits to Oregon hospitals representing 1,587,649 ED visits. We found:
ED visits for dental conditions are common.
Approximately 2% of Oregon ED visits were for non-traumatic dental problems. This condition is the
twelfth most common ED discharge diagnosis. Among young adults (ages 2039 years), it is the second
most common discharge diagnosis. Extrapolation to all Oregon hospitals suggests 28,000 annual
ED dental visits. Hospital admissions are uncommon (2%) but are associated with potentially
serious medical complications.
ED visits for dental conditions refect lack of access to dental care.
ED visits by uninsured Oregonians were eight times more likely to be for dental problems than were visits
by commercially-insured patients. Compared to commercially-insured Oregonians, Oregon Health Plan
(OHP) enrollees visits were four times more likely to be for dental problems.
People living closer to hospitals are more likely to seek dental care in EDs, emphasizing the importance
of providing access to dental care close to where the need is.
ED visits for dental care are unlikely to cure the patients dental problem.
The majority of patients received opioid pain medications and antibiotics, which may reduce pain and
potentially prevent progression to uncommon but serious complications.
Dental procedures are seldom performed in the ED, suggesting that most patients leave the ED still in
need of defnitive dental care.
One quarter of Oregonians who sought care in an ED for a dental problem returned to the ED for further
dental care.
Failure to provide access to dental care may add cost to the healthcare system.
The mean cost per ED dental visit was $294, greater than the cost for a years coverage in an Oregon
Dental Care Organization (average annual capitation payment $228). Extrapolation to all Oregon
hospitals suggests annual costs as high as $8 million for ED dental visits.
These fndings highlight the need for better community resources for oral health. Medicaid expansion as
part of the Afordable Care Act, combined with integration of medical and dental benefts through Oregons
Coordinated Care Organizations, provide unique opportunities to improve oral health and reduce ED dental
visits of Oregonians. However, when that care is not available, preserving ED access remains essential
to relieve the burden of pain, reduce the risk of infectious complications, and identify uncommon but
medically serious conditions associated with dental problems.
POLICY RECOMMENDATION:
Oregon should mandate ED data reporting, similar to requirements in 31 other states. ED claims
collection from individual health systems is slow, burdensome, and results in incomplete data.
A statewide, mandatory ED dataset will facilitate future health policy analyses.
2 Part 1
Part 2: Executive Summary
Part II summarizes analyses from interviews with 34 stakeholders and 17 patients in 6 Oregon communities.
We had three goals: 1) to identify the factors related to ED use for non-traumatic dental conditions (NTDCs);
2) to poll stakeholders on potential solutions that could be implemented to reduce NTDC-related ED use;
and 3) to distill research fndings into prevention-oriented policy recommendations.
The determinants of NTDC-related ED visits are multilevel and multifactorial
ED visits are related to factors at the health system, community, provider, and patient levels.
The health system is disjointed and the state Medicaid program, at the time of the interviews, had
limited dental coverage for adults.
At the community level, lack of urgent care clinics, insufcient dissemination of information on dental
care resources, and no water fuoridation contributes to NTDC-related ED visits.
At the provider level, there are few dentists who accept Medicaid, dental ofce policies are infexible
(particularly in regards to after hours emergencies), and many dentists refer patients directly to the ED.
Social and economic disadvantage, poor oral health behaviors (e.g., symptom-driven dental care use),
dental fears, and lack of a dental home were cited by patients as reasons for individuals utilizing the ED.
Even with the Afordable Care Act and Coordinated Care Organizations, there will be individuals who
do not qualify for dental coverage, leaving some vulnerable individuals susceptible to NTDC-related ED
visits.
Stakeholders ofered potential solutions to reduce ED use for NTDCs, many of which are un-
likely to systematically solve the problem
Train more dentists.
Open mode dental clinics, including urgent care clinics.
Increase availability of dentist-on-call within ED.
Enhance ED-to-dental-ofce referral system.
Assign Medicaid enrollees with primary dental care providers and case managers
Most solutions provided by stakeholders focused predominantly on improving access to dental care,
which is unlikely to meaningfully reduce NTDC-related ED visits
Reducing and preventing ED use for NTDCs involves a systematic, multilevel approach
Focus on primary prevention in adolescents to reduce subsequent ED visits by Medicaid enrollees ages
20 and 30
Develop a statewide surveillance system focusing on adolescents (Smile Survey) and implement metrics
to track progress within this high-risk population
Use the current Medicaid system and work with school nurses within junior and senior high schools to
identify and refer adolescents with dental disease and treatment needs
Educate community about changes in the Oregon Health Plan (Medicaid) and dental benefts
Distribute free toothpaste and reduce availability of sugar sweetened beverages within schools (pouring
rights)
3 Part 1
PART 1
Background
There are an estimated 2 million annual ED visits for non-traumatic dental problems (dental pain and oral
disease caused by caries, pulpitis, periodontal disease) in the United States
1
and the incidence has increased
over the past decade.
26
Use of EDs for non-traumatic dental problems generates over $110 million in
charges per year in the United States
7
. EDs are ill-equipped to provide defnitive dental care such as dental
restorations or tooth extractions
810
. Management of non-traumatic dental problems in the ED consists
primarily of temporary pain and infection control through prescriptions for analgesics and antibiotics
11
.
Elimination of Medicaid dental coverage in Oregon
12
and Maryland
13
led to increases in ED visits for
non-traumatic dental problems. Patient surveys identifed lack of insurance, lack of money, no existing
relationship with a regular dentist, and limited hours of dental care sites as reasons for seeking dental care in
an ED
14
. Multiple studies
17, 9,1117
have consistently identifed lack of insurance, Medicaid insurance, young
adult age (1844 years), and black race as predictors of visiting an ED for dental pain.
Developing interventions to improve dental access in Oregon communities requires state-specifc data but
little research has been done about dental ED use in our state. This report addresses these knowledge gaps.
A separate report, led by Donald Chi, DDS, PhD of the University of Washington, describes fndings from
qualitative analyses of dental community stakeholder interviews.
Methods
In order to characterize dental ED use throughout the entire State of Oregon as accurately as possible, we
obtained emergency department data from two sources. We requested data from a representative sample
of Oregons 58 hospitals selected based on urban/rural location, critical access designation, geographic
distribution, and annual ED visits. In addition, we obtained data from the Oregon All Payer All Claims (APAC)
database, maintained by the Oregon Health Authoritys Ofce for Oregon Health Policy and Research.
The two data sources complement each other in several ways. Despite its name, the All Payer All Claims
dataset contains data on ~6570% of ED visits. It excludes ED visits by the uninsured, as well as ED visits by
enrollees in Medicare fee-for-service plans, some other federal programs, and one commercial insurer.
Conversely, the data obtained directly from hospitals includes all ED visits to those hospitals; however, only
24 hospitals provided data. The APAC dataset includes all Oregon EDs, allowing a statewide picture for those
payer classes included in the data.
With careful attention to the strengths and limitations of each data source, we are confdent in the results
presented in this report. Where there are concerns about our ability to provide an accurate statewide
picture, we have made those limitations explicit in the Appendix, which provides further detail about the
methods used.
4 Part 1
Findings
ED visits for dental conditions are common.
There were 745,348 ED visits in 2010 to the 24 participating hospitals. Of these, 15,018 visits (2%) were
for non-traumatic dental problems. Dental conditions represent the twelfth most common ED primary
discharge diagnosis and are more frequent than headache, pneumonia, and asthma. Among young adults
(ages 2039 years), dental conditions represented the second most common discharge diagnosis.
We describe specifc dental diagnoses in Table 1. The most common diagnosis (41% of visits) was
unspecifed disorder of the teeth. The lack of precision in diagnosis may refect emergency physicians
inability to defnitively diagnose many dental conditions.
Primary Diagnosis ICD9 Code n %*
Unspecifed disorder of the teeth and supporting structures 525.9 6232 41.5
Periapical abscess without sinus 522.5 3521 23.45
Dental caries, unspecifed 521.00 2958 19.7
Acute apical periodontitis of pulpal origin 522.4 1098 7.31
Other dental caries 521.09 611 4.1
Other dental diagnoses 523.9 563 3.8
*denominator is all ED visits with primary non-trauma ED dental diagnosis (denominator = 15,018)
Table 1: Top Primary Non-Trauma Dental Diagnoses, All Patients
Although only 360 (2%) patients with dental ED visits required hospital admission, these cases illustrate the
risks of deferring dental care. Diagnoses included infectious complications of dental conditions, such as
cellulitis and abscess of face or oral soft tissues, cellulitis and abscess of the neck, pneumonia, and bacterial
endocarditis. Other patients were admitted with uncontrolled diabetes, a condition that can be aggravated
by dental infections.
Despite its limitations, the APAC database yields a similar estimate of the total number of dental ED visits
in the state. Of the 1,587,649 ED visits in the APAC database, there were 25,683 ED dental visits. Adding the
uninsured and the other groups not included in APAC supports the estimate of 28,000 dental ED visits per
year obtained from the participating hospitals.
5 Part 1
0
0.2
0.4
0.6
0.8
1
1.2
1.4
1.6
*Asian *Other *Hispanic white (reference) Missing Black Native American
0
1
2
3
4
5
6
7
8
Other Medicare Commercial Medicaid -
Other States
Medicaid
(formerly OHP)
Uninsured
0
1
2
3
4
5
6
Male (reference) Female
0
1
2
3
4
5
6
7
8
9
0-14
(reference)
1
15-19 20-39 40-64 65+
ED visits for dental conditions refect lack of access to dental care.
ED visits by uninsured Oregonians were eight times more likely to be for dental problems than were visits
by commercially-insured patients (Figure 1). Compared to commercially-insured Oregonians, Oregon Health
Plan (OHP) enrollees visits were four times more likely.
Other predictors of an ED dental visit included young adult age (2039 years) and male gender. Asians,
Hispanics, and other race patients were less likely to have an ED dental visit compared to whites.
Gender
Figure 1: Predictors of ED Dental Visits
Insurance
The Y-axis represents the unadjusted relative risk that an individuals ED visit is for
a dental condition, given that they had an ED visit.
Age
Race
Other Medicare Commercial Medicaid Medicaid Uninsured
(reference) (other states) (formerly OHP)
014 1519 2039 4064 65+
(reference)
Male Female
(reference)
Asian Black Hispanic Native Other White Missing
American (reference)
6 Part 1
Figure 2. Number of ED Dental Visits by Patient Residential Zip Code (APAC)
Geographic analyses (Figure 2) show that most users of EDs for dental conditions live near hospitals. This
fnding suggests an opportunity for a solution: Locating dental safety net clinics in communities with high
dental ED use could reduce the unmet dental care needs in these high-use communities.
Non-Traumatic ED Dental Visits
0/Insufficient Data
1 - 3
4 - 13
14 - 37
38 - 300
Hospital Locations
7 Part 1
ED visits for dental care are unlikely to cure the patients dental problem.
The majority of patients received prescriptions for pain medications (56% received opioids and 9%
nonsteroidal anti-infammatory drugs). A signifcant proportion of patients received antibiotics (36%
received penicillins, 16% clindamycin, 2% macrolides, and 2% cephalosporins).
However, dental procedures were seldom performed: 7% of encounters were associated with a facial nerve
block (which provides only temporary relief of pain), while only 2% resulted in drainage of a dental abscess.
Fewer than 0.04% had a tooth extraction. These fndings confrm the perception that EDs lack the proper
equipment (e.g. panoramic dental x-ray machines) and personnel to deliver defnitive dental care.
Over 25% of patients with an ED dental visit had more than one annual ED encounter for non-traumatic
dental problems, suggesting that the problem was not defnitively treated on the frst visit (Figure 3). The
estimate of repeat ED dental visitors is likely an undercount due to the exclusion of uninsured and Medicare
Fee-For-Service patients in APAC. These excluded groups are at higher risk of experiencing an ED dental visit.
Failure to provide access to dental care may add cost to the healthcare system.
In the APAC population, 25,683 ED dental visits accounted for $7.2 million in costs, at a mean cost of $293
per visit. Extrapolation to all Oregon hospitals suggests annual costs as high as $8 million associated with
ED dental visits.
Comparing the cost of ED dental care to the cost of providing an improved dental safety net is beyond the
scope of this study. However, it is striking to note that the average annual capitation payment for an Oregon
Dental Care Organization is $228, less than the $293 average cost for a single dental ED visit
15
.
Figure 3: Number of ED Dental Visits Per Patient
0
2000
4000
6000
8000
10000
12000
0 10 20 30 40 50 60 70 80
Frequency
N
u
m
b
e
r
o
f
p
a
t
i
e
n
t
s
Number of ED Visits
0
2 0 0 0
4 0 0 0
6 0 0 0
8 0 0 0
1 0 0 0 0
1 2 0 0 0
0 1 0 2 0 3 0 4 0 5 0 6 0 7 0 8 0
F r e q u e n c y
8 Part 1
Conclusions
In summary, ED visits for non-traumatic dental problems are common, especially in patients whose
insurance status reduces their access to dental care.
Most ED visits fail to cure the dental condition, and the cost of these visits is substantial. Making available
timely and accessible care by a dental practitioner is likely to reduce dental ED use while improving the oral
health of vulnerable Oregonians.
However, when that care is not available, preserving access to emergency departments for dental conditions
remains essential to relieve the burden of pain, reduce the risk of infectious complications, and identify
uncommon but medically serious conditions associated with dental problems.
POLICY RECOMMENDATIONS
Part I of this study focused on describing the extent and impact of ED dental visits, and Part II will describe
potential solutions. However, our research team noted that collecting ED data from health systems was slow,
laborious (requiring multiple institutional research and business agreement documents), and resulted in
incomplete statewide coverage. Thirty one other states have mandatory ED data reporting requirements
20
,
and similar requirements in Oregon would facilitate health policy analyses.
Oregon should mandate ED data reporting by hospitals. The state already mandates reporting of
inpatient data, and this existing reporting infrastructure could be used to collect ED data.
9 Part 1
Part I: ED Claims Analysis Study Team
Principal Investigator: Benjamin Sun, MD, MPP
Associate Professor, Department of Emergency Medicine, Center for Policy and Research in Emergency
Medicine, Oregon Health and Science University
Co-Investigators:
Robert A. Lowe, MD, MPH
Professor, Department of Medical Informatics and Clinical Epidemiology, and Department of Emergency
Medicine; Senior Scholar, Center for Policy and Research in Emergency Medicine, Oregon Health and
Science University
Eli Schwarz, DDS, MPH, PhD
Professor and Chair, Department of Community Dentistry, Oregon Health and Science University
Project Staf:
Annick Yagapen, CCRP; Susan Malveau, MPH; Zunqiu Chen, MS and Ben Chan, PhD (OHSU)
Site Recruiters:
Sankirtana Danner, MA (OHSU Oregon Rural Practice-based Research Network); Paul McGinnis, MPA
(Eastern Oregon CCO); Erin Owen, MPH (Slocum Research & Education Foundation)
Mapping Consultants:
Molly Vogt, MS (Metro); Clinton Chiavarini, MS (Metro) and Emerson Ong (Oregon Ofce of Rural Health)
10 Part 1
Appendix: Study Methods
In this section, we provide detail about the methods used for this project, including the defnition of an ED
dental visit, data sources, hospitals contributing to the ED dataset, methods used to identify dental ED visits,
methods used to determine medications and procedures associated with ED dental visits, approach to
estimating costs for ED dental care, and methods for geographic analyses of dental ED use.
Defning an ED Dental Visit
To defne an ED dental visit, we used prior research
2, 5, 11, 13, 1619
as well as the content expertise of dental
health service researchers on our study team. We identifed a set of ICD-9 discharge codes consistent with
non-traumatic dental problems. (Appendix Table 1) We focus on non-traumatic dental problems because
emergency physicians can rarely provide defnitive care for these conditions; these visits refect an unmet
need for community dental care. An ED dental visit was defned by presence of these codes as the primary
diagnosis on an ED claim.
We excluded traumatic dental problems as these may represent acute injuries, including isolated dental
injuries as well as those associated with other injuries (e.g. facial lacerations, facial bone fractures,
intracranial bleed). There may be limited alternatives other than EDs for the acute evaluation of such injuries.
Data sources
We collected 2010 data from two data sources: claims data obtained directly from hospital systems, and
the Oregon All Payer All Claims (APAC) database. We describe each dataset and how they complement each
other.
Hospital Claims Data
We requested ED claims data directly from a purposive sample of Oregon hospitals. We initially identifed
45 hospitals that were representative of all 58 Oregon hospitals, by urban/rural location, critical access
designation, geographic distribution, and annual ED visits. We contacted the CEO or CMO of all targeted
hospitals, and we signed Data Use and Business Use Agreements with all participating hospitals.
The strength of these data is the inclusion of all payer groups for the participating hospitals. We used the
hospital claims data to estimate the frequency of ED dental visits and to identify predictors of ED dental
visits.
A limitation of hospital claims data is the lack of uniform reporting on procedures, antibiotics, and costs.
In addition, these data may have limited geographic generalizability.
Of the 45 hospitals that were invited to participate in this study, 24 provided 2010 data on all ED visits.
Appendix Table 2 is a list of all Oregon hospitals sorted by participants and non-participants. Appendix
Figure 1 illustrates the locations of participants and non-participants. Appendix Table 3 uses data from the
American Hospital Association Survey and the Ofce for Oregon Health Policy and Research to illustrate the
diferences between participating and non-participating hospitals. Rural, critical access, and low volume
hospitals are under presented in our sample set. Thus, the analyses of hospital claims data may have limited
generalizability to excluded hospitals.
In Appendix Table 4, we describe the characteristics of all ED visits for both dental and non-dental problems.
The primary discharge diagnoses associated with ED dental visits are presented in the main report (Table 1).
We provide descriptive tables of primary diagnoses, stratifed by both discharged and admitted patients in
Appendix Tables 5 and 6.
11 Part 1
In addition to this descriptive reporting, we calculated the unadjusted relative risk ratios for diferent values
of age, gender, race, and payer that an ED visit would be for a dental condition. The results of these relative
risk analyses are illustrated in the main report (Figure 1).
Five hospitals within the Providence Health System (Seaside; St. Vincent; Hood River; Newberg; and Medford)
provided aggregated, rather than encounter level, data on non-dental ED visits. These hospitals, accounting
for 20% of the data, were included in descriptive reports (Appendix Table 3) but excluded from the relative
risk analysis.
Although our analyses focused on patients with a primary diagnosis of a non-traumatic dental problem,
an additional 3,551 (0.4% of all ED visits) ED visits had a secondary diagnosis of a non-traumatic dental
problem (Appendix Tables 79). The three most common associated primary diagnoses were other acute
pain, antepartum condition, and traumatic wound of tooth. This population likely includes a mixture of
patients with a primary dental problem as well as those with a unrelated primary reason for an ED visit. Our
approach of using only primary diagnoses codes to defne an ED dental visit reduces contamination by ED
visits primarily for a non-dental problem; however, it may result in an undercount of all ED dental visits. We
identifed an additional 301 hospitalizations with a secondary diagnosis of a non-traumatic dental problem;
these cases are described in the Results section and in Appendix Table 9.
The Oregon All Payer All Claims Database
The All Payer All Claims (APAC) database contains statewide information on ED visits by patients covered by
the Oregon Health Plan, commercial payers, and Medicare managed care. Our research group is among the
frst in Oregon to obtain and analyze the APAC data.
The strengths and weaknesses of APAC are the inverse of the hospital claims data. Strengths include unique
information on procedures, antibiotics, and costs. APAC can also be used to generate statewide profles of
ED dental visits.
The major limitation of APAC is the exclusion of certain payer groups. Most notably, APAC omits visits by the
uninsured that represent about 18% of Oregon ED visits, and the uninsured disproportionately use EDs for
non-traumatic dental problems. APAC also currently omits patients who are covered by Medicare Fee-For-
Service (FFS) and federal insurance (TRICARE, FEHB). Finally, one major commercial payer (Kaiser) has not yet
submitted data to APAC. Therefore, we do not rely on APAC to describe patient level characteristics such as
payer or to identify predictors of ED dental visits.
Identifying medications and procedures
With the APAC database, we identifed the top 20 non-refll prescription medication classes that were
dispensed within 3 days after an ED dental visit (Appendix Table 10). An important limitation to note is the
inability to verify that the prescriber and the ED provider were the same; it is possible that some medications
were prescribed by non ED-providers and were not related to the ED dental visit. However, the frequent
prescribing of pain medications and antibiotics noted in the APAC data is consistent with our clinical
experience.
We used billing codes (Current Procedural Terminology [CPT]) to identify procedures performed in the ED
(Appendix Table 11). This analysis excludes CPT Evaluation and Management codes that are based on the
complexity of medical decision making.
12 Part 1
Estimating costs for ED dental care
It is important to note that cost is a distinct concept from charge and payment. Charge is the billed amount,
varies greatly by hospital, and often has little relationship to cost. We did not have access to charge data.
APAC does include data on payments by insurers and patients. According to Oregon State APAC analysts,
payment data have not been verifed, and submitted Oregon Health Plan payment data are likely to be
fawed. Therefore, we do not present payment data in this report.
To estimate true costs refecting resources required to provide ED dental services, we applied the 2010
Center for Medicare and Medicaid Services (CMS) national payment tables to all CPT codes associated with
an ED dental visit. CMS payment tables are commonly used to approximate actual cost of medical services
21
.
Geographic analyses
We used both hospital and APAC data to illustrate where Oregonians who use EDs for dental conditions live.
We provide maps that illustrate frequency counts by zip codes.
There are two important methodologic limitations of our mapping approach for hospital claims data. First,
our hospital claims data did not include all hospitals in Oregon. A resident in a given zip code might have
gone to a nearby ED included in our data or to another nearby ED not included in our data. To address this
limitation, we used data from the Oregon Patient Origin Dataset to identify, for each ZIP code, the market
share for all Oregon hospitals in 2010. We then weighted the counts in each zip code to account for missing
data. For example, if our dataset had 500 ED dental visits originating in zip code 97229 but we only had
hospital data that accounted for 50% of hospital visits originating from that zip code, then we would infate
by a factor of 2 (for an estimated 1000 ED dental visits) to account for missing data. This approach makes the
assumption that ED visit rates are similar in missing data as they are in observed data.
Second, we had very few or no observed data from some zip codes. This may refect a combination of
missing hospital data and low population density in rural areas. If a zip code count was zero or was missing
more than 75% of hospital market share data, then we considered data to be unreliable for that zip code.
This approach reduces the ability to make conclusions about low-population areas and areas which are
poorly represented by our data.
APAC data include all Oregon EDs but exclude patient populations that are not represented in APAC (e.g.
uninsured, Medicare Fee-For-Service). Despite statewide coverage of APAC, there were no reported ED
dental visits for a subset of low-density zip codes.
Despite diferences in data completeness and methodology, the hospital and APAC data show similar
geographic patterns, and patterns were similar for uninsured and OHP-sponsored patients compared to all
ED patients. The robustness of our geographic fndings in two diferent datasets adds to our confdence in
these results.
Because of the similarity between diferent maps of dental ED visits, we present only the APAC map in the
body of the report (Figure 2); the other maps are presented here (Appendix Figures 2-4).
13 Part 1
ICD-9 Discharge Codes For Non-Traumatic Dental Problems
Non-Traumatic Dental Problems
520.0520.9: Disorders of tooth development and eruption
521.0521.9: Diseases of the hard tissue of teeth
522.0522.9: Diseases of pulp and periapical tissues
523.0523.9: Gingival and periodontal diseases
525.0525.9,
excluding 525.11:
Other diseases and conditions of the teeth and supporting structures
Appendix Table 1: ICD-9 Discharge Codes for Non-Traumatic Dental Problems
14 Part 1
Participating Hospital Name
Health
System
Region
Rural/
Urban
Critical
Access
ED
Annual
Visits
Yes Blue Mountain Hospital
self/none
known
NE Oregon rural Yes 2989
Yes
Cottage Grove Community
Hospital
PeaceHealth SW Oregon rural Yes 11378
Yes Grande Ronde Hospital
self/none
known
NE Oregon rural Yes 12306
Yes
Kaiser Sunnyside Medical
Center
Kaiser Portland urban No 52508
Yes Lake District Hospital
Lake Health
District
Cascades
East
rural Yes 3502
Yes
Legacy Emanuel Hospital &
Health Center
Legacy Portland urban No 46485
Yes
Legacy Good Samaritan
Hospital
Legacy Portland urban No 28440
Yes
Legacy Meridian Park
Hospital
Legacy Portland urban No 30735
Yes
Legacy Mount Hood
Medical Center
Legacy Portland urban No 40138
Yes
McKenzie-Willamette
Medical Center
Community
Health Systems
SW Oregon urban No 26803
Yes Mercy Medical Center Catholic Health SW Oregon rural No 40577
Yes OHSU Hospital OHSU Portland No 40268
Yes Peace Harbor Hospital PeaceHealth SW Oregon rural Yes 7667
Yes
Providence Hood River
Memorial Hospital
Providence NE Oregon rural Yes 9341
Yes
Providence Medford
Medical Center
Providence SW Oregon urban No 28892
Yes
Providence Milwaukie
Hospital
Providence Portland urban No 35955
Yes
Providence Newberg
Hospital
Providence Pacifc rural No 18308
Yes
Providence Portland
Medical Center
Providence Portland urban No 67874
Yes
Providence Seaside
Hospital
Providence Pacifc rural Yes 9661
Yes
Providence St. Vincent
Medical Center
Providence Portland urban No 86099
Yes
Sacred Heart Medical
Center RB
PeaceHealth SW Oregon urban No 40666
Appendix Table 2: Participating and Non-Participating Hospitals
15 Part 1
Participat-
ing
Hospital Name
Health
System
Region
Rural/
Urban
Critical
Access
ED
Annual
Visits
Yes
Sacred Heart Medical
Center UD
PeaceHealth SW Oregon No 33528
Yes Sky Lakes Medical Center
self/none
known
Cascades
East
rural No 18974
Yes Tuality Healthcare Tuality Portland No 42416
No Adventist Medical Center
Adventist
Health
Portland No 44155
No
Ashland Community
Hospital
California-
based
SW Oregon rural No 9957
No Bay Area Hospital
self/none
known
SW Oregon No 25075
No
Columbia Memorial
Hospital
self/none
known
Pacifc rural Yes 13939
No Coquille Valley Hospital
self/none
known
SW Oregon rural Yes 4218
No Curry General Hospital
Curry Health
Network
SW Oregon rural Yes 3877
No
Good Samaritan Reg
Medical Center
Legacy Pacifc No 21062
No
Good Shepherd Healthcare
System
self/none
known
NE Oregon rural Yes 16183
No Harney District Hospital
self/none
known
Cascades
East
rural Yes 2430
No
Lower Umpqua Hospital
District
Lower Umpqua
Hospital
District
SW Oregon rural Yes 3436
No
Mid-Columbia Medical
Center
self/none
known
NE Oregon rural No 17223
No
Mountain View Hospital
District
Cascade
Healthcare
Community
Cascades
East
rural Yes 10375
No
Pioneer Memorial Hospital -
Heppner
Cascade
Healthcare
Community
Cascades
East
rural Yes 804
No
Pioneer Memorial Hospital -
Prineville
Cascade
Healthcare
Community
Cascades
East
rural Yes 9203
No
Providence Willamette Falls
Medical Center
WFH Portland urban No 28165
Appendix Table 2: (continued)
16 Part 1
Participat-
ing
Hospital Name
Health
System
Region
Rural/
Urban
Critical
Access
ED
Annual
Visits
No
Rogue Valley Medical
Center
Asante Pacifc urban No 37552
No Salem Hospital Salem Health Pacifc urban No 87822
No
Samaritan Albany General
Hospital
Samaritan
Health
Pacifc urban No 24421
No
Samaritan Lebanon
Community Hospital
Samaritan
Health
Pacifc rural Yes 13170
No
Samaritan North Lincoln
Hospital
Samaritan
Health
Pacifc rural Yes 10017
No
Samaritan Pacifc
Community Hospital
Samaritan
Health
Pacifc rural Yes 12539
No Santiam Memorial Hospital
self/none
known
Pacifc rural No 11408
No Silverton Hospital
Silverton
Health
Pacifc rural No 24341
No Southern Coos Hospital
self/none
known
SW Oregon rural Yes 4156
No
St. Alphonsus Medical
Center - Baker City
Catholic Health NE Oregon rural Yes 7198
No
St. Alphonsus Medical
Center - Ontario
Catholic Health NE Oregon rural No 18639
No St. Anthony Hospital Catholic Health NE Oregon rural Yes 12903
No
St. Charles Medical Center -
Redmond
St. Charles
Cascades
East
rural No 17492
No
St. Charles Medical Center
Bend
St. Charles
Cascades
East
urban No 36606
No
Three Rivers Community
Hospital
Asante SW Oregon rural No 35529
No
Tillamook County General
Hospital
Adventist
Health
Pacifc rural Yes 9722
No
VA Roseburg Healthcare
System
Federal SW Oregon urban No 13586
No
Veterans Afairs Medical
Center
Federal Portland urban No 14320
No Wallowa Memorial Hospital
self/none
known
NE Oregon rural Yes 2677
No West Valley Hospital Salem Health Pacifc rural Yes 12651
No
Willamette Valley Medical
Center
self/none
known
Pacifc rural No 24191
Appendix Table 2: (continued)
17 Part 1
Hospital Study Participation
Participated
Did Not Participate
Appendix Figure 1: Participating and Non-Participating Hospitals
18 Part 1
Variable Non-Sample Study Sample p-value*
Hospitals (n) 36 (60%) 24 (40%) n/a
AHEC Region (n, %)
Cascades East 6 (16.67%) 2 (8.33%)
0.01
NE Oregon 6 (16.67%) 3 (12.5%)
Pacifc 13 (36.11%) 2 (8.33%)
Portland 3 (8.33%) 10 (41.67%)
SW Oregon 8 (22.22%) 7 (29.17%)
Rural (n, %) 26 (72.22%) 10 (41.67%) 0.02
Critical Access Hospital: Yes (n, %) 18 (50%) 7 (29.17%) 0.1
ED Annual Visits (mean, SD) 17806.72 (16121.54) 30646.25 (20524.98) 0.01
Inpatient Beds (mean, SD) 86.08 (96.31) 171.79 (166.9) 0.02
*p<0.05 indicates a statistically signifcant diference between participants and non-participants
Appendix Table 3: Comparison of Participating and Non-Participating Hospitals
19 Part 1
Characteristics of ED Dental Visits
Variable All Other ED Visits ED Dental Visits
ED Visits (n, row %) 730,330 (98%) 15,018 (2%)
Patient Characteristics
Age in Years (n, column%)
014 84429 (15%) 560 (3%)
1519 35187 (6%) 780 (5%)
2039 181939 (31%) 9907 (66%)
4064 173797 (30%) 3555 (24%)
65+ 104070 (18%) 190 (1%)
Male (n, column %) 329,764 (45%) 7470 (49.74%)
Race (n, column %)
White 471,196 (64.52%) 10,012 (66.67%)
Asian 7900 (1.08%) 45 (0.3%)
Black 28,916 (3.96%) 747 (4.97%)
Hispanic 4357 (0.6%) 93 (0.62%)
Native American 7177 (0.98%) 232 (1.54%)
Other 47,532 (6.51%) 609 (4.06%)
Missing 163,252 (22.35%) 3280 (21.84%)
Payer (n, column %)
Missing 1991 (0.27%) 92 (0.61%)
Other 43,923 (6.01%) 176 (1.17%)
Commercial 210,957 (29.11%) 1430 (9.52%)
Medicaid - Other States 3412 (0.47%) 108 (0.72%)
Medicare 166,883 (23.03%) 873 (5.81%)
Oregon Health Plan 173,827 (23.99%) 4930 (32.83%)
Uninsured 129,337 (17.85%) 7409 (49.33%)
Patient Zip Code Measures
Below Poverty Level: mean (std) 10.89 (9.17) 17.94 (20.25)
Completed High School: mean (std) 88.54 (7.2) 86.42 (9.4)
Unemployed: mean (std) 10.78 (8.62) 10.75 (5.97)
Hospital Characteristics
AHEC Region (n, column %)
Cascades East 24018 (3.29%) 453 (3.02%)
NE Oregon 25117 (3.44%) 499 (3.32%)
Pacifc 26,896 (3.68%) 403 (2.68%)
Portland 467,617 (64.03%) 8449 (56.26%)
SW Oregon 186,682 (25.56%) 5214 (34.72%)
Rural (n, column %) 140,331 (19.21%) 3346 (22.28%)
Critical Access Hospital (n, %) 53,552 (7.33%) 1292 (8.6%)
Appendix Table 4: Characteristics of ED Dental and Non-Dental Visits
20 Part 1
Primary Diagnosis ICD9 Code n %*
Unspecifed disorder of the teeth and supporting structures 525.9 6226 41.62
Periapical abscess without sinus 522.5 3477 23.24
Dental caries, unspecifed 521.00 2957 19.77
Acute apical periodontitis of pulpal origin 522.4 1093 7.31
Other dental caries 521.09 611 4.08
Disturbances in tooth eruption 520.6 127 0.85
Chronic gingivitis, plaque induced 523.10 82 0.55
Cracked tooth 521.81 61 0.41
Teething syndrome 520.7 54 0.36
Chronic periodontitis, unspecifed 523.40 44 0.29
Other specifed disorders of the teeth and supporting structures 525.8 37 0.25
Partial edentulism, unspecifed 525.50 29 0.19
Aggressive periodontitis, localized 523.31 23 0.15
Other specifed periodontal diseases 523.8 23 0.15
Acute gingivitis, plaque induced 523.00 22 0.15
Aggressive periodontitis, unspecifed 523.30 19 0.13
Acute periodontitis 523.33 15 0.1
Acquired absence of teeth, unspecifed 525.10 11 0.07
Pulpitis 522.0 9 0.06
Unspecifed gingival and periodontal disease 523.9 4 0.03
*denominator is all ED visits with primary non-trauma ED dental diagnosis who were discharged (denominator = 14,959)
Appendix Table 5: Top 20 Primary Dental Diagnoses, Discharged Patients
21 Part 1
Primary Diagnosis ICD9 Code n %*
Periapical abscess without sinus 522.5 44 74.58
Unspecifed disorder of the teeth and supporting structures 525.9 6 10.17
Acute apical periodontitis of pulpal origin 522.4 5 8.47
Aggressive periodontitis, unspecifed 523.30 1 1.69
Dental caries, unspecifed 521.00 1 1.69
Aggressive periodontitis, localized 523.31 1 1.69
Other specifed periodontal diseases 523.8 1 1.69
*denominator is all ED visits with primary non-trauma ED dental diagnosis who were admitted (denominator = 59)
Appendix Table 6: Top Primary Dental Diagnoses, Admitted Patients
22 Part 1
Secondary Dental Diagnosis ICD9 Code n %*
Unspecifed disorder of the teeth and supporting structures 5259 1014 34.14
Dental caries, unspecifed 52100 911 30.67
Periapical abscess without sinus 5225 517 17.41
Acute apical periodontitis of pulpal origin 5224 229 7.71
Acquired absence of teeth, unspecifed 52510 222 7.47
Partial edentulism, unspecifed 52550 166 5.59
Other dental caries 52109 91 3.06
Chronic gingivitis, plaque induced 52310 84 2.83
Teething syndrome 5207 74 2.49
Other specifed disorders of the teeth and supporting structures 5258 62 2.09
Disturbances in tooth eruption 5206 36 1.21
Complete edentulism, unspecifed 52540 32 1.08
Other specifed periodontal diseases 5238 23 0.77
Cracked tooth 52181 19 0.64
Chronic periodontitis, unspecifed 52340 12 0.4
Acute gingivitis, plaque induced 52300 11 0.37
Unspecifed gingival and periodontal disease 5239 10 0.34
Erosion, unspecifed 52130 6 0.2
Other loss of teeth 52519 5 0.17
Other and unspecifed diseases of pulp and periapical tissues 5229 3 0.1
*denominator is all ED visits with NO primary non-trauma dental diagnosis AND any secondary non-trauma dental
diagnosis (denominator = 2,970)
Appendix Table 7: Top 20 Secondary Dental Diagnoses, All Patients
This table includes patients who had a non dental primary diagnosis but with a secondary
diagnosis consistent with a non-traumatic dental problem.
23 Part 1
Primary Diagnosis ICD9 Code n %*
Other acute pain 33819 324 10.91
Other current conditions classifable elsewhere of mother, antepartum
condition or complication
64893 139 4.68
Open wound of tooth (broken) (fractured) (due to trauma), without
mention of complication
87363 115 3.87
Headache 7840 94 3.16
Cellulitis and abscess of face 6820 83 2.79
Swelling, mass, or lump in head and neck 7842 70 2.36
Other acute postoperative pain 33818 69 2.32
Unspecifed disease of the jaws 5269 53 1.78
Acute pharyngitis 462 49 1.65
Other and unspecifed diseases of the oral soft tissues 5289 42 1.41
Issue of repeat prescriptions V681 42 1.41
Fever, unspecifed 78060 40 1.35
Otalgia, unspecifed 38870 40 1.35
Acute upper respiratory infections of unspecifed site 4659 37 1.25
Unspecifed otitis media 3829 36 1.21
Unspecifed essential hypertension 4019 31 1.04
Open wound of lip, without mention of complication 87343 29 0.98
Migraine, unspecifed, without mention of intractable migraine without
mention of status migrainosus
34690 29 0.98
Syncope and collapse 7802 27 0.91
Nausea with vomiting 78701 26 0.88
*denominator is all ED visits with NO primary non-trauma dental diagnosis AND any secondary non-trauma dental diagnosis
(denominator = 2,970)
Appendix Table 7: (continued)
This table includes patients who had a non dental primary diagnosis but with a secondary diagnosis
consistent with a non-traumatic dental problem.
24 Part 1
Secondary Dental Diagnosis ICD9 Code n %*
Unspecifed disorder of the teeth and supporting structures 5259 975 36.06
Dental caries, unspecifed 52100 848 31.36
Periapical abscess without sinus 5225 443 16.38
Acquired absence of teeth, unspecifed 52510 214 7.91
Acute apical periodontitis of pulpal origin 5224 195 7.21
Partial edentulism, unspecifed 52550 158 5.84
Other dental caries 52109 80 2.96
Chronic gingivitis, plaque induced 52310 74 2.74
Teething syndrome 5207 72 2.66
Other specifed disorders of the teeth and supporting structures 5258 50 1.85
Disturbances in tooth eruption 5206 33 1.22
Complete edentulism, unspecifed 52540 22 0.81
Cracked tooth 52181 17 0.63
Other specifed periodontal diseases 5238 14 0.52
Chronic periodontitis, unspecifed 52340 11 0.41
Acute gingivitis, plaque induced 52300 10 0.37
Erosion, unspecifed 52130 6 0.22
Unspecifed gingival and periodontal disease 5239 5 0.18
Other loss of teeth 52519 4 0.15
Anodontia 5200 2 0.07
*denominator is all ED visits with NO primary non-trauma dental diagnosis AND any secondary non-trauma dental
diagnosis AND patient discharged (denominator = 2,704)
Appendix Table 8: Top 20 Secondary Dental Diagnoses, Discharged
This table includes patients who had a non dental primary diagnosis but with a secondary
diagnosis consistent with a non-traumatic dental problem.
25 Part 1
Primary Diagnosis ICD9 Code n %*
Other acute pain 33819 324 11.98
Other current conditions classifable elsewhere of mother, antepartum
condition or complication
64893 139 5.14
Open wound of tooth (broken) (fractured) (due to trauma), without
mention of complication
87363 115 4.25
Headache 7840 94 3.48
Other acute postoperative pain 33818 68 2.51
Swelling, mass, or lump in head and neck 7842 68 2.51
Cellulitis and abscess of face 6820 67 2.48
Unspecifed disease of the jaws 5269 53 1.96
Acute pharyngitis 462 49 1.81
Issue of repeat prescriptions V681 42 1.55
Other and unspecifed diseases of the oral soft tissues 5289 41 1.52
Otalgia, unspecifed 38870 40 1.48
Fever, unspecifed 78060 38 1.41
Acute upper respiratory infections of unspecifed site 4659 37 1.37
Unspecifed otitis media 3829 36 1.33
Unspecifed essential hypertension 4019 30 1.11
Migraine, unspecifed, without mention of intractable migraine without
mention of status migrainosus
34690 29 1.07
Open wound of lip, without mention of complication 87343 28 1.04
Hemorrhage complicating a procedure 99811 25 0.92
Nausea with vomiting 78701 25 0.92
*denominator is all ED visits with NO primary non-trauma dental diagnosis AND any secondary non-trauma dental diagnosis AND
patient discharged (denominator = 2,704)
Appendix Table 8: (continued)
This table includes patients who had a non dental primary diagnosis but with a secondary diagnosis
consistent with a non-traumatic dental problem.
26 Part 1
Secondary Dental Diagnosis ICD9 Code n %*
Periapical abscess without sinus 5225 74 27.82
Dental caries, unspecifed 52100 63 23.68
Unspecifed disorder of the teeth and supporting structures 5259 39 14.66
Acute apical periodontitis of pulpal origin 5224 34 12.78
Other specifed disorders of the teeth and supporting structures 5258 12 4.51
Other dental caries 52109 11 4.14
Complete edentulism, unspecifed 52540 10 3.76
Chronic gingivitis, plaque induced 52310 10 3.76
Other specifed periodontal diseases 5238 9 3.38
Partial edentulism, unspecifed 52550 8 3.01
Acquired absence of teeth, unspecifed 52510 8 3.01
Unspecifed gingival and periodontal disease 5239 5 1.88
Disturbances in tooth eruption 5206 3 1.13
Teething syndrome 5207 2 0.75
Cracked tooth 52181 2 0.75
Dental caries extending into pulp 52103 2 0.75
Loss of teeth due to caries 52513 2 0.75
Acute periodontitis 52333 1 0.38
Other and unspecifed diseases of pulp and periapical tissues 5229 1 0.38
Chronic periodontitis, unspecifed 52340 1 0.38
*denominator is all ED visits with NO primary non-trauma dental diagnosis AND any secondary non-trauma dental diagnosis
AND patient admitted (denominator = 266)
Appendix Table 9: Top 20 Secondary Dental Diagnoses, Admitted
This table includes patients who had a non dental primary diagnosis but with a secondary
diagnosis consistent with a non-traumatic dental problem.
27 Part 1
Primary Diagnosis ICD9 Code n %*
Cellulitis and abscess of face 6820 16 6.02
Cellulitis and abscess of oral soft tissues 5283 9 3.38
Syncope and collapse 7802 7 2.63
Coronary atherosclerosis of native coronary artery 41401 5 1.88
Diabetes with ketoacidosis, type I [juvenile type], uncontrolled 25013 4 1.5
Bipolar I disorder, most recent episode (or current) depressed,
unspecifed
29650 4 1.5
Pneumonia, organism unspecifed 486 4 1.5
Other chest pain 78659 4 1.5
Other and unspecifed noninfectious gastroenteritis and colitis 5589 3 1.13
Iron defciency anemia secondary to blood loss (chronic) 2800 3 1.13
Cellulitis and abscess of neck 6821 3 1.13
Cellulitis and abscess of oral soft tissues 528.3 3 1.13
Neutropenia, unspecifed 28800 3 1.13
Other bipolar disorders 29689 3 1.13
Acute systolic heart failure 42821 3 1.13
Major depressive afective disorder, recurrent episode, severe, without
mention of psychotic behavior
29633 2 0.75
Acute and subacute bacterial endocarditis 4210 2 0.75
Poisoning by antiallergic and antiemetic drugs 9630 2 0.75
Hyposmolality and/or hyponatremia 2761 2 0.75
Fever, unspecifed 780.6 2 0.75
*denominator is all ED visits with NO primary non-trauma dental diagnosis AND any secondary non-trauma dental diagnosis AND
patient admitted (denominator = 266)
Appendix Table 9: (continued)
This table includes patients who had a non dental primary diagnosis but with a secondary diagnosis
consistent with a non-traumatic dental problem.
28 Part 1
Appendix Table 10: Prescription Medications Dispensed After ED Dental Visit
Medication Class Frequency % ED Visits*
Analgesics - Opioid 14348 56%
Penicillins 9254 36%
Clindamycin 4120 16%
Analgesics - Anti-Infammatory 2242 9%
Antidepressants 678 3%
Antihistamines 671 3%
Mouth/Throat/Dental Agents 618 2%
Antianxiety Agents 520 2%
Macrolides 513 2%
Cephalosporins 462 2%
Anticonvulsants 399 2%
Ulcer Drugs 347 1%
Antiemetics 290 1%
Antiasthmatic and Bronchodilator Agents 283 1%
Musculoskeletal Therapy Agents 279 1%
Antipsychotics/Antimanic Agents 272 1%
Antihypertensives 237 1%
Corticosteroids 204 1%
Beta Blockers 157 1%
Analgesics - Nonnarcotic 151 1%
* denominator is 25,683 ED dental visits identifed in APAC
29 Part 1
Appendix Table 11: Procedures Associated With ED Dental Visits
CPT Code Description Frequency % ED Visits*
64400 Facial Nerve Block 1794 7%
85025 Blood Test: Cell Count 1239 5%
96375 Drug Injection- Subsequent Intravenous Push 867 3%
96372 Drug Injection- Subcutaneous or Intramuscular 843 3%
80053 Blood Test: Metabolic Panel 837 3%
96374 Drug Injection- Initial Intravenous Push 649 3%
96365 Intravenous Infusion 635 2%
36415 Vein Puncture 565 2%
J1170 Hydromorphone Injection 488 2%
J2405 Ondansetron Injection 481 2%
41800 Drainage of Dental Abscess from Dental Structure 478 2%
70450 Computed Tomography of Head or Brain 471 2%
* denominator is 25,683 ED dental visits identifed in APAC
30 Part 1
Appendix Figure 2: Number of ED Dental Visits in 2010 by Patient Residential Zip
Code, Oregon Health Plan Benefciaries (APAC)
Non-Traumatic OHP ED Dental Visits
0/Insufficient Data
1 - 3
4 - 12
13 - 33
34 - 264
Hospitals Locations Hospital Locations
31 Part 1
Appendix Figure 3: Number of ED Dental Visits in 2010 by Patient Residential Zip
Code, All Payers (Hospital Data)
Non-Traumatic ED Dental Visits (Weighted)
0/Insufficient Data
1 - 6
7 - 23
24 - 104
105 - 868
Hospitals Locations Hospital Locations
32 Part 1
Appendix Figure 4: Number of ED Dental Visits in 2010 by Patient Residential Zip
Code, Oregon Health Plan Benefciaries and Uninsured (Hospital Data)
Non-Traumatic OHP/Uninsured ED Dental Visits (Weighted)
0/Insufficient Data
1 - 5
6 - 20
21 - 92
93 - 778
Hospitals Locations Hospital Locations
33 Part 1
References
1. Centers for Disease Control. National Hospital Ambulatory Medical Care Survey: 2010 Emergency
Department summary Tables. 2012; http://www.cdc.gov/nchs/data/ahcd/nhamcs_emergency/
2010_ed_web_tables.pdf. Accessed Dec 26, 2013.
2. Hong L, Ahmed A, McCunnif M, Liu Y, Cai J, Hof G. Secular trends in hospital emergency department
visits for dental care in Kansas City, Missouri, 20012006. Public Health Rep. MarApr 2011;126(2):210219.
3. Ladrillo TE, Hobdell MH, Caviness AC. Increasing prevalence of emergency department visits for
pediatric dental care, 19972001. J Am Dent Assoc. Mar 2006;137(3):379385.
4. Lee HH, Lewis CW, Saltzman B, Starks H. Visiting the emergency department for dental problems: trends
in utilization, 2001 to 2008. American journal of public health. Nov 2012;102(11):e7783.
5. Anderson L, Cherala S, Traore E, Martin NR. Utilization of Hospital Emergency Departments for non-
traumatic dental care in New Hampshire, 20012008. Journal of community health.
Aug 2011;36(4):513516.
6. Wall T. Recent trends in dental emergency department visits in the United States:1997/1998 to
2007/2008. Journal of public health dentistry. Summer 2012;72(3):216220.
7. Nalliah RP, Allareddy V, Elangovan S, Karimbux N. Hospital based emergency department visits
attributed to dental caries in the United States in 2006. The journal of evidence-based dental practice.
Dec 2010;10(4):212222.
8. Pennycook A, Makower R, Brewer A, Moulton C, Crawford R. The management of dental problems
presenting to an accident and emergency department. Journal of the Royal Society of Medicine.
Dec 1993;86(12):702703.
9. Pajewski NM, Okunseri C. Patterns of dental service utilization following nontraumatic dental condition
visits to the emergency department in Wisconsin Medicaid. Journal of public health dentistry. Aug 8 2012.
10. Davis EE, Deinard AS, Maiga EW. Doctor, my tooth hurts: the costs of incomplete dental care in the
emergency room. Journal of public health dentistry. Summer 2010;70(3):205210.
11. Hocker MB, Villani JJ, Borawski JB, et al. Dental visits to a North Carolina emergency department: a
painful problem. North Carolina medical journal. SepOct 2012;73(5):346351.
12. Wallace NT, Carlson MJ, Mosen DM, Snyder JJ, Wright BJ. The individual and program impacts of
eliminating Medicaid dental benefts in the Oregon Health Plan. American journal of public health.
Nov 2011;101(11):21442150.
13. Cohen LA, Manski RJ, Hooper FJ. Does the elimination of Medicaid reimbursement afect the frequency
of emergency department dental visits? J Am Dent Assoc. May 1996;127(5):605609.
14. Dorfman DH, Kastner B, Vinci RJ. Dental concerns unrelated to trauma in the pediatric emergency
department: barriers to care. Archives of pediatrics & adolescent medicine. Jun 2001;155(6):699703.
15. Oregon Health Plan Medicaid Demonstration. Capitation Rate Development. Dental Care Organizations
Remaining During Transition to Coordinated Care Organizations. In: Actuarial Service Unit OHA, ed2013:149.
16. Cohen LA, Manski RJ, Magder LS, Mullins CD. Dental visits to hospital emergency departments by adults
receiving Medicaid: assessing their use. J Am Dent Assoc. Jun 2002;133(6):715724; quiz 768.
34 Part 1
17. Lewis C, Lynch H, Johnston B. Dental complaints in emergency departments: a national perspective.
Annals of emergency medicine. Jul 2003;42(1):9399.
18. Lowe RA. Dental and mental conditions in rural Oregon emergency departments. 23rd Annual Oregon
Rural Health Conference. Newport, Oregon2006.
19. Mullins CD, Cohen LA, Magder LS, Manski RJ. Medicaid coverage and utilization of adult dental services.
J Health Care Poor Underserved. Nov 2004;15(4):672687.
20. Agency for Healthcare Research and Quality. Overview of the State Emergency Department Databases.
Accessed 2/20/14. https://www.hcup-us.ahrq.gov/seddoverview.jsp
21. Muennig P. Cost-Efectiveness Analysis in Health: A Practical Approach. San Francisco: John Wiley & Sons;
2008.
35 Part 2
PART 2
Background
Recent U.S. data suggest signifcant increases in the number of patients utilizing the ED for treatment of
non-traumatic dental conditions (NTDCs) (Lee et al. 2012; Okunseri et al 2012). Studies have identifed
various factors related to NTDC-related ED use (e.g., low-income, racial/ethnic minority status, being insured
by Medicaid, having no insurance, and living in a Health Professional Shortage Area) (Hong et al. 2011;
Okunseri et al. 2008). Young adults ages 20 to 30 years appear to use the ED for NTDCs at higher rates than
other individuals (Chi et al. 2014). No studies to date have used qualitative methods to examine stakeholder
and patient perspectives on NTDC-related ED use and to identify possible strategies to reduce and prevent
ED visits.
The goals of this study were to identify the multilevel determinants of NTDC-related ED use, poll
stakeholders on potential solutions that could be implemented to reduce NTDC-related ED use, generate
a preliminary conceptual model on ED use, and distill research fndings into prevention-oriented policy
recommendations aimed at preventing ED use for NTDCs. We achieved these goals by collecting qualitative
interview data from a sample of community stakeholders and patients in Oregon. This study will help our
team plan future studies that test interventions that reduce and prevent NTDC-related ED use.
36 Part 2
Data
Location and Study Participants
We focused on 6 communities in Oregon State (5 rural and 1 urban). These communities had a history of
participating in research through the Oregon Rural Practice-based Research Network (ORPRN). From these
communities, we recruited a purposive sample of community stakeholders (N=34) and individuals with a
history of ED use for NTDCs (N=17) (Table 1). Community stakeholders were recruited through hospitals
and local dental societies. We used snowball techniques to identify additional stakeholders. The stakeholder
group included ED staf (physicians, nurses, and managers), hospital administrators, dental society leaders
and dentists, non-proft health program executives, and other relevant stakeholders. Patients were recruited
from hospitals and safety net dental clinics.
Data Collection
We generated preliminary 12-item interview scripts for stakeholders and ED utilizers. Cognitive interviewing
methods were used to pre-test the scripts with representative stakeholders and patients. The scripts were
modifed to improve clarity and fow. The scripts were used to train three interviewers. Study participants
were consented and received a $25 gift card as an incentive. Each interview was conducted in person or by
phone and digitally recorded. The study was approved by the University of Washington institutional review
board.
Data Management and Analyses
The digital data were transcribed by a professional medical transcription service. Each transcribed interview
was compared to the digital fle to ensure accuracy. A codebook was created that included three main
domains: 1) perceptions of NTDC-related ED use as a problem; 2) determinants of NTDC-related ED use;
and 3) potential solutions to reduce and prevent NTDC-related ED use. Stakeholder and patient data were
analyzed separately. For the stakeholder data, three trained Research Assistants coded a random sample
of three stakeholder transcripts to establish inter-coder agreement through subjective assessment, a
standard practice in qualitative methods. Discrepancies between the coders were discussed with a fourth
coder and resolved. The remaining 31 transcripts were divided among the three coders. Each transcript
was individually read and coded by two diferent coders using NVivo 8 qualitative data analysis software
(QSR International Pty Ltd, Victoria, Australia) to assign thematic codes to segments of the transcript text.
The two coded versions of each transcript were merged. An identical process was used to code the patient
transcripts. Based on the fndings, we generated a preliminary conceptual model of NTDC-related ED use.
37 Part 2
Main Findings
NTDC-Related ED Visits are a Problem
A number of ED health care providers and hospital administrators stated that NTDC-related ED visits were
not a problem. The main reason was the few number of patients presenting with NTDCs. It appears that
some hospital EDs see a low volume of NTDCs and less dental pain than we used to. However, there were
noted inconsistencies within communities. One potential reason is that EDs do not typically track the
number of NTDCs. In response to an ED health providers complaints about NTDCs, a regional medical center
CEO recently looked into how many dental charges I was doing and in one year discovered it was $750,000
out of a 25-bed hospitalthat was astounding. I had no ideaWe just hadnt noticed.
Other interviewees, including a community organizer, saw NTDC-related ED visits as a big problem.
One female ED patient reported that the ED physician who treated her commented on how there are more
and more people coming into the emergency room for teeth problems. A Registered Nurse with eight years
of clinical experience in the ED estimated that three to ten patients with NTDCs would present to the ED
each day. She commented that NTDCs can really screw up your fow of getting patients in and taking care
of them. An ED Director noted that triaged patients with NTDCs can cause problems in the waiting areas,
particularly when patients have been waiting for up to six hours. They become unhappy with the situation
and are vocal about it, so anybody else who is waiting [starts to develop] a negative overtone. With the
exception of occasional [drug] seekers in the ED who present with the excuse of dental pain but nothing
wrong in the mouth, patients with NTDCs really do have problems with their teeth.
All ED staf and local dentists agreed that care provided in the ED is non-defnitive, usually a combination
of administering a dental nerve block and prescribing analgesics and/or antibiotics. A number of patients
reported that a lot of times [the treating provider doesnt] wont even really look in your mouth and one
patient recalled her ED physician was annoyed at the fact that I was there for my teeth. ED clinicians
reported not having sufcient training, space, or equipment to treat NTDCs. While one ED clinic manager
stated that ED patients need to take responsibility for their own healthcare, which includes their dental
care, most ED staf were sympathetic. An ED Nurse Manager stated that it is a struggle to treat [patients
with NTDCs]you want to treat their pain. An ED physician admitted that we are not getting at the heart of
the issue, which leads to repeat ED visits over time by the same patient, also known as frequent fyers.
A young mother who reported visiting the ED two or three times for NTDCs commented that the ED staf
dont really know what theyre doing with teethor I dont think they really want to deal with itI think
they have more pressing matters. Another mother of two children, who recently went to the ED with an
NTDC as a last option, recalled that
Through the years, [dentists] have told me that [tooth decay] can fester into a bad infection and then it can actually
kill you. Soif you are that bad you need to go to the ER [emergency room]. But, then you get to the ER and they dont
know what to do. Okay, well give her something for pain, thats all we can do. They dont even refer you somewhere.
Just go to the dentist. Thats all they say. Thats pretty much going in circles. Going around and around. Its like I cant
[go to a dentist] cause I cant aford it.
The determinants of NTDC-related ED visits are multilevel and multifactorial
Health System
According to a patient who has utilized the ED multiple times in the past fve years, one reason for NTDC-
related ED visits is federal legislation that ensures access to emergency health care services regardless of an
individuals ability to pay. This retired, uninsured father of a 5-year old child said the person that needs the
help doesnt have money to pay for the [dental] care. The problem with the emergency room is that I know
38 Part 2
that if I have an emergency they have to give me care. They cant deny me. There is a law whether I have
money or not.
Stakeholders believed that a disjointed medical and dental care system prompted many patients to seek
care in the ED. It is not an integrated health solution. It [oral health] is a separate health issue. It is like your
mouth is somehowdiferentthan the rest of your body so I see it is as being treated separately...Dentistry
[is] an afterthought.
Interviewees specifcally raised problems with the Oregon Medicaid program, particularly in terms of dental
service coverage. A non-proft executive said that Medicaid in Oregon is a mirage beneft. A dental society
president who practices at a corporate dental clinic said you just get emergency. Thats it. They will not
cover fllings. Theyonly cover emergencies. A dental clinic coordinator stated that Medicaid will pay a
visit to a provider or to an ER for a dental-related problem, but not pay for the visit to the dentists ofce to
have that problem taken care of. Similarly, a general dentist working at a community health center stated
As soon as that emergency is treated, they wont cover other things which can help prevent the problems from
happening in the frst place.
A quote from an ED manager, who mistakenly believed that the Oregon Health Plan covered dental care for
adults, illustrates that some providers are confused about dental coverage and may blame the victim, the
patient who does not have access to dental care:
[most of] our patientsare on Medicaid. I dont think they understand that they have dental coverage, so some
of them have emergency dental coverage. Some of them have regular dental coverage where they can go and get
cleanings and things like this and I think they just are undereducated on what kind of coverage they have and who to
contact.
In the broader context of federal health care and state-level Medicaid reforms, a hospital director pointed
out that problems with dental provider shortages:
about 16,000 new patients [in my region]will be eligible for the Oregon Health PlanBefore it was just
emergency care for dental servicesand now [enrollees] will be eligible for exams, extractions, fllings, and cleanings
annually. So, whos going to be taking care of all these patients if you have a dentist shortage already and how are
the Dental Care Organizations preparing for that?...Who is going to care for them and how many dentists do we have
that we are going to be able to provide this coverage? Its a big job.
This hospital director went on to explain that dental insurance reform is not likely to completely eliminate
NTDC-related ED visits.
even with the Afordable Care Act and insurance exchanges, you aregoing to have a population of uninsured
people who will not qualify for coverage that are going to be coming to our emergency departments to get dental
needs metThere are going to be families who dont meet the eligibility requirementWe need to make certain we
are ready to handle that.
Community
There were three community-level factors stakeholders reported as being related to NTDC-related ED visits.
The frst was the absence of urgent care clinics. In one community, an ED charge nurse noted a lot that
could be treated at an urgent careend up coming to the emergency roomFrequently these patients
have no other alternative. However, an ED manager in another community believed that urgent care clinic
practices may lead to ED visits for NTDCs:
39 Part 2
I dont particularly like what we have done in our urgent care clinics because if you cant pay, you dont get seen, so
guess where they go, the ER, which is really dumb. Because the visit in urgent care is $100 and the visit in the ED is $600
and if you dont have your copay over there, they wont see you.
The second was insufcient dissemination of information about available resources in the community. A
general dentist who works part-time in a community dental clinic said
We see patients all the time at our clinic that dont know of our program. We have tried to get the word out in all the
emergency rooms, public health clinics, homeless sheltersbut still we hear of patients that dont know about [our
clinic] until they go to the emergency roomI would say that is key: getting the word out of what resources there are.
We dont turn people away because we cant see them.
The third was the absence of community water fuoridation. An ED physician and medical director has
observed that most ED patients do not live in areas with fuoridated waterIf you grow up without
fuoridated water, you are much more vulnerable to dental disease which put[s] you at risk of having
problems that would lead you to deciding to come to an emergency department.
Providers
Common reasons cited by patients for their ED visits were infexible dental ofce policies and referrals to
the ED by dentists. Patients reported that dentists are unavailable to provide emergency dental treatment
during evenings and weekends. In addition, emergency appointments with dental ofces were difcult
to schedule during business hours. A 28-year-old female described the process of turning to the ED after
attempting to seek care from her dentist:
They said they couldnt get me inif the pain is that bad and I [couldnt] wait [for] an appointment to go ahead [and]
go to the hospital.
Most dentists freely admitted that NTDC-related ED visits were a problem. A private practice dentist cited
overburdened dentists as a reason why patients end up in the ED:
There is a lack of OHP [Medicaid] providers in these communitiesThere are a few providers taking the lions share
of OHP, which overburdens themdoesnt allow for care to be delivered in a timely fashion andleads to patient
dissatisfaction, provider dissatisfaction[It] is a fairly broken system that limps along.
Dentists also cited potential legal liabilities associated with treating non-patients of record with NTDCs. A
private practice general dentist commented:
We have a lot of narcotic seekers, they shop from doctor to doctor, so you are very reticent in just giving narcotics over
the phone. You will send them to the emergency room because if we give narcotics, then it is our license that is at risk.
We have no history with the patient knowing if they are actually shopping for doctors and then we suddenly get hit as
giving out drugs. There goes your practice, youre dead in the water. So they do defensive dentistry and send them to
the emergency room because they have the liability coverage to be able to do that.
Patients
Social and economic disadvantage were common reasons cited for why individuals present to the ED
with NTDCs. A common observation was that ED utilizers have no alternatives. A physician and medical
ofcer at a Coordinated Care Organization commented that NTDC-related ED utilizers are more likely to be
impoverishedWe are seeing an increased rate of dental caries in the lower socioeconomic range.
An executive at a non-proft health collaborative described fndings from a recent community health survey
she administered that asked about social determinants of health and fnancing issues, do you have enough
money for housing, do you have enough money for food, do you have problems with transportation, do you
40 Part 2
have someone to talk to, do you have literacy issues? The number one issue by a long shot was not having
enough money to pay for a dentist. She went onto to say that vulnerable individuals have high, high, high
stress in their liveson a chronic basis.
Health-related culture and values were also mentioned as patient-level factors related to ED visits. A nurse
manager observed that people who have been on Medicaid for years and years and years, they just
use the ER. It is the easiest to thing to do. I can go anytime I want. I dont have to have an appointment.
Another nurse manager similarly noted that ED utilizers are not forward thinking. They dont try and make
appointments. They are not engaged in their own care and so they come to the ER because it is an easy, fast
thing to do. It doesnt require any accountability, making an appointment, follow-up, anything. A general
dentist attributed it to lack of responsibility.
Other themes were oral health-related behaviors, including symptom-driven dental care use, inconsistent
visits to the dentist, lack of oral hygiene, and poor diet. One patient who went to the ED after breaking her
tooth on a Friday night stated that I dont really feel the need [to seek regular dental care]although I think
if I was fush with cash, I wouldnt be going to the dentist necessarily. Its not one of my habitsIm the type
that I tend to not go unlessI had no option. Many believed these behaviors lead to repeat ED visits for
NTDCs. I think part of that is if they get antibiotics and pain medication, their symptoms resolve temporarily
and they think they are fne. An ED nurse manager echoed these observations: You seefrequent fyers
that come in over and over and over with dental problemsWe are treating their infection and treating
their pain and then once the infection is better, they dont have pain anymore, but then its going to come
back down the roadWe call back all of our patientspost visitand very frequently [we] ask Were you
able to make a follow-up appointment? They dont have the money for it. They are not following up.
Interviewees mentioned a number of possible reasons for lack of follow up and symptom-driven dental
care use. The frst is the lack of a dental home. An ED physician and hospital medical director noted that
the majority of patients who present to the emergency department for non-traumatic dental emergencies
do not have an established relationship with a dentist. One ED patient explained the diference between
a place to go for emergency care versus a dental home. With the health department [as a place to go for
dental care], I mean it helps, its cheap, but you dont have an actual doctor. Hes not your doctorand I just
wanted to get everything done from a real dentist [versus a diferent dentist each time].
The second is dental fears. A young female dentist in private practice explained that A lot of people have a
really substantial amount of fearof the unknown. Fear of if look you are going to fnd something and I just
dont want to acknowledge its there. Fear of pain, especially people who have a history of drug useseem
to besensitized to any kind of pain like a toothache or a needle. A number of patients confrmed these
observations. A young male cancer survivor admitted being really, really deathly scared of the dentist and a
young female acknowledged emotionally Im scared of the dentistI have not had very good experiences
at the dentist. They are rough.
Other reasons included not being able to take time of from work, lack of transportation, and no money or
insurance. ED clinicians mentioned drug seeking as a common reason for ED visits for NTDCs.
41 Part 2
Selected Patient Narratives
Patient 1
I want to eat without feeling pain in my mouth. There are some times it hurts so bad I develop like a constant migraine
and stuf and it just kills meI was just in such pain, I kind of wasnt even thinking right. I actually took of walking [to
the ED] because I couldnt fnd a ride. I was hurting that bad and I hitchhiked, somebody picked me up and took me
there and actually brought me back
Patient 2
It was giving me such excruciating pain that I decided the emergency room would be next best place to go and they
basically told me you need to see a dentist. It was kind of playing tag.
Patient 3
I cant [go to the dentist] because I cant aford it. With a job or without, I cant aford it. Dont get me wrong, I love my
smile, I like to smile and when I dont have a smile, who would want to get a job, who would want to hire you, because
you have bad teeth. You dont have that confdence anymore because your teeth are bad and that is a problem, too. I
have seen it.
Patient 4
[Going to the ED] did not solve [my dental problem]. [Afterwards, the pain] would always come back, sometimes even
worse and I would have to go to the dentist. I would have to borrow and save and collect cans whatever I had to do
to get the money to get my dental work done. But the more I get done, the more cavities come and the more issues
happenI have been sufering and I dont like pain. Pain is just too much, overwhelming. I am not going to pull all my
teeth and walk around with nothing in my mouth. I just cant see myself doing that. So I want to keep them as long as
I possibly can. I just cant see myself walking around like most people Ive seen with no teeth. They smile and its like,
wow. Some people wont even smile or they will turn their head and talk, no confdence. It is just sad and I dont want
to be like that.
Patient 5
INTERVIEWER: How you do decide to go to the emergency room with a dental problem?
Basically, if I cant make it through the pain until the nerve burns out, then I will try to acquire antibiotics on the street
and deal with it that way. Or, if I know a friend that has one or something like that. I know, youre not supposed to,
but it seems to work. Another trick is I can go to the coop and buy Terramycin for animals and you can take that for
yourself. Put it in caplets. It says not for human consumption, but it seems to work.
INTERVIEWER: What does the Terramycin do, is it a painkiller?
PATIENT: No, its an antibiotic for horses. If you live on a farm and you raise animals, you know it.
INTERVIEWER: Why dont you go to the dentist?
PATIENT: Money, plain and simple. Plain and simple reason, money. I have a 5-year-old daughter that Ive got to take
care of and other bills to pay and survive. It is hard enough to if the pain is so bad that I have to come up with it,
then I will come up with it. Maybe one month, I might not pay the power billso I can go to the dentist, but the next
month I have to pay it of or go on a payment plan. It all depends on how it goes. Hand to mouth. Feast or famine.
PATIENT: If I went [to the ED] with a knife in my back and they said, well heres some painkillers and some antibiotics,
go see your doctor on Monday to take the knife out of your back, I might get a little concerned. Although it is [what]
they do with teeth really. It is obviously broken. It is obviously a problem. Come on.
42 Part 2
Stakeholders ofered potential solutions to reduce ED use for NTDCs, many of which are un-
likely to systematically solve the problem
Interviewees suggested a number of possible solutions that could help to reduce NTDC-related ED visits.
While not all of these may be efective, some of them merit further consideration.
Health system
Assignment of a Primary Dental Care Provider to Medicaid enrollees
Assignment of a Dental Case Worker for Medicaid enrollees
case workers [could] call them [and ask] did you make your appointment? Did you go? You cant go, you need a
ride, I will come get you and take you.
Electronic Beneft Transfer for dental care
if you give [patients with NTDCs] money, they are going to spend it on other things than their teeth. Giving them
money to fx their teeth wont work. Maybe something along the lines of the Oregon Trail Card except it is only for
dental work. Everybodywould try to fnd a way to get around this. They even tried to do it with Oregon Trail Card.
They will try to trade the Oregon Trail Card50 cents on the dollar. It used to be with food stamps they would do that.
The black market creates avenues for everything. There is not going to be a way for you to take an Oregon Dental Card
into a dentist and say you are somebody diferent to get teeth work. It would be impossible to defraud that card. The
biggest problem with anything the government gives us, like money or food stamps or benefts or anything like that is
that they fnd a way to exploit it and trade it for drugs or stuf on the street. The biggest challenge is to prevent that.
Make dental services available in urgent care clinics
NTDCs are an urgent care problemnot an emergency department problem.
There is this mental thing of, if I go to the ED, its free. I dont particularly like what we have done in our
urgent care clinics because if you cant pay, you dont get seen, so guess where they go, the ER. Because the
visit in urgent care is $100 and the visit in the ED is $600 and if you dont have your copay over there, they
wont see you. It is like we are ofoading the nonpaying participants to the highest level of care which is
really silly.
Development of appropriate dental clinic policies on after-hour dental emergencies
Providers
Train more dentists
Open mode dental clinics, including urgent care clinics
Continuing education for ED staf
Increase availability of dentist-on-call within ED
Enhance ED-to-dental-ofce referral system
Patients
Improve patient oral health-related behaviors, including hygiene and diet.
43 Part 2
Preliminary Conceptual Model On NTDC-Related ED Use
Based on the data provided by stakeholders and patients, we developed a preliminary conceptual model
that describes initial and repeat ED use for NTDCs, both of which future interventions will need to prevent
and reduce (Figure 1).
The model incorporates health system and community factors as important contextual infuences on the
triangulated relationship between patients, dentists, and the ED.
Initially (at time 0), patients may seek care from a dentist for NTDCs. However, various barriers to dental care
exist. Dental ofces do not provide care after hours or may not be able to schedule emergency patients
during the day. As a result, dentists refer patients with NTDCs to the ED. While ED care may be free to
patients, the ED is equipped to provide only palliative care, which temporarily addresses acute symptoms
associated with NTDCs. ED clinicians refer patients to a dentist, but barriers to dental care have not been
eliminated. Subsequently (at time 1), patients come to rely on the ED for palliative care, leading to repeat ED
use for NTDCs.
Various intervention points exist at the health system, community, provider, and patient levels.
44 Part 2
Policy Recommendations
Based on fndings from Aim 1 and the potential solutions proposed by stakeholders in Aim 2, we draw the
following multilevel policy recommendations that we believe will systematically reduce and prevent ED use
for NTDCs.
Target Population
Medicaid enrollees are at high risk for NTDC-related ED use
NTDC-related ED use is primarily a problem of young adults ages 20 and 30, which means that all of
these individuals were likely to have treatable dental disease during adolescence
Medicaid-enrolled adolescents have comprehensive dental benefts, which ofers an opportunity to
target these high risk individuals, treat disease, and reinforce oral health behaviors (toothbrushing with
fuoride toothpaste, healthy diet, regular visits to the dentist) that prevent NTDC-related ED use later
in life.
Multilevel Solutions
Develop a statewide surveillance system focusing on adolescents (Smile Survey) and implement metrics
to track progress within this high-risk population
Assemble community planning groups consisting of adolescents to help develop feasible interventions
aimed at adolescent oral health promotion
Use the current Medicaid system and work with school nurses within junior and senior high schools to
identify and refer adolescents with dental disease and treatment needs
Reinforce primary care dental providers and case management for adolescents in Medicaid
Educate community about changes in the Oregon Health Plan (Medicaid) and dental benefts
Distribute free toothpaste and reduce availability of sugar sweetened beverages within schools (pouring
rights)
Develop community-based strategies to promote and protect community water fuoridation
Additional Solutions
Encourage interprofessional collaborations between dentists and pharmacists and implement oral
health education interventions within pharmacies, which patients who require prescription medications
will visit
Use denturists to provide removable prosthodontic care (partial dentures) for patient requiring tooth
extractions
Provide continuing education courses for dentists on appropriate management of NTDCs to take
advantage of chemotherapeutic management of dental disease including topical fuoride, povidone
iodine, and diammine silver fuoride.
Deliver continuing education courses for ED staf on appropriate prescribing of antibiotics to reduce
costs to Medicaid
45 Part 2
Conclusions
There was agreement among interviewed stakeholders and patients that the ED does not have the trained
stafs, equipment, or space to deliver defnitive dental care. As a result, EDs are only able to provide palliative
care (e.g., antibiotics, analgesics). Patients described overwhelming social, economic, and behavioral barriers
to preventive and restorative dental care that might help to prevent NTDCs and use of the ED, including
repeat ED visits for unresolved NTDCs.
The determinants of ED use for NTDCs are multilevel and multifactorial. Future strategies aimed at reducing
and preventing NTDC-related ED use will require systematic multilevel interventions that focus on high risk
adolescents. Such interventions will need to modify patient oral health-related behaviors, involve medical
and dental care providers, incorporate community-level solutions like water fuoridation, and reform existing
programs and policies aimed at vulnerable populations, including Medicaid.
46 Part 2
AIM 2 Study Team
University of Washington
Donald L. Chi, DDS, PhD, Principal Investigator
Peter Milgrom, DDS, Co-Investigator
Erin Masterson, MPH, Lead Data Analyst
Christopher Shyue, BA, Data Analyst
Hilary Chen, BS, Data Analyst
Zoljargal Bayarsaikhan, Data Analyst
Oregon Rural Practice-based Research Network (ORPRN)
Sankirtana Danner, MFT, Lead Research Coordinator
Jillian Currey, MPH, CCRP, Research Coordinator
Molly DeSordi, BS, Research Coordinator
Mark Remiker, MA, Research Coordinator
47 Part 2
References
1. Chi DL, Masterson EE, Wong J. Emergency department use for non-traumatic dental conditions for
individuals with intellectual and developmental disabilities. Intellect Dev Disabil. 2014. Accepted for
publication.
2. Hong L, Ahmed A, McCunnif M, Liu Y, Cai J, Hof G. Secular trends in hospital emergency department
visits for dental care in Kansas City, Missouri, 20012006. Public Health Rep. 2011 MarApr;126(2):2109.
3. Lee HH, Lewis CW, Saltzman B, Starks H. Visiting the emergency department for dental problems: trends
in utilization, 2001 to 2008. Am J Public Health. 2012 Nov;102(11):e7783.
4. Okunseri C, Okunseri E, Thorpe JM, Xiang Q, Szabo A. Patient characteristics and trends in nontraumatic
dental condition visits to emergency departments in the United States. Clin Cosmet Investig Dent. 2012
Jan 16;4:17.
5. Okunseri C, Pajewski NM, Brousseau DC, Tomany-Korman S, Snyder A, Flores G. Racial and ethnic
disparities in nontraumatic dental-condition visits to emergency departments and physician ofces:
a study of the Wisconsin Medicaid program. J Am Dent Assoc. 2008 Dec;139(12):165766.
Vous aimerez peut-être aussi
- NDA Luminese. FDADocument40 pagesNDA Luminese. FDAJoaquim Fernandez PerezPas encore d'évaluation
- Professional, Structural and Organisational Interventions in Primary Care For Reducing Medication ErrorsDocument147 pagesProfessional, Structural and Organisational Interventions in Primary Care For Reducing Medication ErrorsGurgehPas encore d'évaluation
- Breach of Duty of Care in Medical Negligence: Scope and LimitationDocument55 pagesBreach of Duty of Care in Medical Negligence: Scope and LimitationNaina Mathew100% (1)
- NTP Monograph: Health Effects of Low-Level LeadDocument176 pagesNTP Monograph: Health Effects of Low-Level LeadExpert assessoriaPas encore d'évaluation
- Wikipedia Handbook of Biomedical InformaticsDocument709 pagesWikipedia Handbook of Biomedical InformaticsMonark Huny100% (1)
- Interventions For Dissociated Vertical Deviation (Review) : CochraneDocument37 pagesInterventions For Dissociated Vertical Deviation (Review) : CochraneMacarena AlvarezPas encore d'évaluation
- deGruyter-Medical Errors and Patient SafetyDocument128 pagesdeGruyter-Medical Errors and Patient SafetySPas encore d'évaluation
- Final Report - Jyotish GogoiDocument45 pagesFinal Report - Jyotish GogoiRajat SinghPas encore d'évaluation
- Framework For HR ADocument52 pagesFramework For HR AHS RattiPas encore d'évaluation
- Primary Health Care Systems (Primasys) : Case Study From NigeriaDocument44 pagesPrimary Health Care Systems (Primasys) : Case Study From NigeriaDapo OrimoloyePas encore d'évaluation
- Retention of The Health Workforce in Rural and Remote Areas: A Systematic ReviewDocument37 pagesRetention of The Health Workforce in Rural and Remote Areas: A Systematic ReviewChandra ArhaPas encore d'évaluation
- Lateral PositionDocument162 pagesLateral PositionParli HarunPas encore d'évaluation
- Primary Health Care Systems (Primasys) : Case Study From GeorgiaDocument44 pagesPrimary Health Care Systems (Primasys) : Case Study From GeorgiaTengiz VerulavaPas encore d'évaluation
- Gizat's Final ResearchDocument40 pagesGizat's Final ResearchGizat FelekePas encore d'évaluation
- THCU - SituationalAssesmentToolsDocument273 pagesTHCU - SituationalAssesmentToolsdhernández_gualdrónPas encore d'évaluation
- State of Inequality - Reproductive Maternal Newborn and Child HealthDocument124 pagesState of Inequality - Reproductive Maternal Newborn and Child HealthDiana Alexa ForeroPas encore d'évaluation
- Hospital Survey On Patient Safety Culture User'S GuideDocument41 pagesHospital Survey On Patient Safety Culture User'S GuideanggaPas encore d'évaluation
- MAAVN001 Final KAP Report DF CC 0611Document35 pagesMAAVN001 Final KAP Report DF CC 0611Baleegh Al-sharabyPas encore d'évaluation
- Mekonnen Gizachew PDFDocument60 pagesMekonnen Gizachew PDFkelid IbrahimPas encore d'évaluation
- IARC Monograph On EMF Radiation - No 102Document480 pagesIARC Monograph On EMF Radiation - No 102mvannierPas encore d'évaluation
- CDC Growth ChartsDocument203 pagesCDC Growth ChartsLindsey KathleenPas encore d'évaluation
- Who His HSR 17.27 EngDocument40 pagesWho His HSR 17.27 EngAkampurira IanPas encore d'évaluation
- Lower Folate Levels in Schizophrenia Meta-AnalysisDocument7 pagesLower Folate Levels in Schizophrenia Meta-AnalysisRuy AntonucciPas encore d'évaluation
- MHSOS Complete Chapter One Instructor's Sneak PeekDocument159 pagesMHSOS Complete Chapter One Instructor's Sneak PeekHealth Professions Press, an imprint of Paul H. Brookes Publishing Co., Inc.93% (15)
- FPSA Myanmar 2018Document45 pagesFPSA Myanmar 2018Min Zaw Thein Thein MoePas encore d'évaluation
- Diarrhoea Global ReviewDocument61 pagesDiarrhoea Global ReviewHusnainPas encore d'évaluation
- Cosm reportDocument92 pagesCosm reportrandomaeiou7273Pas encore d'évaluation
- Guias Aorta 2019 PDFDocument97 pagesGuias Aorta 2019 PDFRomeo GuevaraPas encore d'évaluation
- Research For Emergency Medicine Residents 3rd EditionDocument110 pagesResearch For Emergency Medicine Residents 3rd Editionsmith.kevin1420344Pas encore d'évaluation
- Local Production and Access To Medicines in Low-And Middle-Income CountriesDocument56 pagesLocal Production and Access To Medicines in Low-And Middle-Income CountriesMUHAMMAD SAQIB SHABBIR UnknownPas encore d'évaluation
- KHWF 2017report Fullreport 042317-MR-commentsDocument104 pagesKHWF 2017report Fullreport 042317-MR-commentsh3493061100% (1)
- Herling Et Al-2018-Cochrane Database of Systematic ReviewsDocument104 pagesHerling Et Al-2018-Cochrane Database of Systematic ReviewsRodrigoSachiFreitasPas encore d'évaluation
- Cochrane RC CoronariosDocument211 pagesCochrane RC CoronariosRenzo RosalesPas encore d'évaluation
- CD012669 PDFDocument156 pagesCD012669 PDFnoviPas encore d'évaluation
- Sexually Transmitted InfectionsDocument336 pagesSexually Transmitted Infectionsfalih1959100% (1)
- Uplift GuideDocument239 pagesUplift GuideDr. FaizanPas encore d'évaluation
- Aftryp SWG PDFDocument182 pagesAftryp SWG PDFij EducationPas encore d'évaluation
- Early Versus Delayed Post-Operative Bathing or Showering To Prevent Wound ComplicationsDocument25 pagesEarly Versus Delayed Post-Operative Bathing or Showering To Prevent Wound ComplicationsagusPas encore d'évaluation
- Patterns and Correlates of Anabolic-Androgenic Steroid UseDocument112 pagesPatterns and Correlates of Anabolic-Androgenic Steroid Useshubhashish sharmaPas encore d'évaluation
- Zambia's 2017-2021 National Health Strategic PlanDocument127 pagesZambia's 2017-2021 National Health Strategic PlanNg'andu Kayunna DavidPas encore d'évaluation
- The benefits of personalised medicineDocument72 pagesThe benefits of personalised medicineAnuradha Monga KapoorPas encore d'évaluation
- Nchs PDFDocument201 pagesNchs PDFDyah Ajeng PratiwiPas encore d'évaluation
- Mobile Phone Messaging For Facilitating Self-Management of Long-Term Illnesses (Review)Document52 pagesMobile Phone Messaging For Facilitating Self-Management of Long-Term Illnesses (Review)José Carlos Sánchez-RamirezPas encore d'évaluation
- Cochrane Database of Systematic Reviews (Reviews) || -- Hing, Caroline B -- 2011Document45 pagesCochrane Database of Systematic Reviews (Reviews) || -- Hing, Caroline B -- 2011lite.trawler-0xPas encore d'évaluation
- WHO FGM GuidelinesDocument64 pagesWHO FGM GuidelinesMuhammmed abdi wahaabPas encore d'évaluation
- Primary Health Care Systems PRIMASYS - ThailandDocument36 pagesPrimary Health Care Systems PRIMASYS - ThailandheryantomardiPas encore d'évaluation
- J Jenvman 2015 08 013Document11 pagesJ Jenvman 2015 08 013Al MamunPas encore d'évaluation
- CD006966Document49 pagesCD006966felaxis fPas encore d'évaluation
- ESVS 2020 guidelines on management of vascular graft and stent graft infectionsDocument46 pagesESVS 2020 guidelines on management of vascular graft and stent graft infectionsGhaithPas encore d'évaluation
- Cost Analysis of Services at Victoria Hospital St. LuciaDocument41 pagesCost Analysis of Services at Victoria Hospital St. LuciaAdelPas encore d'évaluation
- Veterinary Clinical Epidemiology, From Patient To Population, 4th Edition (VetBooks - Ir)Document273 pagesVeterinary Clinical Epidemiology, From Patient To Population, 4th Edition (VetBooks - Ir)Stephany Claros0% (1)
- HIO Medical Audit Guidelines For Primary Health Care Clinics and Hospital OjoDocument126 pagesHIO Medical Audit Guidelines For Primary Health Care Clinics and Hospital OjojhonronPas encore d'évaluation
- APIC Ortho Guide BookDocument80 pagesAPIC Ortho Guide Bookmattpiano535Pas encore d'évaluation
- BC's Provincial Strategy for Anxiety DisordersDocument61 pagesBC's Provincial Strategy for Anxiety Disordersjdulmage77Pas encore d'évaluation
- White Paper: On Joint ReplacementDocument144 pagesWhite Paper: On Joint ReplacementCosme MejiaPas encore d'évaluation
- Alcohol and Drug Services Study (ADSS) The National Substance Abuse Treatment System: Facilities, Clients, Services, and StaffingDocument169 pagesAlcohol and Drug Services Study (ADSS) The National Substance Abuse Treatment System: Facilities, Clients, Services, and StaffinglosangelesPas encore d'évaluation
- Primary Clinic StandardsDocument50 pagesPrimary Clinic StandardsBelay TadessePas encore d'évaluation
- Animal and Translational Models for CNS Drug Discovery: Reward Deficit DisordersD'EverandAnimal and Translational Models for CNS Drug Discovery: Reward Deficit DisordersRobert A. McArthurPas encore d'évaluation
- Letter To Judge Hernandez From Rural Oregon LawmakersDocument4 pagesLetter To Judge Hernandez From Rural Oregon LawmakersStatesman JournalPas encore d'évaluation
- Cedar Creek Fire Soil Burn SeverityDocument1 pageCedar Creek Fire Soil Burn SeverityStatesman JournalPas encore d'évaluation
- Roads and Trails of Cascade HeadDocument1 pageRoads and Trails of Cascade HeadStatesman JournalPas encore d'évaluation
- Cedar Creek Fire Sept. 3Document1 pageCedar Creek Fire Sept. 3Statesman JournalPas encore d'évaluation
- Complaint Summary Memo To Superintendent Re 8-9 BD Meeting - CB 9-14-22Document4 pagesComplaint Summary Memo To Superintendent Re 8-9 BD Meeting - CB 9-14-22Statesman JournalPas encore d'évaluation
- Cedar Creek Vegitation Burn SeverityDocument1 pageCedar Creek Vegitation Burn SeverityStatesman JournalPas encore d'évaluation
- School Board Zones Map 2021Document1 pageSchool Board Zones Map 2021Statesman JournalPas encore d'évaluation
- Mount Hood National Forest Map of Closed and Open RoadsDocument1 pageMount Hood National Forest Map of Closed and Open RoadsStatesman JournalPas encore d'évaluation
- Salem Police 15-Year Crime Trends 2007 - 2015Document10 pagesSalem Police 15-Year Crime Trends 2007 - 2015Statesman JournalPas encore d'évaluation
- Windigo Fire ClosureDocument1 pageWindigo Fire ClosureStatesman JournalPas encore d'évaluation
- Matthieu Lake Map and CampsitesDocument1 pageMatthieu Lake Map and CampsitesStatesman JournalPas encore d'évaluation
- Salem Police 15-Year Crime Trends 2007 - 2021Document10 pagesSalem Police 15-Year Crime Trends 2007 - 2021Statesman JournalPas encore d'évaluation
- Revised Closure of The Beachie/Lionshead FiresDocument4 pagesRevised Closure of The Beachie/Lionshead FiresStatesman JournalPas encore d'évaluation
- Cedar Creek Fire Aug. 16Document1 pageCedar Creek Fire Aug. 16Statesman JournalPas encore d'évaluation
- Social-Emotional & Behavioral Health Supports: Timeline Additional StaffDocument1 pageSocial-Emotional & Behavioral Health Supports: Timeline Additional StaffStatesman JournalPas encore d'évaluation
- Salem Police Intelligence Support Unit 15-Year Crime TrendsDocument11 pagesSalem Police Intelligence Support Unit 15-Year Crime TrendsStatesman JournalPas encore d'évaluation
- LGBTQ Proclaimation 2022Document1 pageLGBTQ Proclaimation 2022Statesman JournalPas encore d'évaluation
- BG 7-Governing StyleDocument2 pagesBG 7-Governing StyleStatesman JournalPas encore d'évaluation
- Oregon Annual Report Card 2020-21Document71 pagesOregon Annual Report Card 2020-21Statesman JournalPas encore d'évaluation
- WSD Retention Campaign Resolution - 2022Document1 pageWSD Retention Campaign Resolution - 2022Statesman JournalPas encore d'évaluation
- Proclamation Parent & Guardian Engagement in Education 1-11-22 Final, SignedDocument1 pageProclamation Parent & Guardian Engagement in Education 1-11-22 Final, SignedStatesman JournalPas encore d'évaluation
- SIA Report 2022 - 21Document10 pagesSIA Report 2022 - 21Statesman JournalPas encore d'évaluation
- All Neighborhoods 22X34Document1 pageAll Neighborhoods 22X34Statesman JournalPas encore d'évaluation
- Salem-Keizer Parent and Guardian Engagement in Education Month ProclamationDocument1 pageSalem-Keizer Parent and Guardian Engagement in Education Month ProclamationStatesman JournalPas encore d'évaluation
- Failed Tax Abatement ProposalDocument8 pagesFailed Tax Abatement ProposalStatesman JournalPas encore d'évaluation
- Salem-Keizer Discipline Data Dec. 2021Document13 pagesSalem-Keizer Discipline Data Dec. 2021Statesman JournalPas encore d'évaluation
- All Neighborhoods 22X34Document1 pageAll Neighborhoods 22X34Statesman JournalPas encore d'évaluation
- SB Presentation SIA 2020-21 Annual Report 11-9-21Document11 pagesSB Presentation SIA 2020-21 Annual Report 11-9-21Statesman JournalPas encore d'évaluation
- Zone Alternates 2Document2 pagesZone Alternates 2Statesman JournalPas encore d'évaluation
- Crib Midget Day Care Emergency Order of SuspensionDocument6 pagesCrib Midget Day Care Emergency Order of SuspensionStatesman JournalPas encore d'évaluation
- Installation and Operating Instructions Gen-Key: Energy DivisionDocument22 pagesInstallation and Operating Instructions Gen-Key: Energy DivisionAnonymous RcxX0FcPas encore d'évaluation
- Cpar Lesson 1Document44 pagesCpar Lesson 1althea villanuevaPas encore d'évaluation
- DP4XXX PricesDocument78 pagesDP4XXX PricesWassim KaissouniPas encore d'évaluation
- CH06 Binding MaterialsDocument114 pagesCH06 Binding MaterialsAbass AwalehPas encore d'évaluation
- She Walks in BeautyDocument6 pagesShe Walks in Beautyksdnc100% (1)
- Instruction Manual for Capacitor Voltage TransformersDocument22 pagesInstruction Manual for Capacitor Voltage Transformerst.o.i.n.gPas encore d'évaluation
- A P1qneer 1n Neuroscience: Rita Levi-MontalciniDocument43 pagesA P1qneer 1n Neuroscience: Rita Levi-MontalciniAntPas encore d'évaluation
- Business Research Chapter 1Document27 pagesBusiness Research Chapter 1Toto H. Ali100% (2)
- Best Practice Guidelines For Cardiac Rehabilitation and Secondary Prevention: A SynopsisDocument16 pagesBest Practice Guidelines For Cardiac Rehabilitation and Secondary Prevention: A SynopsisErdy VincentPas encore d'évaluation
- TK17 V10 ReadmeDocument72 pagesTK17 V10 ReadmePaula PérezPas encore d'évaluation
- Comparing Means of Two GroupsDocument8 pagesComparing Means of Two GroupsRobert Kier Tanquerido TomaroPas encore d'évaluation
- LAC and Location UpdateDocument10 pagesLAC and Location UpdateAndres RockePas encore d'évaluation
- (Homebrew) ShamanDocument15 pages(Homebrew) ShamanVictor Wanderley CorrêaPas encore d'évaluation
- Excel File - Business Computing - End Term (To Be Shared Vide Email)Document301 pagesExcel File - Business Computing - End Term (To Be Shared Vide Email)Aman SankrityayanPas encore d'évaluation
- Useful List of Responsive Navigation and Menu Patterns - UI Patterns - GibbonDocument16 pagesUseful List of Responsive Navigation and Menu Patterns - UI Patterns - Gibbonevandrix0% (1)
- Emg 1204 Introduction To Materials Science Tutorial I Attempt All These Questions Question OneDocument2 pagesEmg 1204 Introduction To Materials Science Tutorial I Attempt All These Questions Question Onesteve gateriPas encore d'évaluation
- Pamantasan NG Lungsod NG Maynila - Freshmen AdmissionDocument6 pagesPamantasan NG Lungsod NG Maynila - Freshmen AdmissionPoppy HowellPas encore d'évaluation
- KoL Mekflu - 9Document104 pagesKoL Mekflu - 9Maha D NugrohoPas encore d'évaluation
- Lala Hardayal - BiographyDocument6 pagesLala Hardayal - Biographyamarsingh1001Pas encore d'évaluation
- Total Cost of Ownership in PV Manufacturing - GuideDocument12 pagesTotal Cost of Ownership in PV Manufacturing - GuidebirlainPas encore d'évaluation
- Dslam Commissioning Steps Punjab For 960 PortDocument8 pagesDslam Commissioning Steps Punjab For 960 Portanl_bhn100% (1)
- Sample Problems Part FormDocument4 pagesSample Problems Part FormkenivanabejuelaPas encore d'évaluation
- Tauros TBM Guidance SystemDocument3 pagesTauros TBM Guidance SystemMiloš StanimirovićPas encore d'évaluation
- Tie Technology DK SKDocument32 pagesTie Technology DK SKVladimir PleșcaPas encore d'évaluation
- Gulliver's Travels Misogyny or MisanthropyDocument3 pagesGulliver's Travels Misogyny or MisanthropyKingshuk MondalPas encore d'évaluation
- 1st Activity in ACCA104Document11 pages1st Activity in ACCA104John Rey BonitPas encore d'évaluation
- The 5th Edition of The World Health Organization Classification - of Haematolymphoid Tumours Myeloid and Histiocytic - Dendritic NeoplasmsDocument17 pagesThe 5th Edition of The World Health Organization Classification - of Haematolymphoid Tumours Myeloid and Histiocytic - Dendritic NeoplasmsADMINISTRACION LABORATORIO INTERMEDICAPas encore d'évaluation
- Tiotropium Bromide: Spiriva Handihaler, Spiriva RespimatDocument9 pagesTiotropium Bromide: Spiriva Handihaler, Spiriva RespimatAssem Ashraf KhidhrPas encore d'évaluation
- Anuj Singh ResumeDocument4 pagesAnuj Singh ResumeAnuj BaghelPas encore d'évaluation
- RTL8185 Windows7 FixDocument2 pagesRTL8185 Windows7 FixJamesHackPas encore d'évaluation