Académique Documents
Professionnel Documents
Culture Documents
1st Adime - HW
Transféré par
api-243208495Titre original
Copyright
Formats disponibles
Partager ce document
Partager ou intégrer le document
Avez-vous trouvé ce document utile ?
Ce contenu est-il inapproprié ?
Signaler ce documentDroits d'auteur :
Formats disponibles
1st Adime - HW
Transféré par
api-243208495Droits d'auteur :
Formats disponibles
Students Name: Laryssa Grguric Patient/Clients Initials: W.H.
Date: 02/04/14
ASSESSMENT:
S: Pt. Went to ED of NUMC after experiencing blurry vision during the Super Bowl game. Pt. had
previously weaned himself off of insulin and was insulin free x1 year (primary MD aware per pt.) Due
to blurry vision, pt. checked his FSBG and monitor registered ~500 mg/dL. Pt. then used leftover insulin
and gave himself 10U of insulin to attempt to lower blood sugar so he could finish watching the game. BG
did not improve even though he only ate salad after administering insulin. Pt. also experienced nausea &
vomitting PTA but it has since subsided. Pt reports his UBW is within the 140s.
O: 45 y/o ! c " admitting Dx of hyperglycemia. Ht. 74 Wt. 108.6 kg/239# BMI 31.1 kg/m
2
. Previous
admission wt (11/2011): 267#. PMH TIA x 2, HTN, DM type 2, dyslipidemia, GERD. Biochemical data
assessment shows ! FSBG 2/2: >600 (admission), 2/4: 336, 116, 317, ! chol 240, !TG 285, " HDL 32,
!LDL 156. Hemoglobin A1c 11.1%.
Ht. Current Wt UBW/%UBW IBW range /%IBW BMI
74 239# (2/2) 240s/100% 158.4-193.6#/136% 30.7
Estimated energy needs (note equation used):
Adj BW= 199.9#
MSJ 2 to obesity (BMI 31.1) using Adj BW, SF 1.2-1.3:
2224-2409 kcal/day
Estimated protein needs (note g/kg):
1.0-1.2 g/kg
31.1-37.32 g/day
Other nutrient needs: N/A Fluid needs: 35-40 mL/kg
1088.5-1244 mL/day
Diet History (24 recall):
Diet hx obtained in hospital:
Dinner: ~50% vegetable soup, 75% jerk chicken, 100% mashed potato c " gravy, 0% collard greens (due to
GERD sx), 100% pound cake dessert
Breakfast: 1 apple, 100% grits, 1 hardboiled egg pt. reported being hungry after breakfast.
Lunch (observed at bedside): ~50% split pea soup, ~50% lasagna (due to pasta sauce causing GERD Sx),
0% spinach (due to GERD Sx), 100% pineapple fruit cup
Evaluation of Diet History (brief, e.g., limited in calcium and vitamin D, consumes ! amount of sugar, etc.)
Pt. avoids foods that can cause GERD sx (obtained prefs related to GERD and relayed information to
kitchen).
PTA pt. reports following a regular diet but told me he watches his diet to control BG (does not want to
be on insulin) may be contradictive statement. Pt. is aware of DM diet and has received prior education
but speaking with pt. it appears DM diet is followed loosely.
Pt. reports adding extra fruit and avoiding sweets/soda in his diet. Pt. also chooses to bake foods vs. fry.
Recall of "usual" foods reveal a lot of carbohydrate rich foods such as breads, pasta, starchy vegetables, etc.
Pt. did not seem aware of portion control when discussed.
Physical Activity (describe patients physical activity): Low active; pt. reports wt. gain s/p TIA but he is
slowly increasing activity
Diet Order:
Intake approximately 75% at meals / observed at lunch, per pt.
Pertinent lab values (Date, # or $; why you think it may be high or low)
! FSBG 2/2: >600 (admission), 2/4: 336, 116, 317, ! chol 240, !TG 285, " HDL 32, !LDL 156.
Hemoglobin A1c 11.1%.
2/3: BUN 10 WNL, Creat 0.8 WNL
FSBG & A1c reveals uncontrolled DM possibly 2 to d/c insulin & metformin and non-compliance to DM
diet.
TG levels may be related to uncontrolled DM, chol (HDL, LDL) may be related to
Nutritional Risk Factors (GI, chewing/swallowing difficulties, etc.)
N/A; pt. has good appetite and PO intake is %75%
Usual Meds or Dietary supplements; implications/pertinent side effects
Pt. has weaned himself off of insulin @ home but takes Metformin, Norvasc & Crestor
Medications in Hospital
Medication Implications/Pertinent Side Effects
Humalog
Levemir
Norvasc
Crestor
Metformin
Food allergies: Shellfish
Food intolerances: Pasta sauce, collard greens, spinach (other dark leafy greens) due to GERD
Stage of Change: Contemplation: pt. aware diet can affect DM but not motivated to change at this point.
Other Comments: Current diet Rx DM 1800 kcal recommend changing diet to 2000 kcal, " na, " chol,
" fat plus addition of HS snack (1/2 sandwich turkey/tuna) due to pt. reports of hunger & calculated EEN.
NUTRITION DIAGNOSIS(ES):
Problem Etiology (related to) Signs and Symptoms (as evidenced by)
P-E-S Statements:
Excessive carbohydrate intake related to food and nutrition compliance limitations evidenced by !
hemoglobin A1C of 11.1%, ! FSBG >120 mg/dL and verbalization of incomplete knowledge during
interview c " pt.
Limited adherence to nutrition-related recommendations related to food and nutrition related knowledge
deficit concerning how to make nutrition-related changes evidenced by expected laboratory outcomes not
achieved (A1c 11.1%), inability to recall DM diet, uncertainty as to how to consistently apply
food/nutrition information and lack of appreciation of the importance of making recommended nutrition-
related changes.
*Chosen due to RDs note in chart indicating that pt received extensive nutrition education regarding DM
diet. This is also the 2
nd
time pt. has been admitted to NUMC from ED for hyperglycemia. Pt. also
disclosed, he would rather die than miss the Super Bowl.
INTERVENTIONS (Food/and/or Nutrient Delivery; Nutrition Education; Nutrition Counseling;
Coordination of Nutrition Care)*
GOALS PLANS
Weight reduction 1# per week towards 215# (10%
wt. loss, BMI of 27.6).
Educate pt. on portion control (using DM
exchanges) 2000kcal diet pattern
Educate pt. on label reading make pt. aware
of serving sizes on label
Educate pt. on how wt. loss can benefit DM
To improve HbA1c of 11.1% towards 7%. Educate pt. to engage in carbohydrate counting
using DM exchanges (2000kcal diet pattern)
Educate on proper snacking, meals for ! BG
levels
Encourage pt. to continue to engage in self-
monitoring of blood glucose levels (pt. has
monitor @ home).
Recommend MD to discuss continuance of DM
diet education for pt. in NUMC Outpatient
Diabetes Clinic.
Using the Evidence Analysis Library evaluate one of your interventions and note the evidence for your
intervention.
SMBG is shown to be effective in improving HbA1c if subjects are aware of how to use the information to
make changes in their diabetes management (Grade II). H.W. has a blood glucose monitor at home but was
not aware of how helpful it can be in the management of diabetes. During education, we discussed how to
test blood sugars pre and post meals to see how the meals/certain foods affect the blood sugar level. I
encouraged H.W. to become a detective by keeping a log of foods and BG. I told H.W. this can help him
to become more hands on in his diabetic treatments (since his previous self-weaning of insulin indicates he
wants to be more in control of his disease). I wondered if he had self-weaned off of insulin because he did
not like needles but when asked the patient said he had no problem. Therefore, I think with this new
reinforcement and knowledge (including portion control), H.W. will be successful and have a more
managable HbA1c (~7%) in the near future. I have encouraged him to utilize the outpatient clinic at
NUMC for follow up.
MONITORING: # all that apply
___X_Weight __X___food intake at meals __N/A___supplement intake
__X___Labs (specify): FSBG to access DM control, BUN/Creat to access renal sufficency
Vous aimerez peut-être aussi
- Adime Case Study #19 Nutrition AssessmentDocument3 pagesAdime Case Study #19 Nutrition AssessmentJennifer BehiminoPas encore d'évaluation
- ADIME+Example 2Document3 pagesADIME+Example 2schmekshy1Pas encore d'évaluation
- Sample Case StudyDocument10 pagesSample Case Studyapi-702059884Pas encore d'évaluation
- 3 Adime Form For Diabete Case 1Document2 pages3 Adime Form For Diabete Case 1api-309275032Pas encore d'évaluation
- Adime Due 10 29Document3 pagesAdime Due 10 29api-437192216Pas encore d'évaluation
- Medical Nutrition TherapyDocument4 pagesMedical Nutrition TherapycjgregoryPas encore d'évaluation
- Celiac Adime FinalDocument2 pagesCeliac Adime Finalapi-287759747100% (1)
- Adime For DiabetesDocument2 pagesAdime For Diabetesapi-383891195Pas encore d'évaluation
- Adime Malnutrition and OncolgyDocument6 pagesAdime Malnutrition and Oncolgyapi-300587226100% (1)
- NCP RenalDocument22 pagesNCP Renalمحمود على ما تفرجPas encore d'évaluation
- Adime PT 2Document8 pagesAdime PT 2api-357368000Pas encore d'évaluation
- Report Kadaugan Sa MactanDocument15 pagesReport Kadaugan Sa MactanGem Benturado0% (1)
- 11 Nutrition Across The Lifespan - InfancyDocument39 pages11 Nutrition Across The Lifespan - InfancyKathleen AngPas encore d'évaluation
- Adime HenryDocument4 pagesAdime Henryapi-486579190Pas encore d'évaluation
- Adime NoteDocument2 pagesAdime Noteapi-383891195Pas encore d'évaluation
- Adime 1Document1 pageAdime 1api-308400395Pas encore d'évaluation
- Adime AssessmentDocument3 pagesAdime Assessmentapi-302346627Pas encore d'évaluation
- Oncology AdimeDocument2 pagesOncology Adimeapi-299929867Pas encore d'évaluation
- Adolescent Case StudyDocument2 pagesAdolescent Case Studydsaitta108Pas encore d'évaluation
- Scale For Ranking Health Conditions and Problems According To PrioritiesDocument2 pagesScale For Ranking Health Conditions and Problems According To PrioritiesJenina Kaye Mostoles GravidesPas encore d'évaluation
- Adime 2 FinalDocument2 pagesAdime 2 Finalapi-437596453Pas encore d'évaluation
- Nutr 425 Diabetes AdimeDocument3 pagesNutr 425 Diabetes Adimeapi-341618058Pas encore d'évaluation
- NCMA 215 Course Task 15 - Lecture Module Week 9: Andrea B. Autor BSN 2YC-2Document2 pagesNCMA 215 Course Task 15 - Lecture Module Week 9: Andrea B. Autor BSN 2YC-2Gina PrancelisoPas encore d'évaluation
- Nutrition Support Case StudyDocument6 pagesNutrition Support Case StudydakotaPas encore d'évaluation
- Final Adime Note AnemiacasestudyDocument2 pagesFinal Adime Note Anemiacasestudyapi-253526841Pas encore d'évaluation
- Adime 2 UchcDocument9 pagesAdime 2 Uchcapi-307029735Pas encore d'évaluation
- CVD Case StudyDocument4 pagesCVD Case Studyapi-435010651Pas encore d'évaluation
- NCP Online PortfolioDocument10 pagesNCP Online Portfolioapi-351011524Pas encore d'évaluation
- fshn420 - Cancer Case StudiesDocument5 pagesfshn420 - Cancer Case Studiesapi-703153445Pas encore d'évaluation
- Date Performed: August 18, 2015 Group No. and Section: Group 5 WCDE-A Date Submitted: September 1, 2015 Group MembersDocument28 pagesDate Performed: August 18, 2015 Group No. and Section: Group 5 WCDE-A Date Submitted: September 1, 2015 Group MembersCm MacaliaPas encore d'évaluation
- MNT pt1Document5 pagesMNT pt1api-339312954Pas encore d'évaluation
- Diabetes Mandatory Case Study AdimeDocument2 pagesDiabetes Mandatory Case Study Adimeapi-434982019Pas encore d'évaluation
- Nutrition & Diet Therapy: By: Odessa S. Bugarin, ManDocument46 pagesNutrition & Diet Therapy: By: Odessa S. Bugarin, ManWincy SalazarPas encore d'évaluation
- Adime Note PracticeDocument2 pagesAdime Note Practiceapi-497774789100% (1)
- Basic Information About Newborn ScreeningDocument5 pagesBasic Information About Newborn ScreeningJohn Ray AnderPas encore d'évaluation
- Final CTN Liver Cirrhosis Meal PlanDocument5 pagesFinal CTN Liver Cirrhosis Meal Planrafael514Pas encore d'évaluation
- Malnutriton Case StudyDocument4 pagesMalnutriton Case Studyapi-302848761Pas encore d'évaluation
- NCM 105 LEC DISCUSS Tools-NCPDocument36 pagesNCM 105 LEC DISCUSS Tools-NCPPatt100% (1)
- CHNDocument34 pagesCHNCatherine RomeroPas encore d'évaluation
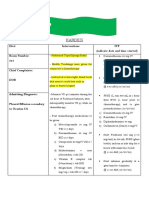
- Kardex: Diet: Interventions IVF (Indicate Date and Time Started) Room Number: 313Document2 pagesKardex: Diet: Interventions IVF (Indicate Date and Time Started) Room Number: 313kuro hanabusaPas encore d'évaluation
- Course ReflecDocument8 pagesCourse Reflecapi-301376054100% (1)
- Testing The DifferenceDocument42 pagesTesting The DifferenceHafiza IqraPas encore d'évaluation
- Case Study 1Document15 pagesCase Study 1api-272464131100% (2)
- NCM 105A Exercise 7 1Document6 pagesNCM 105A Exercise 7 1Mariel DimaculanganPas encore d'évaluation
- Adime Note Allison 2Document3 pagesAdime Note Allison 2api-457873289Pas encore d'évaluation
- Cancer and DietDocument34 pagesCancer and DietAyesha RazzaqPas encore d'évaluation
- Case Study Adime NoteDocument2 pagesCase Study Adime Noteapi-240616135Pas encore d'évaluation
- Bs NCPDocument10 pagesBs NCPapi-340851914Pas encore d'évaluation
- AdimeDocument4 pagesAdimeapi-307132349Pas encore d'évaluation
- Case Study FinalDocument2 pagesCase Study Finalapi-307578607Pas encore d'évaluation
- Nursing Care PlanDocument53 pagesNursing Care PlanAsma AlsaketPas encore d'évaluation
- Different Hospital Diet Handout 1 by Les'NitzDocument4 pagesDifferent Hospital Diet Handout 1 by Les'Nitzapi-3739910100% (1)
- Scale RankingDocument2 pagesScale Rankingapi-3728995Pas encore d'évaluation
- Adime Note TemplateDocument3 pagesAdime Note Templateapi-273243547100% (1)
- Calculation NCM 105 FinalsDocument6 pagesCalculation NCM 105 FinalsMa. Christina ConcepcionPas encore d'évaluation
- Activity # 2 - Santos, Aira Kristelle M.Document9 pagesActivity # 2 - Santos, Aira Kristelle M.Ai MendozaPas encore d'évaluation
- WEEK 3 Classification of Nutrients NutritionDocument33 pagesWEEK 3 Classification of Nutrients NutritionLaida PaguitalPas encore d'évaluation
- Valeriano - 3-Day Diet RecallDocument5 pagesValeriano - 3-Day Diet RecallCarl ValerianoPas encore d'évaluation
- Dietary TherapyDocument48 pagesDietary TherapyVanetPas encore d'évaluation
- Medicine and Nutrition Case StudyDocument5 pagesMedicine and Nutrition Case Studyapi-384113918Pas encore d'évaluation
- Resume - Di Grguric PDFDocument2 pagesResume - Di Grguric PDFapi-243208495Pas encore d'évaluation
- Liquacel Flier Draft bw2Document1 pageLiquacel Flier Draft bw2api-243208495Pas encore d'évaluation
- Clinical in Service Usct PDFDocument32 pagesClinical in Service Usct PDFapi-243208495Pas encore d'évaluation
- Toxic Epidermal Necrolysis - Grguric Case Study Presentation PDFDocument36 pagesToxic Epidermal Necrolysis - Grguric Case Study Presentation PDFapi-243208495Pas encore d'évaluation
- PMR BW 2ndDocument25 pagesPMR BW 2ndapi-243208495Pas encore d'évaluation
- PMR IrDocument29 pagesPMR Irapi-243208495Pas encore d'évaluation
- PMR 1st PDocument26 pagesPMR 1st Papi-243208495Pas encore d'évaluation
- Adimechart jg2Document3 pagesAdimechart jg2api-243208495Pas encore d'évaluation
- Tenbestbrainfoods 2Document1 pageTenbestbrainfoods 2api-243208495Pas encore d'évaluation
- AntioxfreeradflyerDocument1 pageAntioxfreeradflyerapi-243208495Pas encore d'évaluation
- Fiber HandoutDocument1 pageFiber Handoutapi-243208495Pas encore d'évaluation
- DmsupphandoutwipDocument1 pageDmsupphandoutwipapi-243208495Pas encore d'évaluation
- Potato Cabbage SauteDocument1 pagePotato Cabbage Sauteapi-243208495Pas encore d'évaluation
- Hidden Sugar Word SearchDocument1 pageHidden Sugar Word Searchapi-243208495Pas encore d'évaluation
- SSB Lesson Handout To Hand inDocument1 pageSSB Lesson Handout To Hand inapi-243208495Pas encore d'évaluation
- Nhanes IiiDocument9 pagesNhanes Iiiannaafia69969Pas encore d'évaluation
- Fall Forward: Guide To Picking Your Own Food at Local FarmsDocument8 pagesFall Forward: Guide To Picking Your Own Food at Local FarmsRSO Employment CenterPas encore d'évaluation
- MSM Information BookletDocument36 pagesMSM Information Bookletzimko100% (3)
- Metformin: Dosing & UsesDocument8 pagesMetformin: Dosing & UsesMaria Alejandra Siachoque JaraPas encore d'évaluation
- Insulin Infusion Protocol LaborDocument4 pagesInsulin Infusion Protocol LaborJohb CaballeroPas encore d'évaluation
- 1-Bank Soal TOEFLDocument72 pages1-Bank Soal TOEFLfadiah19Pas encore d'évaluation
- Jeff Cadge/the Image Bank/Getty ImagesDocument48 pagesJeff Cadge/the Image Bank/Getty ImagesdmcoombsPas encore d'évaluation
- Eaton, Konner, Shostak - 1988 - Stone Agers in The Fast Lane Chronic Degenerative Diseases in Evolutionary PerspectiveDocument11 pagesEaton, Konner, Shostak - 1988 - Stone Agers in The Fast Lane Chronic Degenerative Diseases in Evolutionary PerspectivelessentomePas encore d'évaluation
- Defeat Diabetes With A Vegan DietDocument48 pagesDefeat Diabetes With A Vegan DietVegan Future100% (1)
- 15 ConclusionDocument2 pages15 ConclusionAnjnaKandariPas encore d'évaluation
- Diabetic Foot ImfectionsDocument26 pagesDiabetic Foot ImfectionsYoga Pribadi UtomoPas encore d'évaluation
- Vedda Blood Sugar Remedy Web v2Document110 pagesVedda Blood Sugar Remedy Web v2thilanga100% (2)
- 12a Diabetic Emergencies DKA Case StudiesDocument13 pages12a Diabetic Emergencies DKA Case StudiesAnonymous yTdBi7100% (1)
- Abstract Book 19 OktDocument42 pagesAbstract Book 19 OktRika Fatmadona100% (1)
- How The First Nine Months Shape The Rest of Your LifeDocument9 pagesHow The First Nine Months Shape The Rest of Your Lifeمحمد عريف حكيم60% (5)
- Competency Appraisal 1 Disturbance in Metabolism EndocrineDocument46 pagesCompetency Appraisal 1 Disturbance in Metabolism EndocrineJohn Paul M. TagapanPas encore d'évaluation
- Gestational Diabetes Mellitus: Science in MedicineDocument7 pagesGestational Diabetes Mellitus: Science in MedicinerizqarrPas encore d'évaluation
- Raw Food Diet How It Reduces The Risks of Stroke Caused by The Typical American Diet in Conventional and Traditional Chinese Medicine PerspectivesDocument17 pagesRaw Food Diet How It Reduces The Risks of Stroke Caused by The Typical American Diet in Conventional and Traditional Chinese Medicine PerspectivesJohn NguyenPas encore d'évaluation
- Diabetes Type I Powerpoint 2Document10 pagesDiabetes Type I Powerpoint 2api-317440960Pas encore d'évaluation
- Project Information Cataloging System (PICS)Document68 pagesProject Information Cataloging System (PICS)Joshua Dela CruzPas encore d'évaluation
- CarePlan #2Document3 pagesCarePlan #2Monika StasiakPas encore d'évaluation
- Physical Education ProjectDocument47 pagesPhysical Education ProjectSaloni Roy100% (3)
- DM Type IIDocument48 pagesDM Type IILila HeridyatnoPas encore d'évaluation
- Psychology of Adulthood and Aging NotesDocument36 pagesPsychology of Adulthood and Aging Notesmerck0160% (5)
- A Short Review On Diabetes and Vilvam: December 2014Document5 pagesA Short Review On Diabetes and Vilvam: December 2014nasmiPas encore d'évaluation
- Insulin and Oral Hypoglycemic AgentsDocument27 pagesInsulin and Oral Hypoglycemic Agentsapi-19916399100% (1)
- 1 Pag 3Document14 pages1 Pag 3Mr. LPas encore d'évaluation
- Aoki Et. Al. v. Gilbert Et. Al.Document42 pagesAoki Et. Al. v. Gilbert Et. Al.PriorSmartPas encore d'évaluation
- Part 5 DrugsDocument35 pagesPart 5 DrugsJune Dumdumaya100% (4)
- 3071 Glicarea Si DiabetDocument41 pages3071 Glicarea Si DiabetKaycsa AdrianaPas encore d'évaluation